Abstract
Study Design: Randomized Control Trial. Objective: A randomized control trial was planned to aim to assess whether subcutaneous Injection of Teriparatide and Tablet Reunion (combination of Cissus Quadrangularis and Dalbergia sissoo) improves maxillofacial fracture healing as compared to the control group. Methods: 24 patients of mandibular fracture with or without concomitant maxillofacial fractures were randomly divided into 3 equal groups (Group 1—Control, Group 2—Tablet Reunion, and Group 3—Injection Teriparatide) and the treatment duration was 4 weeks. Pain, fracture site mobility, bite force, serum markers, and radiographic healing were assessed preoperatively and postoperatively at regular intervals till 12 weeks. Results: Group 2 showed early pain relief, although it was insignificant. Group 3 showed the highest anterior bite force at all the time points. Change in mean posterior bite force (PBF) showed a statistically significant increase at 8th week and 12th week in intergroup comparison; however, at 12th week, Group 3 was significantly better than Group 1 and reported the highest posterior bite force compared to other groups. Serum calcium and PTH level showed no significant difference, whereas Serum ALP showed a statistically significant increase in Group 3. The radiographic assessment showed no significant difference among the 3 groups. Conclusions: Both the intervention group drugs showed a promising effect on accelerating the fracture healing and improving bite force restoration with the osteoanabolic action; however, early radiographic healing and increased serum osteogenic markers in Group 3 indicate its possible optimistic role in maxillofacial fracture healing.
Introduction
Fracture healing is a complex cascade that involves several local and systemic regulatory factors, cytokines, and hormones that recapitulates the sequential stages of embryonic endochondral ossification restoring the damaged skeletal organ to its pre-injury cellular composition, structure, and biomechanical function. Numerous surgical and non-surgical methods have been used in the past literature to facilitate fracture healing and reduce surgical morbidity [1,2,3,4,5,6].
In recent years, there has been a shift of interest in using osteoanabolic agents to promote fracture healing. Teriparatide is a recombinant protein form of parathyroid hormone consisting of the first (N-terminus) 34 amino acids, which is the bioactive portion of the hormone. Intermittent injection recombinant human PTH (Teriparatide) is the anabolic agent approved by the U.S. Food and Drug Administration in 2002 for osteoporosis management [7]. Teriparatide upregulates both bone formation and resorption, resulting in a net positive balance, maintained over the fulltime course. The term “anabolic window” refers to the proportion of bone production to resorption. In addition, during teriparatide treatment, dynamic bone histomorphometry parameters such as the percent of mineralization surface/bone surface (MS/BS %) correspond with serum PINP [8]. During the whole 24 months of teriparatide treatment, evidence from clinical trials reveals that bone growth outnumbers bone resorption.
The utilization of complementary and alternative medicine especially Ayurveda is a universal phenomenon, both in developing as well as developed countries. According to World Health Organization, 70–80% of the world’s population rely on nonconventional medicines mainly of herbal sources in their healthcare [9]. Fundamental research in the past centuries has shown bone healing properties of Cissus quadrangularis (CQ) and Dalbergia sissoo (DS). A combination of CQ (500 mg) and DS (400 mg)is commercially available as Tablet Reunion (TbR). CQ contains a high amount of carotene A, anabolic steroidal substances, and calcium, which have shown marked influence on the rate of fracture healing and quicker mineralization of the callus, thus shortening the bone healing duration. Recent animal and human studies have shown that a standardized extract made from leaves of DS has a significant osteogenic effect which was attributed to a novel compound caviunin 7-O-[β-D-apiofuranosyl-(1→6)-β-D glucopyranoside [10,11]. There is insufficient data in the literature for use of osteoanabolic drugs in the promotion of maxillofacial fracture healing. A prospective, randomized control trial was planned aiming to assess whether Injection Teriparatide (TPTD) and TbR improve maxillofacial fracture healing as compared to the control group. Further, the safety and efficacy of both these drugs were evaluated.
Materials and Methods
Trial Design
This was a single-center, open-labeled, parallel-group with active control, randomized control trial and was conducted in accordance with the Declaration of Helsinki regarding medical research in 2016 guidelines after obtaining ethical approval from Institutional Ethics Committee (AIIMS/IEC/ 2018/769)following CONSORT guidelines (Figure 1) and was registered with Clinical Trial Registry of India (CTRI/ 2019/07/020 148).
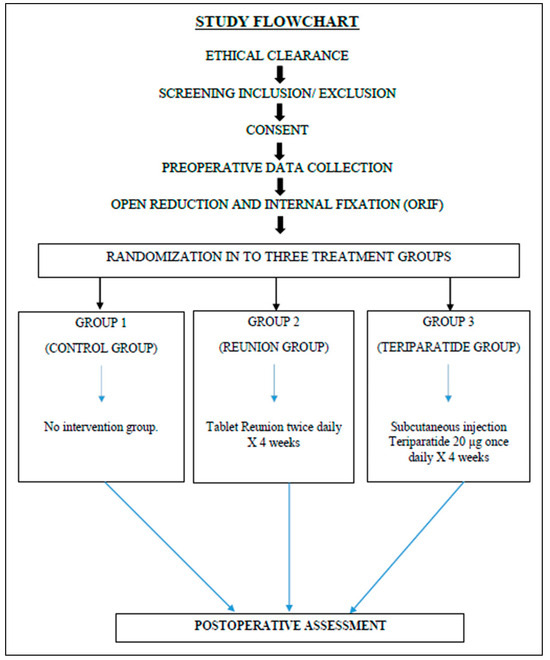
Figure 1.
Flowchart of the study.
Settings and Consents
All the patients with mandibular fractures with or without concomitant maxillofacial fractures visiting the Department of Dentistry or the Department of Trauma and Emergency of our Institute were analyzed from July 2019 to May 2020, and eligible patients fulfilling the inclusion and exclusion criteria were enrolled after taking the written informed consent.
Eligibility Criteria
The inclusion criteria for this study were as follows: ASA (American Society of Anesthesiologists) I and II patients with age group between 18–60 years in both the sex; patients of maxillofacial fracture including fracture mandible. Patients with hypercalcemia, Paget disease, malignant tumors, prior exposure to radiation treatment, less than 50% of teeth, myofascial pain dysfunction syndrome or temporomandibular joint dysfunction, significant polytrauma, and pregnant or lactating female patients were excluded from the study.
Sample Size Calculation
Assuming a standard deviation of 1.5 in the study group and 2.5 in the control group with an effect size of 1.5 and clinical meaningful mean difference of 3 weeks (although the study has a mean difference of 6.2) in 2 treatment groups, with 90% power and alpha error of 5%, the sample size is estimated to be 8 per treatment group.
Randomization, Allocation Concealment, and Blinding
Random allocation was done with a permuted block design using a computerized randomization allocation software 2.0 by an individual “A” with an allocation ratio of 1:1:1. Allocation concealment was ensured by using sequentially numbered opaque envelopes (SNOE) and different Individual “B” for patient recruitment. Both these individuals were unrelated to the study.
Intervention
In group 1, after Open reduction and internal fixation (ORIF) with semi-rigid fixation (titanium mini plates and screws), no fracture healing promoting drugs were administered. In group 2, TbR 1 tablet twice daily, and in group 3, 20 μg TPTD subcutaneously once daily with modified insulin pen were administered for 4 weeks after ORIF. No other osteogenic supplements like calcium and vitamin D were given throughout the treatment time.
Outcome Measures
- The pain was evaluated using a numerical rating scale (NRS) score preoperatively and postoperatively at first week, second week, fourth week, and sixth week.
- Fracture site mobility was evaluated preoperatively and postoperatively at first week, fourth week, and eighth week.
- In our study, we had used Flexi-force sensor for recording bite force which was standardized and calibrated by evaluating 20 healthy individuals. The mean ABF and PBF were recorded —140 N and 350 N, and these values were used for further comparison. ABF and PBF measurement was done in all the patients preoperatively and postoperatively at first week, second week, fourth week, sixth week, eighth week, and 12th week.
- Serum osteogenic markers (Ca, PTH, and ALP) were evaluated preoperatively and postoperatively at the fourth week.
Statistical Analysis
Data were expressed as mean ± standard deviation/error. Independent Student t-test was used for comparison of numerical variables between 2 groups. One-way ANOVA test followed by post-hoc was used to compare numerical data between 3 groups. Intragroup comparison of mean changes in outcomes was evaluated by Paired t-test. Pearson correlation coefficient was used to assess the correlation between parameters. Categorical data were analyzed using Fischer’s exact test or Chi-square test. Two-way ANOVA was used to assess the interaction of demographic variables with treatment categories. Analysis was done using SPSS version 23 (IBM Corp. Ltd, Newark, USA). A P-value less than .05 was considered to be significant.
Results
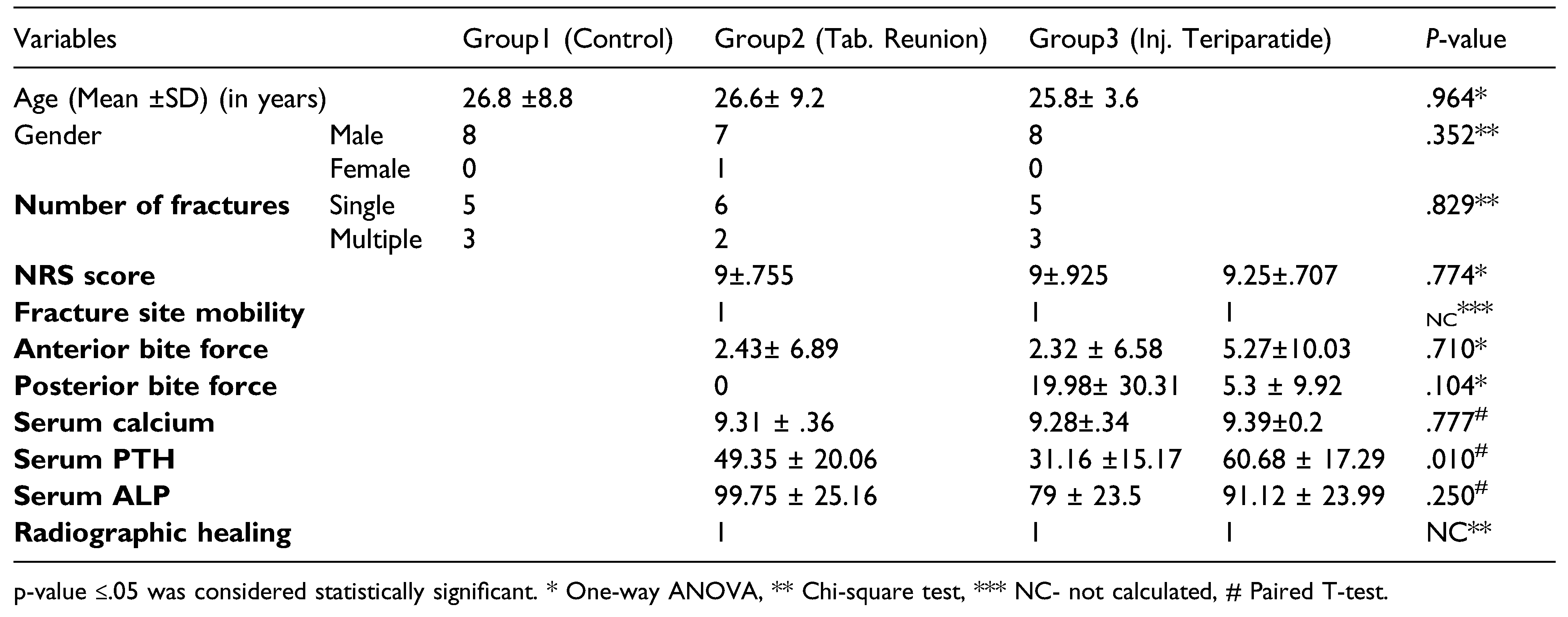
In our study (Table 1), patients were found to be homogeneously distributed in all the 3 groups as evident from statistically insignificant differences observed in relation to various demographic variables like age, gender, and type of fracture, and baseline parameters like pain, fracture site mobility, ABF and PBF, and serum osteogenic markers like serum calcium, serum ALP, and radiographic assessment as shown in Table 1. Preoperative serum intact PTH showed a significant difference with a P-value of .01. It was elevated in group 3.

Table 1.
Baseline demographic characteristics of Control and Treatment groups.
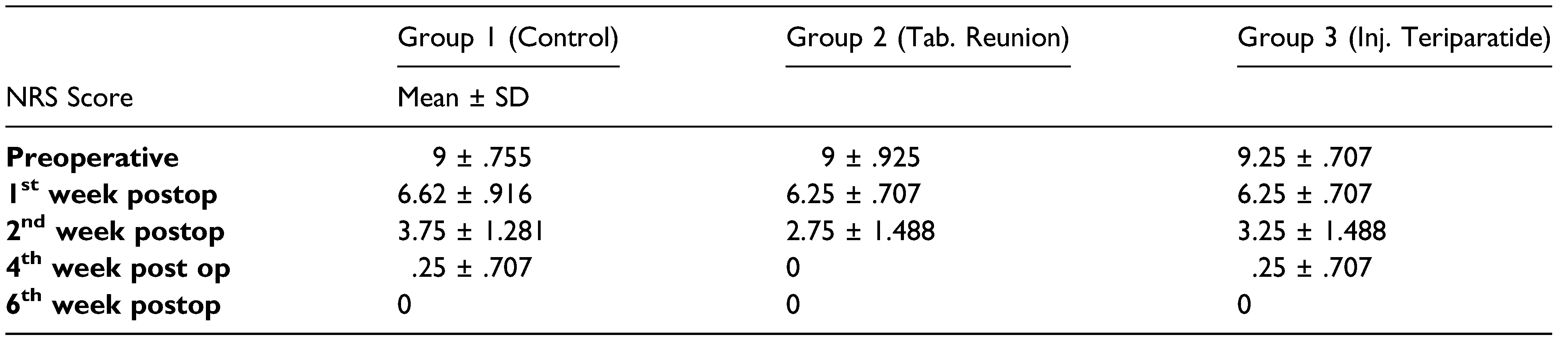
The mean NRS score progressively decreased in all the treatment groups at all time points. There was an early decrease in NRS score at second week and pain was absent at fourth week in group 2 as compared to the other groups on evaluation postoperatively as shown in Table 2.

Table 2.
Mean NRS score in the Control and Treatment groups.
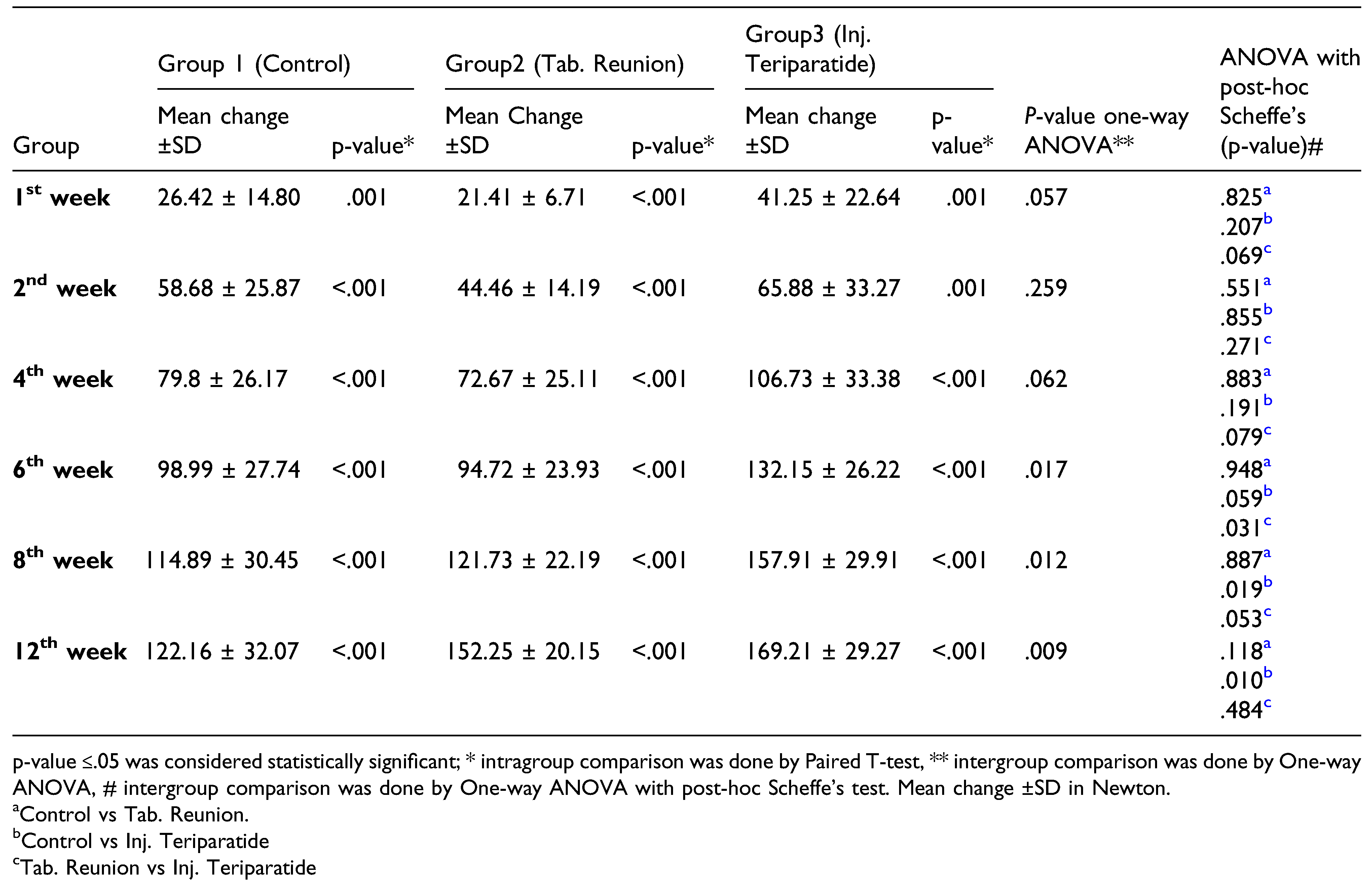
In group 1, 37.55% of patients regained normal mean ABF (140N) before 12 weeks, that is, 1 patient regained mean ABF in the sixth week and 2 in the eighth week. In group 2, 75% of patients (6/8) achieved normal mean ABF within 12 weeks. However, 87.5% of patients in group 3 showed better and speedy recovery in terms of ABF. There was a significant difference noted in intergroup comparison in mean change in ABF at sixth week (P = .017), eighth week (P = .012), and 12th week (P = .009). More patients in group 2 (6/8) and group 3 (7/8) achieved normal mean anterior bite force than group 1 (3/8). There was a statistically significant difference in intergroup comparison between group 2 and group 3 (P=.031) at the sixth week while comparing the change in mean ABF. At 8th week (P = .019) and 12th week (P = .010), a statistically significant difference was found while comparing group 1 and group 3 (Table 3). Kaplan–Meier survival curves showed a significant difference in the percentage of individuals achieving normal mean ABF in Group 3 as compared to Group 1 and Group 2 over 12 weeks (P-values – Log Rank = .016) (Figure 2).

Table 3.
Comparison of Mean change in anterior bite force in the Control and Treatment groups.
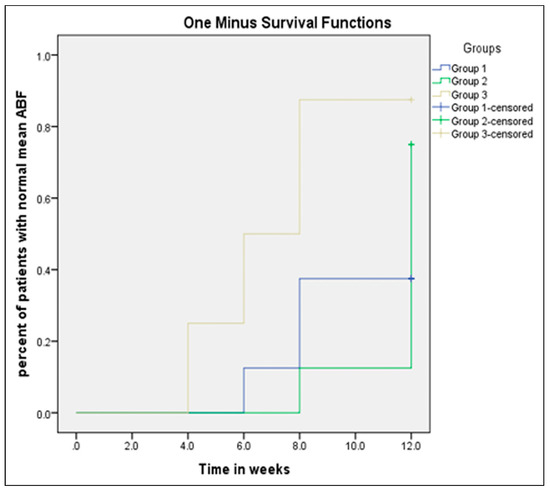
Figure 2.
Kaplan–Meier survival estimates. Proportion of patients achieving mean anterior bite force in weeks. The y-axis gives the proportion of patients who have achieved maximum anterior bite force over time (weeks on x-axis).
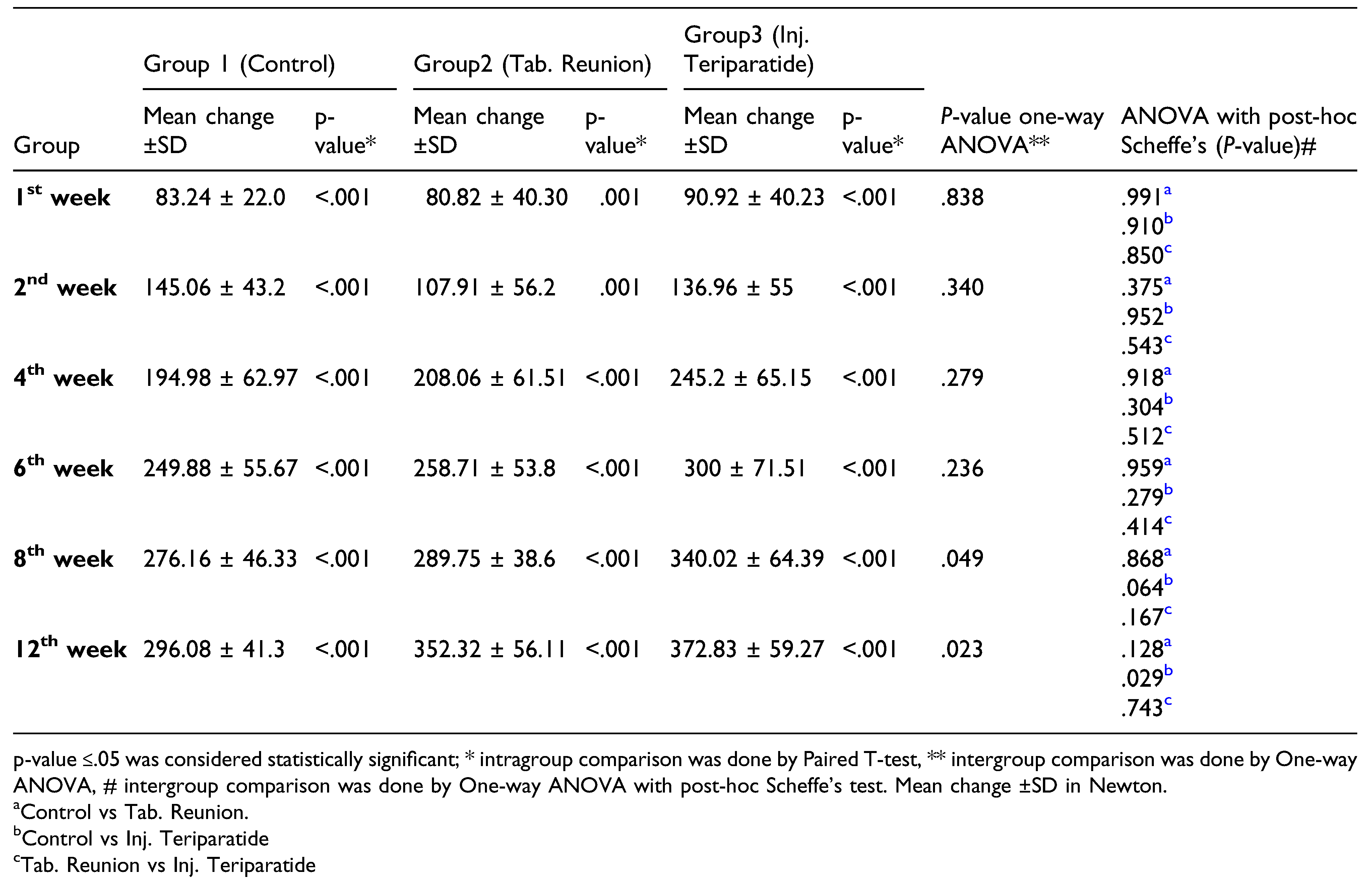
Group 1 showed delayed recovery as none of the patients regained normal mean PBF (350 N) by 12 weeks. In group 3, 62.5% of patients (5/8) achieved mean PBF by the 12th week (1 patient in the sixth week and 4 patients in the 12th week). The maximum number of patients with the return to normal PBF was observed in group 2 as 75% of patients, that is, 6/8 of patients achieved mean PBF at a final time point (12th week). Group 3, however, showed speedy recovery in terms of PBF by 1 patient out of 8 patients in the sixth week and 5/8 patients in the 12th week. The result of the intergroup comparison showed a significant difference at the eighth week (P = .049) and 12th week (P = .023). On intergroup comparison with post-hoc Scheffe’s test, at 12th week (P = .029), only group 3 was better than group 1 in mean change in PBF statistically (Table 4). As shown in Kaplan–Meier survival curves, there is a significant difference in the percentage of individuals achieving normal mean PBF in Group 3 as compared to Group 1 and Group 2 over 12 weeks (P-values – Log Rank = .009). (Figure 3)

Table 4.
Comparison of Mean change in posterior bite force in the Control and Treatment groups.
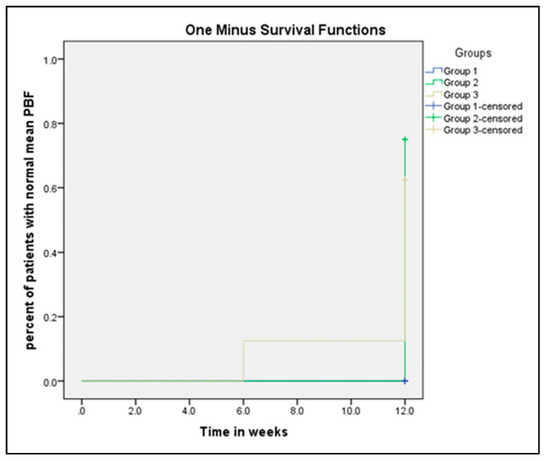
Figure 3.
Kaplan–Meier survival estimates. Proportion of patients achieving mean posterior bite force in weeks. The y-axis gives the proportion of patients who have achieved maximum posterior bite force over time (weeks on x-axis).
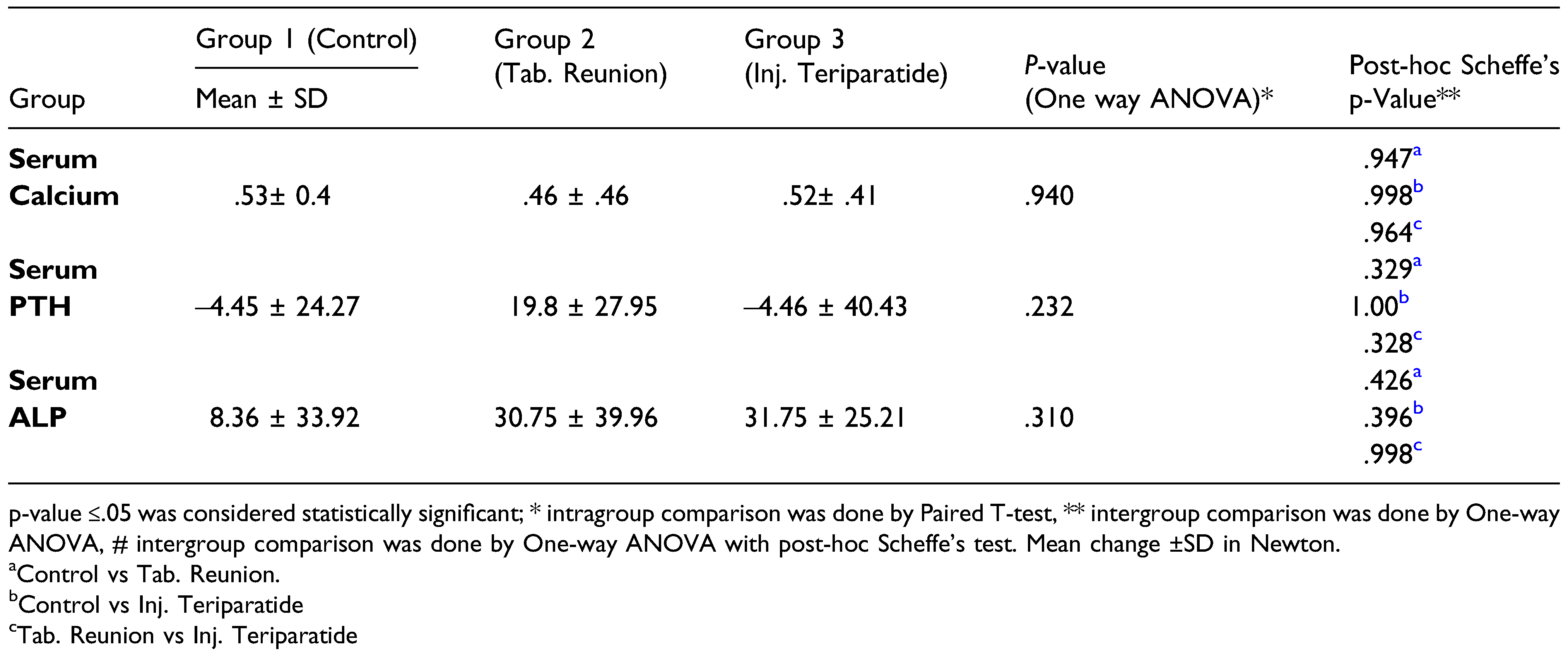
During the intergroup comparison, maximum mean serum calcium level at fourth week postoperatively was seen in group 3 followed by group 1 and group 2. Mean postoperative PTH level decreased in group 1 and group 3. Group 2 showed an increase in PTH levels. On intragroup comparison of preoperative and postoperative serum intact PTH level, there was no significant difference among the 3 groups. A rise in ALP was seen maximum in group 3 followed by group 2 and group 1. Group 3 showed a statistically significant increase in ALP on intragroup comparison, that is, preoperative ALP = 91.12±23.99 and postoperative ALP =122.87±28.37 (P=.009).
The intergroup comparison of mean change in serum osteogenic markers showed that there was no significant difference among the 3 groups (Table 5).

Table 5.
Mean change in Pre and Post Serum osteogenic markers.
The validity of radiological evaluation was established by evaluating 10 random OPGs of the patients by the same assessor after 2 weeks and generating intra-rater reliability of minimal discrepancy (kappa coefficient <.9) and confirming reliability and acceptability of OPG for the study.
Even though all the 3 groups showed progressive radiographic healing in OPG at all the time intervals, in group 3, 100% patients showed absence of fracture line on evaluation at 12th week. In group 2, 87.5% of patients, and in group 1, 62.5% of patients showed the same. Group 3 showed better radiographic healing compared to group 2 and group 1. No major complications were reported in both the intervention groups.
Discussion
Modern research efforts in fracture healing have focused on stimulating fracture healing by various surgical, pharmacological, cellular, and biophysical strategies. The interaction between the factors affecting fracture healing and their effects on callus formation is still incompletely explained. The use of newer drugs that can stimulate fracture repair with minimal side effects is an emerging field of experimentation, which would in turn reduce clinical and socio-economical problems associated with fracture healing.
There was a statistically insignificant difference in the preoperative NRS scores among the 3 treatment groups. ORIF may have helped to reduce the displaced fracture fragments in anatomical position and restricted the movement of fracture fragments, thus reducing the pain at 1st week in our study also. However, the early relief in pain reported in group 2 could be suggested due to the presence of flavonoids in DS which is known to inhibit prostaglandin synthesis. Since prostaglandins are involved in pain perception and are inhibited by flavonoids, it could be suggested that the reduced availability of prostaglandins due to the action of flavonoids of DS might be liable for its analgesic effect [12,13,14,15].
Evidence from studies evaluating pain with injection teriparatide is controversial. Some studies [16,17,18]. have shown improvement in pain perception in pelvic fractures of postmenopausal women, multiple osteoporotic vertebral compression fractures, and sacral insufficiency fractures after the use of subcutaneous teriparatide daily ranging from 8 weeks to 6 months. On the contrary, some authors [19,20] did not find any statistically significant pain improvement in postmenopausal women with proximal humerus fractures and distal radial fractures, respectively.
ORIF resulted in inadequate reduction and fixation for the fracture fragments, [21,22,23] and as a result, there was no postoperative fracture site mobility in any of the patients in all 3 groups. As a result, the true effect of both intervention drugs on improvement in fracture site mobility could not be evaluated in the present study. Its actual role in terms of mobility reduction may be evaluated in the closed reduction cases model which is rarely preferred as a treatment option these days.
The maximum bite force is significant parameter of masticatory function and is relatively easy to measure and analyze. When used in patients treated surgically for maxillofacial fractures, records of maximum bite force act as excellent assessment criteria for restoration of skeletal architecture and healing of the masticatory system. Bite force can either be measured directly by placing a transducer between a pair of the tooth or by indirect evaluation of bite force by employing other physiologic variables known to the functionally related to the force production.
Our results confirm the early return of bite force in the interventional group as compared to the control group. Interestingly, group 3 patients achieved mean ABF beyond the normal mean ABF (140 N) in the eighth week itself.
Group 2 showed a delayed catch-up in achieving normal mean ABF as compared to group 3. At 12 weeks, both group 2 and group 3 had mean ABF beyond normal, but these results were not seen in group 1. The Kaplan–Meier survival curve shows that outcome was achieved earlier in Group 3 (fourth week) in contrast to the 8th and 12th week of Group 2 and group 1, respectively. On analyzing the results, both group 2 and group 3 medications may be recommended as adjuncts for early bone healing therapy
Similar to mean ABF, mean PBF gradually increased after ORIF from first week to 12th week and it was consistently higher in group 3 followed by group 2 and group 1. However, there was no statistically significant difference in PBF at any of the time points in group 2 and group 3. The Kaplan–Meier survival curve shows that the outcome was achieved earlier in Group 3 (sixth week) in contrast to the 12th week of Group 2. A small sample size of our study may have been a reason to produce such inconclusive results. None of the patients in this study had confounding factors like preoperative TMD, orthodontic therapy, and missing tooth which could have affected bite forces.
Positive results have been found in terms of bite force which was found to be maximum in the CQ group compared to the control group [24,25]. As it is the first study on the effect of teriparatide in maxillofacial fractures, there is no preexisting data for its comparison in the restoration of bite force. The result of our study showed that at 12th week postoperatively, both group 2 and group 3 achieved more than normal threshold ABF (140N) and PBF (350N) as compared to the control group. These changes can be considered as an aid in the early healing of the bone and the restoration of the functional operation of the masticatory system.
Sufficient levels of calcium in the serum are necessary for the formation of the hydroxyapatite that helps to mineralize the fracture callus and gives bone its compressive strength. There was a significant increase in serum calcium (SCa) at the fourth postoperative week in all 3 groups, independent of the intervention used (P < .05) confirming the role of extracellular calcium in physiological bone healing. But this change is marginal as it is a known fact that calcium is a very well-regulated mineral in the human body. Under the influence of PTH, calcium levels may be increased or decreased as they both run in an intricate balance with each other. The increased levels of Ca in Group 3 were supported by Satterwhite et al., [23] who reported a transient increase in SCa level (4.25 h) which was returned to predose levels by 16–24 h after each dose following once daily subcutaneous administration of 20 μg teriparatide in osteoporotic patients. This transient increase in Sca is consistent with the known effects of endogenous PTH on mineral metabolism. Exogenous PTH in form of TPTD may have further heightened this response.
Increased levels of calcium in group 2 were further corroborated by a study by Mohammad et al., [26] who showed a significant increase in serum calcium levels in the CQ group as compared to the Ocimum sanctum group in mandibular fractures. However, Singh et al. [27] while comparing CQ, Moringaoleifera, and Osteoseal in mandibular fractures, showed an insignificant increase in calcium levels in the CQ group. A similar insignificant increase in calcium results was found by Rasale et al. [28] while evaluating CQ in long bone fractures.
PTH stimulates both bone formation and bone resorption, the duration, and periodicity of exposure to PTH govern the net effect on bone mass that is whether it is catabolic or anabolic [29]. Continuous exposure to PTH results in catabolic effects on the skeleton while an intermittent, low dose of PTH results in osteoanabolic effects. Group 1and group 3 showed increased serum calcium levels at the fourth week with decreased PTH levels which may be supported by the normal bone healing mechanism of the body. During normal fracture healing, calcium is required for mineralization and maturation of callus which leads to a decrease in extracellular calcium concentration giving positive feedback to PTH to increase serum calcium concentration by reabsorption, which further gives negative feedback to decrease PTH level [30]. This cycle of change in PTH levels in physiologic healing is known. However, when PTH is administered exogenously, the body response may change. The correlation analysis showed statistical significance in mean change in preoperative and postoperative serum calcium level and mean change in preoperative and postoperative serum PTH level, but there was no correlation with any other factors. Nan Ban et al., [31] showed that PTH levels were significantly higher at the seventh day and 14th day in normal hip fracture healing as compared to delayed healing patients. In our study, however, we have evaluated the PTH at the fourth week postoperatively. Anastasilakis et al. [32] noted that while administration of 20 μg teriparatide injection for 18 months, intact PTH remained suppressed as long as teriparatide was administered and increased after treatment discontinuation attributed to the suppressive effect of teriparatide. The amino terminal of PTH is probably the part of the molecule that exerts the negative feedback.
On intergroup comparison, however, there was no statistically significant difference among the 3 groups. This could be due to the smaller sample size. Although in normal fracture healing, serum ALP levels are known to rise, similar results were found with the use of CQ and teriparatide also. There are reported cases of extremely elevated levels of serum alkaline phosphatase after long-term administration of teriparatide for osteoporosis and rapid decline to normal serum levels after discontinuation of medication [33].
Pankaj et al. [34] noted fracture line which was visible at the baseline faded in subsequent study visits at the eighth week in plain radiograph in patients with a long bone fracture who were treated with DS. Brahmkshatriya et al. [35] reported there was early periosteal reaction and bridging between the fractures end at the site of mandibular fracture on the 21st day and complete deposition of the bone fragment on 45th day in CQ group. As compared to this, no clinical evidence of bridging between the bony fragment on the 21st postoperative day and minimum bridging at the site of fracture on the day of the 45th day was seen in the control group.
Kim et al. [36] in their case series of 3 patients with the femoral fracture treated with teriparatide, used a series of plain radiographs for the assessment of radiographic healing at postoperative second week, eighth week, and 1 year, and they reported abundant callus formation, progression of callus formation, and replacement of callus with hard bony callus. On the contrary, a recent systematic review of 3 trials on the effectiveness of teriparatide on fracture healing patients who were treated with teriparatide therapy reported that there was no statistically significant difference in fracture healing rate compared with the patients in the control group on radiographic assessment on plain radiographs. Due to the small sample size, a coherent pattern in correlation could not be ascertained.
Because TbR and TPTD need to be administered daily by oral route or subcutaneous injection, respectively, it is supposed to affect the patient’s acceptance and adherence. Compliance was defined as patient self-report of 80% of daily injections administrating since the previous visit. Acceptance of pen injection was asked verbally at each follow-up. Mild discomfort and scared while self-injection in the early days were reported by the patients, but they became more comfortable with use and learning was easy with self-injection pen over time. Considering the positive results obtained in respect to early functional recovery in Group 3, despite its price, it can be said to be prudent based on the cost-benefit ratio. As we have administered both the drugs for a short duration (4 weeks), there were no complications reported in the TPTD group and only 2 patients in TbR group reported nausea. This is in contrast to the literature available that the side effects associated with TPTD are seen initially and regress gradually with time.
Both the intervention group drugs showed a promising effect on accelerating fracture healing and improving functional outcome (bite force restoration) with the osteoanabolic action. However, there was no statistical difference in pain, fracture site mobility, radiographic healing, and serum markers except serum ALP level. Though not statistically significant but early radiographic healing, increased level of serum osteogenic markers, better restoration of bite force in TPTD group indicates its possible optimistic role in maxillofacial fracture healing. More studies with larger sample sizes are warranted to confirm the efficacy of these drugs in maxillofacial fracture.
Limitations of the Study
The sample size of the study was small. A larger sample size could have given conclusive propositions. The high cost of teriparatide is also one of the limiting factors against its routine use. Assessor blinding was ensured throughout the study, but different forms of the drug could not allow patient blinding. CT is a more accurate and reliable method with fewer chances of interpretation errors to evaluate bone formation radiographically, but we have used OPG only due to cost and associated radiation hazard.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank the patients for their cooperation and regular follow-up.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Appendix
| Abbreviations | |
| ABF | Anterior Bite Force |
| PBF | Posterior Bite force |
| PTH | Parathormone |
| ALP | Alkaline phosphatase |
References
- Kazem Shakouri, S.; Soleimanpour, J.; Salekzamani, Y.; Oskuie, M.R. Effect of low-level laser therapy on the fracture healing process. Laser Med Sci. 2010, 25, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Kyllönen, L.; D’Este, M.; Alini, M.; Eglin, D. Local drug delivery for enhancing fracture healing in osteoporotic bone. Acta Biomater. 2015, 11, 412–434. [Google Scholar] [PubMed]
- Anil, S.; Al-Sulaimani, A.F.; Beeran, A.E.; Chalisserry, E.P.; Varma, H.P.R.; Al Amri, M.D. Drug Delivery Systems in Bone Regeneration and Implant Dentistry [Internet]. In: Turkyilmaz I, ed. Current Concepts in Dental Implantology. InTech; 2015. Available online: http://www.intechopen.com/books/current-concepts-in-dentalimplantology/drug-delivery-systems-in-bone-regenerationand-implant-dentistry. (accessed on 28 December 2020).
- Petrisor, B.; Lisson, S.; Sprague, S. Extracorporeal shockwave therapy: A systematic review of its use in fracture management. Indian J Orthop. 2009, 43, 161. [Google Scholar]
- Pounder, N.M.; Harrison, A.J. Low intensity pulsed ultrasound for fracture healing: A review of the clinical evidence and the associated biological mechanism of action. Ultrasonics. 2008, 48, 330–338. [Google Scholar]
- Della Rocca, G. The science of ultrasound therapy for fracture healing. Indian J Orthop. 2009, 43, 121. [Google Scholar] [CrossRef]
- Brixen, K.T.; Christensen, B.; Ejersted, C.; Langdahl, B.L. Teriparatide (Biosynthetic Human Parathyroid Hormone 1-34): A New Paradigm in the Treatment of Osteoporosis. Pharmacol Toxicol. 2004, 94, 260–270. [Google Scholar]
- Silva, B.C.; Bilezikian, J.P. Parathyroid hormone: anabolic and catabolic actions on the skeleton. Curr Opin Pharmacol. 2015, 22, 41–50. [Google Scholar]
- Chan, K. Some aspects of toxic contaminants in herbal medicines. Chemosphere. 2003, 52, 1361–1371. [Google Scholar]
- Khedgikar, V.; Gautam, J.; Kushwaha, P.; et al. A standardized phytopreparation from an Indian medicinal plant (Dalbergia sissoo) has antiresorptive and bone-forming effects on a postmenopausal osteoporosis model of rat. Menopause. 2012, 19, 1336–1346. [Google Scholar]
- Kushwaha, P.; Khedgikar, V.; Gautam, J.; et al. A novel therapeutic approach with Caviunin-based isoavonoid that en routes bone marrow cells to bone formation via BMP2/Wntb-catenin signaling. Cell Death Dis 16.
- Migliaccio, S.; Brama, M.; Spera, G. The differential effects of bisphosphonates, SERMS (selective estrogen receptor modulators), and parathyroid hormone on bone remodeling in osteoporosis. Clin Interv Aging. 2007, 2, 55–64. [Google Scholar] [PubMed]
- Hajare, S.W.; Suresh, C.; Tandan, S.K.; Sarma, J.; Lal, J.; Telang, A.G. Analgesic and antipyretic activities of Dalbergia sissoo leaves. Indian J Pharmacol [Internet]. 2000, 32, 357–360. Available online: https://www.ijp-online.com/article.asp?issn=0253-7613 (accessed on 29 December 2020).
- Panthong, A.; Supraditaporn, W.; Kanjanapothi, D.; Taesotikul, T.; Reutrakul, V. Analgesic, anti-inflammatory and venotonic effects of Cissus quadrangularis Linn. J Ethnopharmacol. 2007, 110, 264–270. [Google Scholar] [PubMed]
- Mishra, G.; Srivastava, S.; Nagori, B.P. Pharmacological and Therapeutic Activity of Cissus Quadrangularis: An Overview 13.
- Waalen, J. Current and emerging therapies for the treatment of osteoporosis. J Exp Pharmacol. 2010, 121. [Google Scholar]
- Chen, C.M.; Lin, P.Y.; Chen, Y.C.; et al. Effects of teriparatide on lung function and pain relief in women with multiple osteoporotic vertebral compression fractures. Surg Neurol Int. 2014, 5 (Suppl. 7), S339–S342. [Google Scholar] [PubMed]
- Kasukawa, Y.; Miyakoshi, N.; Ebina, T.; et al. Enhanced bone healing and decreased pain in sacral insufficiency fractures after teriparatide treatment: retrospective clinical-based observational study. Clinical Cases in Mineral and Bone Metabolism. 2017, 14, 140. [Google Scholar]
- Johansson, T. PTH 1-34 (teriparatide) may not improve healing in proximal humerus fractures. Acta Orthop. 2016, 87, 79–82. [Google Scholar]
- Aspenberg, P.; Genant, H.K.; Johansson, T.; et al. Teriparatide for acceleration of fracture repair in humans: A prospective, randomized, double-blind study of 102 postmenopausal women with distal radial fractures. J Bone Miner Res. 2010, 25, 404–414. [Google Scholar]
- Vivek, G.K.; Shetty, A.; Vaibhav, N.; Imran, M. A comparative study of single 3-D titanium plate versus conventional Champy’s 2 miniplate fixation in the management of mandibular anterior fracture: A prospective clinical study. Journal of Advanced Clinical & Research Insights. 2016, 3, 194–199. [Google Scholar]
- Al-Moraissi, E.A.; Mounair, R.M.; El-Sharkawy, T.M.; El-Ghareeb, T.I. Comparison between three-dimensional and standard miniplates in the management of mandibular angle fractures: a prospective, randomized, double-blind, controlled clinical study. Int J Oral Maxillofac Surg. 2015, 44, 316–321. [Google Scholar] [PubMed]
- Sehgal, S.; Ramanujam, L.; Prasad, K.; Krishnappa, R. Threedimensional v/s standard titanium miniplate fixation in the management of mandibular fractures A randomized clinical study. J Cranio-Maxillofacial Surg. 2014, 42, 1292–1299. [Google Scholar]
- Mohammad, S.; Pal, U.; Pradhan, R.; Singh, N. Herbal remedies for mandibular fracture healing. Natl J Maxillofac Surg. 2014, 5, 35. [Google Scholar] [PubMed]
- Singh, N.; Singh, V.; Singh, R.; Pant, A.; Pal, U.; Malkunje, L.; et al. Osteogenic potential of cissus qudrangularis assessed with osteopontin expression. Natl J Maxillofac Surg. 2013, 4, 52. [Google Scholar]
- Satterwhite, J.; Heathman, M.; Miller, P.D.; Mar´ın, F.; Glass, E.V.; Dobnig, H. Pharmacokinetics of Teriparatide (rhPTH[1-34]) and Calcium Pharmacodynamics in Postmenopausal Women with Osteoporosis. Calcif Tissue Int. 2010, 87, 485–492. [Google Scholar]
- Singh, V.; Pal, U.; Mohammad, S.; Singh, N.; Dhasmana, S.; Singh, N. Clinical evaluation of cissus quadrangularis and moringa oleifera and osteoseal as osteogenic agents in mandibular fracture. Natl J Maxillofac Surg. 2011, 2, 132. [Google Scholar] [PubMed]
- Rasale, P.L.; Raut, S.Y.; Narkhede, H.P.; Muddeshwar, M.G. Biochemical and hormonal evaluation of Cissus quadrangularis in accelerating healing process of bone fracture: A clinical study. Int J Res Ayurveda Pharm. 2014, 5, 461–469. [Google Scholar]
- Thouverey, C.; Caverzasio, J. Suppression of p38α MAPK Signaling in Osteoblast Lineage Cells Impairs Bone Anabolic Action of Parathyroid Hormone. J Bone Miner Res. 2016, 31, 985–993. [Google Scholar]
- Khan, M.; Jose, A.; Sharma, S. Physiology, Parathyroid Hormone. [Internet]. StatPearls , Treasure Island (FL). StatPearls Publishing; 2020. Available online: http://www.ncbi.nlm.nih.gov/books/NBK499940/ (accessed on 29 December 2020).
- Ban, Z.-N.; Li, Z.-J.; Gu, Q.-S.; Cheng, J.; Huang, Q.; Xing, S.-X. Correlation of serum PTH level and fracture healing speed in elderly patients with hip fracture. J Orthop Surg Res. 2019, 14, 361. [Google Scholar]
- Anastasilakis, A.D.; Polyzos, S.A.; Goulis, D.G.; Slavakis, A.; Efstathiadou, Z.; Kita, M.; et al. Endogenous intact PTH is suppressed during Teriparatide (rhPTH 1-34) administration in postmenopausal women with established osteoporosis. Endocr J. 2008, 55, 613–616. [Google Scholar]
- Javinani, A.; Aghaei Meybodi, H.R.; Kavosi, H. Extremely elevated serum alkaline phosphatase level upon treatment with teriparatide: a case report. J Med Case Rep. 2020, 14, 87. [Google Scholar] [PubMed]
- Amol, D. Safety and Efficacy of a Standardized Extract from Leaves of Dalbergia sissoo in Healing of Long Bone Fracture: A Pilot Clinical Study. J Complement Med Altern Healthc [Internet]. 2018, 5. Available online: https://juniperpublishers.com/jcmah/JCMAH.MS.ID.555654.php (accessed on 22 December 2020).
- Brahmkshatriya, H.R.; Shah, K.A.; Ananthkumar, G.B.; Brahmkshatriya, M.H. Clinical evaluation of Cissus quadrangularis as osteogenic agent in maxillofacial fracture: A pilot study. Ayu. 2015, 36, 169–173. [Google Scholar]
- Kim, S.-M.; Kang, K.-C.; Kim, J.W.; Lim, S.-J.; Hahn, M.H. Current Role and Application of Teriparatide in Fracture Healing of Osteoporotic Patients: A Systematic Review. Journal of Bone Metabolism. 2017, 24, 65. [Google Scholar] [PubMed]
© 2022 by the author. The Author(s) 2022.