Introduction
Ocular protrusion measurement is usually done in ophthalmology or endocrinology, for diagnosis of orbital diseases.[
1] Differences in degree of ocular protrusion manifest as exophthalmos or enophthalmos. In maxillofacial surgery, studies have shown that ocular protrusion measurement is an important aspect in planning of exophthalmos or enophthalmos correction, arising primarily or secondarily from trauma or in syndromes.
Exophthalmometry has been used as a tool for measurement of corneal position in relation to the bony orbit. Over the years, there have been many devices that were developed for measuring ocular protrusion. It started with the design of an instrument to measure ocular protrusion by Cohn[
2] and many exophthalmometers were devised following his invention. Each tried to overcome the drawbacks of the other. Hertel had introduced his device in 1905 which was considered to be an exophthalmometer that produced reliable and reproducible results.[
3] As with any other exophthalmometer, this device had also many drawbacks and was modified by many to suit their purposes and overcome the shortcomings.
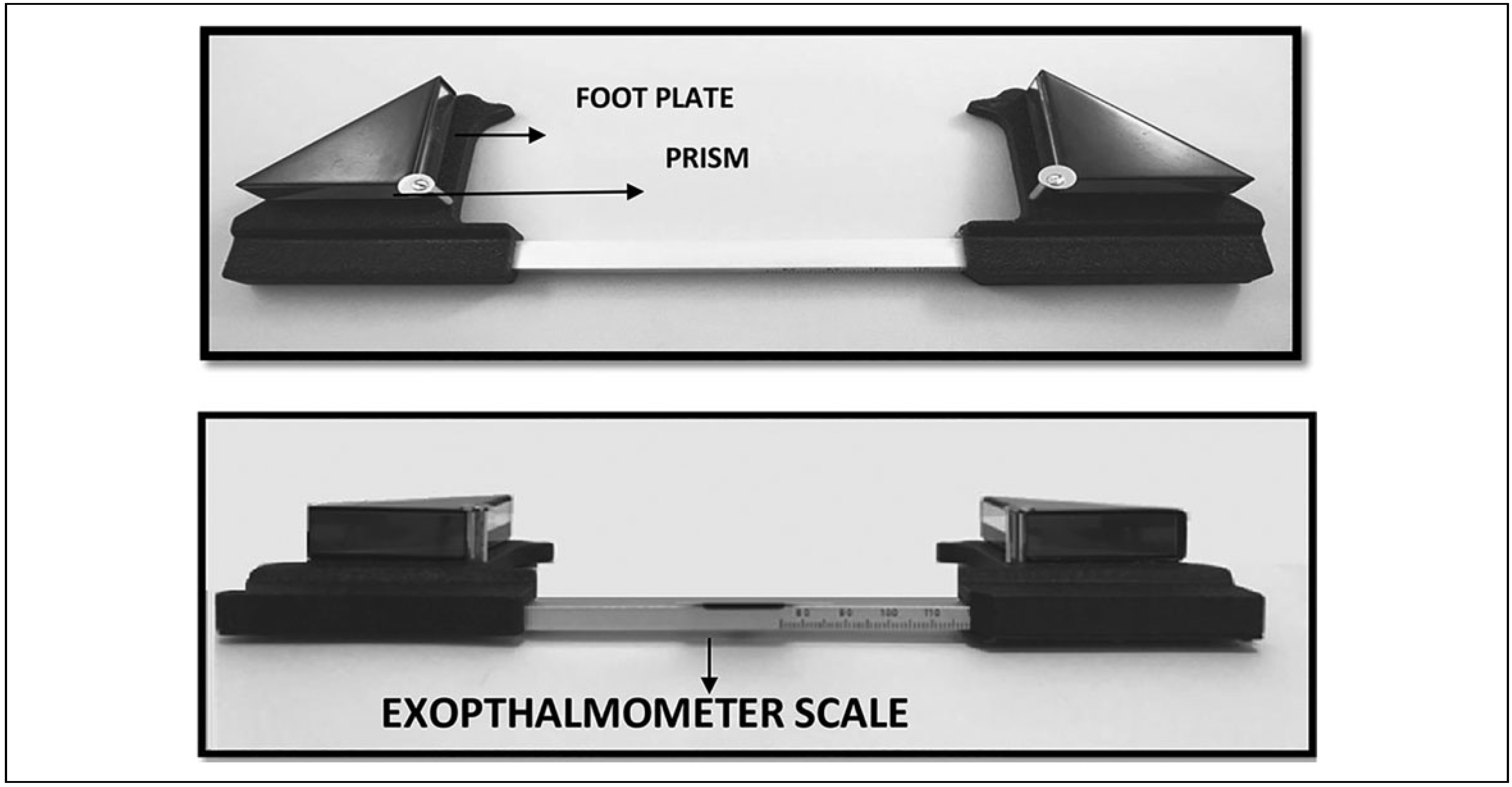
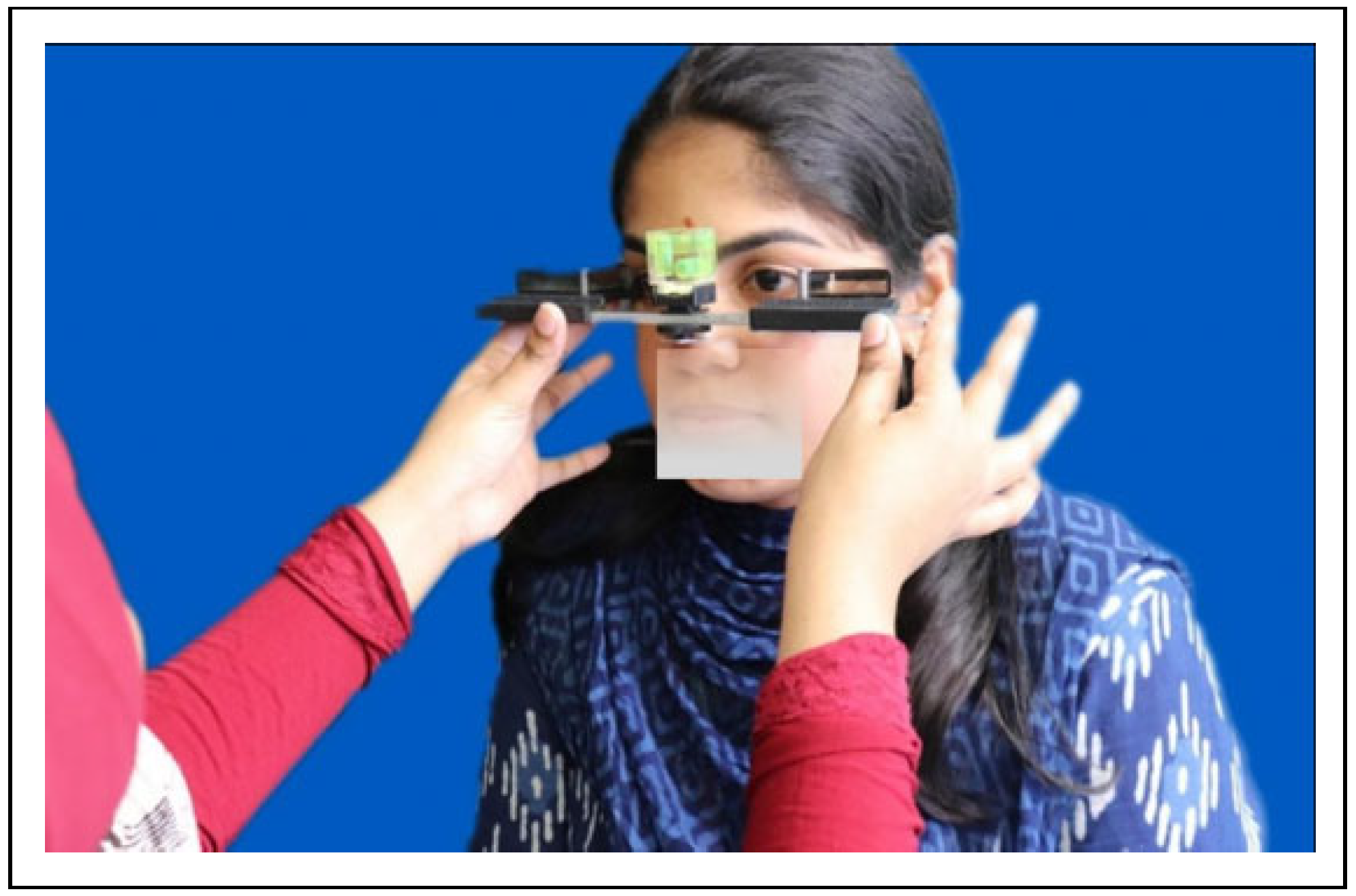
One of the drawback of the instrument was that the readings in Hertel exophthalmometer (
Figure 1) may vary if too much pressure was applied on the orbital rims while seating of the footplates, parallax errors may arise, the instrument relied on intact orbital rims for its placement and rotation of the instrument can occur at the horizontal axis.[
4]
The zygomatic bone being a part of the lateral wall of orbit causes changes in the orbital volume when displaced by a fracture. One of the accepted ways to ensure adequate reduction of the complex zygomatic bone is restoration of orbital volume. It has been agreed by Choi et al that posttraumatic enophthalmos is increased in proportion to the orbital volume.[
5] Enophthalmos occurs with an increase in volume of the bony orbit with consequent posterior displacement of the globe.[
5] An increase in orbital volume is noted in orbital wall fractures which can manifest as enophthalmos. Moreover, most studies have presented that an enophthalmos of greater than 2 mm is an indication for orbital wall surgery.[
6] Secondary post-traumatic deformities of orbit are difficult to correct than those corrected primarily.[
7] Hence, this situation warrants an adequate and proper assessment of intraoperative reduction of zygomatic complex fractures.
Modalities of checking adequate reduction of zygomatic and orbital fractures and restoration of orbital volume intraoperatively include the use of ultrasonography (USG), mobile spiral computed tomography (CT), C-arm fluoroscopy, and C-arm cone-beam CT.[
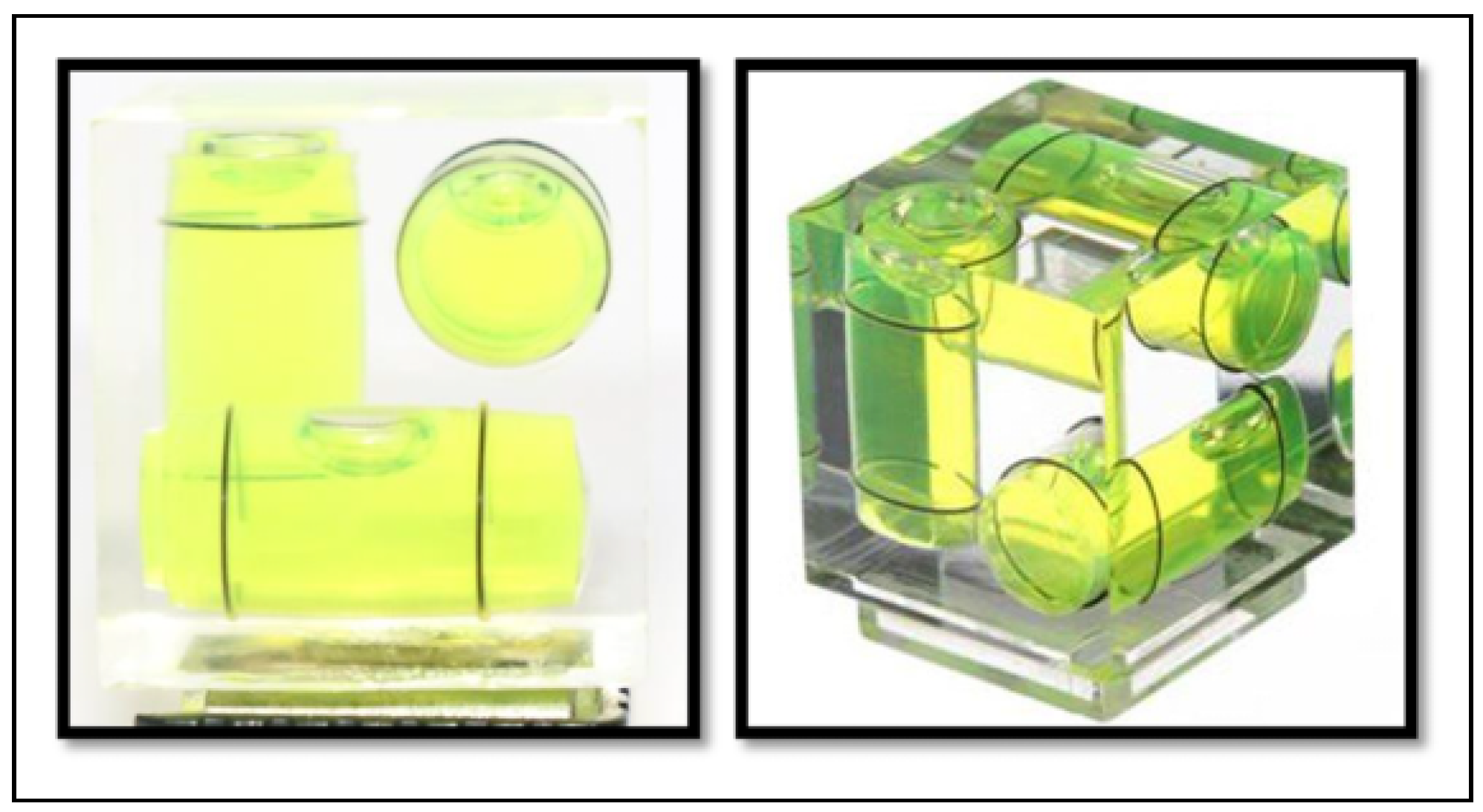
8] These methods may not be suitable at all times. We thus hypothesized that Hertel instrument may be used for this purpose. But the design of Hertel exophthalmometer is such that it requires to be rested on intact lateral orbital rims and this will not be suitable in zygomatic or orbital fractures. So we modified the Hertel exophthalmometer by adding a 3-dimensional (3D) spirit level, which helped to position the instrument in a reproducible way (
Figure 2).
Results
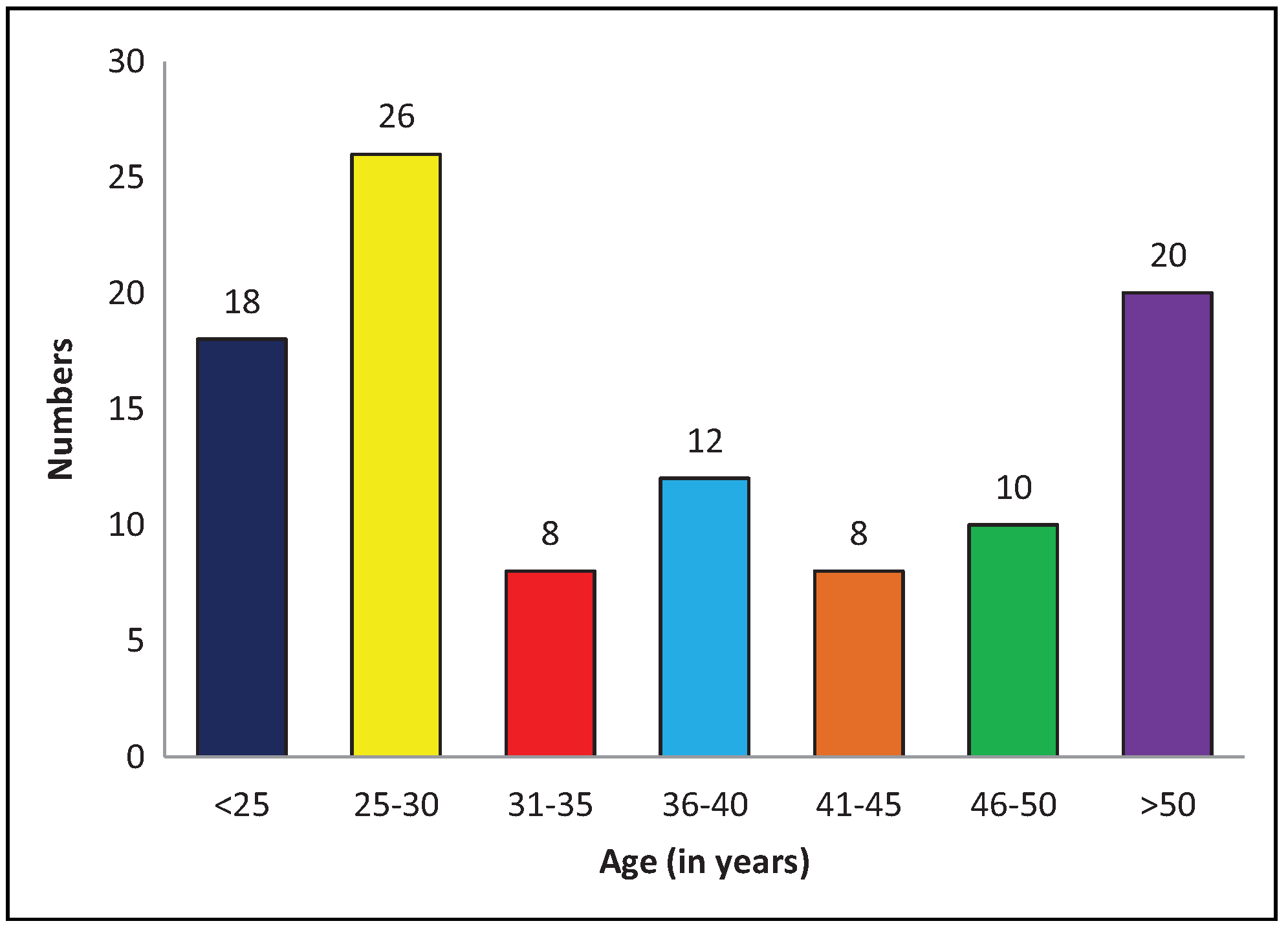
A total of 100 patients were involved in the study. There were 53 female and 47 male. The gender and age distribution is shown in
Table 1 and
Figure 4.
The descriptive statistics of the 100 exophthalmometer readings are given in
Table 2. The minimum reading observed by both standard Hertel and modified Hertel exophthalmometer was 17 for right and left eyes. The maximum reading observed by both standard Hertel and modified Hertel exophthalmometer was 25 on the right eye and 24 on the left eye in our study. The mean reading of standard Hertel on the right eye is 21.1 ± 1.5. The mean reading of standard Hertel on the left eye is 19.8 ± 1.6. The mean reading of modified Hertel on the right eye is 20.9 ± 1.5. The mean reading of modified Hertel on the left eye is 19.6 ± 1.8.
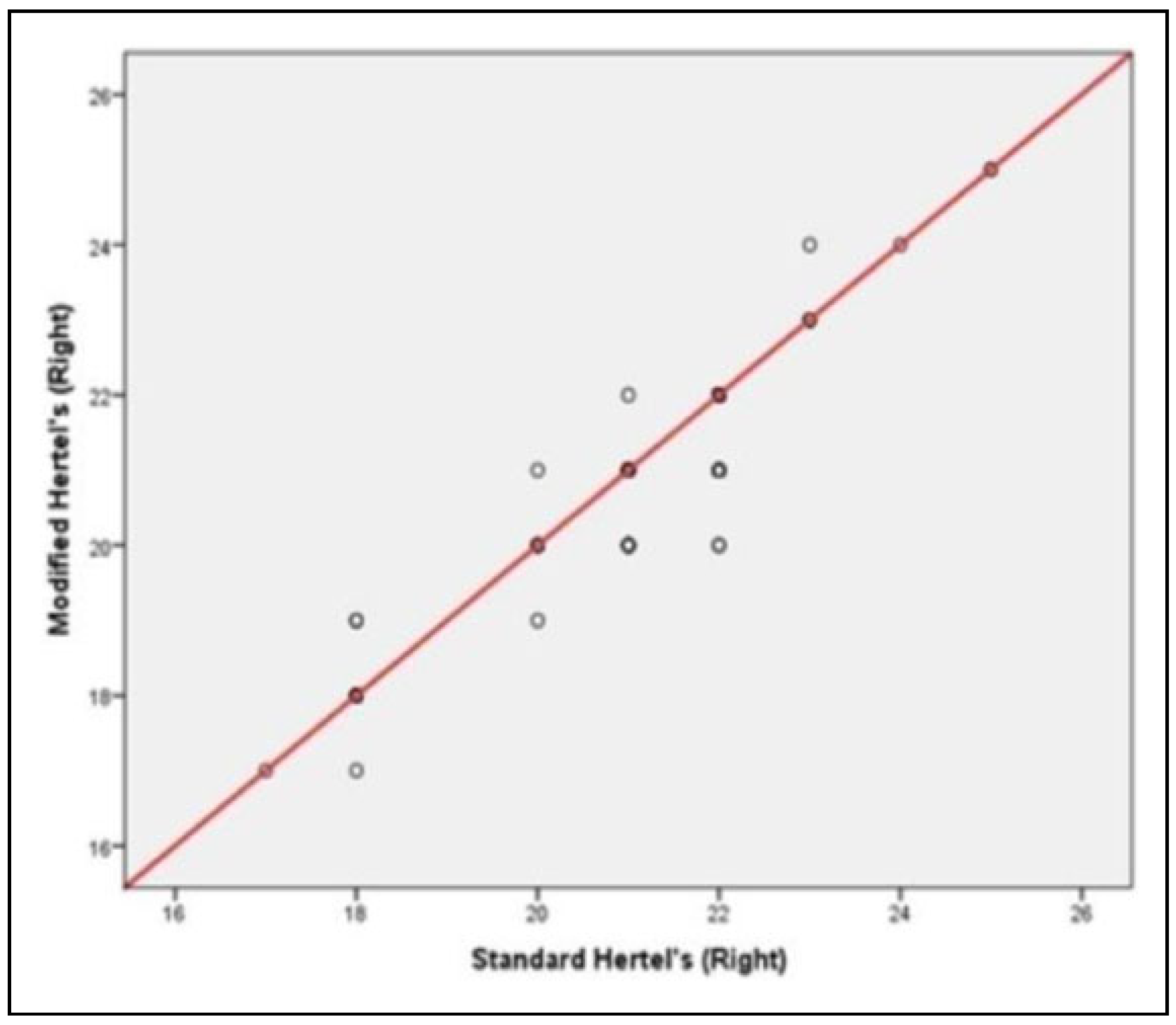
The findings of correlation analysis by Pearson coefficient are presented in
Table 3. The correlation coefficient between standard Hertel and modified Hertel exophthalmometer in the right eye is .933 with a value of
P < .001. The correlation coefficient between standard Hertel and modified Hertel exophthalmometer in the left eye is .919 with a value of
P < .001.
The scatterplot showing correlation between standard and modified Hertel instrument is presented in
Figure 5 and
Figure 6.
This shows a largely positive correlation between these 2 values. The positive correlation shows that when the values of standard Hertel exophthalmometer increase, the values in modified Hertel exophthalmometer will also increase.
The mean values of each age group in each category are described in
Table 4. The mean values obtained in the right eye for our study population was 20.68 for the age group below 30 years, 21.13 for age group from 31 to 50 years, and 21.89 for ages above 50 as measured by Hertel exophthalmometer. The mean values obtained in the left eye for our study population was 19.75 for the age group below 30 years, 19.29 for age group from 31 to 50 years, and 20.89 for ages above 50 as measured by Hertel exophthalmometer. The mean of modified Hertel values obtained in the right eye for patients of age below 30 was 20.50, of age from 31 to 50 was 20.89, and greater than 50 was 21.83. The mean of modified Hertel values obtained in the left eye for patients of age below 30 was 19.45, of age from 31 to 50 was 19.24, and greater than 50 was 20.94.
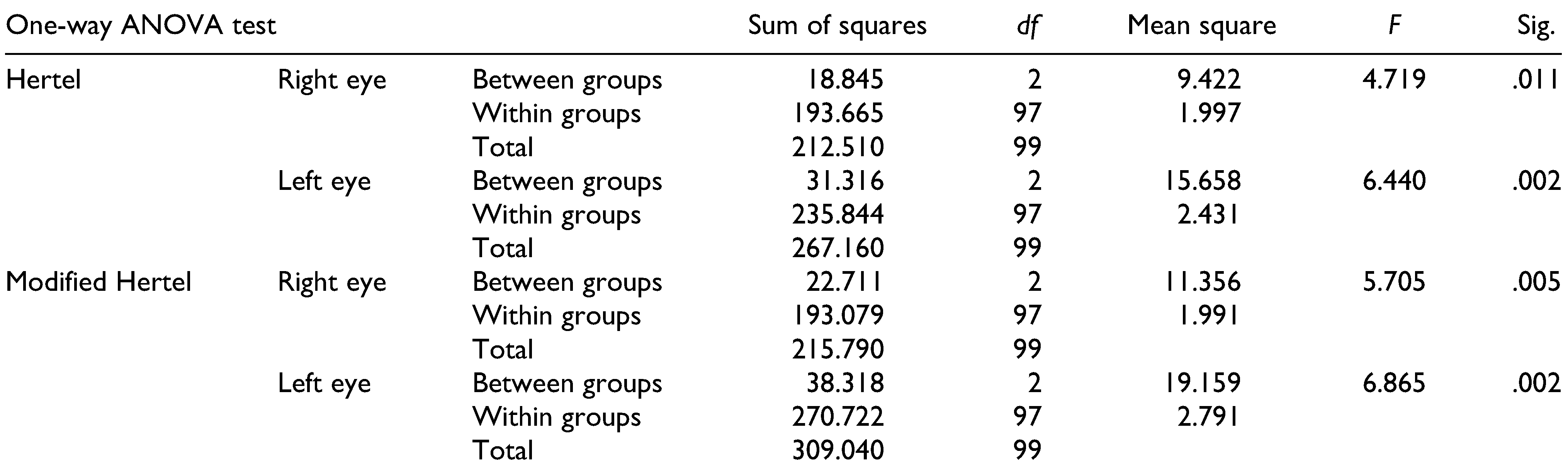
One-way ANOVA test was performed to check the correlation between exophthalmometry values and age of both exophthalmometers. The
F and
P values for Hertel right eye was 4.719 and .011 and for left eye was 6.440 and .002, respectively. The
F and
P values for modified Hertel right eye was 5.705 and .005 and for left eye was 6.865 and .002, respectively (
Table 5).
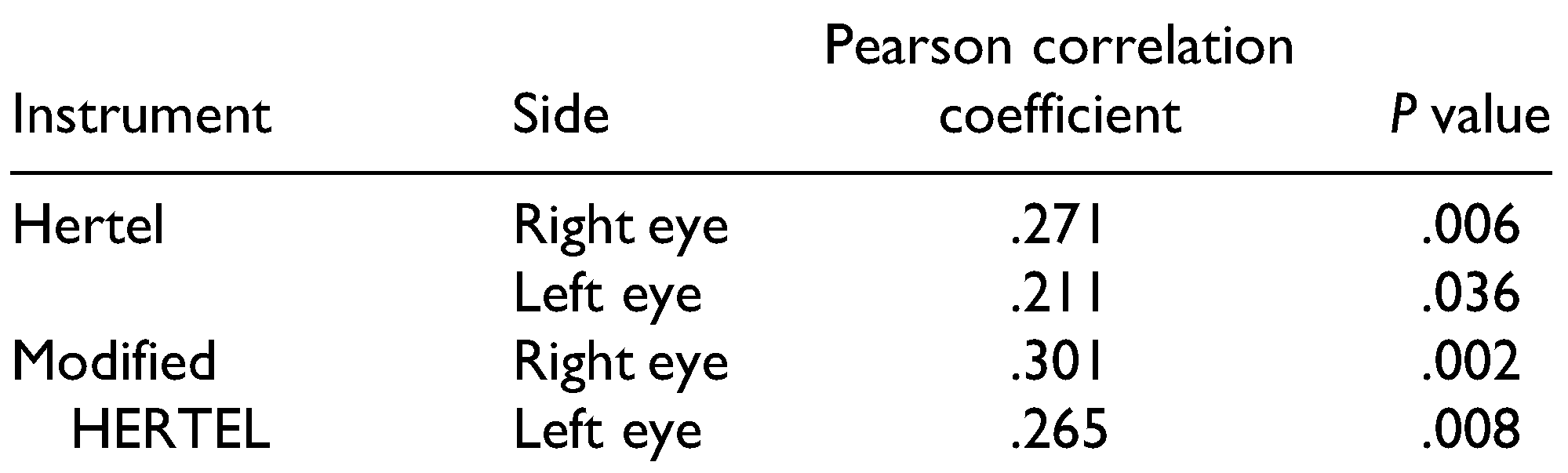
The table shows an increase in exophthalmometric values with age which is statistically significant.The Hertel and modified Hertel instrument readings correlated positively as an increase in age for right eye Hertel with a Pearson correlation coefficient of .271 (
P = .006), for left eye with a Pearson correlation coefficient of .211 (
P = .036), for right eye modified Hertel with a Pearson correlation coefficient of .301 (
P = .002) and left eye modified Hertel with a Pearson correlation coefficient of .265 (
P = .008). There has been an increase in exophthalmometry values with age in Hertel and modified Hertel exophthalmometer.
Both Hertel readings and modified Hertel readings are positively correlated with age and all these correlations are statistically significant (
Table 6).
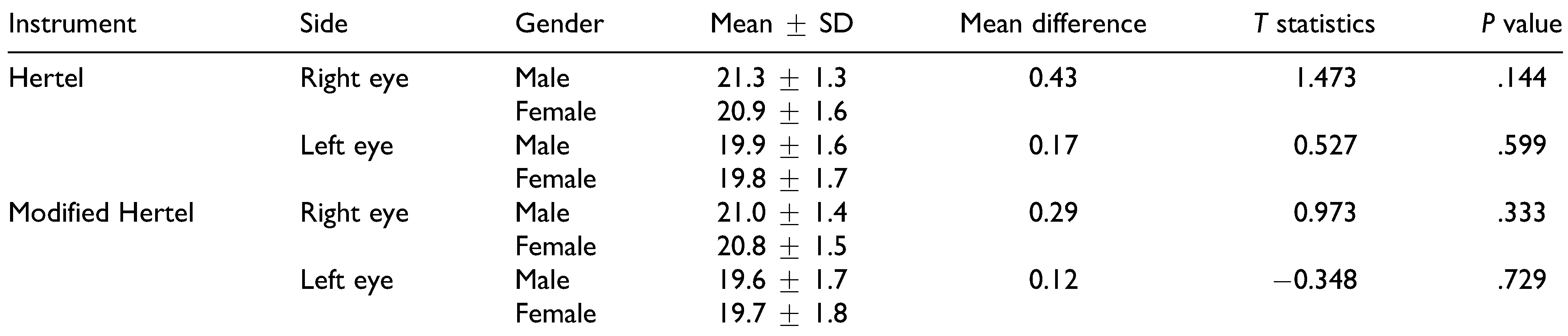
The mean values between male and female were also calculated in the study. It was found that the mean of Hertel exophthalmometer value in our study population in male was 21.3 ± 1.3 mm for the right eye and 19.9 ± 1.6 mm for the left eye. In female, it was 20.9 ± 1.6 mm for the right eye and 19.8±1.7 mm for the left eye. In modified Hertel exophthalmometer, the mean value of ocular protrusion in male was 21.0 ± 1.4 mm for the right eye and 19.6 ± 1.7 mm for the left eye. In female, it was 20.8 ± 1.5 mm for the left eye and 19.7 ± 1.8 mm for the right eye (
Table 7).
There was no statistically significant difference in the values of male and female in both modified and standard Hertel exophthalmometer.
Discussion
Birch-Hirschfield defines absolute exophthalmos as “the difference between the level of the cornea and a point on the orbital rim.”[
9] Enophthalmos is defined as retrodisplacement of globe within the bony confines of the orbit.[
10]
The Hertel exophthalmometer is the most widely used instrument for the measurement of globe position and is a reliable method for measuring the ocular protrusion.[
3] Hertel exophthalmometer involves measuring the distance between the corneal apex and lateral orbital rim and noting the position of this alignment on the millimeter scale. The measurement obtained on the scale can be taken as the exor enophthalmos. Relative exophthalmometry can also be done by using Hertel exopthalmometer.[
11]
But there are 3 major disadvantages of the Hertel instrument as described by Ameri and Fenton:
The resting of the footplate on the lateral orbital rim may be unreliable if too much pressure is applied or if the instrument is not placed properly.
There can be possible rotation of the instrument at the horizontal plane.
Since it has 2 prisms that reflects the cornea, there can be parallax error while the measurement is recorded.[
4]
Also, the application of the Hertel exophthalmometer mainly relied on orbital rims that were intact. Following the development of Hertel exophthalmometer, many people had attempted to modify his instrument to suit various applications and purposes.
The exophthalmometer has found its use in oral and maxillofacial surgery as an instrument to measure restoration of orbital volume, which indirectly results in adequate reduction of zygomatic fractures and prevents postoperative complications like enophthalmos.
Yeatts et al in the year 1992 modified the Hertel exophthalmometer by using the external auditory canal as a reference point in case of fractured orbital rims. They showed no statistical difference between the 2 methods.[
12]
Kratky and Hurwitz in the year 1993 developed a fixation adapter that attaches to a standard Hertel instrument and transfers fixation to the forehead and nasion from the lateral orbit. As concluded by this study, the new fixation adapter applied to the Hertel instrument may be useful in assessing trauma and surgical cases where the lateral orbital rim has been damaged.[
13]
The purpose of our study was to validate the modified instrument to measure adequate restoration of orbital volume after reduction of zygomatic fractures. It has been already agreed that Hertel exophthalmometer is a reliable method for measuring orbital volume.[
3] The anteroposterior displacement caused by orbital trauma can be assessed by Hertel exophthalmometer. The drawback of this instrument that prevented us from using in zygomatic fractures is that it used the lateral orbital rims as a stable point. The lateral orbital rim was often displaced in fractures of zygoma and orbit. The challenge was to modify the instrument to create a stable reference point using the unaffected lateral orbital rim. The solution was in the form of a 3D spirit level incorporated in the horizontal beam of the Hertel instrument. This 3D spirit level allows repeated positioning of the instrument by placing the footplate on the unaffected side and paralleling the spirit level in the
X (horizontal) and
Y (anteroposterior) axes (
Figure 7). Validation of the modified Hertel instrument was done in normal individuals is essential for future use in ensuring adequate reduction in zygomatic fractures, which was done in our study.
An increase in orbital volume is noted in orbital wall fractures which can manifest as enophthalmos.[
14] Significant correlation was observed between the degree of enophthalmos and the volume of herniated orbital contents.[
15] The mechanism for traumatic enophthalmos can be due to enlargement of the bony orbit due to bone loss, loss of ligament support (Lockwood’s ligament), posttraumatic fat atrophy, fat displacement, fat contracture, or neurogenic causes.[
16] Enophthalmos usually correlates with orbital volume and height of retrobulbar portion of orbit.[
17] Post-traumatic enophthalmos is increased in proportion to the orbital volume.[
15]
According to a study by Nasir et al, the most important factor to predict a post-traumatic enophthalmos in the acute phase was the fracture size. It is 3 times more likely to be observed in pure orbital blowout fracture in patients with a floor defect size of more than 150 mm
2.[
18] Preoperative measurements of orbital volume can be used as quantitative values to predict the final degree of enophthalmos in pure blowout fractures.[
5]
Any abnormal relationship between the globe and bony orbit can manifest clinically as exophthalmos or enophthalmos.[
19] Displacement of one or more walls of orbit by fracture causes change in orbital volume. For 3 mm of displacement of either the inferior or medial wall, orbital volume will change from 7% to 12%.[
20] Studies reveal that area of fractures greater than 1.9 cm
2 and volume of herniated tissue more than 0.9 ml causes a change in the degree of enophthalmos. Enophthalmos becomes clinically evident when the relative exophthalmometric value of affected side lies between 3 mm and 4 mm or more.[
21] Late enophthalmos of 2 to 3 mm caused by an unrepaired zygomatic or orbital blowout fracture can cause aesthetic and functional impairment.[
22] A difference of at least 3 to 4 mm in exophthalmometric measurements is necessary to establish pathology.[
23] Usually, 2 mm of enophthalmos corresponds to a bone defect area of approximately 2.75 cm
2 in patients with medial orbital wall fracture.[
24]
A perfect secondary correction of enophthalmos is not easily achieved.[
25] The outcome is better when appropriate fracture reduction and fixation occurs at the first surgery.[
26] The results that are obtained after secondary deformity correction are never as good as obtained in primary repair.[
7] Enophthalmos can be reversed by early or late bone reconstruction which restore the position and shape of the orbital soft tissue by correcting the volume and shape of the bony orbit.[
16] The objective of surgery for correction of enophthalmos in patients with a volume discrepancy should be to decrease the volume of the bony orbit and to increase the anterior projection of the globe.[
6] This can be achieved if intraoperative assessment of globe projection is done after reduction of fractures.
There is no simple and reliable method to assess proper reduction of zygomatic fractures. Various methods like USG,[
27] CT,[
28] and C-arm[
29] had been used in attempt to check proper reduction and restoration of orbital volume. But there are practical difficulties in these methods. Ramli et al found that measurement taken in CT and Hertel exophthalmometry should not be used interchangeably as it will lead to errors in clinical interpretation. Proptosis measures show a lower value in CT scans than in exophthalmometers.[
28] Ocular protrusion values of CT scan showed only intermediate accuracy with the Hertel exophthalmometer.[
30] Nkenke et al did a study on differences in globe position using Hertel exophthalmometry, optical 3D imaging, and CT.[
11] They found that Hertel exophthalmometry can lead to errors in reading when surrounding soft tissue edema or displaced lateral rims is present. Our modification can overcome this issue as the footplate lies only on the unaffected rim.
Normative data in standard and in modified Hertel exophthalmometer in normal individuals were obtained in our study, and values between the 2 instruments were compared. Included in the study were normal adult individuals of age 18 to 50 without any obvious pathology. Children were also excluded from the study as there seems to be an increase in Hertel value in adults as compared to children.[
31] Hyperopic individuals were also excluded as it was found that people with refractive errors may have a false increase in values.[
32]
There is a possibility of parallax errors while measuring in Hertel exophthalmometer as it is a 2-mirror instrument. By aligning the reference line properly with no-parallaxalignment-line given in the reflecting side, this problem can be avoided. The patient should be consistently positioned as far from the reflecting surface of the instrument as possible. These measures were described by Frueh in 2007 and were employed in our study.[
33] The same instrument was used in this study to avoid inter-instrument bias.[
34]
Correlation of age and gender of the patients with exophthalmometry values of standard Hertel and modified exophthalmometer was also done in our study. There was a significant difference, an increasing trend of exophthalmometric values between younger and older adults showing a positive correlation. This was found to be in accordance with many studies.[
31,
35] Hertel exophthalmometry values of 20.5 to 21 mm can be pathological if there is no excessive myopia.[
31] He also added that whenever there is a suspicion of exophthalmos, many factors must be taken into consideration, such as history, race, sex, age, physical type, stature, state of nutrition, cranial form or refraction before establishing diagnosis.[
36,
37]
In a study to determine normative exophthalmometric data in white and black adults, it was found that the normal protrusion in white men was 16.5 mm, white women was 15.4 mm, black men was 18.5 mm, and black women was 17.8.[
38] In another study, the mean protrusion value for black men and women was found to be 24.12 and 22.74, respectively.[
32] In our study, for modified Hertel exophthalmometer, the mean value of ocular protrusion in male was 21.0 ± 1.4 mm for the right eye and 19.6 ± 1.7 mm for the left eye. In female, it was 20.8 ± 1.5 mm for the left eye and 19.7 ± 1.8 mm for the right eye (
P > .05). There was no statistically significant difference in gender as obtained in our study as proved by many other studies in the literature.[
35,
37]
Another aspect that should have been dealt with in this study is interand intra-observer variance and reliability. Various studies have shown with the Hertel exophthalmometer there is some unavoidable and negligible interand intra-observer variance in readings done with the Hertel exophthalmometer.[
3,
39,
40,
41] This was not done in this study to exclude chances of confusion and risk of false values during statistical analysis. However, we plan to implement this topic exclusively in another study.
By comparing these parameters, we could prove that there has been no statistically significant difference in the normative data between standard Hertel and modified Hertel exophthalmometer. Hence, our instrument can be used in cases of zygomatic fractures for assessment of preand postoperative ocular protrusion values, intraoperative assessment for orbital volume restoration after reduction.