Abstract
Study Design: Systematic review. Objective: There is a growing trend toward evidence-based management of third molars in the fracture line of mandibular angle fractures (MAFs). This study aimed to differentiate MAF fixation complications by degree of third molar eruption and by extraction strategy in patients undergoing Champy fixation. Methods: PubMed, EMBASE, OVID, SCOPUS, the Cochrane Library, and clinicaltrials.gov were queried through May 2020 for English-language publications for MAFs with third molar involvement for this systematic review. Bias was assessed using author-defined criteria. Relative risk (RR) of post-operative complications associated with extracted unerupted and retained partially erupted third molars (Group I) was calculated against controls of retained unerupted and extracted partially erupted third molars (Group II). Results: Ten studies reported complications by eruption or extraction; however, only one study stratified complications by both eruption and extraction to meet inclusion criteria. The risk of bias was medium as only cases meeting defined follow-up were included. 73 cases (N) were included: 34 qualified for Group I and 39 for Group II. Quantitative synthesis of individual case data demonstrated significantly higher complication rate in Group I compared to Group II (23.5% vs 5.1%) (RR 4.6, 95% CI 1.04–20.1). No significant differences were observed between groups for infectious complications, mechanical complications, nonunion, or dehiscence. Reoperation was required significantly more often for Group I (P = 0.043). Conclusions: For MAFs involving the third molar, concomitant extraction of unerupted as well as retention of partially erupted third molars increases risk of complications with Champy fixation technique. For these patients, alternative strategies for fixation should be considered.
1. Introduction
Championed by Ellis and colleagues and validated by many others, Champy et al.’s fixation technique is the contemporary preferred treatment for noncomminuted mandibular angle fractures (MAFs) in dentulous patients. [,,,] Irrespective of fixation choice, managing third molars in the line of fracture via extraction or retention has largely been operator dependent. [] In 2019, Khavanin et al.’s meta-analysis introduced high-level evidence for third molar management, and identified concomitant extraction as a risk factor for inferior alveolar nerve morbidity. [] This was a crucial step in shifting the rationale behind operative decisions away from surgeon dogma and toward uniform evidence-basis. Still poorly defined, however, is how the degree of third molar eruption in relation to extraction management influences post-operative complications.
Among patients undergoing Champy fixation for MAFs involving the third molars that are not fully erupted, does the degree of third molar eruption in combination with operative management correlate with worse surgical outcomes, including dehiscence, infection, nonunion, hardware failure, malocclusion, and need for reoperation? Rooted in the concepts of extraction impacting bone stock and pericoronitispropagating wound morbidity, we hypothesize that either concomitant extraction of unerupted third molars or retention of partially erupted third molars comprises a “highrisk” course of operative management, resulting in greater complication burden. We performed a systematic review of available literature to evaluate if our hypothetical high-risk operative management group (i.e., extraction of unerupted + retention of partially erupted third molars) has an increased risk of post-operative complications than a hypothetical low-risk group (i.e., retention of unerupted + extraction of partially retained third molar).
2. Methods
2.1. Study Design and Sample
To address the research purpose, the investigators used the Preferred Reporting Items for Systematic Review and MetaAnalysis Protocols (PRISMA-P) 2015 to design this systematic review’s protocol. The null hypothesis considered neither degree of third molar eruption nor concurrent tooth extraction or retention during Champy fixation to influence post-operative complication occurrence.
The studies reviewed were generated from online searches of PubMed, SCOPUS, OVID, EMBASE, the Cochrane Library, and clinicaltrials.gov, performed in May 2020 without date restrictions, using combinations of the following: “mandibular angle fracture”, “third molar”, “eruption OR impaction”, “tooth in line of fracture”, “one vs two miniplate fixation”, “Champy”, “single miniplate”, and “double miniplate.” Citation sources of existing metaanalyses were consulted. [,,] Reference lists of collected studies were additionally reviewed.
Two authors independently reviewed titles and abstracts. Nonrelevant abstracts were used for citation exclusion. The authors independently performed full-text reviews. Differences in opinion were addressed through a second round of full-text reviews followed by input from remaining authors.
2.2. Eligibility
English-language studies of MAFs treated with a single superior miniplate or two miniplates were eligible. Inclusion required reporting third molar eruption (i.e.,, impacted, partially, or fully erupted; unerupted; or resolved) and retention or extraction during fixation. Clinical trials and observational studies were eligible. Outcomes of interest included post-operative infection, dehiscence, hardware failure, nonunion, malocclusion, reoperation, and minor complications (those managed without inpatient readmission). Bench studies and studies in non-human subjects, patients with prior tooth extraction, and comminuted or infected fractures were excluded.
2.3. Variables
Primary predictor variables for analysis were extraction management (extraction vs retention) of an either unerupted or partially erupted third molar. The primary outcome variable was incidence of total complication. Secondary outcome variables subdivided complications into major complications (defined as need for reoperation or readmission to the hospital) and minor complications. Complications were further broken down into mechanical, infectious, nonunion, and dehiscence subtypes.
2.4. Data Collection
A priori consensus for data extraction was reached during the study design phase after the hypothesis had been determined. Data were extracted for type of study, case demographics (patient age, gender, and medical comorbidities), MAF details (etiology, associated fractures, time to surgery, and third molars in the line of fracture), degree of third molar eruption (impacted, partially erupted, and unerupted/resolved), fixation method (Champy/single miniplate and two miniplates), and concomitant third molar extraction or retention, postoperative intermaxillary fixation, complications, and follow-up. Numerical data were extracted as counts and frequencies. One author extracted data into a preformed sheet which subsequently was verified by the second author. This process was unblinded to individual study authors and source.
2.5. Quality Assessment
Quality assessment was conducted via qualitative summary of study design, methodology, criteria for fracture inclusion/exclusion, patient covariates and treatment allocation, followup length, and patient attrition. These criteria were determined to be more appropriate than established instruments traditionally applied to randomized trials and investigations of intervention rather than epidemiology (i.e., Cochrane collaboration’s tool). Specifically, we evaluated for soundness of hypothesis as agreed upon by two authors, appropriateness of patients included, relevance of collected data to the hypothesis, soundness of statistical analysis, and if the data reported were granular enough for us to test our hypothesis.
2.6. Data Analysis
MAF cases were aggregated into two created groups: Group I, comprising unerupted and concomitantly extracted third molars and retained partially erupted third molars, and Group II, comprising impacted retained third molars and partially erupted and concomitantly extracted third molars. Count data for individual events of complication occurrence and nonoccurrence (i.e., complication-free surgical outcome) were collected in each group. Frequencies were determined from pooled event data to determine each group’s overall complication rates. Pooled counts of Group I were compared against that of Group II to generate weighted relative risks (RR) and 95% confidence interval (CI) for post-operative complication development. Where relative risks could not be generated, Χ2 analyses were performed, with a p-value of 0.05 set for significance. Analyses were performed using SPSS version 25 (IBM Corp, Armonk, NY, USA) and Excel (Microsoft, Redmond, WA, USA).
3. Results
3.1. Study Selection
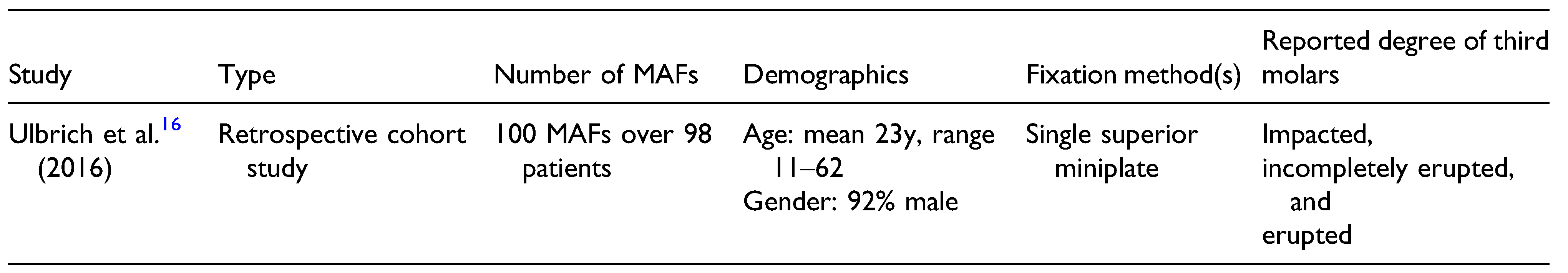
Citation screening and attrition are depicted in Figure 1. Ten studies were ultimately reviewed twice to determine final inclusion: four randomized trials [,,,] and six retrospective observation studies. [,,,,,] Four studies examined only isolated fractures [,,,] and one study examined bilateral MAFs. [] All studies reported single superior miniplate fixation via intraoral approach. Two studies also reported cases of two-miniplates fixation, [,] and three studies reported cases treated with a single 3D miniplate, [] single lateral miniplate (transbuccal), [] and strut plate. [] Three studies reported complications with respect to third molar eruption [,,] or concurrent extraction. [,,] Only Ulbrich et al.’s study stratified outcomes by both eruption and third molar extraction vs retention, meeting inclusion criteria; details are summarized in Table 1. [] Rationale for study exclusion is provided in Table 2.
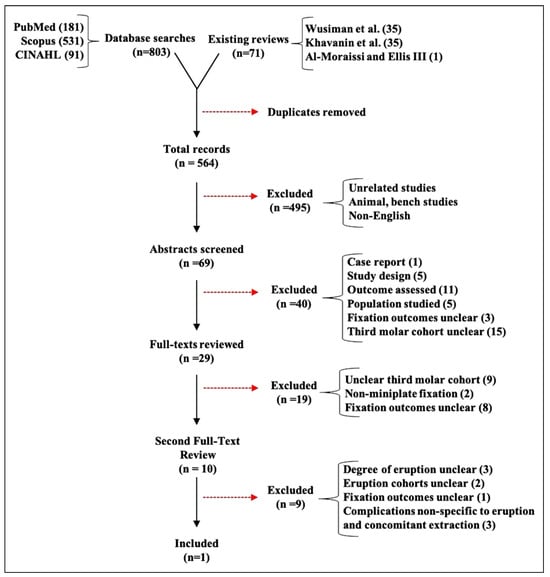
Figure 1.
PRISMA flowchart of records search, citation attrition, and selection for inclusion in this study.

Table 1.
Study Characteristics of the Included Study.

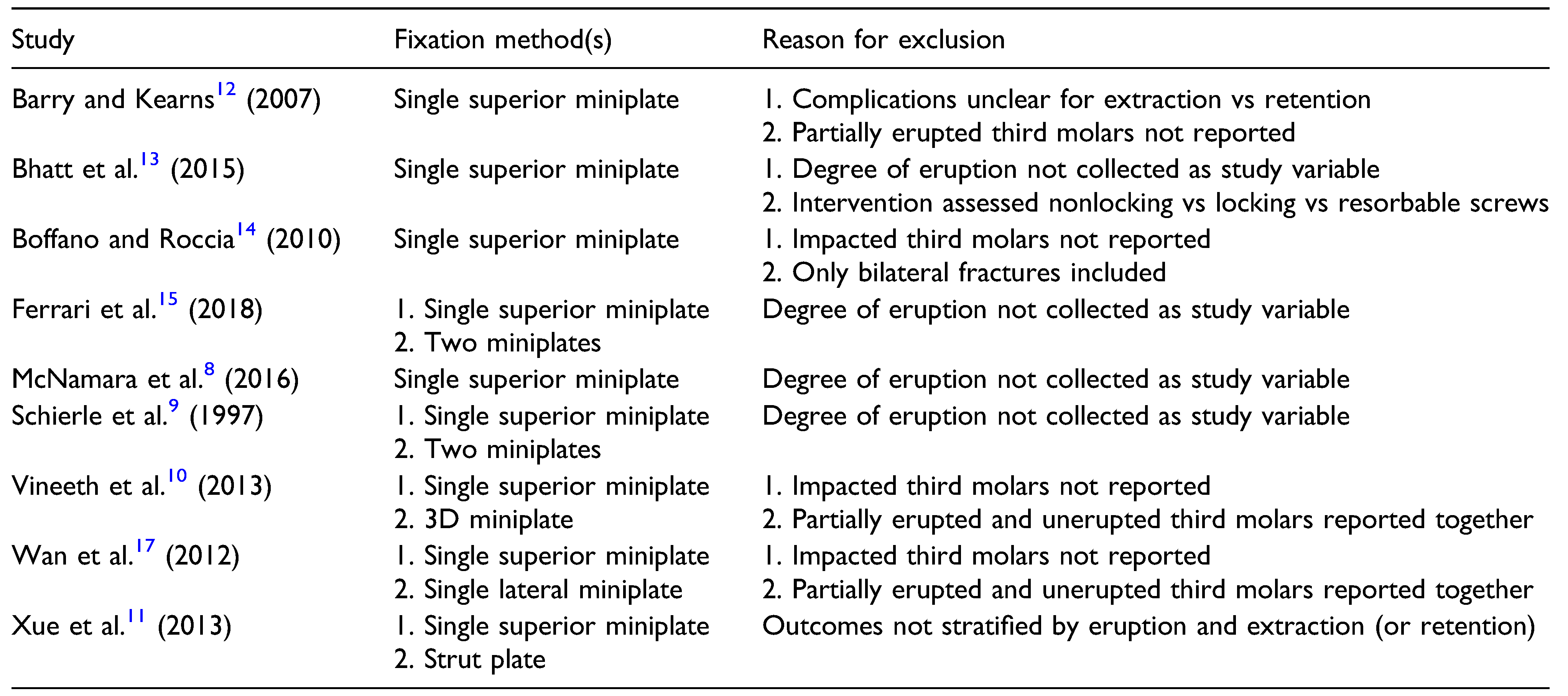
Table 2.
Studies Reviewed Twice for Inclusion Consideration With Reason(s) for Exclusion.
3.2. Characteristics of Included Studies
98 patients with MAFs involving 100 involved third molars were included. Mean age was 23 years (range 11–62), 91.8% of fractures were in men, 54% were assault-related, and 39% were isolated to the mandibular angle (72% of associated fractures were of the contralateral paramedian mandible). All MAFs were treated via Champy fixation at mean 1.4 days (range 0–12d.) after the inciting event, with concomitant extraction of loose, infected, and molars impeding adequate reduction. No post-operative intermaxillary fixation was used and all patients received periand post-operative antibiotics for mean 7.8 days (range 1–14d). Follow-up ranged at least 6 months and maximum 12 months.
Heterogeneity was of no concern given that only one study met all inclusion criteria. Nonconsecutive patient enrollment yielded medium risk of bias. Study design, methodology, operative technique and perioperative management, and results reporting were highly transparent.
3.3. Influence of Molar Eruption and Extraction on Complications
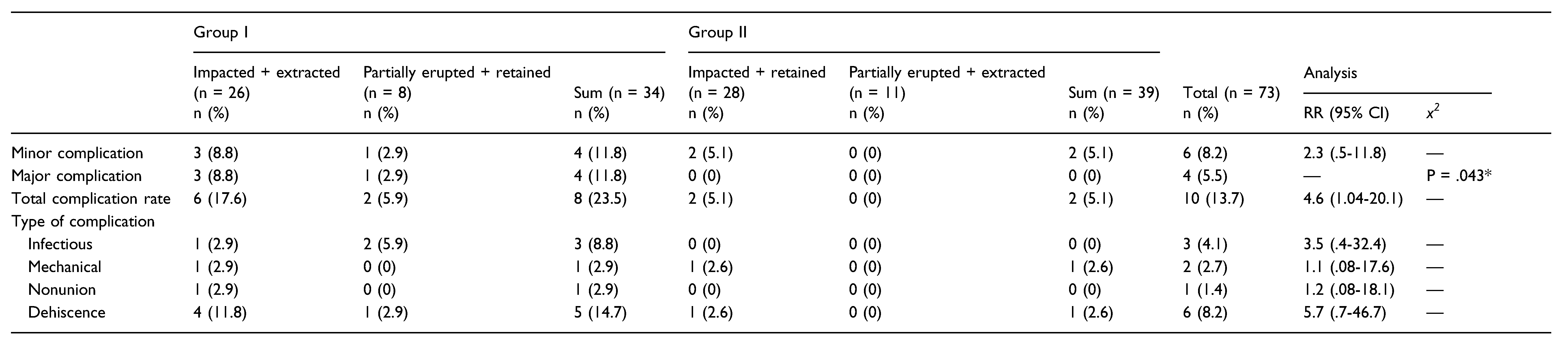
73 MAFs were analyzed to test our hypothesis: 27 of the 100 reported were fully erupted and so excluded from analysis. 34 and 39 MAFs qualified for Group I and II, respectively. Table 3 shows the rates of complications of each group, with relevant statistics. The pooled overall complication rate was 13.7%. Pooled rates of infectious complication were 4.1%, mechanical complication 2.7%, nonunion 1.4%, dehiscence 8.2%, reoperation 5.5%, and minor complications 8.2%. Infectious complications occurred in 8.8% in Group I and 2.5% in Group II (RR 3.5 [95% CI, 0.4–32.4]).

Table 3.
Complication Rates of High(Group I) and Low-Risk (Group II) Operative Management Groups. Values Given as Absolute Numbers and Percentages. Relative Risks (RR) Calculated When Possible. As no Major Complications Were Observed for Group II, RR was Non-Calculable; x2 Analysis was Performed Instead, with p-Value Set for Significance at <.05, Marked With an Asterisk.
Mechanical complications occurred in 2.9% in Group I and 2.6% in Group II (RR 1.1 [95% CI, 0.08–17.6]).
Nonunion occurred in 2.9% in Group I and 0% in Group II (RR 1.2 [95% CI, 0.08–18.1]). Dehiscence occurred in 14.7% in Group I and 2.6% in Group II (RR 5.7 [95% CI, 0.7–46.7]). Minor complications not requiring readmission occurred in 11.8% of Group I and 5.1% of Group II (RR 2.3 [95% CI, 0.5–11.8]). Reoperation was required in 5.5% of all cases and significantly differed between Groups I (11.8%) and II (0%) (P = 0.043 via Χ 2 analysis); as Group II had a 0% reoperation rate, a relative risk could not be calculated. The overall complication rate was 23.5% in Group I vs 5.1% in Group II (RR 4.6, 95% CI 1.04–20.1). Figure 2 lays out all computable RRs in a forest plot.
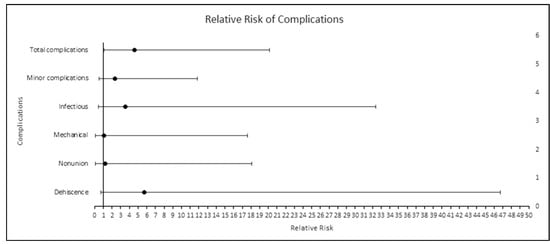
Figure 2.
Relative risk of calculable complications of Group I with comparison to Group II. 95% confidence intervals.
4. Discussion
We aimed to determine if extraction of unerupted third molars and retention of partially erupted third molars performed concurrent to Champy fixation confer greater postoperative complications. To determine situational appropriateness for employing Champy fixation, we collected high-risk cases involving extracted unerupted and retained partially erupted third molars and compared complication rates with a low-risk group of MAFs involving retained unerupted and extracted partially erupted third molars. High-risk cases experienced significantly more complications (23.5%) than their counterparts (5.1%), with extraction of impacted third molars and retention of partially erupted third molars conferring nearly five-fold greater postoperative complication risk (RR 4.6, 95% CI 1.04–20.1).
Similar to Bobrowski et al.’s one vs two miniplate metaanalysis, differences in specific complications did not meet statistical significance. []
For decades, molar extraction has remained ubiquitous in oromaxillofacial trauma literature, a testament to the importance of identifying the appropriate situations benefiting from extraction. Regardless of extraction or retention, wide ranges in subsequent complication morbidity further indicate the importance of defining situations benefiting from one vs the other. For instance, extracting unerupted third molars during fixation can yield notable bone loss secondary to the burring process and creation of a cortical window, whereas retaining partially erupted third molars can enable asymptomatic or undiagnosed pericoronitis to seed hardware, resulting in loosened fixation. [,,,] Both operative scenarios suggest two miniplate fixation, rather than Champy fixation, may be preferred due to superior biomechanical strength ability as proven in vitro. [,]
It behooves this study to compare complication rates with those of two miniplate fixation. While high-level evidence from Al-Moraissi and Ellis, Wusiman et al. and more have compared Champy vs two miniplate outcomes, and no studies of either fixation method have stratified reported complications by eruption and extraction. [,] To bridge this gap, and despite no studies currently providing results respective to both eruption and extraction, other studies’ outcomes were used as a historical comparison group against our findings. Meta-analyses from AlMoraissi and Ellis and Wusiman et al. both reported 37% reduced complication risk with Champy fixation compared to two miniplates (OR and RR 0.67). [,] These findings, when compared to our study’s 23.5% overall complication rate and calculated relative complication risk with high-risk third molars, suggest value in considering two miniplate fixation for certain MAF population segments. Such cases include presentations with absolute indications for unerupted third molar extraction (i.e.,, fractured tooth root) or MAFs involving partially erupted third molars. Involvement of partially erupted third molar should elicit careful assessment of symptom history and, because antibiotics have not been proven effective in treating acute or chronic pericoronitis, any findings consistent with pericoronitis history should indicate consideration of extraction. [,] If extraction results in loss of bone stock, treatment strategies should consider two miniplate fixation in addition to the Champy technique, which remains the preferred evidence-based fixation for most MAF cases.
Potential sources of bias in this review include small sample size, English-language bias, and database bias. Because extracted data originated from one nonrandomized observational study, bias related to patient and/or treatment allocation is possible. Because our focus was on cases (highand low-risk third molars) and outcomes (complications) that have not been previously reported, our observed positive associations require external validation by future studies to better assess our hypothesis. However, because the authors of the included study presented their methodology and data uniformly and completely for all cases and outcomes of our interest, data were able to be pooled and combined numerically to produce relative risks without detraction from missing values or need for assumption. Furthermore, because only one study met inclusion in our study, the wide variations in outcomes commonly affecting data synthesis ability of systematic reviews with multiple included studies is avoided, paradoxically enhancing reproducibility of our findings.
5. Conclusions
Contemporary evidence recommends Champy fixation as standard preference for isolated mandibular angle fracture treatment. However, in the context of extraction of unerupted third molars or retention of partially erupted third molars, Champy fixation may represent a previously unidentified higher risk for complicated outcomes, given this review’s findings of increased risk of post-operative complication in this subgroup. Prospective clinical trials are required to clarify differences in the efficacy of one vs two miniplate fixation for patients with high-risk third molar involvement in the line of fracture.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Ellis, E. Management of fractures through the angle of the mandible. Oral. Maxillofac. Surg. Clin. N. Am. 2009, 21, 163–174. [Google Scholar] [CrossRef]
- Ellis, E., 3rd. A prospective study of 3 treatment methods for isolated fractures of the mandibular angle. J. Oral. Maxillofac. Surg. 2010, 68, 2743–2754. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Ellis, E. What method for management of unilateral mandibular angle fractures has the lowest rate of postoperative complications? a systematic review and metaanalysis. J. Oral. Maxillofac. Surg. 2014, 72, 2197–2211. [Google Scholar] [CrossRef]
- Champy, M.; Lodde, J.P.; Schmitt, R.; Jaeger, J.H.; Muster, D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J. Maxillofac. Surg. 1978, 6, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Gerbino, G.; Tarello, F.; Fasolis, M.; De Gioanni, P.P. Rigid fixation with teeth in the line of mandibular fractures. Int. J. Oral. Maxillofac. Surg. 1997, 26, 182–186. [Google Scholar] [CrossRef]
- Khavanin, N.; Jazayeri, H.; Xu, T.; Pedreira, R.; Lopez, J.; Reddy, S.; Shamliyan, T.; Peacock, Z.S.; Dorafshar, A.H. Management of teeth in the line of mandibular angle fractures treated with open reduction and internal fixation: A systematic review and metaanalysis. Plast. Reconstr. Surg. 2019, 144, 1393–1402. [Google Scholar] [CrossRef] [PubMed]
- Wusiman, P.; Abasi, K.; Maimaitishawuti, D.; Moming, A. Management of mandibular angle fractures using one miniplate or two miniplate fixation system: A systematic review and meta-analysis. J. Oral. Maxillofac. Surg. 2019, 77, 1673.e1–1673.e11. [Google Scholar] [CrossRef]
- McNamara, Z.; Findlay, G.; O’Rourke, P.; Batstone, M. Removal versus retention of asymptomatic third molars in mandibular angle fractures: A randomized controlled trial. Int. J. Oral. Maxillofac. Surg. 2016, 45, 571–574. [Google Scholar] [CrossRef]
- Schierle, H.P.; Schmelzeisen, R.; Rahn, B.; Pytlik, C. Oneor two-plate fixation of mandibular angle fractures? J. CranioMaxillo-Facial Surg. 1997, 25, 162–168. [Google Scholar] [CrossRef]
- Vineeth, K.; Lalitha, R.M.; Prasad, K.; Ranganath, K.; Shwetha, V.; Singh, J. A comparative evaluation between single noncompression titanium miniplate and three dimensional titanium miniplate in treatment of mandibular angle fracture–A randomized prospective study. J. Craniomaxillofac. Surg. 2013, 41, 103–109. [Google Scholar] [CrossRef]
- Xue, A.S.; Koshy, J.C.; Wolfswinkel, E.M.; Weathers, W.M.; Marsack, K.P.; Hollier, L.H. A prospective study of strut versus miniplate for fractures of mandibular angle. Craniomaxillofac. Trauma. Reconstr. 2013, 6, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Barry, C.P.; Kearns, G.J. Superior border plating technique in the management of isolated mandibular angle fractures: A retrospective study of 50 consecutive patients. J. Oral. Maxillofac. Surg. 2007, 65, 1544–1549. [Google Scholar] [CrossRef]
- Bhatt, K.; Arya, S.; Bhutia, O.; Pandey, S.; Roychoudhury, A. Retrospective study of mandibular angle fractures treated with three different fixation systems. Natl. J. Maxillofac. Surg. 2015, 6, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Roccia, F. Bilateral mandibular angle fractures: Clinical considerations. J. Craniofac Surg. 2010, 21, 328–331. [Google Scholar] [CrossRef]
- Ferrari, R.; Lanzer, M.; Wiedemeier, D.; Rucker, M.; Bredell, M. Complication rate in mandibular angle fractures-one vs. two plates: A 12-year retrospective analysis. Oral. Maxillofac. Surg. 2018, 22, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Ulbrich, N.; Ettl, T.; Waiss, W.; Gosau, M.; Moralis, A.; Reichert, T.E.; Mueller, S. The influence of third molars in the line of mandibular angle fractures on wound and bone healing. Clin. Oral. Investig. 2016, 20, 1297–1302. [Google Scholar] [CrossRef]
- Wan, K.; Williamson, R.A.; Gebauer, D.; Hird, K. Open reduction and internal fixation of mandibular angle fractures: Does the transbuccal technique produce fewer complications after treatment than the transoral technique? J. Oral. Maxillofac. Surg. 2012, 70, 2620–2628. [Google Scholar] [CrossRef]
- Bobrowski, A.N.; Sonego, C.L.; Chagas, O.L. Postoperative infection associated with mandibular angle fracture treatment in the presence of teeth on the fracture line: A systematic review and meta-analysis. Int. J. Oral. Maxillofac. Surg. 2013, 42, 1041–1048. [Google Scholar] [CrossRef]
- Shetty, V.; Freymiller, E. Teeth in the line of fracture: A review. J. Oral. Maxillofac. Surg. 1989, 47, 1303–1306. [Google Scholar] [CrossRef]
- Neal, D.C.; Wagner, W.F.; Alpert, B. Morbidity associated with teeth in the line of mandibular fractures. J. Oral. Surg. 1978, 36, 859–862. [Google Scholar]
- de Amaratunga, N.A. The effect of teeth in the line of mandibular fractures on healing. J. Oral. Maxillofac. Surg. 1987, 45, 312–314. [Google Scholar] [CrossRef] [PubMed]
- Galvão, E.L.; da Silveira, E.M.; de Oliveira, E.S.; da Cruz, T.M.M.; Flecha, O.D.; Falci, S.G.M.; Gonçalves, P.F. Association between mandibular third molar position and the occurrence of pericoronitis: A systematic review and meta-analysis. Arch. Oral. Biol. 2019, 107, 104486. [Google Scholar] [CrossRef]
- Levy, F.E.; Smith, R.W.; Odland, R.M.; Marentette, L.J. Monocortical miniplate fixation of mandibular angle fractures. Arch. Otolaryngol. Neck Surg. 1991, 117, 149–154. [Google Scholar] [CrossRef]
- Choi, B.H.; Kim, K.N.; Kang, H.S. Clinical and in vitro evaluation of mandibular angle fracture fixation with the two-miniplate system. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 1995, 79, 692–695. [Google Scholar] [CrossRef] [PubMed]
- Curran, J.B. An assessment of the use of prophylactic antibiotics in third molar surgery. Int. J. Oral. Surg. 1974, 3, 1–6. [Google Scholar] [CrossRef]
- Pasupathy, S.; Alexander, M. Antibiotic prophylaxis in third molar surgery. J. Craniofac Surg. 2011, 22, 551–553. [Google Scholar] [CrossRef]
© 2021 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).