Comparison of Efficacy and Safety of Hybrid Arch Bar with Erich Arch Bar in the Management of Mandibular Fractures: A Randomized Clinical Trial
Abstract
:Introduction
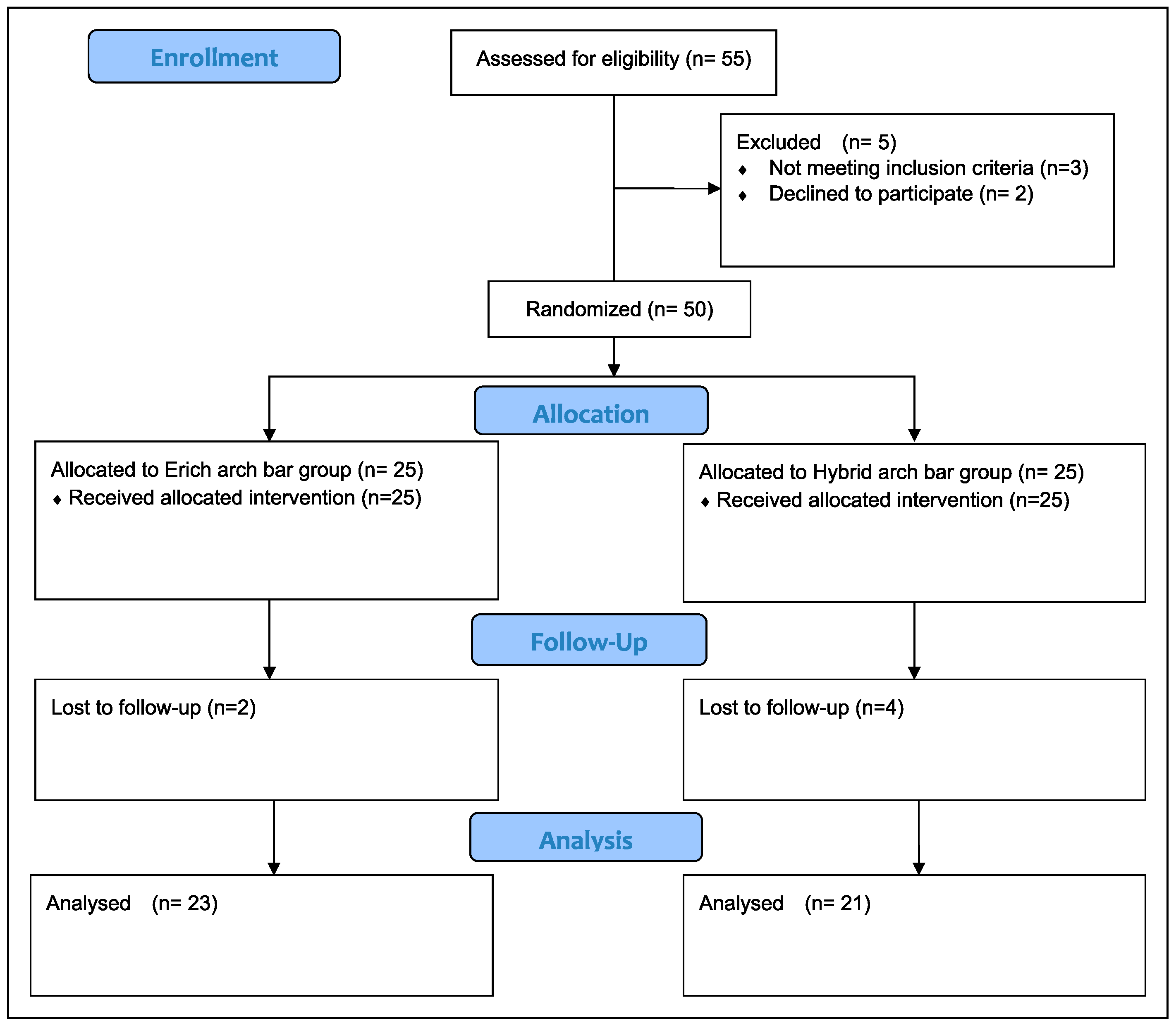
Materials and Method
- No debris present: 0
- Debris present but not covering the arch bar: 1
- Debris covering not more than half the arch bar: 2
- Debris covering more than half of the arch bar: 3
- No bleeding on provocation: 0
- Light bleeding on provocation: 1
- Moderate bleeding on provocation: 2
- Spontaneous bleeding: 3
- No gingival enlargement: 0
- Enlargement present but not covering the arch bar: 1
- Enlargement covering the arch bar: 2
- No soft tissue covering the screw head: 0
- Soft tissue covering not more than half the screw head: 1
- Soft tissue covering more than half the screw head: 2
- Soft tissue completely covering the screw head: 3
- Non-perceptible (no mobility): 0
- Mild (mobility less than 1 mm/loose hardware that can be tightened): 1
- Perceptible (mobility more than 1 mm/missing hardware or those hardware requiring removal): 2
Statistical Analysis
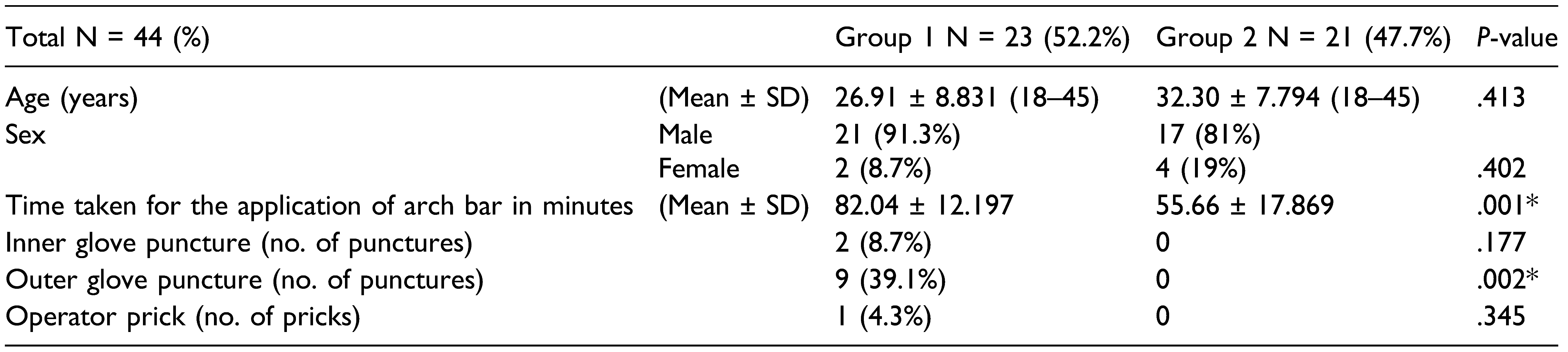
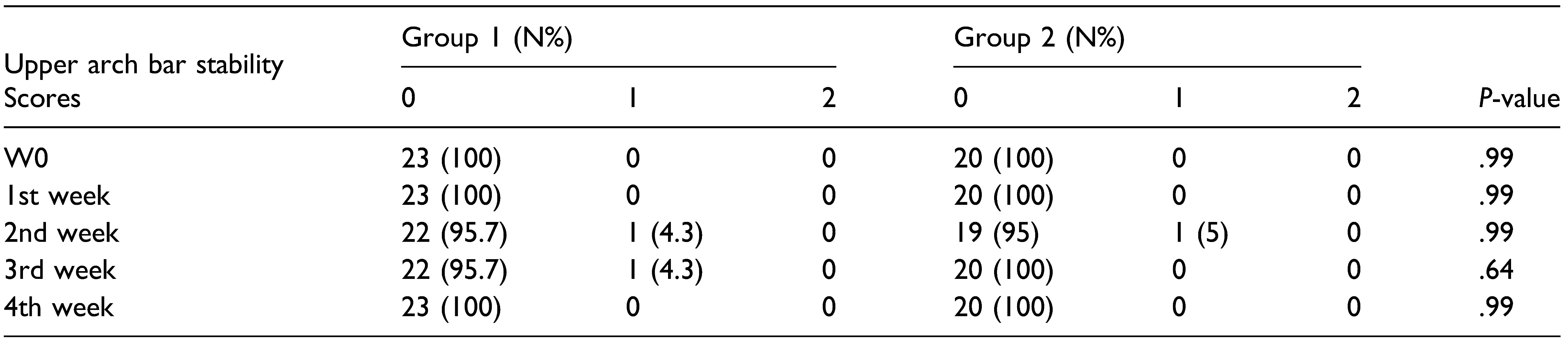
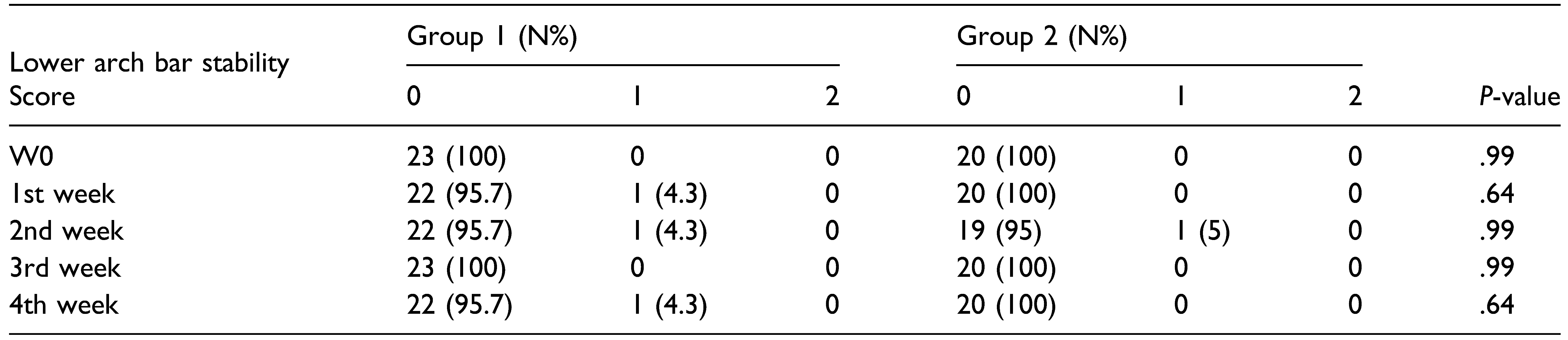
Results
Time Taken for the Application of Arch Bar
Operator Prick and Glove Puncture
Oral Hygiene
Discussion
Conclusion
Funding
Declaration of Conflicting Interests
References
- Kendrick, D.E.; Park, C.M.; Fa, J.M.; Barber, J.S.; Indresano, A.T. Stryker SMARTLock hybrid maxillomandibular fixation system: Clinical application, complications, and radiographic findings. Plast. Reconstr. Surg. 2016, 137, 142e–150e. [Google Scholar] [CrossRef] [PubMed]
- King, B.J.; Christensen, B.J. Hybrid arch bars reduce placement time and glove perforations compared with Erich arch bars during the application of intermaxillary fixation: A randomized controlled trial. J. Am. Associat. Oral Maxillofac. Surg. 2019, 77, e81228. [Google Scholar] [CrossRef] [PubMed]
- Chao, A.H.; Hulsen, J. Bone-supported arch bars are associated with comparable outcomes to Erich arch bars in the treatment of mandibular fractures with intermaxillary fixation. J. Oral Maxillofac. Surg. 2015, 73, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, A.; Reddy, U.; Warad, N.; Badal, S.; Jamadar, A.; Qurishi, N. Intermaxillary fixation screws versus Erich arch bars in mandibular fractures: A comparative study and review of literature. Ann. Maxillofac. Surg. 2016, 6, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Menon, G.; Rattan, V. Erich arch bar versus hanger plate technique for intermaxillary fixation in fracture mandible: A prospective comparative study. Natl. J. Maxillofac. Surg. 2018, 9, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Rai, A.; Datarkar, A.; Borle, R.M. Are maxillomandibular fixation screws a better option than Erich arch bars in achieving maxillomandibular fixation? A randomized clinical study. J. Oral Maxillofac. Surg. 2011, 69, 3015–3018. [Google Scholar] [CrossRef] [PubMed]
- Bouloux, G.F. Does the use of hybrid arch bars for the treatment of mandibular fractures reduce the length of surgery? J Oral Maxillofac Surg 2018, 76, 2595–2597. [Google Scholar] [CrossRef] [PubMed]
- Pieper, S.P.; Schimmel e, S.R.; Johnson, J.A.; Harper, J.L. A prospective study of the efficacy of various gloving techniques in the application of Erich arch bars. J. Oral Maxillofac. Surg. 1995, 53, 1174–1176. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, H.M.; Parhiz, A. Complications using intermaxillary fixation screws. J. Oral Maxillofac. Surg. 2011, 69, 1411–1414. [Google Scholar] [CrossRef] [PubMed]
- Alves, M.J.F.; Baratieri, C.; Araujo, M.T.S.; Souza, M.M.G.; Maia, L.C. Root damage associated with intermaxillary screws: A systematic review. Int. J. Oral Maxillofac. Surg. 2012, 41, 1445–1450. [Google Scholar] [CrossRef]
- Fabbroni, G.; Aabed, S.; Mizen, K.; Starr, D.G. Transalveolar screws and the incidence of dental damage: A prospective study. Int. J. Oral Maxillofac. Surg. 2004, 33, 442–446. [Google Scholar] [CrossRef]
- Hartwig, S.; Boettner, A.; Doll, C.; et al. Drill-related root injury caused by intraoperative intermaxillary fixation: An analysis of 1067 screw applications. Dent. Traumatol. 2017, 33, 45–50. [Google Scholar] [CrossRef]
- Coletti, D.P.; Salama, A.; Caccamese, J.F., Jr. Application of intermaxillary fixation screws in maxillofacial trauma. J. Oral Maxillofac. Surg. 2007, 65, 1746–1750. [Google Scholar] [CrossRef] [PubMed]
- Roccia, F.; Rossi, P.; Gallesio, C.; Boffano, P. Self-tapping and self-drilling screws for intermaxillary fixation in management of mandibular fractures. J. Craniofac. Surg. 2009, 20, 68–70. [Google Scholar] [CrossRef] [PubMed]
- Schulte-Geers, M.; Kater, W.; Seeberger, R. Root trauma and tooth loss through the application of pre-drilled transgingival fixation screws. J. Cran-Max-Fac. Surg. Off. Public. Eur. Assoc. Cran-Max-Fac. Surg. 2012, 40, e214–e217. [Google Scholar] [CrossRef] [PubMed]
- Nandini, G.D.; Balakrishna, R.; Rao, J. Self tapping screws v/s Erich arch bar for inter maxillary fixation: A comparative clinical study in the treatment of mandibular fractures. J. Maxillofac. Oral Surg. 2011, 10, 127–131. [Google Scholar] [CrossRef] [PubMed]
- West, G.H.; Alan Griggs, J.; Chandran, R.; Vincent Precheur, H.; Buchanan, W.; Caloss, R. Treatment outcomes with the use of maxillomandibular fixation screws in the management of mandible fractures. J. Oral Maxillofac. Surg. 2014, 72, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Van den Bergh, B.; Blankestijn, J.; Van Der Ploeg, T.; Tuinzing, D.B.; Forouzanfar, T. Conservative treatment of a mandibular condyle fracture: Comparing intermaxillary fixation with screws or arch bar. A randomised clinical trial. J. Cranio-Maxillofacial Surg. 2015, 43, 671–676. [Google Scholar] [CrossRef] [PubMed]
- Coburn, D.G.; Kennedy, D.W.G.; Hodder, S.C. Complications with intermaxillary fixation screws in the management of fractured mandibles. Br. J. Oral Maxillofac. Surg. 2002, 40, 241–243. [Google Scholar] [CrossRef] [PubMed]
- Khelemsky, R.; Powers, D.; Greenberg, S.; Suresh, V.; Silver, E.; Turner, M. The hybrid arch bar is a cost-beneficial alternative in the open treatment of mandibular fractures. Craniomaxillofacial Trauma. Reconstr. 2019, 12, 128–133. [Google Scholar] [CrossRef] [PubMed]
 |
 |
 |



© 2022 by the author. Multimed Inc.
Share and Cite
Sankar, H.; Rai, S.; Jolly, S.S.; Rattan, V. Comparison of Efficacy and Safety of Hybrid Arch Bar with Erich Arch Bar in the Management of Mandibular Fractures: A Randomized Clinical Trial. Craniomaxillofac. Trauma Reconstr. 2023, 16, 94-101. https://doi.org/10.1177/19433875221080019
Sankar H, Rai S, Jolly SS, Rattan V. Comparison of Efficacy and Safety of Hybrid Arch Bar with Erich Arch Bar in the Management of Mandibular Fractures: A Randomized Clinical Trial. Craniomaxillofacial Trauma & Reconstruction. 2023; 16(2):94-101. https://doi.org/10.1177/19433875221080019
Chicago/Turabian StyleSankar, Hariram, Sachin Rai, Satnam S. Jolly, and Vidya Rattan. 2023. "Comparison of Efficacy and Safety of Hybrid Arch Bar with Erich Arch Bar in the Management of Mandibular Fractures: A Randomized Clinical Trial" Craniomaxillofacial Trauma & Reconstruction 16, no. 2: 94-101. https://doi.org/10.1177/19433875221080019
APA StyleSankar, H., Rai, S., Jolly, S. S., & Rattan, V. (2023). Comparison of Efficacy and Safety of Hybrid Arch Bar with Erich Arch Bar in the Management of Mandibular Fractures: A Randomized Clinical Trial. Craniomaxillofacial Trauma & Reconstruction, 16(2), 94-101. https://doi.org/10.1177/19433875221080019




