Abstract
Study Design: For certain condylar fractures, extracorporealization of the condylar segment may be performed via extra-oral vertical ramus osteotomy (EVRO) to facilitate reduction and fixation. This approach can similarly be used for condylesparing resection of osteochondromas of the condyle. Due to controversy regarding long-term health of the condyle after extracorporealization, we conducted a retrospective analysis of surgical outcomes. Objective: For certain condylar fractures, extracorporealization of the condylar segment may be performed via extraoral vertical ramus osteotomy (EVRO) to facilitate reduction and fixation. This approach can similarly be used for condylesparing resection of osteochondromas of the condyle. Due to controversy regarding long-term health of the condyle after extracorporealization, we investigated the viability of this technique through a retrospective analysis of outcomes. Methods: Twenty-six patients were treated using EVRO with extracorporealization of the condyle for both condylar fractures (18 patients) and osteochondroma (8 patients). Of the 18 trauma patients, 4 were excluded due to limited follow up. Clinical outcomes were measured, including occlusion, maximum interincisal opening (MIO), facial asymmetry, incidence of infection, and temporomandibular joint (TMJ) pain. Radiographic signs of condylar resorption were investigated, quantified, and categorized using panoramic imaging. Results: Average follow-up was 15.9 months. Average maximum interincisal opening was 36.8 mm. Four patients demonstrated mild resorption and one patient demonstrated moderate resorption. Two cases of malocclusion were attributed to failed repairs of other concurrent facial fractures. Three patients reported TMJ pain. Conclusions: Extracorporealization of the condylar segment with EVRO to facilitate open treatment of condylar fractures is a viable treatment option when more conventional approaches prove unsuccessful.
Introduction
Condylar fractures represent a unique challenge for the maxillofacial trauma surgeon. Fractures in this region of the mandible are common and may represent anywhere from 21.1% to 52% of all mandibular fractures [1,2,3]. In spite of their frequency, there still exists significant controversy regarding the most appropriate management [4]. Although many of these cases can be satisfactorily managed using a closed or non-surgical approach, it has become increasingly evident that open or surgical treatment should be considered the standard of care in a large percentage of these injuries, providing patients with superior outcomes in terms of long-term function and facial aesthetics [5,6]. This determination will often come down to an evaluation of multiple factors, including patient preference, patient comorbidities, surgeon preference and experience, fracture pattern, and the presence of concomitant fractures of the mandible and midface. Zide et al. [7] classically described four absolute and four relative indications for open reduction. However, innovations in rigid internal fixation, surgical techniques and computed tomography have given rise to new considerations in determining the approach to treatment [8,9]. Alyahya et al. [10] recently proposed an algorithm which advocates open treatment for any dislocated or displaced fractures or in any case where the occlusion cannot be reduced. Neff [11] suggests that open treatment should be considered the “gold standard” and recommends closed treatment for only select cases. In general, indications will vary between providers and often the decision will come down to a matter of individual training and experience [4,7].
Determining the most appropriate surgical access presents its own challenge. Several different approaches have been described with successful outcomes, including extraoral, intraoral, and endoscopic techniques [12,13]. Generally, the access chosen is based on the location of the fracture along the condylar process, as well as its degree of comminution and displacement. Additionally, improved access is balanced against the risk of complications, most notably facial nerve paresis and injury to the parotid gland [14,15]. Regardless of the approach, the access of choice must provide adequate exposure to allow for appropriate reduction and fixation of the fracture to achieve restoration or preservation of occlusion, pain-free function, and facial symmetry. Thus, in cases where conventional techniques fail to provide adequate access to achieve these goals, another technique has been proposed in which the displaced condylar segment is explanted to allow for direct visualization and manipulation of the fracture. Using an extraoral sub-sigmoid or vertical ramus osteotomy (EVRO) to facilitate removal of the distal segment of the fracture allows extracorporealization of the two segments so that they can be reduced and fixated on the surgical table. This technique was first described by Nam in 1978 with good clinical results over long-term follow-up. Boyne later described the same technique, which he implemented for treatment of condylar fractures, resection of bony pathology, and access for vascular surgical procedures involving the internal carotid artery [16,17]. Since these earlier reports, several studies have been published which demonstrate good functional outcomes and complication rates comparable to more conservative surgical approaches. In spite of this, significant controversy remains surrounding the use of this technique, particularly due to concerns related to the inherent loss of vascularity created by explantation of the mandibular segments [17,18,19,20].
This approach can similarly be used for the treatment of osteochondromas of the condyle in which a condyle-sparing resection is performed. Boyne [16] described the utility of the technique in oncological resection of the condyle. Choung et al. [17] implemented a similar technique using intraoral vertico-sagittal ramus osteotomy for recontouring of condylar hyperplasia. Pertaining specifically to osteochondromas, the unmatched access and direct visualization afforded by explantation of the condylar segment helps to ensure complete resection of the exophytic lesion in order to prevent recurrence [21]. As described by Meng et al. [22], the majority of these lesions (55.9%) present on the medial aspect of the condylar head, making proper access challenging. Creation of a vertical ramus osteotomy also helps to facilitate reconstruction. When at least half of the condylar head can be spared, as per the convention at our institution, the recontoured segment can be re-implanted as an autologous free bone graft, sparing the donor site morbidity associated with a costochondral graft. In the case of condylectomy, the condylar neck can be reshaped and repositioned superiorly to serve as a neo-condyle and this series of patients and the technique utilized has been previously described by our department [21,23].
Due to the controversy surrounding the technique and concerns regarding the long-term health of the condyle, we seek to demonstrate the viability of extracorporealization of the mandibular condyle for the treatment of patients with condylar process fractures and osteochondromas. We hope to show, via retrospective analysis, good clinical outcomes over long-term follow-up, particularly in regard to stability of patient function and occlusion.
Materials and Methods
This is a retrospective chart review of a consecutive series of patients treated from 2004 to 2019 via extracorporealization of the condylar segment using EVRO for condylar fractures and osteochondromas. Criteria for inclusion consisted of patients treated by the University of Maryland Department of Oral and Maxillofacial Surgery for condylar fractures, including condylar neck and condylar base fractures, and osteochondromas using the EVRO technique as described below. Criteria for exclusion included a complete lack of follow-up data for patients who could not be successfully contacted to arrange follow-up. These criteria were utilized for patients who were evaluated using clinical outcome measures, such as facial asymmetry and maximum interincisal opening (MIO). For patients who were additionally evaluated radiographically, exclusion criteria also included a lack of post-operative panoramic radiographs available on record taken at both short-term (within 2 weeks) and long-term (greater than 6 weeks) follow-up.
For patients with limited follow-up (less than 1 year after surgery), an attempt was made by the researchers to contact the patients for additional follow-up and panoramic imaging. Each of the patients who were successfully contacted signed an informed written consent explaining their participation in the study, including all potential risks and benefits involved. The performance of this chart review and the arrangement of additional follow-up were approved by the Institutional Review Board at the University of Maryland, Baltimore. The study was conducted in accordance with the Declaration of Helsinki regarding ethical principles and good clinical practices.
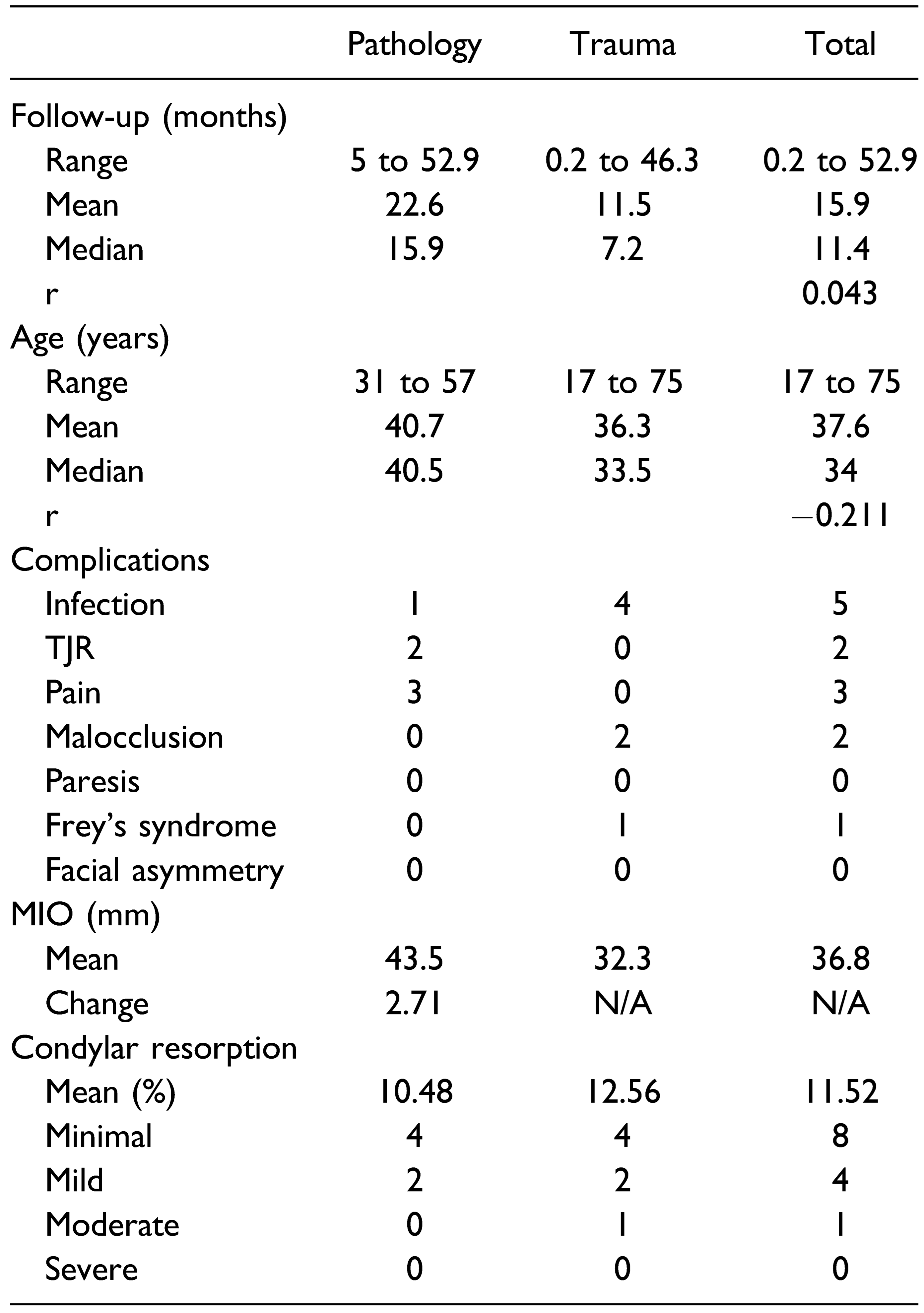
For each patient, clinical outcome measures and demographic data were collected from follow-up data including age at diagnosis, maximum interincisal opening (MIO), presence or absence of facial asymmetry, presence or absence of TMJ pain, presence or absence of malocclusion, incidence of post-operative infection, and need for further surgical intervention. Additionally, a comparison was made between baseline and follow-up imaging using panoramic radiographs to assess for radiographic evidence of condylar resorption in a vertical dimension for patients with appropriate post-operative imaging on record (n = 13). Per the exclusion criteria previously described, the baseline radiograph was taken post-operatively within 2 weeks of surgery and the follow-up radiograph was taken at least 6 weeks after surgery. These images were calibrated with MiPACS imaging software (Medicor Imaging, Charlotte, N.C.) using the diameter of a 2.0 mm screw head. The same screw head was used for both images in each patient. Then, using a technique previously described by J.M. Park et al., percent resorption of the condyle was calculated by comparing measurements of the vertical height of the condylar process between the two panoramic images. A horizontal line was drawn running tangential to the nadir of the sigmoid notch and measurements were then taken along a vertical line running perpendicular from this horizontal inferiorly to the apex of the condylar head superiorly (Figure 1) [18]. The degree of resorption was then calculated by dividing the difference between these measurements into the measurement for the first post-operative radiograph. All of the measurements were obtained by a single author (M.R.E.) using measurement tools available in the MiPACS imaging software. Resorption up to 25% of the condylar process was considered to be minimal and within the margin of error for the technique. Resorption between 26-50% was considered mild, 51-75% moderate, and 76-100% severe. A Pearson’s correlation coefficient (r) was calculated using Microsoft Excel for both age and length of follow-up as they relate to the degree of condylar resorption to better demonstrate the relationship of these variables.
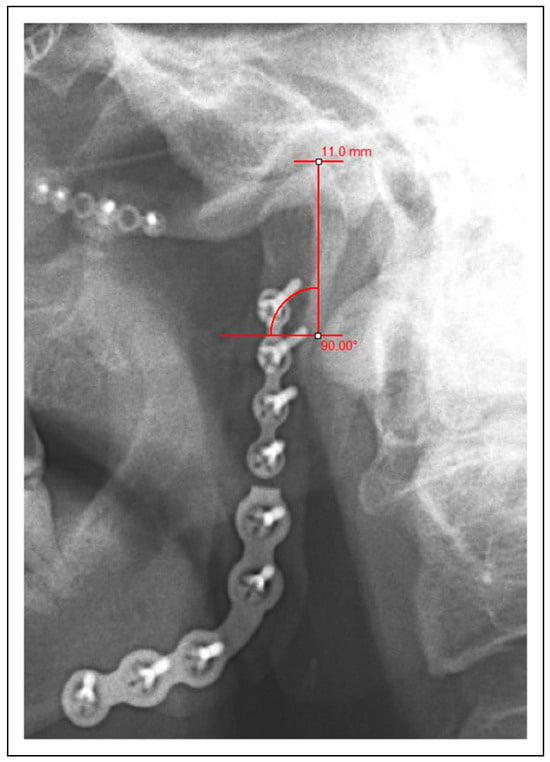
Figure 1.
Measurement of the condylar process on a postoperative panoramic radiograph using MiPACS imaging software. Calibration was performed using a 2.0 mm screw head. Measurements were taken from a horizontal line running tangential to the nadir of the sigmoid notch up to the apex of the condylar head along a perpendicular line.
The surgical technique utilized involved an extraoral approach in all cases using either a submandibular or retromandibular incision. For osteochondroma patients, a preauricular approach was also used in some cases. Once the fracture or lesion is exposed, the mandibular ramus is pre-plated with a fixation plate positioned across the line of the planned sub-sigmoid osteotomy. The osteotomy is performed with care taken to protect the inferior alveolar nerve and the mandibular segments are explanted. With direct access, the fracture can be properly reduced and fixated or the osteochondroma can be resected extracorporeally on the surgical table. The segment can then be re-implanted as a free bone graft and fixated in place using the pre-drilled screw holes once the occlusion has been verified (Figure 2). Maxillomandibular fixation was utilized or not utilized depending on surgeon preference and the status of concurrent fractures. This was performed using elastics, wire fixation or both and for a variable length of time ranging from 1 week to 2 months. There was no documented consistency in the prescribing of post-operative medications or physical therapy exercises.

Figure 2.
Extracorporealization of the mandibular condyle via EVRO in order to facilitate reduction and fixation of the fracture. The condylar fracture is reduced on the back table. The ramus was pre-plated prior to the creation of a sub-sigmoid osteotomy. The condylar process is then fixated to the ramus prior to re-implantation.
Results
In total, 26 patients were considered as part of our retrospective chart review, including 18 trauma patients and 8 osteochondroma patients. Four trauma patients were excluded from the series due to inadequate follow-up data. Two trauma patients were successfully contacted and brought back for additional follow-up and imaging. Final analysis included a total of 22 patients, 14 trauma patients and 8 osteochondroma patients. The patients had a mean age of 37.6 years with a range of 17 to 75 years. The patients had a mean follow-up of 15.9 months with a range of 0.2 to 52.9 months. Mean MIO was 36.8 mm. Of these 22 patients, 13 patients met criteria for radiographic analysis. The mean follow-up for these patients was 22.8 months with a range of 2.5 to 52.9 months. Mean condylar resorption in these patients was 11.5% with a range of –17 to 55.7%. Eight patients were found to have minimal resorption, 4 patients had mild and 1 patient had moderate resorption. No patients were found to have severe resorption. Out of the 22 patients seen in follow-up, only 2 patients were noted to have a malocclusion. These cases were attributed to failed repair of concurrent Le Fort level fractures in one case and failed repair of a concurrent dentoalveolar fracture in the other. Three patients reported TMJ pain. Five patients developed postoperative infection, 4 trauma patients and 1 osteochondroma patient. Two of these patients went on to require total joint replacement (TJR) with an alloplastic prosthesis, including one patient who underwent concurrent disc repositioning using Mitek anchors, which was not the case for any other patient included, and another patient with a history of kidney transplant who was on immunosuppressant medication. The other 3 patients were treated successfully with incision and drainage with or without hardware removal and antibiotics. One patient treated for osteochondroma developed Frey’s syndrome which was treated with Botox injections. There was no evidence of facial asymmetry or facial nerve deficit noted on follow-up (Table 1).

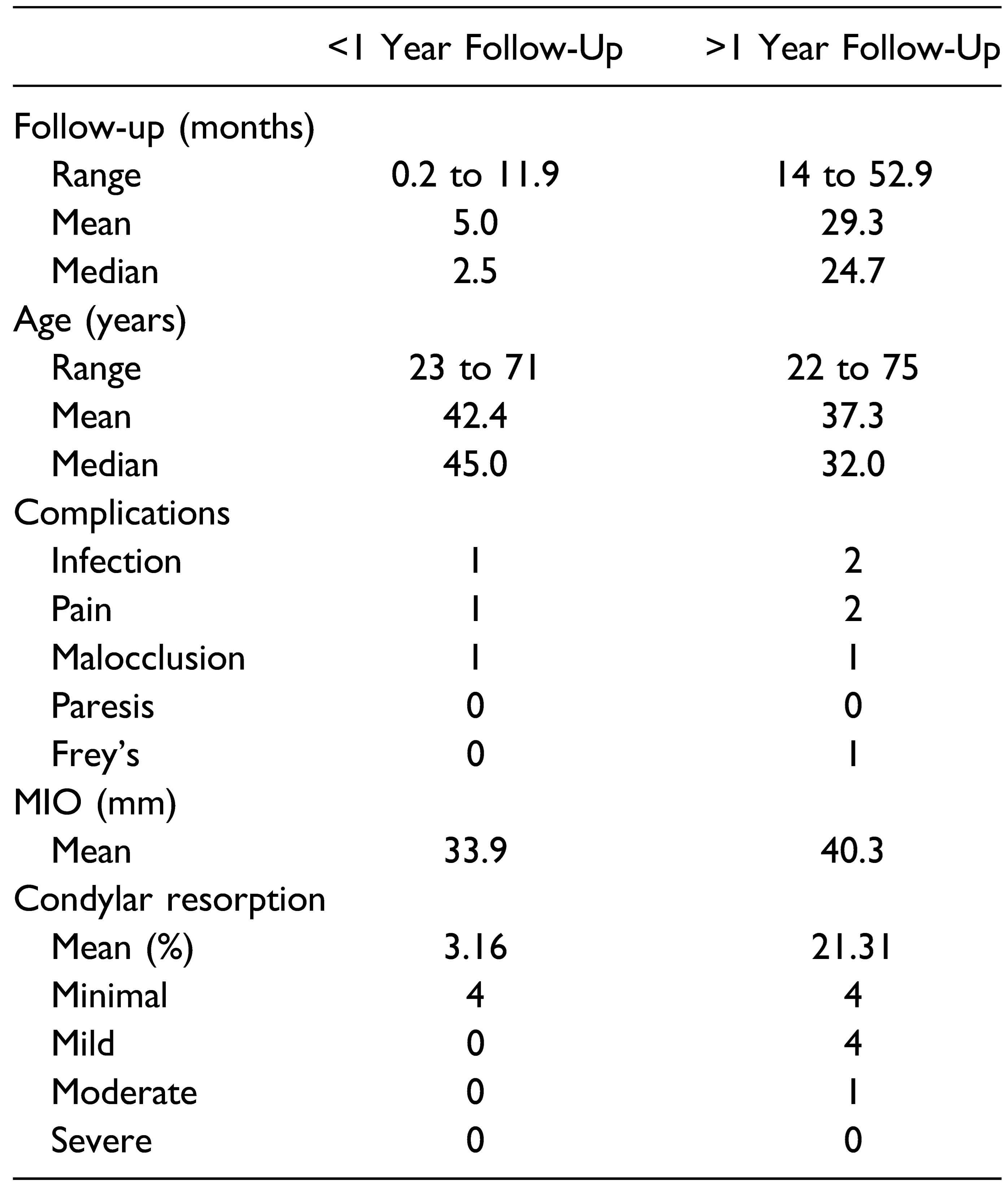
Table 1.
Summary of Length of Follow-Up, Age, Complication, MIO, and Condylar Resorption Data Including the Pearson’s Correlation Coefficient (r) for Age and Length of Follow-Up as They Relate to Condylar Resorption.
Differences in outcomes were noted when the patients were divided into pathology (i.e., osteochondroma) and trauma subgroups. Pathology patients demonstrated a greater mean MIO on follow-up as compared to trauma patients (43.5 mm vs 32.3 mm). Due to the nature of their initial presentation, a premorbid MIO was documented for the pathology patients, and for these patients, a change in MIO was calculated. Overall, these patients demonstrated a mean net improvement of 2.71 mm. Condylar resorption was similar between the two groups, with a slightly higher mean resorption for trauma patients (12.6% vs 10.5%). Of the patients considered to have mild resorption, 2 were pathology patients and 2 were trauma patients. The only patient with moderate resorption was a trauma patient. Length of follow-up differed between the two groups as well, and the average was substantially higher in the pathology group (22.6 months vs 11.5 months). There did not appear to be a strong correlation between patient age and condylar resorption (r = –0.21) or between length of follow-up and condylar resorption (r = 0.04) (Table 1). However, differences were appreciated when comparing patients with less than 1 year of follow-up to patients with greater than 1 year of follow-up. Mean MIO was greater for patients with greater than 1 year follow-up (40.3 mm vs 33.9 mm). Mean condylar resorption was also greater for patients with longer follow-up (21.31% vs 3.16%) and mild to moderate resorption was only seen in patients with greater than 1 year follow-up (Table 2).

Table 2.
Summary of length of follow-up, age, complication, MIO, and condylar resorption data for patients with less than 1 year of follow-up vs patients with greater than 1 year of follow-up.
Discussion
Since the technique was originally described, extracorporealization of the mandibular condyle with EVRO has been evaluated in multiple studies with largely successful outcomes. Despite the results of these studies, there remains controversy regarding the use of this technique and its effect on the long-term health of the condyle. By stripping the blood supply derived from the periosteum and the muscle attachment, the re-inserted condyle acts as a free autologous bone graft and is potentially vulnerable to significant resorption or potentially avascular necrosis [17,18,19,20]. Previous studies have demonstrated evidence of condyle resorption or remodeling on radiographic evaluation, but these findings do not appear to be associated with any significant effect on function or occlusion. Similarly, the patients in our series had good functional outcomes despite radiographic evidence of resorption in several patients.
Overall, we found an average condylar resorption of 11.5% with a range of -17 to 55.7%. When separating the patients by etiology, there appeared to be a slightly greater degree of resorption on average for the trauma patients (12.6% vs 10.5%). This difference was not particularly large and the sample size in our study was not sufficient to determine statistical significance. Furthermore, 3 of the patients in the pathology cohort had negative values which likely contributed to the difference in mean resorption. This finding was likely due to the technique utilized to perform our measurements. This technique was necessarily imperfect because of its reliance on the two-dimensional imaging (i.e., panoramic radiographs) available for these patients. These images were often taken by different technicians using different equipment with variable patient positioning. Improper patient angulation and positioning, radiographic artifact, and anatomic overlap all have the potential to introduce error in obtaining measurements. Because of this, we elected to utilize a convention similar to that described by S.Y. Park et al. [19] in which the patients were categorized as previously described into minimal, mild, moderate and severe resorption. The majority of the patients had minimal resorption, 2 trauma patients and 2 pathology patients had mild resorption and 1 trauma patient had moderate resorption. There were also differences noted when dividing patients into those with less than 1 year of follow-up and those with greater than 1 year follow-up. Nothing greater than minimal resorption was seen for patients at less than one year of follow-up and the average percent resorption was considerably lower for these patients. It stands to reason that condylar resorption would take time to become radiographically apparent and that patients with short-term follow-up may not demonstrate any appreciable change. Also of note, the 2 patients with greatest degree of resorption were also patients who developed surgical site infections post-operatively which were treated with incision and drainage and antibiotics and likely contributed to this resorption (Figure 3).
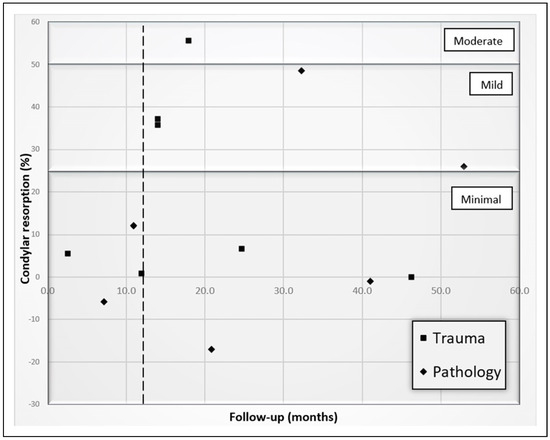
Figure 3.
Scatter plot of patients in our series comparing the percent condylar resorption seen radiographically with the follow-up time in months. Sections of the grid have been differentially shaded to highlight minimal, mild and moderate ranges of resorption and each data point is marked to differentiate between trauma and pathology patients per the legend. A dotted line has been added to better delineate one year of follow-up.
We assessed function in terms of post-operative range of motion of the mandible by assessing MIO, occlusion, and pain at follow-up. Per the AAOMS Parameters of Care, we considered any jaw opening >=35 mm to be within a functional and acceptable range [24,25]. The average MIO for our patients was above this threshold at 36.8 mm. In total, 13 of 20 patients had an MIO >=35 mm (the two patients who required total joint replacement were not included in this analysis). When separating the patients into trauma and pathology groups, the pathology group had better functional outcomes with both a greater mean MIO (43.5 mm vs 32.3 mm) and a greater number of patients with an MIO above the threshold for trismus (6 out of 8 vs 7 out of 12). These patients also demonstrated an average net improvement in opening on post-operative follow-up (2.71 mm). The more limited opening demonstrated by trauma patients could be attributed to concurrent soft tissue injury that occurred at the time of the fracture. Another possibility could be the difference in adherence to physical therapy and range of motion exercises between the trauma patients who presented acutely to our institution and the pathology patients who presented electively for evaluation and management of their lesions. Patients with less than 1 year of follow-up were noted to have a lower average MIO. This finding is likely influenced by the inclusion of several patients with only very short-term follow-up whose function may still be affected by post-surgical edema and would likely improve with more time and range of motion exercises. Previous studies of outcomes for closed and open treatment of condylar fractures reported post-operative MIO ranging from 28 to 48.7 mm for closed treatment and from 24.8 to 49.2 mm for open treatment [5,6]. As with the differences noted in condylar resorption, no significant comparisons can be made due to the small sample size.
Occlusion remained stable throughout follow-up in all pathology patients and in all trauma patients except for 2 patients. In both cases, the malocclusions identified could be easily attributed to the failed repair of concurrent facial fractures, including a Le Fort level fracture in one case and an anterior dentoalveolar fracture in the other. Only 3 patients endorsed TMJ pain which was described as mild or moderate. No facial asymmetries were noted on follow-up. Of note, all of the patients demonstrated deviation on opening toward the side of injury as a result of having stripped the attachment of the lateral pterygoid muscle during extracorporealization. However, this did not have any demonstrable effect on function. Five patients developed post-operative infection, 4 of whom were trauma patients. Although 3 of these patients recovered after incision and drainage and antibiotic treatment, 2 trauma patients went on to require total joint replacement. One of these two patients had a history of kidney transplantation and was on immunosuppressant medication which likely contributed to development and severity of the infection. The other patient had bilateral condylar fractures, only one of which was treated in an extracorporeal manner. However, Mitek anchors were placed bilaterally at the time of repair in order to reposition the disc. She subsequently developed surgical site infections bilaterally and ultimately required alloplastic joint replacement bilaterally. In both cases, it is likely that the poor vascularity of the re-implanted mandibular bone played a significant role in the evolution and severity of these infections. However, in both cases there are confounding elements which make causality more difficult to establish.
Outcomes were similarly good for previous studies which evaluated this technique. Boyne presented 15 cases which were followed for more than 8 years. On follow-up, he only noted the presence of a “slight resorption” which occurred during the first 2 post-operative years. He described the changes as a “slight flattening of the condyle” which appeared to be “consistent with physiological bone loss.” He did not note any occlusal discrepancies on follow-up, nor did the patients develop any TMJ pain or discomfort related to the procedure [16]. Gupta et al. reported 18 cases followed between 2 to 11 years and only noted resorption in 1 case. The patient experienced “complete resorption of the condylar head” during 11 years of follow-up. They reported mouth opening of between 35 and 43 mm after 6 months of follow-up, including 1 week of physiotherapy for all patients. They also reported 2 cases with “minor occlusal discrepancy” which were corrected with one week of light occlusal traction [20].
J.M. Park et al. compared outcomes between patients treated with extracorporeal fixation (35 patients) and those treated with closed reduction (36 patients) after 12 months of follow-up. The presence or absence of condyle resorption was determined on follow-up, defined as resorption of greater than 1/3 of the length of the premorbid condyle, and no significant difference was noted between the two treatment groups. However, they did find a significantly higher rate of resorption in condylar head vs neck fractures, complex or compound vs simple fractures, and displaced vs nondisplaced fractures. They noted five cases of malocclusion in the extracorporeal reduction group and three cases in the closed reduction group, which did not represent a significant difference [18]. S.Y. Park et al compared outcomes between three treatment groups: extracorporeal fixation, conventional open reduction, and closed reduction. Condylar resorption was measured and then categorized as severe (greater than 2/3 the length of the premorbid condyle), moderate (1/3 to 2/3), or mild (less than 1/3) with an average follow-up of 19 months. Four patients from the extracorporeal fixation group exhibited moderate resorption, while neither of the other 2 groups demonstrated appreciable resorption. They also found that comminuted fractures demonstrated a significantly higher rate of resorption compared with simple fractures. They reported an average MIO of 36.8 mm for their extracorporeal fixation group, which was similar to the other two groups [19]. Pain was identified in all three groups with no significant difference between them.
Our study is limited by a small sample size, making it impossible to draw statistically significant conclusions. We were also limited by the retrospective nature of the study design. Since the technique in question is necessarily more invasive than other approaches, it is rarely used in the treatment of condylar fractures, and only as a last resort when a less invasive surgical approach is not feasible. Additionally, the decision to utilize this approach is often made intraoperatively once the operator has already tried and failed to achieve adequate reduction and fixation via other means. On the other hand, osteochondromas are relatively rare and not every lesion can or should be treated using this technique. Because of these factors, even though a prospective randomized controlled trial would provide more compelling data, it would not be reasonable to study this technique in a prospective manner. There is also great deal of heterogeneity in the cases reviewed which limits our study. There are differences in the type of fixation utilized, the fracture patterns, the surgical access and the operators involved in treatment. As previously discussed, two-dimensional panoramic imaging was used for analysis of radiographic evidence of condylar resorption. The use of these images was unavoidable, but likely led to imperfect measurements of the condylar process. The potential inaccuracies in this analysis are an additional limitation of our study.
We were also limited by a lack of consist long-term follow-up, particularly in the trauma group. An examination of patient function and temporomandibular stability over a longer period of time could be useful, especially since one might expect to see bony remodeling continue to occur late in the post-operative course. Furthermore, as other studies have done, a comparison between the EVRO technique and conventional techniques may be useful in determining the degree to which extracorporealization contributes to increased bony resorption. However, as stated previously, this is a technique which is used at our institution as a last resort when other surgical approaches have failed, so a comparison between techniques would not make practical sense. Probably the most concerning finding in our study is the need for TJR in two of the cases reviewed. As discussed earlier, there are confounding variables which may have contributed to the eventual need for reconstruction though the vascularity of the condylar segment is of valid concern. One must also consider the fact that the symptoms which ultimately drove the decision to proceed with reconstruction (i.e., malocclusion and limited mouth opening) may also have resulted from an untreated or inappropriately treated fracture if managed using a more conventional approach.
Although there clearly exists a risk of radiographically evident condylar resorption, these changes do not appear to have any substantial effect on patient function, particularly in terms of mouth opening and occlusal stability. As this technique is unavoidably more invasive than conventional approaches, it should not be utilized routinely for condylar fracture repair. Further research is warranted, ideally with a greater sample size and longer follow-up. Overall, we feel that extracorporealization of the condyle via EVRO is a viable technique that can be utilized effectively in select cases with good functional outcomes and should be considered when other conservative surgical approaches are not possible.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Haug, R.H.; Prather, J.; Indresano, A.T. An epidemiologic survey of facial fractures and concomitant injuries. J. Oral Maxillofac. Surg. 1990, 48, 926–932. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E., 3rd; Moos, K.F.; el-Attar, A. Ten years of mandibular fractures: An analysis of 2,137 cases. Oral Surg. Oral Med. Oral Pathol. 1985, 59, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Zachariades, N.; Mezitis, M.; Mourouzis, C.; Papadakis, D.; Spanou, A. Fractures of the mandibular condyle: A review of 466 cases. Literature review, reflections on treatment and proposals. J. Cranio-Maxillo-Fac. Surg. 2006, 34, 421–432. [Google Scholar] [CrossRef]
- Ellis, E.; Throckmorton, G.S. Treatment of mandibular condylar process fractures: biological considerations. J. Oral Maxillofac. Surg. 2005, 63, 115–134. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Ellis, E. Surgical treatment of adult mandibular condylar fractures provides better outcomes than closed treatment: A systematic review and meta-analysis. J. Oral Maxillofac. Surg. 2015, 73, 482–493. [Google Scholar] [CrossRef]
- Chrzanovic, B.R. Surgical versus non-surgical treatment of mandibular condylar fractures: A meta-analysis. Int J Oral Maxillofac Surg 2015, 44, 158–179. [Google Scholar] [CrossRef] [PubMed]
- Zide, M.F.; Kent, J.N. Indications for open reduction of mandibular condyle fractures. J. Oral Maxillofac. Surg. 1983, 41, 89–98. [Google Scholar] [CrossRef]
- Haug, R.H.; Assael, L.A. Outcomes of open versus closed treatment of mandibular subcondylar fractures. J. Oral Maxillofac. Surg. 2001, 59, 370–376. [Google Scholar] [CrossRef]
- Brandt, M.T.; Haug, R.H. Open versus closed reduction of adult mandibular condyle fractures: A review of the literature regarding the evolution of current thoughts on management I. J. Oral Maxillofac. Surg. 2003, 61, 1324–1332. [Google Scholar] [CrossRef]
- Alyahya, A.; Bin Ahmed, A.; Nusair, Y.; Ababtain, R.; Allussain, A.; Alshafei, A. Mandibular condylar fracture: A systematic review of systematic reviews and a proposed algorithm for management. Br. J. Oral Maxillofac. Surg. 2020, 58, 625–631. [Google Scholar] [CrossRef]
- Neff, A. Open reduction and internal fixation in temporo-mandibular joint traumatology: Current concepts and future perspectives. Stomatol. Dis. Sci. 2019, 3, 2. [Google Scholar] [CrossRef]
- Haug, R.H.; Brandt, M.T. Traditional versus endoscope-assisted open reduction with rigid internal fixation (ORIF) of adult mandibular condyle fractures: A review of the literature regarding current thoughts on management. J. Oral Maxillofac. Surg. 2004, 62, 1272–1279. [Google Scholar] [CrossRef]
- Jensen, T.; Jensen, J.; Norholt, S.E.; Dahl, M.; Lenk-Hansen, L.; Svensson, P. Open reduction and rigid internal fixation of mandibular condylar fractures by an intraoral approach: A long-term follow-up study of 15 patients. J. Oral Maxillofac. Surg. 2006, 64, 1771–1779. [Google Scholar] [CrossRef]
- Rozeboom, A.V.J.; Dubois, L.; Bos, R.R.M.; Spijker, R.; de Lange, J. Open treatment of condylar fractures via extraoral approaches: A review of complications. J. Cranio-Maxillo-Fac. Surg. 2018, 46, 1232–1240. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Louvrier, A.; Colletti, G.; et al. Does the surgical approach for treating mandibular condylar fractures affect the rate of seventh cranial nerve injuries? A systematic review and meta-analysis based on a new classification for surgical approaches. J. Cranio-Maxillo-Fac. Surg. 2018, 46, 398–412. [Google Scholar] [CrossRef]
- Boyne, P.J. Free grafting of traumatically displaced or resected mandibular condyles. J. Oral Maxillofac. Surg. 1989, 47, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Choung, P.H.; Nam, H.V. An intraoral approach to treatment of condylar hyperplasia or high condylar process fractures using the intraoral vertico-sagittal ramus osteotomy. J. Oral Maxillofac. Surg. 1998, 56, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Park, J.M.; Jang, Y.W.; Kim, S.G.; et al. Comparative study of the prognosis of an extracorporeal reduction and a closed treatment in mandibular condyle head and/or neck fractures. J. Oral Maxillofac. Surg. 2010, 68, 2986–2993. [Google Scholar] [CrossRef]
- Park, S.Y.; Im, J.H.; Yoon, S.H.; Lee, D.K. A follow-up study on extracorporeal fixation of condylar fractures using vertical ramus osteotomy. J. Korean Assoc. Oral. Maxillofac. Surg. 2014, 40, 76–82. [Google Scholar] [CrossRef]
- Gupta, V.; Sahoo, N.K. Extracorporeal fixation of displaced mandibular condylar fracture: Viable option. Med. J. Armed Forces India 2009, 65, 229–231. [Google Scholar] [CrossRef]
- Ord, R.A.; Warburton, G.; Caccamese, J.F. Osteochondroma of the condyle: Review of 8 cases. Int. J. Oral Maxillofac. Surg. 2010, 39, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Meng, Q.; Chen, S.; Long, X.; Cheng, Y.; Deng, M.; Cai, H. Oral and maxillofacial radiology: The clinical and radiographic characteristics of condylar osteochondroma. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 114, e66–e74. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Lage, J.L.; Gonzalez, J.; Pineda, A.; Alvarez, I. Condylar reconstruction by oblique sliding vertical-ramus osteotomy. J. Cranio-Maxillofacial Surg. 2004, 32, 155–160. [Google Scholar] [CrossRef] [PubMed]
- AAOMS Parameters of Care: AAOMS Clinical Practice Guidelines for Oral and Maxillofacial Surgery (AAOMS ParCare), 6th ed.; Elsevier: Amsterdam, The Netherlands, 2017.
- Dijkstra, P.U.; Huisman, P.M.; Rodenburg, J.L. Criteria for trismus in head and neck oncology. Int. J. Oral Maxillofac. Surg. 2006, 35, 337–342. [Google Scholar] [CrossRef]
© 2022 by the author. Multimed Inc.