A Demographic Analysis of Craniomaxillofacial Trauma in the Era of COVID-19
Abstract
:Introduction
Materials and Methods
Results
Discussion
Funding
Authors’ Note
Ethical Approval
Conflicts of Interest
References
- van den Elzen, M.E.P.; Versnel, S.L.; Hovius, S.E.R.; Passchier, J.; Duivenvoorden, H.J.; Mathijssen, I.M.J. Adults with congenital or acquired facial disfigurement: impact of appearance on social functioning. J Craniomaxillofac Surg. 2012, 40, 777–782. [Google Scholar] [CrossRef] [PubMed]
- De Sousa, A. Psychological issues in acquired facial trauma. Indian J Plast Surg. 2010, 43, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Allareddy, V.; Allareddy, V.; Nalliah, R.P. Epidemiology of facial fracture injuries. J Oral Maxillofac Surg. 2011, 69, 2613–2618. [Google Scholar] [CrossRef]
- Jin, K.-S.; Lee, H.; Sohn, J.-B.; et al. Fracture patterns and causes in the craniofacial region: an 8-year review of 2076 patients. Maxillofac Plast Reconstr Surg. 2018, 40, 29. [Google Scholar] [CrossRef]
- Roden, K.S.; Tong, W.; Surrusco, M.; Shockley, W.W.; Van Aalst, J.A.; Hultman, C.S. Changing characteristics of facial fractures treated at a regional, level 1 trauma center, from 2005 to 2010: an assessment of patient demographics, referral patterns, etiology of injury, anatomic location, and clinical outcomes. Ann Plast Surg. 2012, 68, 461–466. [Google Scholar] [CrossRef]
- Chrcanovic, B.R. Factors influencing the incidence of maxillofacial fractures. Oral Maxillofac Surg. 2012, 16, 3–17. [Google Scholar] [CrossRef]
- Corfield, A.R.; MacKay, D.F.; Pell, J.P. Association between trauma and socioeconomic deprivation: a registry-based, Scotland-wide retrospective cohort study of 9,238 patients. Scand J Trauma Resusc Emerg Med. 2016, 24, 90. [Google Scholar] [CrossRef]
- Brattstro¨ m, O.; Eriksson, M.; Larsson, E.; Oldner, A. Socioeconomic status and co-morbidity as risk factors for trauma. Eur J Epidemiol. 2015, 30, 151–157. [Google Scholar] [CrossRef]
- Dalstra, J.A.A.; Kunst, A.E.; Borrell, C.; et al. Socioeconomic differences in the prevalence of common chronic diseases: an overview of eight European countries. Int J Epidemiol. 2005, 34, 316–326. [Google Scholar] [CrossRef]
- Shaw, K.M. Chronic disease disparities by county economic status and metropolitan classification, behavioral risk factor surveillance system, 2013. Prev Chronic Dis. [CrossRef]
- Banerjee, D.; Rai, M. Social isolation in Covid-19: the impact of loneliness. Int J Soc Psychiatry. 2020, 66, 525–527. [Google Scholar] [CrossRef]
- Balanzá-Martínez, V.; Kapczinski, F.; de Azevedo Cardoso, T.; et al. The assessment of lifestyle changes during the COVID-19 pandemic using a multidimensional scale. Rev Psiquiatr Salud Ment. 2021, 14, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.N.; Armitage, C.J.; Tampe, T.; Dienes, K. Public perceptions and experiences of social distancing and social isolation during the COVID-19 pandemic: a UK-based focus group study. BMJ Open. 2020, 10, e039334. [Google Scholar] [CrossRef] [PubMed]
- Noman, A.H.M.; Griffiths, M.D.; Pervin, S.; Ismail, M.N. The detrimental effects of the COVID-19 pandemic on domestic violence against women. J Psychiatr Res. 2021, 134, 111–112. [Google Scholar] [CrossRef] [PubMed]
- Viero, A.; Barbara, G.; Montisci, M.; Kustermann, K.; Cattaneo, C. Violence against women in the Covid-19 pandemic: A review of the literature and a call for shared strategies to tackle health and social emergencies. Forensic Sci Int. 2021, 319, 110650. [Google Scholar] [CrossRef]
- Northern Ohio Data and Information Service. Cleveland State University. Updated February, 2021. Available online: http://levin.urban.csuohio.edu/nodis/maps_thematic.html (accessed on 8 February 2021).
- IBM Corp. IBM SPSS Statistics; Version 27.0; IBM Corp, 2020. [Google Scholar]
- Microsoft Corp. Microsoft Excel; Microsoft Corp, 2018. [Google Scholar]
- Microsoft Corp. Microsoft Powerpoint; Microsoft Corp, 2018. [Google Scholar]
- Adobe Inc. Adobe Illustrator; Adobe Systems, 2019. [Google Scholar]
- Birkmeyer, J.D.; Barnato, A.; Birkmeyer, N.; Bessler, R.; Skinner, J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff. 2020, 39, 2010–2017. [Google Scholar] [CrossRef]
- Garrafa, E.; Levaggi, R.; Miniaci, R.; Paolillo, C. When fear backfires: emergency department accesses during the Covid-19 pandemic. Health Policy. 2020, 124, 1333–1339. [Google Scholar] [CrossRef]
- Wong, L.E.; Hawkins, J.E.; Langness, S.; Murrell, K.L.; Iris, P.; Sammann, A. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. In NEJM Catalyst Innovations in Care Delivery; Published online May 14, 2020. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0193 (accessed on 20 May 2021).
- Campedelli, G.M.; Aziani, A.; Favarin, S. Exploring the immediate effects of COVID-19 containment policies on crime: an empirical analysis of the short-term aftermath in Los Angeles. Am J Crim Just. 2020, 1–24. [Google Scholar] [CrossRef]
- Payne, J.L.; Morgan, A.; Piquero, A.R. COVID-19 and social distancing measures in Queensland, Australia, are associated with short-term decreases in recorded violent crime. J Exp Criminol 2020, 1–25. [Google Scholar] [CrossRef]
- Garude, K.; Natalwala, I.; Hughes, B.; West, C.; Bhat, W. Patterns of adult and paediatric hand trauma during the COVID-19 lockdown. J Plast Reconstr Aesthet Surg. 2020, 73, 1575–1592. [Google Scholar] [CrossRef]
- Bozkurt, A.; Jung, I.; Xiao, J.; et al. A global outlook to the interruption of education due to COVID-19 pandemic: navigating in a time of uncertainty and crisis. Asian Journal of Distance Education. 2020, 15, 1–126. [Google Scholar]
- Brodeur, A.; Cook, N.; Wright, T. On the effects of COVID-19 safer-at-home policies on social distancing, car crashes and pollution. Journal of Environmental Economics and Management. 2021, 106, 102427. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, L. The untold toll—the pandemic’s effects on patients without Covid-19. New England Journal of Medicine. 2020, 382, 2368–2371. [Google Scholar] [CrossRef] [PubMed]
- U.S. Census Bureau. QuickFacts: Cuyahoga County, OH; United States. Available online: https://www.census.gov/quickfacts/fact/table/cuyahogacountyohio,US/PST045219 (accessed on 20 May 2021).
| Total Cohort | Pre-Pandemic (2019) | Pandemic (2020) | ||
| n = 165 | n = 125 | n = 40 | Statistics | |
| Detail | 25th/50th/75th or No. (%) | Mean + SD or No. (%) | Mean + SD or No. (%) | P-value |
| Age | 28 y/45 y/67 y | 27 y/44 y/67 y | 33 y/51 y/84 y | 0.390 |
| Male | 116 (70.3%) | 89 (71.2%) | 27 (67.5%) | 0.656 |
| Caucasian | 95 (57.6%) | 67 (53.6%) | 28 (70.0%) | 0.068 |
| Married | 45 (27.3%) | 35 (28.0%) | 10 (25.0%) | 0.711 |
| Private Insurance | 64 (38.8%) | 47 (37.6%) | 17 (42.5%) | 0.580 |
| Unemployed | 36 (21.8%) | 27 (21.6%) | 9 (22.5%) | 0.905 |
| Psychiatric History | 29 (17.6%) | 23 (18.4%) | 6 (15.0%) | 0.623 |
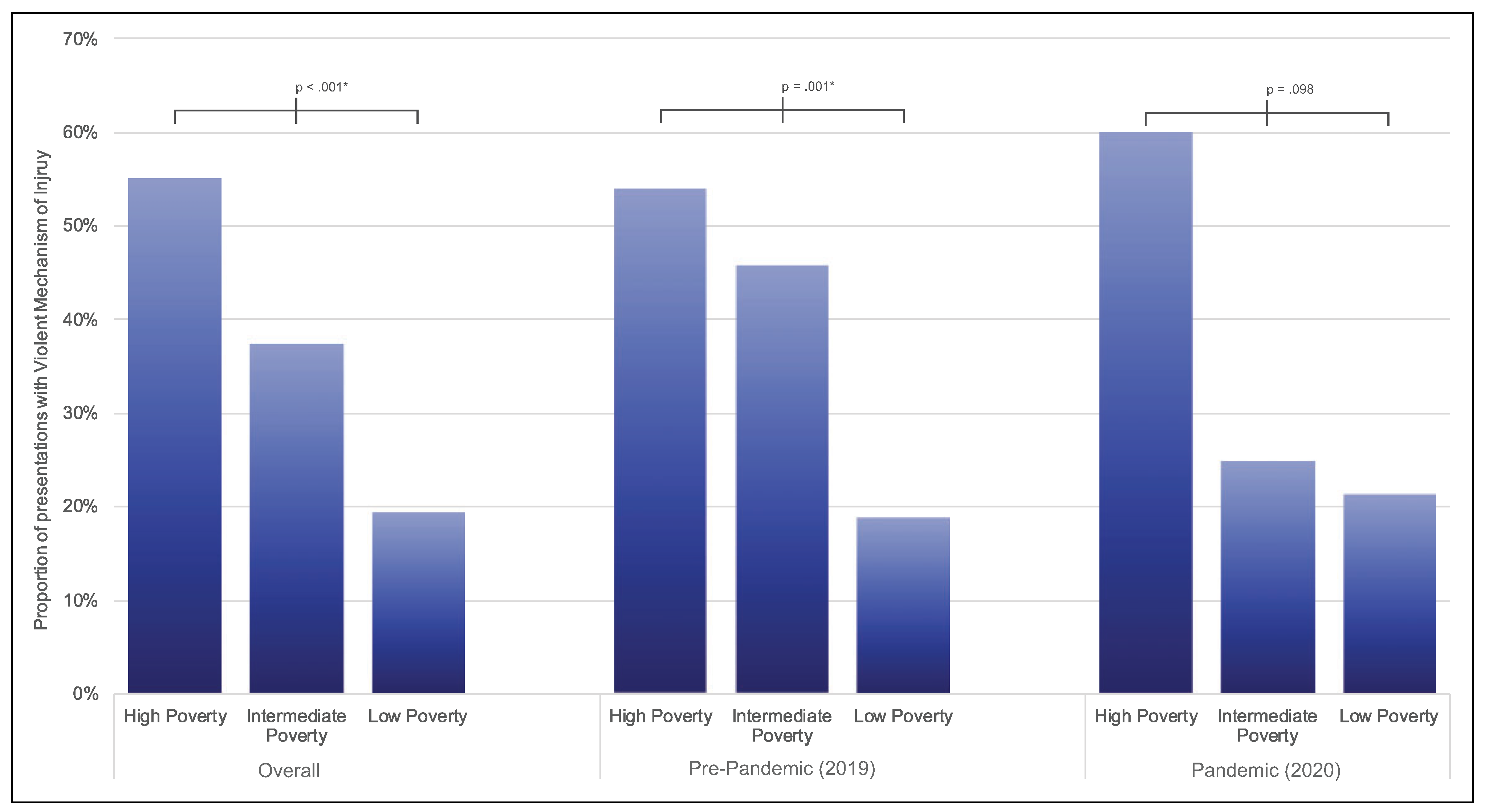
| ≤10% Poverty | 62 (38.3%) | 48 (39.3%) | 14 (35.0%) | 0.026* |
| 10.1-25% Poverty | 40 (24.7%) | 24 (19.7%) | 16 (40.0%) | |
| >25% Poverty | 60 (37.0%) | 50 (41.0%) | 10 (25.0%) |
| Total | Pre-Pandemic (2019) | Pandemic (2020) | ||
| Cohort n = 165 | n = 125 | n = 40 | Statistics | |
| Detail | 25th/50th/75th or No. (%) | 25th/50th/75th or No. (%) | 25th/50th/75th or No. (%) | P-value |
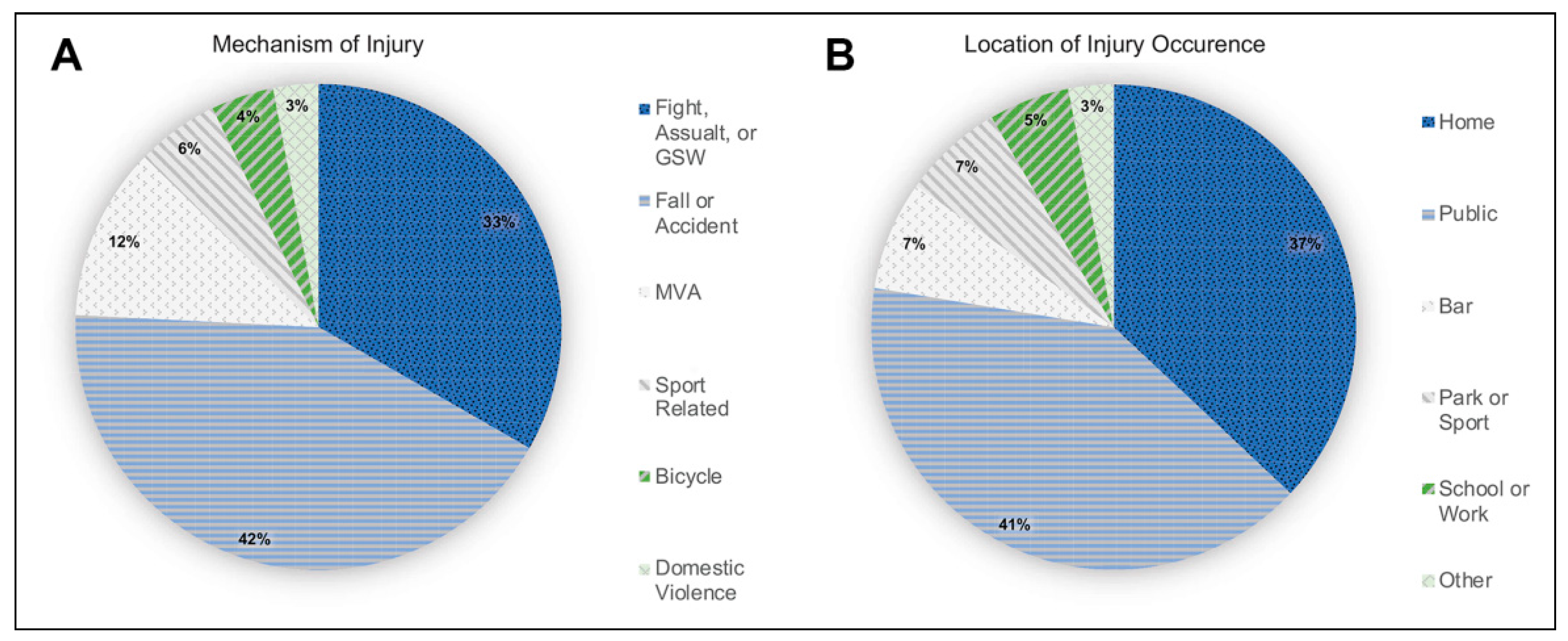
| Injury at Home | 62 (37.6%) | 43 (34.4%) | 19 (47.5%) | 0.136 |
| Intoxication | 45 (27.3%) | 38 (30.4%) | 7 (17.5%) | 0.111 |
| Violent MOI | 60 (36.4%) | 47 (37.6%) | 13 (32.5%) | 0.559 |
| Isolated Fracture | 73 (44.2%) | 58 (46.4%) | 15 (37.5%) | 0.324 |
| Isolated Injury | 105 (63.6%) | 73 (58.4%) | 32 (80.0%) | 0.013* |
| Hospital Admission | 77 (46.7%) | 56 (44.8%) | 21 (52.5%) | 0.396 |
| Surgical Intervention | 28 (17.0%) | 18 (14.4%) | 10 (25.0%) | 0.120 |
| Time to Operation | 1 d/7 d/11 d | 1 d/5 d/10 d | 6 d/9 d/12 d | 0.109 |
© 2021 by the author. The Author(s) 2021.
Share and Cite
Clark, R.C.; Desai, B.; Davidson, E.H. A Demographic Analysis of Craniomaxillofacial Trauma in the Era of COVID-19. Craniomaxillofac. Trauma Reconstr. 2022, 15, 288-294. https://doi.org/10.1177/19433875211047037
Clark RC, Desai B, Davidson EH. A Demographic Analysis of Craniomaxillofacial Trauma in the Era of COVID-19. Craniomaxillofacial Trauma & Reconstruction. 2022; 15(4):288-294. https://doi.org/10.1177/19433875211047037
Chicago/Turabian StyleClark, Robert C., Bijal Desai, and Edward H. Davidson. 2022. "A Demographic Analysis of Craniomaxillofacial Trauma in the Era of COVID-19" Craniomaxillofacial Trauma & Reconstruction 15, no. 4: 288-294. https://doi.org/10.1177/19433875211047037
APA StyleClark, R. C., Desai, B., & Davidson, E. H. (2022). A Demographic Analysis of Craniomaxillofacial Trauma in the Era of COVID-19. Craniomaxillofacial Trauma & Reconstruction, 15(4), 288-294. https://doi.org/10.1177/19433875211047037




