Abstract
Study Design: Retrospective cross-sectional study. Objective: The objective of this retrospective study was to evaluate the clinical outcomes of Modified temporal incision in the management of zygomatic arch fractures (ZAF). Patients and Methods: Records of 34 patients who underwent open reduction for zygomatic arch fractures were retrieved and included in the study between 2011 and 2018. These patients were followed up at 4 weeks, 8 weeks and 12 weeks respectively. Clinical parameters such as post-operative infection, hematoma, scarring, degree of mouth opening, palpability of plates, alopecia and weakness of temporal branch of Facial nerve recorded were analyzed for complications of modified temporal incision in the management of ZAF. Results: A thorough analysis of the clinical parameters revealed that at the end of 4 weeks scarring was present in 4 patients and temporal branch of Facial nerve weakness was present in 21 patients. None of the patients had hematoma, infection or palpability of miniplates. At the end of 8 weeks the only complication recorded was weakness of temporal branch of Facial nerve in 21 patients. By 12 weeks, all patients had complete recovery and none of the patient had weakness of temporal branch of Facial nerve. Conclusion: The results obtained proved that the Modified temporal incision can be considered as a reliable method in the management of zygomatic arch fractures. The incision can be adopted with confidence in suitable cases of zygomatic arch fractures without any permanent morbidity.
Introduction
Zygomatic bone of the maxillofacial skeleton gives the lat- eral projection to the human face. Fracture of zygomatic arch leads to both cosmetic and functional deformity. It also increases the width of the face. Zygomatic arch fractures (ZAF) can be considered as one of the commonest fractures amenable for closed reduction techniques if they were mini- mally displaced. On contrary, it demands a good surgical expertise to perform Open reduction and internal fixation (ORIF) in a highly displaced and malunited fractures.
Various incisions such as hemi-coronal, coronal, preauri- cular and temporal incisions were widely used, subjected to their own advantages and disadvantages. At our institute, we used Modified temporal incision to expose, reduce and fix suitable cases of zygomatic arch fractures (in these 34 patients). A retrospective study was conducted to analyze the clinical outcomes of Modified temporal incision in the ORIF of ZAF.
Exclusion Criteria
- Zygomaticarch treated by closed reduction under LA.
- Zygomatic arch fracture with cranial bone fracture associated with neurological defi-cits.
- Bilateral zygomatic arch fractures treated with ORIF.
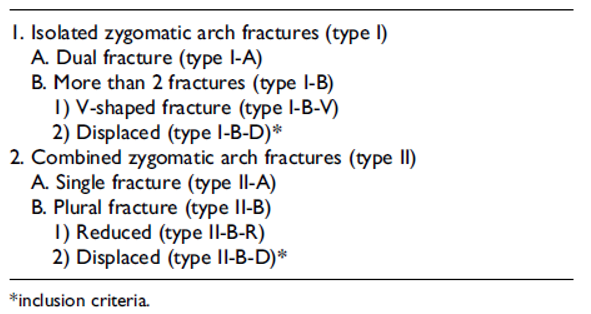
- Ozyazgan’s classification.
Type I A
I-B-V
Type II A
II-B-R.
Patients were analyzed for clinical parameters such as post-operative infection, hematoma, scarring, degree of mouth opening, palpability of plates, alopecia and weakness of temporal branch of Facial nerve. They were analyzed at
Materials and Methods
The study was carried out for the period of 7 years (2011–2018) at the Department of Dentistry, IGMC&RI after getting ethical committee clearance (IEC no: 17/ 163/IEC/PP/2018). In-patient records, follow up records, CT scans(pre- and post-operative), radiographs(pre- and post-operative) and photographs(pre- and post-operative) of the patients who underwent ORIF for ZAF were retrieved and analyzed for clinical outcomes of Modified temporal incision in the management of ZAF
Inclusion Criteria
- ZAF treated between 2 days and 60 days of the injury which included malunited or non-united frac- tures with trismus.
- Ozyazgan’s classification was followed to classify ZAF and associated ZMC fractures (Table 1).
 Table 1. O¨ zyazgan et al. Classification of Zygomatic Arch Fractures. J Oral MaxillofacSurg 2007.[1].
Table 1. O¨ zyazgan et al. Classification of Zygomatic Arch Fractures. J Oral MaxillofacSurg 2007.[1].
The 2 categories indicated for open reduction were (Ozyaz- gan’s criteria)
- -
- Type-I-B(D).
- -
- Type-II-B(D).
The above 2 categories along with
- -
- bilateral or unilateral Lefort I, II and III fractures.
- -
- bilateral or unilateral mandibular fractures.
Hematoma is defined as a pool of clotted or partially clotted blood in an organ, tissue or body space usually caused by a broken blood vessel.
An ideal scar is defined as a linear imperceptible line, not pigmented, not raised and no distortion to adjacent structures.[2,3] The width of the linear scar > 3 mm in the entire length of the incision was recorded as presence of scar in our study.
Palpability of miniplates was recorded depending on the patient’s feedback on the realization of the presence of miniplates during routine daily activities.
The maximum width of alopecia in the entire length of incision was recorded in mm. The width of the alopecia >3 mm in the entire length of the incision was recorded as presence of alopecia in our study.
The grading of Facial nerve function according to House Brackmann scale[4] was applied for the assessment of tem- poral nerve weakness after surgery.
The recovery of Facial nerve without medical or surgical management following the surgery were explained based on Seddon[5] and Sunderland[6] classification. Seddon and Sunderland classification is based on the patho physiologic events following nerve injury and it is correlated with the post-operative recovery.
Results
All patients who underwent the procedure were males (N ¼ 34).
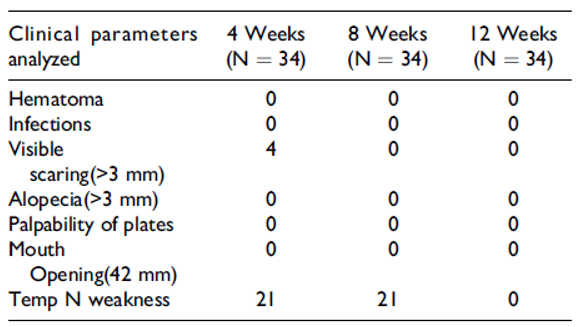
Four patients had visible scarring of >3 mm at the end of 4 weeks. None of the patients had a wider scar of >3 mm in the entire length after 12 weeks. Scar formed was linear, imperceptible, not pigmented, not raised and no distortion to adjacent structures was recorded at 12 weeks (Table 2). 62% of patients’ experienced temporary weakness of Facial nerve. The grading of Facial nerve function according to House Brackmann scale[4] was applied for the assessment of temporal nerve weakness after surgery (Table 3). The tem- poral nerve weakness was in Grade IV in 21 patients (N ¼ 34) at the end of 4 weeks. At the end of 8 weeks the nerve function improved and progressed to Grade III in 12 patients and grade II in 9 patients (N ¼ 34). In 12 weeks, there was a complete recovery of nerve function and it was in Grade I.

Table 2.
Assessment of Clinical Parameters After Surgery.

Table 3.
Assessment of Facial N Function According to House Brackmann Scale.[4].
The recovery of nerve function (Seddon and Sunderland classification) was complete and without synkinesis in 3 months. The iatrogenic nerve injury can be correlated for grade I(neurapraxia-conduction blockage due to compres- sion or demyelination and no damage to axon or nerve sheath) and grade II(axonal degeneration due to compres- sion with intact perineurium, endoneurium and epineurium). The maximum width of alopecia in the entire length of incision was recorded in mm (Table 2). In our study the maximum width of alopecia recorded was less than 3 mm in all patients (we used cold steel scalpel). Patients had no complaints about alopecia, as alopecia was well hidden in the hairline
Mouth opening (more than or equal to 42 mm) was attained and maintained after 1 week of the surgery even in cases of malunion with complete trismus (Table 2).
None of the patients had hematoma, infection, restric- tion in mouth opening or complaints about palpability of mini plates during routine daily activities (Table 2).
All patients were satisfied with the aesthetic outcome of the procedure. Patients had no complaints about scar in the temporal region nor alopecia in the incision line. Further none of the patients had complaints about temporal nerve weakness in spite of repeated clinical testing during follow up.
Surgical Procedure
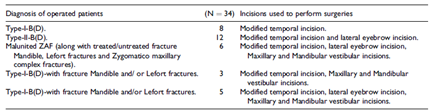
Surgery was done under general anesthesia following strict aseptic precautions. Appropriate incisions were made depending on the type of ZAF and associated fractures (Table 4) (Figure 1, Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7, Figure 8, Figure 9, Figure 10, Figure 11, Figure 12, Figure 13, Figure 14, Figure 15, Figure 16, Figure 17, Figure 18, Figure 19, Figure 20, Figure 21 and Figure 22). Primarily, the branches of the superficial temporal artery were marked. The incision was placed below the superficial temporal artery and 1 cm above the zygomatic arch. The length of the incision was decided upon the position of the anterior most part of ZAF to be fixed. The length of the incision advocated was 5 mm to 6.5 cm. In patients with anterior ZAF an incision length of 6.5 cm was utilized. Care was taken to have the incision marked 1 cm above the zygomatic arch to protect the temporal branch of facial nerve, the location of temporal branch of Facial nerve was far more anterior to the incision. The incision was carried out into skin and the superficial fascia. A blunt dissection was done to identify temporalis fascia and muscle. The temporal branch of facial nerve runs lateral to the temporalis fascia. The fascia was elevated along with the nerve which protects the temporal branch of facial nerve. Further, the zygomatic arch was reached by blunt dissection. No electro surgical pencil was used for nerve testing during the procedure. An incision was made in the superior border of zygomatic arch to expose to ZAF. A Rowe’s zygomatic elevator was used to reduce the bony fragments and to regain the projection of the face. 1.5 mm titanium miniplates (6hole or 4hole) was fixed with 1.5 mm × 6 mm titanium screws appropriately. Wound was closed in layers with 3/0 vicryl and 3/0 silk/ 3/o prolene.

Table 4.
Incisions Used to Perform Surgeries.
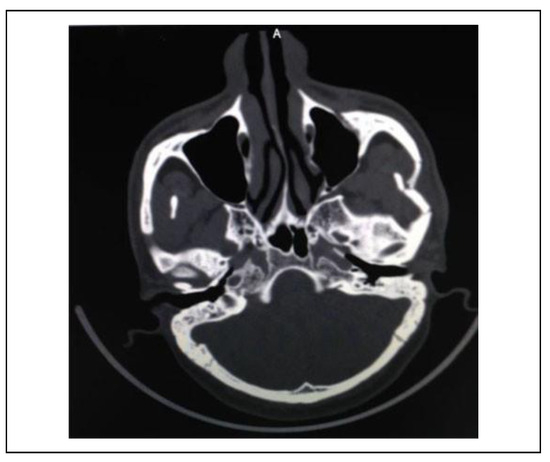
Figure 1.
Pre-operative CT-scan

Figure 2.
Incision marking.

Figure 3.
Layerwise dissection.

Figure 4.
Fracture site exposed.

Figure 5.
Fixation with miniplates.

Figure 6.
Fixation of frontozygomatic region—Type II-B-D.

Figure 7.
Subcuticular suturing.

Figure 8.
Post-operative—4 weeks (temporal nerve weakness).

Figure 9.
Post-operative—12 weeks (temporal nerve weakness resolved).
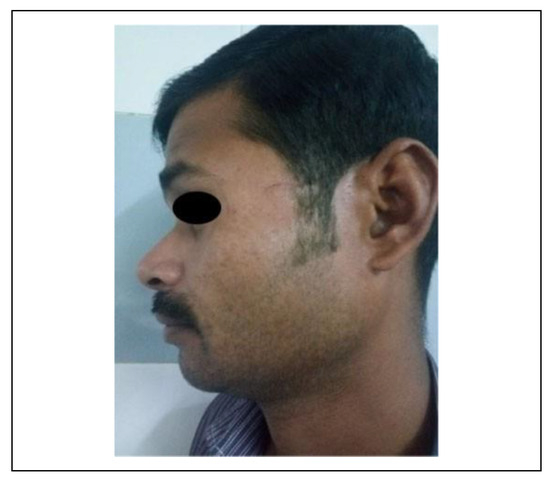
Figure 10.
Scar at 12 weeks.
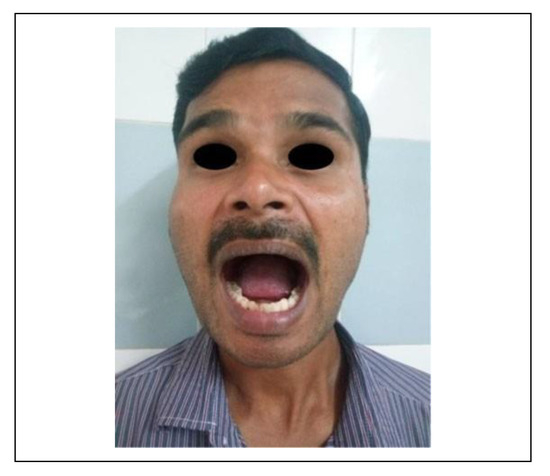
Figure 11.
Mouth opening at 12 weeks.
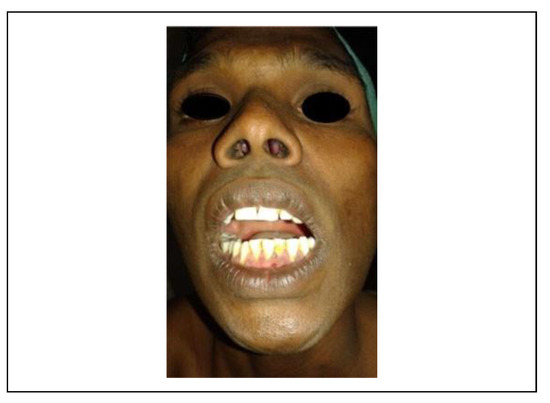
Figure 12.
Pre-operative mouth opening.

Figure 13.
Malunited ZAF and ZMC fracture—2 months old.

Figure 14.
Zygomatic arch and superficial (temporal artery marking).

Figure 15.
Exposure of temporalis fascia.
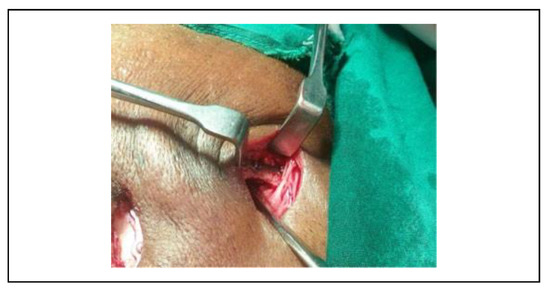
Figure 16.
Miniplate fixation over the zygomatic arch.

Figure 17.
Post-operative scar (4 weeks).
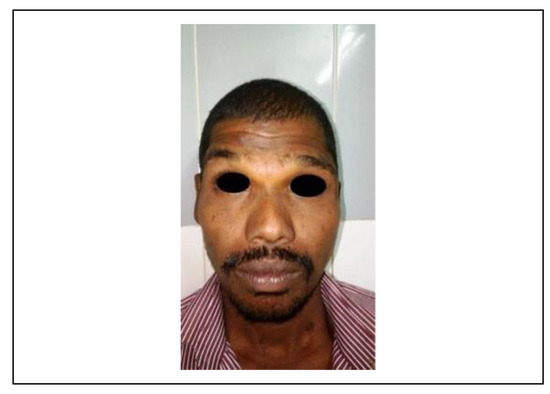
Figure 18.
Post-operative—4 weeks (temporal nerve weakness).

Figure 19.
Post-operative—7 yrs (temporal nerve weaknessresolved).Figure 20. Post-operative SMV view—7 yrs.
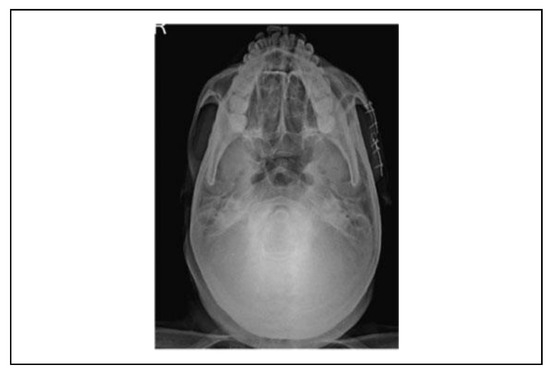
Figure 20.
Post-operative SMV view—7 yrs.
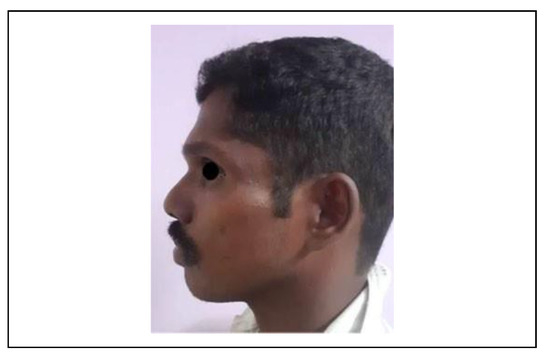
Figure 21.
Post-operative scar—7 yrs.

Figure 22.
Post-operative mouth opening—7 yrs.
Discussion
Zygomatic arch is a horizontal bar of bone. Its anterior two-third is formed by the temporal process of zygomatic bone and posterior one-third is formed by zygomatic pro- cess of temporal bone. This thin bar of bone adds to the lateral projection of the face.
ZAF’s are preferred to be managed by array of closed reduction techniques[7,8] like Gillie’s temporal approach, Keen’s intra-oral approach and percutaneous J-hook.[9,10] The arch gets naturally splinted due to periosteal continuity.
The attachment of temporal fascia aids in stabilization of mildly displaced ZAF.[11] In cases of undisplaced ZAF com- bined with other mid face fractures, closed anatomical reduction of ZAF along with ORIF of other midface frac- tures was advocated.[12,13] Open reduction of displaced ZAF becomes mandatory when the projection of the face is lost.[13]
Proper stabilization of combined fractures in three- dimensional plane aids in stabilization of undisplaced ZAF.[14] Turk et al[15] claims that more than 1500 cases of ZAF were amenable to closed reduction, if the zygomatic com- ponent is fixed. Closed reduction techniques are always the preferred method as it does not leave any visible scar and it does not risk the temporal branch of Facial nerve.
Reinforcement of these closed reduction were done by external and internal splints like K wire, finger splints, percutaneous stenting,[16] malleable aluminum stent,[17] Foley’s catheter etc.[18,19,20,21] with debatable success.
In cases of a displaced zygomatic arch the natural splint- ing mechanism by masseter and temporalis fascia is lost and they may not be amenable for closed reduction. Thus, management of ZAF becomes complicated if they are unstable or malunited. Perfection in restoration of ZAF is important in the management of midface fractures and Zygoma fractures.[22] Adequate and effective management of ZAF is absolutely important due to the risk of ankylosis with Coronoid process of the mandible.
One another technique used in the management of ZAF is endoscopy-assisted bone reduction.[23] Endoscopic reduction method was employed in the management of comminuted ZAF too.
The treatment plan for ZAF whether isolated or com- bined depends on the following factors: the displacement of bone fragments, fractures unstable after closed reduction and if the fractures were malunited.
Ozyazgan et al[1] advised surgical intervention for Type-I-B(D) and Type-II-B(D).Open reduction of ZAF were routinely done by coronal, hemi-coronal, preauricular, mod- ified preauricular, anterior temporal hairline incision[24] and modified temporal incision.[25]
Coronal incisions are routinely used for open reduction of ZAF. They have a definite role in the management of ZAF if they are associated with pan facial fractures com- prising of supraorbital rim, frontal bone, lateral orbital rim, zygomatic bone and the arch. Furthermore, the coronal incision has its own complications recorded in the literature worldwide. These include hematoma, infection, hyper- trophic scar, alopecia, temporal hollowing and weakness of temporal branch of facial nerve.[26] Coronal incision is time tested and it is widely used in the management of pan facial fractures, Lefort II and Lefort III osteotomies since 1970.[27] The actual time taken for reaching the surgical site by coronal incision ranges from 25 min to 40 min.[28] The fracture exposure, visibility and ease of surgery with coronal incision are considered excellent. Localized alope- cia recorded following bicoronal incision with use of cold steel scalpel (in both skin and subcutaneous tissue) was 2.8 mm to 3.5 mm.[29]
Gabrielli et al[30] studied alopecia after bicoronal incision and recorded alopecia on 18 percent of patients (maximal width of alopecia being 1 cm).
However, maxillofacial surgeons who studied the inci- sion recommend judicious use of coronal incision with a caution that it should not be overused for simple situations.
Moreover, Modified temporal incision can be adopted with confidence as coronal incision also does not spare temporal nerve.
Massarelli et al[31] used pretrichial incision in the manage- ment of maxillofacial fractures. The incision was originally used in the foreheadplasty and brow lift surgeries. He inferred that the zig zag pretrichial incision provides excellent exposure and reported no wide scars or alopecia. Thus, a search for an ideal incision for the management of ZAF which provides maximum exposure, minimum morbidity to the temporal branch of facial nerve and good cosmetic results was of prime importance in the evolution of maxillofacial surgery.
Modified temporal incision takes 10 to 15 minutes for the fracture exposure. The length of the incision can be reduced if the fracture site is located in the posterior one-third of the arch. The results of the present study clearly indicate that the complications like hematoma infection, temporal hollowing, alopecia and visible scarring were negligible with modified temporal incision. The scar formed was partially hidden in the hairline and the exposed part was well accepted by the patients. It almost gives an imperceptible scar. With respect to exposure of fracture site, incision gives adequate exposure to ZAF. The expo- sure is better with posterior one-third of ZAF. Anterior two-third of ZAF demands more retraction and slightly longer incision.
The only recorded complication of this incision from our study is weakness of temporal branch of Facial nerve. How- ever, it was found to be a purely temporary complication. Complete recovery of the nerve weakness was observed in 3 months. The recovery of temporal N weakness had occurred without any intervention like physiotherapy or usage of sup- plements. The recovery of Facial nerve without medical or surgical management following the surgery can be explained based on Seddon and Sunderland classification. Seddon and Sunderland classification is based on the patho physiologic events following nerve injury and it is correlated with the post-operative recovery.
The recovery of nerve function was complete and with- out synkinesis in 3 months. The iatrogenic nerve injury can be correlated for grade I(neurapraxia-conduction blockage due to compression or demyelination and no damage to axon or nerve sheath) and grade II(axonal degeneration due to compression with intact perineurium, endoneurium and epineurium). In Grade I and Grade II injury complete recovery occurs over several weeks to months without any intervention.[32] The temporal nerve weakness can be clini- cally attributed to the traction applied during fixation of fractures in the anterior one-third of the zygomatic arch.
In our study we noted that the patients who had fractures in the anterior two-thirds of arch demanded retraction and all these patients had temporary temporal nerve weakness. The weakness of temporal branch of Facial nerve was found to be temporary in the study by Yang et al.[24] He employed an anterior temporal hairline incision. In this study he used vertical incision in the temporal region followed by horizontal incision to release the periosteum in the zygomatic arch. It was reported that the neurapraxia of temporal nerve resolved completely in 6 months.
Conclusion
The modified temporal incision proved to be a promising technique with advantages of minimal incision and ade- quate exposure. The only complication is paresthesia of temporal Branch of Facial nerve, which resolved in 3 months. Further the reason for the temporary nerve weak- ness observed in our study was due to surgical traction during fixation of more anterior fractures. Hence modified temporal incision is not an ideal choice for anterior zygo- matic arch fractures. A comparative study with coronal incision to prove the efficiency of the Modified temporal incision in terms of less operating time, temporary weak- ness of Facial N, minimal scar formation and considerably less alopecia is highly recommended.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Ozyazgan I, Gu¨nay GK, Eskitas¸c¸ioglu T, Ozko¨se M, Coruh A. A new proposal of classification of zygomatic arch fractures. J Oral Maxillofac Surg. 2007, 65, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Watson D, Reuther MS. Scar revision techniques-pearls and pitfalls. Facial Plast Surg. 2012, 28, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Rudolph R, Schneider G. Scar revision. In: Georgiade GS, Riefkohl R, Levin LS eds. Plastic Maxillofacial and Recon- structive Surgery, 8: Williams and Wilkins; 1997, 1997.
- House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985, 93, 146–147. [Google Scholar] [CrossRef]
- Seddon, HJ. Surgical Disorders of the Peripheral Nerves. Churchill Livingstone; 1972.
- Sunderland, S. Nerves and Nerve Injuries. 2nd ed. Churchill Livingstone; 1978. 780-795.
- Werner JA, Frenkler JE, Lippert BM, Folz BJ. Isolated zygomatic arch fracture: report on a modified surgical technique. Plast Reconstr Surg. 2002, 109, 1085–1089. [Google Scholar] [CrossRef] [PubMed]
- Gupta A, Lehl G. Minimal access percutaneous approach for the management of zygomatic arch fractures. Int J Oral Maxillofac Surg, 8: 46.
- Zingg M, Laedrach K, Chen J, et al. Classification and treat- ment of zygomatic fractures—a review of 1,025 cases. J Oral Maxillofac Surg. 1992, 50, 778–790. [Google Scholar] [CrossRef]
- Zingg M, Chowdhury K, Ladrach K, Vuillemin T, Sutter F, Raveh J. Treatment of 813 zygoma-lateral orbital complex fractures—new aspects. Arch Otolaryngol Head Neck Surg. 1991, 117, 611–620. [Google Scholar] [CrossRef]
- Banks, P. Killey’s Fracture of the Middle Third of the Facial Skeleton. 5th ed. Varghese Publishing House; 1992.
- Hollier LH, Thornton J, Pazmino P, Stal S. The management of orbito zygomatic fractures. Plast Reconstr Surg. 2003, 111, 2386–2392. [Google Scholar] [CrossRef]
- Gruss JS, Van Wyck L, Phillips JH, Antonyshyn O. The Importance of the zygomatic arch in complex midfacial fracture repair and correction of posttraumatic orbitozygo- matic deformities. Plast Reconstr Surg. 1990, 85, 878–890. [Google Scholar] [CrossRef]
- Gruss JS, Phillips JH. Complex facial trauma: the evolving role of rigid fixation and immediate bone graft reconstruc- tion. Clin Plast Surg. 1989, 16, 93–104. [Google Scholar] [CrossRef]
- Turk JB, Ladrach K, Raveh J. Repair of zygomatico malar complex fractures. The Swiss method. Arch Facial Plast Surg. 1999, 1, 123–126. [Google Scholar] [CrossRef]
- Rohrich RJ, Hollier LH, Watumull D. Optimizing the man- agement of orbito zygomatic fractures. Clin Plast Surg. 1992, 19, 149–165. [Google Scholar] [CrossRef]
- Shah P, Mirza T, Simpson M. The unstable fractured zygomatic arch—simple solutions for a difficult situation. Br J Oral Maxillofac Surg. 2016, 54, 115. [Google Scholar] [CrossRef]
- Guven, O. Stabilisation of the delayed zygomatic arch fracture. Int J Oral Maxillofac Surg. 1987, 16, 445–447. [Google Scholar] [CrossRef]
- Lew DH, Park BY, Lee HB, Lew JD. Simple fixation method for unstable zygomatic arch fracture using double Kirschner’ wires. Plast Reconstr Surg. 1998, 101, 1351–1354. [Google Scholar]
- Randall DA, Bernstein PE. Epistaxis balloon catheter stabilization of zygomatic arch fractures. Ann Otol Rhinol Laryngol. 1996, 105, 68–69. [Google Scholar] [CrossRef] [PubMed]
- Uglesic V, Virag M. A method of zygomatic arch stabilization. Br J Oral Maxillofac Surg. 1994, 32, 396–397. [Google Scholar] [CrossRef]
- Stanley, RB. The zygomatic arch as a guide to reconstruction of comminuted malar fractures. Arch Otolaryngol Head Neck Surg. 1989, 115, 1459–1462. [Google Scholar] [CrossRef]
- Chen CT, Lai JP, Chen YR, Tung TC, Chen ZC, Rohrich RJ. Application of endoscope in zygomatic fracture repair. Br J Plast Surg. 2000, 53, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Yang QF, Wang F, Ying K, Li JP, Xu MD. Application of temporal anterior hairline incision in internal fixation of zygomatic complex fracture [in Chinese]. Shanghai Kou Qiang Yi Xue. 2005, 14, 113–116. [Google Scholar]
- Prakasam M, Dolas RS, Managutti A, Deepashri K. A modified temporal incision: an alternative approach to the zygomatic arch. J Maxillofac Oral Surg. 2010, 9, 428–433. [Google Scholar] [CrossRef]
- Kerawala CJ, Grime RJ, Stassen LF, Perry M. The bicoronal flap (craniofacial access): an audit of morbidity and a proposed surgical modification in male pattern baldness. Br J Oral Maxillofac Surg. 2000, 38, 441–444. [Google Scholar] [CrossRef] [PubMed]
- Marschall MA, Cohen M, Garcia J, Schafer ME. Craniofacial approach for the reconstruction of severe facial injuries. J Oral Maxillofac Surg, 3: 46.
- Kumar VS, Rao NK, Mohan KR, et al. Minimizing complica- tions associated with coronal approach by application of var- ious modifications in surgical technique for treating facial trauma: a prospective study. Natl J Maxillofac Surg. 2016, 7, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Kadakia S, Badhey A, Ashai S, Lee TS, Ducic Y. Alopecia following bicoronal incisions. JAMA Facial Plast Surg. 2017, 19, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Gabrielli MA, Monnazzi MS, Gabrielli MF, Hochuli-Vieira E, Pereira-Filho VA, Mendes Dantas MV. Clinical evaluation of the bicoronal flap in the treatment of facial fractures: retro- spective study of 132 patients. J Craniomaxillofac Surg. 2012, 40, 51–54. [Google Scholar] [CrossRef]
- Massarelli O, Gobbi R, Soma D, Raho MT, Tullio A. An aesthetically possible alternative approach for craniomaxillo- facial trauma: the “pretrichial incision”. Craniomaxillofac Trauma Reconstr. 2011, 4, 161–170. [Google Scholar] [CrossRef]
- Campbell, WW. Evaluation and management of peripheral nerve injury. Clin Neurophysiol. 2008, 119, 1951–1965. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).