Abstract
In the palatal defects due to surgical resection, flap selection is very important for a correct reconstruction. Different methods have been suggested over the time, however the pedicled buccal fat pad is a simple, effective, reliable flap for reconstruction after palate tumor resection. The aim of the present study is to introduce a new surgical technique for palate reconstruction with pedicled buccal fat pad flap exposing the advantages. The Authors performed this procedure in 17 patients in order to treat medium-sized oncologic surgical defect of palate region in the period between 2016 and 2019. Complete wound healing after only 4 weeks without complication after 12 months follow-up was observed. This is the first cases series described with this new technique.
Introduction
Anatomically, the buccal fat pad (BFP) is a fat mass that is distinct from subcutaneous fat and is situated in the masticatory space close to parotid duct, facial nerve and masticatory muscles.
The body fat is divided into 3 lobes (anterior, intermediate, and posterior) and 4 extensions (buccal, pterygoid, pterygopalatine, and temporal superficial and profound).[1]
The portions more appropriated and easily accessible from oral cavity for flap harvesting are the body and the buccal extension, which together constitute 55% to 70% of total weight.
BFP has an estimated volume of 10 ml, thickness of 6 mm and an approximate weight of 9.3 mg.[2] The BFP’s size is quite constant among different people and normal weight and volume were observed even in cachectic patients.[3]
Blood supply is provided by the buccal and deep temporal branches of the maxillary artery, the transverse facial branch of the superficial temporal artery and from a few branches of the facial artery.
The buccal fat pad was described for the first time as an anatomical element by Bichat in 1802, and the first use of the pedicled buccal fat pad for oral reconstruction was reported by Egyedi in 1977.[4]
Over the time this flap has gained popularity for the reconstruction of intraoral defect thanks to its features: it is simple flap with rich blood supply and optimal anatomical location. It also presents excellent functional outcome and very low complication rates.
The pedicled BFP has different applications in oral and maxillofacial reconstruction, it can be employed in the correction of fistula and oroantral communication, reconstruction of maxillary defect, correction of congenital palate defect, treatment of jaw bone necrosis and oral submucous fibrosis, reconstruction after TMJ ankylosis release and closure of surgical defect after oral tumor excision. [5,6,7,8]
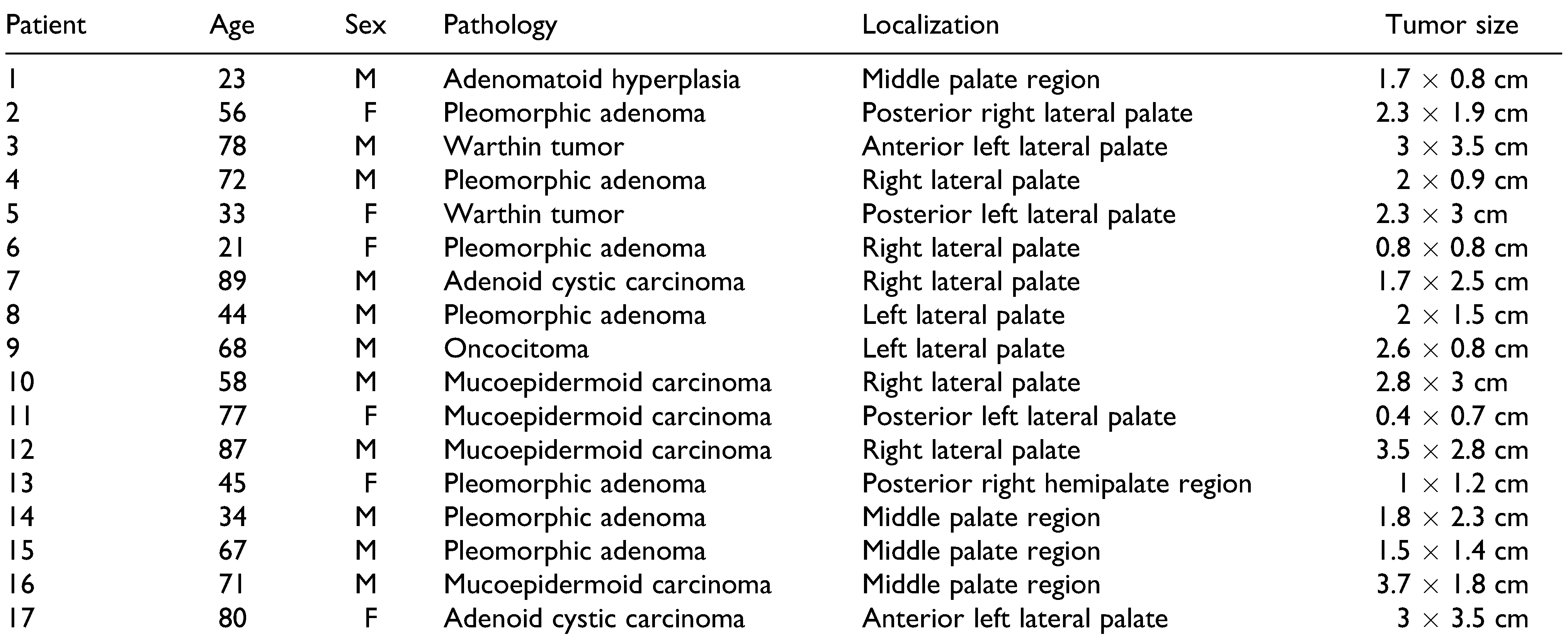
In the field of oncologic oral reconstruction, the hard palate is the location where pedicled BFP has been mostly used.[9] With this paper, the Authors introduce a new tunneled pedicled buccal fat pad flap to improve the efficacy of the reconstruction of the palate mucosa defect, every time there is a residue of healthy mucosa between the surgical defect and the incision made for flap harvesting (Figure 1).
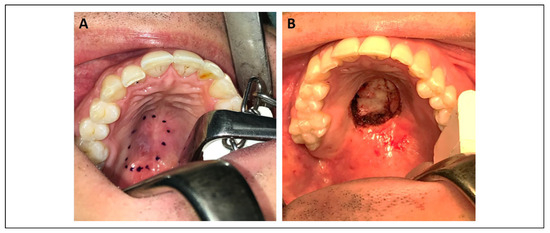
Figure 1.
A. Marking of defect prior resection, B. Surgical defect after resection of tumor.
Surgical Technique
According to our technique, the buccal fat pad flap is taken through an incision made in the posterior third of superior vestibular sulcus extended inferiorly to the mandibular ramus. The incision cuts mucosa and buccinator fibers, exposing the maxillary periosteum and the fat pad. Its fascia is severed, the fat pad is gentle pulled out and the fat septum dissected along the flap with distension of the pedicle (Figure 2).
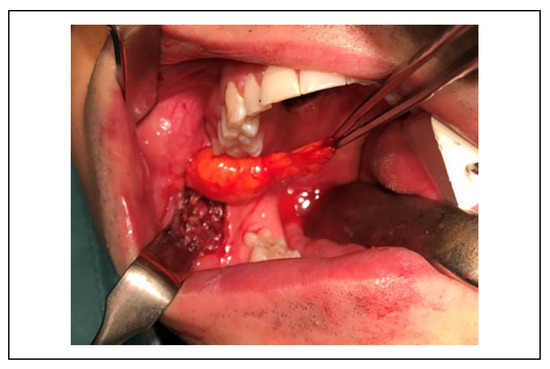
Figure 2.
Preparation of pedicled buccal fat pad.
At this point, starting from the lower part of the incision, made for the preparation of the flap, it is created a submucosal tunnel by blunt dissection, which reaches the palatal surgical defect (Figure 3).
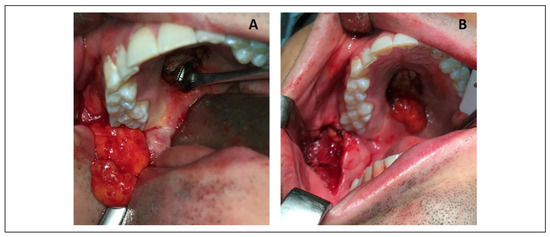
Figure 3.
A. Creation of submucosal passage with the surgical instrument through the tunnel, B. The flap through the tunnel to reach the surgical defect.
The submucosal tunnel passes behind the upper retromolar trigone and then continues into the palate.
The upper part of tunnel, is delimited by the mucosa plane, while the deep part is delimited first by the buccinator muscle and the superior pharyngeal constrictor muscle, then by the palatine aponeurosis of the tensor muscle of the velum palatinum and finally by the horizontal lamina of the palatine bone. The tunnel is submucosal along its path therefore a blunt dissection is indicated for its preparation and is not necessary to elevate the fibrous palatine aponeurosis so firmly adherent to the periosteum.
During the preparation of the tunnel we have to avoid not only mucous perforations but also a too thin upper dissection plan, that can lead to ischemia of the mucosa itself. In this phase, a complication that could arise is the lesion of the aponeurosis of the tensor muscle of the velum palatinum with the consequent transitory velopharyngeal insufficiency.
In addition, it should be taken into consideration the artery and minor palatine nerves that must remain below our dissection plan. Bleeding of the major palatine artery is a complication that could occur during the creation of the tunnel, however bipolar electrocautery is sufficient to do hemostasis.
A sufficiently large submucosal dissection is recommended to allow an easy passage of the pedicle, without any compression and tension of the same. Moreover, compared to the classical technique, by tunneling under the mucosa the length of usable tissue of the flap increases about 1 centimeter allowing to cover a larger and/or more distant palate defect.
The flap is passed through the tunnel and positioned in the palate defect, then it is sutured with 2 or 3 resorbable stitches without any tension and covered by fibrin glue to avoid dehiscences. Antibiotic prophylaxis with cefazolin 2 gr iv peri-operative was prescribed.
In the post-operative period, an accurate oral hygiene with mouthwashes containing 0.2% chlorhexidine, and a soft cold/mild temperature diet for 7 to 10 days are recommended. The patients can brush their teeth starting 1 day after surgery. Ten day after surgery mouth opening exercises are suggested for 4 to 6 weeks to prevent mouth opening limitations.
Discussion
In oral and maxillofacial oncologic surgery, the goal of treatment is not only eradication of disease but also the management of surgically created intraoral defect.
For this reason, in the field of modern oral reconstructive surgery, better surgical techniques are researched to improve the final outcome.
Palate defects are often inevitable after palate tumor resection. Various techniques have been suggested for the coverage of palatal defect which include secondary healing, local flap such as buccal advancement flap, palate rotation flap, tongue flap, or combined buccal and palate double layered closure flap, pedicled BFP. [8,10,11,12]
Microvascular free flaps have also been described for a medium-sized defect however the invasiveness of procedure, operative time and morbidity do not recommend their use.[13]
Since introduction of the buccal fat pad for reconstruction of maxillary defect in 1977,[4] most studies have described the highly successful of the BFP in the reconstruction of different oral defect after tumor resection.[9,14,15]
The BFP is a very versatile flap because it can be used in different direction, for example it can displace anteriorly up to the canine region, posteriorly in the hard palate tuberosity region, retromolar region, the soft palate, and to the anterior tonsillar pillar.[16] Currently, pedicled BFP is the most used flap for immediate small-medium-sized defect reconstruction after palate tumor resection.[8,17]
However, the Authors introduce a new tunneled pedicled BFP in order to improve the reconstruction techniques and the final result.
The tunneled described by the Authors in this new flap not only keeps unchanged the characteristics and peculiarity of classic pedicled BFP such as simplicity and easily harvesting, rich blood supply, rich source of ASCs, low morbidity and failure rate with perfect epithelialization outcome, but presents also the following further advantages:
- Avoids the overstress of flap tissue, that could lead to fragmentation of the flap and in a long term can lead ischemic necrosis at the edge, reducing the risk of partial flap loss, reported in some studies.[18]
- The pedicle included under the mucosal plane instead of directly located in the oral cavity allows a less bulk, that reduces patient’s discomfort and facilitates speech, feeding and swallowing.
- There is no tissue of the flap in masticator space, so this allows patients with partial or total mobile dental prostheses to use them immediately after surgery without compromise of the flap.
- Improves and accelerates healing compared with free graft BFP.[[2[3]
In this technique the extraction of posterior maxillary molars is not necessary and was never performed. Moreover, impacted or erupted third molar is not a contraindication because the tunnel for flap’s passage is created behind the upper retromolar trigone.
The Authors from 2016 to 2019 performed 17 procedure of tunneled pedicled BFP for reconstruction medium-sized middle palate defect after oncologic resection (Table 1). No patients received preoperative radiation therapy.

Table 1.
Summary Table of Treated Patients. Age, Sex, Pathology, Location and Tumor Size (Median Age: 59. 11 Male, 6 Female).
In all patients the defect was adequately repaired, the epithelialization of the flap is complete within 4 weeks (Figure 4). No infection, bleeding, hematoma, oronasal communication, dehiscence or partial flap loss were observed. The “transitory velopharyngeal insufficiency” was observed in 1 patient, probably due to edema of tensor muscle of the velum palatinum, and it spontaneously regressed in 3 weeks. During 12 months follow-up, no retraction or limitation of mouth opening have occurred.
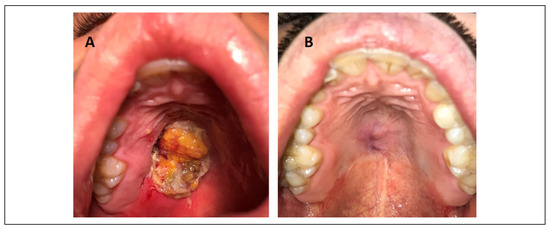
Figure 4.
A. Reconstruction of the defect at the end of surgery with new tunneled buccal fat pad flap, B. Follow-up after 12 months with complete epithelization and healing of the surgical wound.
Conclusion
The new surgical technique for palate reconstruction defect is simple and reliable procedure that can be performed with a very low morbidity for medium-sized middle palate defect.
Submucosal tunnel for pedicle passage introduced by the Authors adds some advantages in final outcomes in terms of healing and less discomfort for the patient proving to be a technique able to adds itself to surgical technique available today.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Authors’ Note
Authors not received funding for this work from any of the following organizations: National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI); and other(s).
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Zhang, H.M.; Yan, Y.P.; Qi, K.M.; Wang, J.Q.; Liu, Z.F. Anatomical structure of the buccal fat pad and its clinical adaptations. Plast Reconstr Surg. 2002, 109, 2509–2518; discussion 2519–2520. [Google Scholar] [CrossRef] [PubMed]
- Racz, I.; Maros, T.N.; Seres-Sturm, L. Structural characteristics and functional significance of the buccal fat pad (corpus adiposum buccae). Morphol Embryol. 1989, 35, 73–77. [Google Scholar]
- Baumann, A.; Ewers, R. Application of the buccal fat pad in oral reconstruction. J Oral Maxillofac Surg. 2000, 58, 389–392; discussion 392–393. [Google Scholar] [CrossRef] [PubMed]
- Egyedi, P. Utilization of the buccal fat pad for closure of oroantral and/or oro-nasal communications. J Maxillofac Surg. 1977, 5, 241–244. [Google Scholar] [CrossRef] [PubMed]
- Hanazawa, Y.; Itoh, K.; Mabashi, T.; Sato, K. Closure of oroantral communications using a pedicled buccal fat pad graft. J Oral Maxillofac Surg. 1995, 53, 771–775. [Google Scholar] [CrossRef] [PubMed]
- Yeh, C.Y. Application of the buccal fat pad to the surgical treatment of oral submucous fibrosis. Int J Oral Maxillofac Surg. 1996, 25, 130–133. [Google Scholar] [CrossRef] [PubMed]
- Ibikunle, A.A.; James, O.; Adeyemo, W.L. Buccal fat pad for interpositional arthroplasty in temporomandibular joint ankylosis. J Maxillofac Oral Surg. 2019, 18, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Koç, O.; Tüz, H.H.; Tosun, E. A novel use of buccal fat pad flap for immediate reconstruction of palatal tumor resection defect. J Craniofac Surg. 2019, 30, 593–595. [Google Scholar] [CrossRef] [PubMed]
- Colella, G.; Tartaro, G.; Giudice, A. The buccal fat pad in oral reconstruction. Br J Plast Surg. 2004, 57, 326–329. [Google Scholar] [CrossRef] [PubMed]
- Mohan, V.; Nair, R.U.; Usha, A.M. Versatility of tongue flaps for closure of palatal defects—case report. J Clin Diagn Res. 2017, 11, ZD31–ZD33. [Google Scholar] [CrossRef] [PubMed]
- Moore, B.A.; Magdy, E.; Netterville, J.L.; Burkey, B.B. Palatal reconstruction with the palatal island flap. Laryngoscope. 2003, 113, 946–951. [Google Scholar] [CrossRef] [PubMed]
- De Riu, G.; Meloni, S.M.; Bozzo, C.; Meloni, F.; Tullio, A. A double buccal fat pad flap for middle palate defect closure—a new technique for palate closure. Int J Oral Maxillofac Surg. 2006, 35, 1057–1059. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.Y.; Ahn, H.C.; Lee, J.H.; Chang, J.W. Flap selection for reconstruction of wide palatal defect after cancer surgery. Arch Craniofacial Surg. 2019, 20, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.A.; Bailey, B.M.W.; Swinson, B.; Witherow, H. Use of the buccal fat pad in the reconstruction and prosthetic rehabilitation of oncological maxillary defects. Br J Oral Maxillofac Surg. 2005, 43, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-K.; Han, W.; Kim, S. The use of the buccal fat pad flap for oral reconstruction. Maxillofac Plast Reconstr Surg. 2017, 39, 5. [Google Scholar] [CrossRef] [PubMed]
- Hassani, A.; Shahmirzadi, S.; Saadat, S. Applications of the buccal fat pad in oral and maxillofacial surgery. In A Textbook of Advanced Oral and Maxillofacial Surgery Volume 3; Motamedi, M.H., Ed.; IntechOpen, 2016; pp. 417–436. [Google Scholar]
- Oliveira Neto, J.Q.; Cetira Filho, E.L.; Andrade, G.S.; Silveira, D.X.; Carvalho, A.C.G.S. Technique of the buccal fat pad flap as an alternative for the surgical defect of pleomorphic adenoma. J Craniofac Surg. 2019, 30, 798–799. [Google Scholar] [CrossRef] [PubMed]
- Padgavankar, P.; Rudagi, B.; Bandral, M.; Hammannawar, R. Reconstruction of palate with buccal fat pad secondary to resection of desmoplastic ameloblastoma. Plast Aesthetic Res. 2015, 2, 91. [Google Scholar] [CrossRef]
© 2021 by the author. The Author(s) 2021.