Abstract
Study Design: A retrospective study investigating maxillofacial bone fractures in the pediatric and adolescent population. Objective: The aim of this study was to present our experience in the management of pediatric facial bone fractures. Methods: This was a retrospective study of maxillofacial bone fractures in children and adolescents between the ages <1 year and 19 years in a Saudi Arabian subpopulation. Data collected include demographics, etiology, pattern, and treatment of maxillofacial bone fractures. Data were analyzed using IBM SPSS Statistics for Windows Version 25 (IBM Corp.). Results were presented as simple frequencies and descriptive statistics. Results: Of the 1297 patients with maxillofacial bone fractures, 247 were cases involving children and adolescents giving a prevalence of 19.0% (247 patients, N = 1297). There were 233 males and 14 females with an M:F ratio of 16.6:1. The ages ranged from 9 months to 19 years with a mean ± SD of 14.4 ± 4.6. The age-group between 16 and 20 years had the highest frequency of patients (144 (58.4%)). In the 1- to 5-year group, falls accounted for most of the etiology (15 (6.1%)), while in the 16- to 20-year group, motor vehicular accident (MVA) was the main reason (120 (48.6%)). The majority of the fractures occurred in the mandible with 151(61.1%) cases. Open reduction and internal fixation (ORIF) were the main treatment modality in 171 (69.2%) patients. Conclusions: MVA was the main etiology of maxillofacial fractures in children and adolescents with male predominance, while the mandible had been the most frequently fractured bone. ORIF was the main treatment modality.
Introduction
Children and young adults or adolescents represent a special group of trauma patients in oral and maxillofacial surgery, largely due to significant differences of the facial skeleton in comparison to adults.[1] These differences, depending on the age, include craniofacial bone ratio (the cranium-to-face ratio is 8:1 at birth and 2.5:1 in adulthood; the cranium quadruples in size from birth to adulthood, while the face undergoes a 12-fold increase in growth), tiny size of bones, developing sinuses, the presence of growth centers, quicker healing period, and existence of developing tooth germs.[1] Facial bone fractures are uncommon in the very young children because of the greater cranium-toface ratio. The cranial protrusion tends to absorb blunt trauma, leading to skull fractures rather than facial bone fractures that are in retruded position.[2] As the child ages, this cranium-to-face ratio reverses and more facial bone fractures occur. Thus, the epidemiology of maxillofacial bone fractures varies across these age differences. Overall, the prevalence of pediatric maxillofacial bone fractures has been reported to vary between 1.0% and 15.0%.[3] Prevalence is the lowest (1%) in patients under 5 years because of the high cranium-to-face ratio.[4] When the child grows from 6 to 14 years, the prevalence of maxillofacial fractures increases to between 1% and 14.7%, with two peaks occurring during 6 to 7 years when the child starts school and 12 to 14 years when there is increased bodily activities and involvement in sports.[5] The etiology of maxillofacial injuries in children varies according to social, cultural, and environmental factors, however, the main causes worldwide is traffic accidents (vehicular and bicycle), falls, altercations, and sports-related accidents.[6] In the pediatric age-group, fracture patterns are similar to adult, however, the frequency of each bone fracture differs in this agegroup. Studies in this age-group have reported mandibular fractures to be the most common and naso-ethmoidal fractures the least frequent.[7] Within the mandible, condylar and para-symphyseal fractures are reported to be more frequent.[8] In terms of management of pediatric maxillofacial bone fractures, anatomical reduction must be done earlier and immobilization period shorter with a maximum duration of 2 weeks as compared to 4 to 6 weeks in adults because they have greater osteogenic potential and faster healing rates than adults.[2]
Studies have reported prevalence rates, patterns, and management of pediatric maxillofacial bone fractures in other regions of Saudi Arabia,[9,10,11] however, none has been reported in Najran, a southern city of the Kingdom. Therefore, our aim is to report the prevalence, sociodemographics, causes, pattern, and treatment of maxillofacial fractures in children and young adults in Najran, Kingdom of Saudi Arabia.
Materials and Methods
This was a retrospective study of maxillofacial bone fractures seen and managed among children and adolescents in a major referral hospital in the Southern province of the Kingdom of Saudi Arabia over a 20-year period from December, 1999 to December, 2019. Data collected include demographics such as age and gender of patients, etiology, and the pattern of maxillofacial bone fracture. Fractures of the naso-orbito-ethmoidal and nasal regions were excluded because, as our hospital policy, it fell under the management of ENT surgeons. Ethical clearance was obtained from the Ethics and Research Committee of King Khalid Hospital Najran, the Kingdom of Saudi Arabia with IRB number H-11-N-081.
Data were stored and analyzed using IBM SPSS Statistics for Windows Version 25 (IBM Corp.). The Pearson χ2 was used to compare categorical variables. Results were presented as simple frequencies and descriptive statistics. Statistical significance was set at P ≤ .05.
Results
Of the 1297 patients with maxillofacial bone fractures, 247 were cases involving children and adolescents giving a prevalence of 19.0% (247 patients, N = 1297). There were 233 males and 14 females with an M:F ratio of 16.6:1. The ages ranged from 9 months to 19 years with a mean ± SD of 14.4 ± 4.6.
Patients in the age-group 16 to 20 years had the highest frequency of maxillofacial bone fractures (144 (58.4%)). The majority of the fractures (173 (70.0%)) were caused by motor vehicle accidents (MVAs) with a significant difference statistically (P = .002) when etiology was compared with gender of the patients (Table 1). Distribution of fractured maxillofacial bones is as presented in Table 2, where most of them (151 (61.1%)) involved the mandible with a significant difference of P = .000 when etiology was compared with the fractured bones. In the age-group between <1 year and 5 years, mainly falls (15 (6.1%)) accounted for the etiology of the fractures, while in the age-group 16 to 19 years, MVA (120 (48.6%)) was the main reason (Table 2). Surprisingly, assault only accounted for 3 (1.2%) cases in the study population, all in the age-group of 16 to 20 years.

Table 1.
Distribution of Age Groups and Etiology of Facial Fractures in Children and Adolescents According to Gender.

Table 2.
Distribution of Age-Group of Patients and Fractured Maxillofacial Bones According to Etiology of Injury.
Most of the fractures were of the simple type in 202 (81.8%) of cases, while only 12 (4.8%) were of greenstick type that was observed mainly in children under 10 years (Table 3). Comminuted fractures were seen more in the adolescence group from age 15 years (Table 3). Mandibular fractures had the highest frequency of occurrence with 151 cases, representing 61.1%, followed by the maxilla with 42 (17.0%) cases. Other fracture distributions were as presented in Table 3. Open reduction and internal fixation (ORIF) was the main treatment modality for the fractures in 175 (70.8%) of the fractures in this study. These comprised the use of plate osteosynthesis in 171 (69.2%) cases, mainly in the age-group 16 to 20 years. Mono-cortical screws were used for all the patients in the mixed dentition stage. Wire osteosynthesis was used in only 4 (1.6%) cases (Table 4).

Table 3.
Distribution of Fractured Maxillofacial Bone With Type of Fracture.

Table 4.
Distribution of Treatment Modalities According to Age-Group of Participants.a.
Table 5 also presents that 43.3% of ORIF, comprising 41.7% with plates and 1.6% with wires, used in the treatment of maxillofacial fractures, were performed in the mandible.

Table 5.
Distribution of Fractured Maxillofacial Bone According to Treatment Modalities.
All of who had ORIF with plates and screws had them removed. None of our patients had resorbable plates as the fixative material.
Discussion
In general terms, a patient is considered to be a pediatric patient from birth until the age of 18 years, whereas the World Health Organization (WHO) defines adolescence as the period in human growth and development that occurs after childhood and before adulthood, from the ages of 10 years to 19 years.[12]
Children and the adolescents are growing continuously, therefore they have unique physiological and anatomical differences that require additional consideration during diagnosis and treatment planning.[8] It is imperative for the managing oral and maxillofacial surgeon to realize the possible influence of injury and treatment to the developing maxillofacial skeleton. This study provides an overview of the prevalence, pattern, and different treatment modalities of maxillofacial bone fracture in children and adolescents.
Since the World War II, the prevalence of maxillofacial bone fractures in children and adolescents (young adults) has been well reported in the literature.[13] Different modifications and judgments have been proposed in the etiology, incidence, and management in this special group of patients.[14] Studies have reported prevalence of maxillofacial bone fracture in the pediatric population to vary between 1.0% and 15.0% in under 16 years[3,15,16] and between 0.87% and 1.0% under the age of 5 years.[4] The lower prevalence in the patients under 5 years has been attributed to being less active, lighter weight nature, and strict parental guidance, making them to fall less frequently.[17] We have reported a much higher prevalence of 6.9% in the current study in the under 5-year group as compared to 1.0% reported in the literature. This high figure in a Saudi Arabian subpopulation might be attributed to the fact that the male child is more frequently exposed to outdoor activities such as contact sports, bicycle riding, and even an early introduction to car driving from a very young age. Similarly, our study has reported a higher overall prevalence of 19.7% of maxillofacial bone fractures in the pediatric population. The reason might be similar to the under 5-year group higher prevalence rate. Almasri et al[10] have reported a prevalence of 11.9% in the pediatric population from the Makkah region of the kingdom. Almasri[9]in a study of severity and cause of maxillofacial trauma in the Southern Aseer region of Saudi Arabia reported a male:female ratio of 10:1 and found it to be relatively high after comparing it with previous studies from other parts of the Kingdom namely Jeddah (4:1)[18] and Al-Madina (4.8:1).[11] He attributed this relatively high ratio rate in the Aseer Region to the local culture in the region where females spend more time at home, while males spend more time on motor vehicles as the primary means of transport and entertainment. In addition, reckless driving, failure to follow traffic rules, and driving by unlicensed teenagers (adolescents) may contribute further to the incidence of MVAs.
In major cities, the mechanism of maxillofacial injuries can be attributed to low-energy MVAs compared to highenergy injuries in some rural and mountain areas such as Southern Aseer Region.[10] This assertion may also apply to the Southern Region of Najran as our study has shown. In our study, the peak prevalence of fractures was observed in the age-group 16 to 19 years, although there has been a steady rise in the prevalence rate of age-group 4 to 7 years. This observation corroborated the literature wherein it was documented that as the age of the child increases, the prevalence increases. Vyas et al[19] have reported their work that more than half in adolescents from 15 to 17 years old had a maxillofacial bone fracture. This peak prevalence, shown by the current study and substantiated by Vyas et al,[19] occurred during puberty and adolescence. This age-group has been associated with increased unsupervised physical activities and sports.[5,20] While our peak age-group was reported to be 16 to 19 years, other studies have reported lower peak age groups.[15,21] This could have been attributed to different classification of age groups of pediatric patients in different countries.
Worldwide, the prevalence of maxillofacial bone fractures is higher in males than in females and also in all age groups.[22,23,24,25] This male predominance, which has remained consistent over time, has been reported to range from 1.1:1 to 8.5:1.[23] The current study, however, has reported a very wide gap of 16.6:1 between the genders that has not beenreported in the English literature. However, the M:F ratio of 10:1 reported in the Aseer study[9] and the findings from our study in Najran suggests that the overwhelming prevalence of males over females in the maxillofacial fractures in the southern part of the Kingdom is far higher than other parts of Saudi Arabia. The southern region of Saudi Arabia constitutes a very conservative and cultural population, such that females spend more time at home with little or no outdoor activities, while the males spend more time in motor vehicles as a means of transport and entertainment.[9] Furthermore, because women not allowed to drive before in Saudi Arabia, they therefore less susceptible to accidents. However, with the recent permission given to women to drive in the kingdom, the ratio may change in the near future. Generally, male predominance has been attributed to greater and more dangerous physical activities among boys.[5,24,26] On the contrary, Zimmermann et al[2] have reported that below the age of 5 years, gender differences are less noteworthy. However, position in our study was different as there was still a male predominance in the under 5-year group.
In the current study, the commonest etiology of pediatric maxillofacial bone fracture was an MVA as seen in 70% of the study group. This etiology was observed to increase with an increase in the age-group of the patients. Parents are advised to provide protection to their children while driving in a motor vehicle by always keeping them in the rear seats, strapped comfortably in seat belts, child seats, and helmets for on motorcycles or bicycle.[27]
The majority of the citizens and residents in the kingdom have access to cars either as rented or privately owned, especially by the very young people.[28] Reckless driving, failure to follow traffic rules, and, sometimes, driving by unlicensed individuals also contribute heavily to the high incidence of MVA in the region.[1]
Kaban[14] has opined that the usual adult seat belts do not restrain or protect pediatric patients very well because the anterior superior iliac spine is underdeveloped therefore making the restraint to lie on the abdomen and chest. This results in the child lashing forward with greater momentum than adults during sudden deceleration of the car because of greater body mass above the waist and high center of gravity.[14] Studies have reported the common etiology of maxillofacial bone fractures in children below 5 years to fall. The present data are consistent with those of previously published studies.[14,15] In this age-group, low-velocity forces, for example, falls in the home environment, are the most common etiology. In one of our series, a 2-year-old boy had a greenstick fracture of the mandibular symphysis and complete high condylar fracture with medial displacement of the fracture segment (Figure 1A to C). Tell-tail signs like bruise, contusion, ecchymosis, and lacerations in the chin region should be highly suggestive of a combination of mandibular symphysis and condylar fracture (Figure 1D). In adolescence, Braimah et al[29] have reported entanglement injury as a rare etiology of maxillofacial injury. This mechanism of injury involves entanglement of loose clothing worn by females in the conveyor belt of local grinding machine.[29] This mechanism was not observed in our series, despite wearing of loose apparel by the female folks. Surprisingly, assault accounted for only 3 (1.2%) cases in the study population and all in the 16 to 20 years age-group. Despite adolescents been involved in interpersonal violence worldwide,[6,30] this was not observed in our study. This discrepancy could be explained by the fact that Southwestern Saudi Arabia (and especially the city of Najran) have a low violence rate compared to other regions and countries.

Figure 1.
A, Anterior–posterior 3D view of a 2-year-old showing greenstick fracture of the symphysis and right condyle of mandible (with medial displacement fracture fragments). B, True lateral 3D CT scan view of 2-year-old showing fracture of right condyle of mandible. C, 3D CT scan view of a 2-year-old showing greenstick fracture of the lingual aspect of the symphysis of mandible. D, Clinical Photograph of a 2-year-old showing bruising of the chin, a tell-tale sign of symphyseal and condylar fractures. CT indicates computed tomography.
The lesser mineralization of pediatric bones allows them to be bent in response to external forces thus producing greenstick fractures.[28] Greenstick fractures are incomplete fractures of flexible bone, which typically occurs only in children. This is usually seen in the mandible at the lower sub-condylar region in children above 6 years.[31] Similar to our observation, all the greenstick fractures occurred in the mandible and in children above 6 years. Simple fractures were observed in the majority of our study group (81.8%) with statistical significance while comminuted fractures were seen in only 13.3% of our patients. This observation in the latter could be attributed to the high-velocity impact forces secondary to RTA, which is the most frequent etiological factor of maxillofacial bone fracture. Older children as seen in our study are more likely to be exposed to highvelocity maxillofacial injuries such as RTA.[2] With the younger children, high-velocity injuries to the maxillofacial region are not common. Possibility of underreporting them because of high mortality from associated brain trauma could explain its rarity.[2]
It has been reported that the mandible is the most commonly fractured maxillofacial bones in the pediatric population and that the incidence increases with increase in age of the children.[2,4,31] This was corroborated by our findings as the mandible was the most fractured bone (61.1%) to increase in frequency as the child ages into adolescence (Table 3). In the midface, our findings showed maxillary, zygomatic complex, and orbital bone fractures with frequencies of 42 (16.9%), 36 (14.5%), and 15 (6.0%), respectively. Midface fractures in the pediatric population are rare with high impact velocity forces because most of the impact is received by the skull due to the small face and big cranium.[2,3] As this ratio in facial proportion reverses with age, more midface involvement with fractures will then occur.[3] This trend was also observed in our study as the frequency of midface fractures increased with increasing age. Due to anatomical, physiological, and psychological factors, many of the injuries in adults that will require surgical skills and armamentarium could be managed conservatively in children.
Children and young adults have greater osteogenic potential and faster healing rates than adults.[2] Consequently, anatomical reduction in children must be accomplished much earlier, usually within 4 days and immobilization times should be shorter with a maximum of 2 weeks as compared to 4 to 6 weeks in adults.[13] Another important factor in the treatment of children and young adults is the issue of concomitant injuries with respect to fitness for anesthesia and duration of surgery.[13] In our series, though concomitant injuries were not part of our objective, all patients were appropriately given clearance from neurosurgery, general surgery, pediatric surgery, ophthalmology, and cardiothoracic surgery depending on the associated injuries before the management of the maxillofacial injuries under general anesthesia. One 10-yearold child, who sustained fractured right body of mandible, haemarthrosis in left temporomandibular joint, and cervical trauma with dislocation of C6-C7, had Halo Vest applied by the neurosurgeons to protect the cervical spine prior to ORIF of the fractured mandible. In this case, the most appropriate treatment was ORIF with plate osteosynthesis and allows early postoperative mouth opening exercises to prevent left temporomandibular joint ankylosis (Figure 2A to D). Few of our cases were managed by observation, medications, and soft diet in the under 5-year patients. A large proportion of our cases (69.2%) were treated with ORIF using plates with majority among the age 12 to 19 years. Similar treatment rate by ORIF in older pediatric age-group has been reported by Vetter et al[32] This agegroup has been reported to be involved in high-risk activities including driving, which makes them predisposed to injuries.[5] Khan et al[27] attributed the higher prevalence of maxillofacial fractures among the age-group to increase participation in social activities or contact sports, higher incidence of assaults and interpersonal and a general reduction of parental supervision. Skeletal maturity of the maxilla and mandible is reached by approximately 14 to 16 years in girls and 16 to 18 in boys. Since the mandible is the last facial bone to reach skeletal maturity, it is vulnerable to growth-related injuries for the longest time period.[12] Additionally, these age groups have all their permanent teeth erupted, therefore, there is no apprehension about tooth bud injuries during ORIF. Furthermore, it has been reported that this age-group is more likely to be treated like grown adults.[33] In a study comparing the use of conventional plates and resorbable plates in the management of paediatric maxillofacial fractures, Burlini et al[34] recommended the use of resorbable plates for fixation of the fractures. According to them, the advantages of resorbable plates over the conventional plates are that the former completely undergoes hydrolysis after bone healing within 12 to 14 months, do not cause restriction and reduction of bone growth, and avoids the need for a second operation unlike the latter which requires removal in 6 to 8 months at a second operation. Some of the patients in the younger age-group below 8 years in our series, who had a gross displacement of the fracture fragments, were treated with ORIF using microplates with mono-cortical screws. In these groups of patients, the fracture sites involved the symphysis and body regions where the permanent incisors and premolars have moved upward away from the lower border of the mandible. It has been reported that growth disruption is rare in mandibular body.[2] The mandible follows the downward and forward growth pattern of the face with the addition of upward and backward growth of the condyles to maintain contact with the glenoid fossa. Vertical height is gained at the condyle through endochondral replacement, and height is added via remodeling of the ramus.[12]
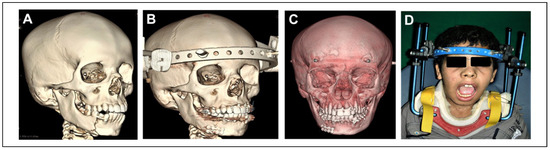
Figure 2.
A, Oblique right lateral 3D CT scan of a 10-year old male victim of MVA showing fractured right body of mandible temporarily fixed with wire. Patient also had left TMJ hemathrosis and cervical trauma with dislocated C6-C7. B, Postoperative 3D CT scan showing ORIF of the fractured right body of mandible. Note the Halo frame used for management for his neck trauma. C, Postoperative 3D CT scan of the 10-year-old patient modified to highlight the 2 microplates in the right body of mandible. D, Postoperative photo of the 10-year-old patient showing satisfactory mouth opening after exercises and wearing a Halo Vest for management of his cervical injuries. Patient was operated wearing this appliance to protect his neck. CT indicates computed tomography; MVA, motor vehicle accident; ORIF, open reduction and internal fixation.
The maxillary fractures were treated with maxillomandibular fixation and elastic traction if the teeth were adequately erupted; if not, then ORIF was used (Figure 3A to E). From our series, the majority of the midface fractures, involving maxilla, zygoma, and orbit, were also managed by ORIF with miniplates in the adolescents and microplates in the pediatric patients. This showed that most of our cases were high-velocity facial impact resulting in gross displacement of fracture segments (Figure 4A to D). All pediatric patients who had ORIF with plate osteosynthesis had the plates removed after bone healing at a second procedure. This is to prevent long-term growth disturbance as reported in the literature.[34]

Figure 3.
A, Photo of a 4-year-old boy who was accidentally knocked down by a reversing car at home showing bilateral infraorbital ecchymosis and anterior open bite suggesting Le fort II maxillary fracture. B, Photo of a 4-year-old boy showing close-up view of anterior open bite as a result of the displaced maxillary fracture. C, Intraoperative photo of the 4-year-old patient with Le Fort II fracture showing split palate. Patient was operated 10 days after recovering from head injury. D, Postoperative photo of the 4-year-old patient with Le Fort II fracture with split palate treated by closed reduction and maxillomandibular fixation with elastics. E, Postoperative photo of the 4-year-old patient, after removal of arch bars, showing restoration of normal occlusion.
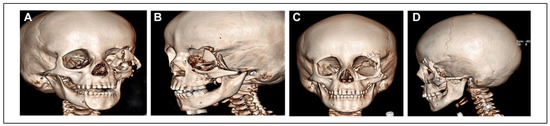
Figure 4.
A, Right oblique lateral view of 3D CT scan of a 5-year-old victim of RTA showing comminuted fractures of left zygomatic complex and orbital floor. Note that patient had a ruptured left eye. B, Left oblique anterior posterior view of 3D CT scan of a 5-yearold victim of RTA showing comminuted fracture of left zygomatic complex and orbital floor. C, Anteroposterior view of postoperative 3D CT scan of a 5-year-old victim of RTA showing ORIF of comminuted fracture of left zygomatic complex and reconstruction of the orbital floor after evisceration of ruptured left globe. D, Left lateral view of postoperative 3D CT scan of the same patient. CT indicates computed tomography; RTA, road traffic accident; ORIF, open reduction and internal fixation.
Conclusion
We have presented an overview of the etiology, incidence, and management of maxillofacial bone fractures among children and adolescents in a major referral hospital in a southwestern city of Kingdom of Saudi Arabia. The male prevalence in maxillofacial fractures among children and adolescents is the highest so far recorded among all the studies in other parts of the Kingdom. High-velocity MVA was observed as the main etiology, and mandible was the most frequently fractured bone in the maxillofacial region. ORIF were the main treatment modality because most of the fractures were grossly displaced. Mono-cortical screws should be employed when ORIF with plate osteosynthesis indicated in the pediatric age-group, especially the mixed dentition stage.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Atrou, I.; Heologie-lygidakis, N.; Tzerbos, F. Surgical protocols and outcome for the treatment of maxillofacial fractures in children: 9 years’ experience. J Craniomaxillofac Surg. 2010, 38, 511–516. [Google Scholar] [CrossRef]
- Zimmermann, C.E.; Troulis, M.J.; Kaban, L.B. Pediatric facial fractures: recent advances in prevention, diagnosis and management. Int J Oral Maxillofac Surg. 2006, 35, 2–13. [Google Scholar] [CrossRef]
- Eggensperger Wymann, N.M.; Ho¨lzle, A.; Zachariou, Z.; Iizuka, T. Pediatric craniofacial trauma. J Oral Maxillofac Surg. 2008, 66, 58–64. [Google Scholar] [CrossRef]
- Haug, R.H.; Foss, J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000, 90, 126–134. [Google Scholar] [CrossRef]
- Ferreira, P.C.; Amarante, J.M.; Silva, P.N.; et al. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plast Reconstr Surg. 2005, 115, 1500–1508. [Google Scholar] [CrossRef] [PubMed]
- Gassner, R.; Tuli, T.; Ha¨chl, O.; Moreira, R.; Ulmer, H. Craniomaxillofacial trauma in children: a review of 3,385 cases with 6,060 injuries in 10 years. J Oral Maxillofac Surg. 2004, 62, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Imahara, S.D.; Hopper, R.A.; Wang, J.; Rivara, F.P.; Klein, M.B. Patterns and outcomes of pediatric facial fractures in the United States: a survey of the National Trauma Data Bank. J Am Coll Surg. 2008, 207, 710–716. [Google Scholar] [CrossRef] [PubMed]
- Shand, J.M. Paediatric oral & maxillofacial surgery. Aust Dent J. 2018, 63 (Suppl 1), S69–S78. [Google Scholar]
- Almasri, M. Severity and causality of maxillofacial trauma in the Southern Region of Saudi Arabia. Saudi Dent J. 2013, 25, 107–111. [Google Scholar] [CrossRef]
- Almasri, M.; Amin, D.; AboOla, A.F.; Shargawi, J. Maxillofacial fractures in Makka City in Saudi Arabia; an 8-year review of practice. Am J Public Health Res. 2015, 3, 56–59. [Google Scholar]
- Albeshir, H.; Ahmed, S.W.; Awaji, M. , et al. Pediatric maxillofacial injuries in madinah—a retrospective study. J Public Health Policy Plann. 2018, 2, 73–80. [Google Scholar]
- Steed, M.B.; Schadel, C.N. Management of pediatric and adolescent condylar fractures. Atlas Oral Maxillofac Surg Clin North Am. 2017, 25, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, R.; Gopalkrishnan, K.; Anand, J. Pediatric facial fractures: a 10-year study. J Maxillofac Oral Surg. 2018, 17, 158–163. [Google Scholar] [CrossRef]
- Kaban, L.B. Diagnosis and treatment of fractures of facial bones in children 1943–1993. J Oral Maxillofac Surg. 1993, 51, 722–729. [Google Scholar] [CrossRef]
- Tanaka, N.; Uchide, N.; Suzuki, K. , et al. Maxillofacial fractures in children. J Craniomaxillofac Surg. 1993, 21, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Ida, S.; Matsuya, T. Paediatric maxillofacial fractures: their aetiological characters and fracture patterns. J Craniomaxillofac Surg. 2002, 30, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Oji, C. Fractures of the facial skeleton in children: a survey of patients under the age of 11 years. J Craniomaxillofac Surg. 1998, 26, 322–325. [Google Scholar] [CrossRef]
- Jan, A.M.A.; Alsehaimy, M.; Al-Sebaei, M.; Jadu, F.M. A retrospective study of the epidemiology of maxillofacial trauma in Jeddah, Saudi Arabia. J Am Sci. 2015, 11, 57–61. [Google Scholar]
- Vyas, R.M.; Dickinson, B.P.; Wasson, K.L.; Roostaeian, J.; Bradley, J.P. Pediatric facial fractures: current national incidence, distribution, and health care resource use. J Craniofac Surg. 2008, 19, 339–349. [Google Scholar] [CrossRef]
- Thorén, H.; Iso-Kungas, P.; Iizuka, T.; Lindqvist, C.; To¨rnwall, J. Changing trends in causes and patterns of facial fractures in children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009, 107, 318–324. [Google Scholar] [CrossRef]
- Holland, A.J.; Broome, C.; Steinberg, A.; Cass, D.T. Facial fractures in children. Pediatr Emerg Care. 2001, 17, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Adams, C.D.; Januszkiewcz, J.S.; Judson, J. Changing patterns of severe craniomaxillofacial trauma in Auckland over eight years. Aust N Z J Surg. 2000, 70, 401–404. [Google Scholar] [CrossRef] [PubMed]
- Adekeye, E.O. Pediatric fractures of the facial skeleton: a survey of 85 cases from Kaduna, Nigeria. J Oral Surg. 1980, 38, 355–358. [Google Scholar]
- Ogunlewe, M.O.; James, O.; Ladeinde, A.L.; Adeyemo, W.L. Pattern of paediatric maxillofacial fractures in Lagos, Nigeria. Int J Paediatr Dent. 2006, 16, 358–362. [Google Scholar] [CrossRef]
- Ferreira, P.; Marques, M.; Pinho, C.; Rodrigues, J.; Reis, J.; Amarante, J. Midfacial fractures in children and adolescents: a review of 492 cases. Br J Oral Maxillofac Surg. 2004, 42, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Al Shetawi, A.; Lim, A.; Singh, Y.K.; Portnof, J.E.; Blumberg, S.M. Pediatric maxillofacial trauma: a review of 156 patients. J Oral Maxillofac Surg. 2016, 74, 1420.e1–4. [Google Scholar] [CrossRef]
- Khan, S.R.; Khan, Z.A.; Hanif, S.; Riaz, N.; Warrach, R.A. Pattern of facial fractures in children. Br J Oral Maxillofac Surg. 2019, 57, 1009–1013. [Google Scholar] [CrossRef]
- Al-Bokhamseen, M.; Salma, R.; Al-Bodbaij, M. Patterns of maxillofacial fractures in Hofuf, Saudi Arabia: a 10-year retrospective case series. Saudi Dent J. 2019, 31, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Braimah, R.O.; Ibikunle, A.A.; Taiwo, A.O. Rare etiological factor of maxillofacial injury: case series seen and managed in a tertiary referral centre. J Emerg Trauma Shock. 2016, 9, 81–84. [Google Scholar] [CrossRef]
- Prigozen, J.M.; Horswell, B.B.; Flaberty, S.K. , et al. All-terrain vehicle-related maxillofacial trauma in the pediatric population. J Oral Maxillofac Surg. 2006, 64, 1333–1337. [Google Scholar] [CrossRef]
- Coban, Y.K.; Bekircan, K. Greenstick fracture of the mandible in a child. J Craniofac Surg. 2017, 28, 1116–1117. [Google Scholar] [CrossRef] [PubMed]
- Vetter, J.D.; Topazian, R.G.; Goldberg, M.H.; Smith, D.G. Facial fractures occurring in a medium-sized metropolitan area: recent trends. Int J Oral Maxillofac Surg. 1991, 20, 214–216. [Google Scholar] [CrossRef] [PubMed]
- McGraw, B.L.; Cole, R.R. Pediatric maxillofacial trauma. Agerelated variations in injury. Arch Otolaryngol Head Neck Surg. 1990, 116, 41–45. [Google Scholar] [CrossRef]
- Burlini, D.; Conti, G.; Amadori, F.; Bardellini, E.; De Gulli, C. Management of paediatric maxillofacial fractures: conventional methods and resorbable materials. Eur J Paediatr Dent. 2015, 16, 24–28. [Google Scholar] [PubMed]
© 2020 by the author. The Author(s) 2020.