Abstract
Study Design: The present study is a systematic review of the literature. Objective: The goal of this study is to review our experience and the current literature on airway management techniques in maxillofacial trauma. Methods: Independent searches of the PubMed and MEDLINE databases were performed from January 1, 2019 to February 1, 2019. Articles from the period of 2008 to 2018 were collected. All studies which described both airway management and maxillofacial trauma using the Boolean method and relevant search term combinations, including “maxillofacial,” “trauma,” and “airway,” were considered. Results: A total of 452 relevant articles in total were identified. Articles meeting inclusion criteria by abstract review included 68 total articles, of which 16 articles were focused on airway management techniques for maxillofacial trauma in the general population and were deemed appropriate for inclusion in the literature review. Conclusions: Establishing an effective and stable airway in patients with maxillofacial trauma is of paramount concern. In both the acute setting and during delayed reconstruction, special considerations must be taken when securing a reliable airway in this patient population. The present article provides techniques for securing the airway and algorithms for utilization of these techniques, including both during the initial evaluation and the definitive operative management.
Introduction
Facial fracture injuries are a major public health concern in the United States, with over 400,000 emergency department visits taking place within a single year, placing a burden of nearly US$1 billion on the American health care system.[1] Stabilization of these patients requires a multifaceted approach and begins with the basic tenets of securing stable airway, breathing, and circulation.[2] Successfully establishing an airway in cases of maxillofacial trauma often requires special consideration of bony and soft tissue damage as well as mechanism of injury. Airway mismanagement can lead to hypoxia, aspiration, further oropharyngeal or laryngeal trauma, and death.[3,4,5]
Maxillofacial trauma often presents in conjunction with cervical spine injury, skull fractures with associated pneumocephalus or intracranial bleeding, and facial lacerations.[6,7] Intracranial injuries particularly may be associated with obtundation, necessitating establishment of an airway even without the presence of respiratory distress. Consequences of generalized craniofacial trauma, including jaw displacement, blood and vomitus in the respiratory tract, and blunt or penetrating trauma directly to the neck, can further complicate effective airway stabilization.[8]
In the emergent setting, pertinent patient factors must first and foremost be considered, including the potentially underdeveloped pediatric airway or the increased ventilatory difficulty of bag masking an obese or hirsute patient. Proper head positioning can prevent airway collapse under pressure, and a laryngeal mask can be used as a salvage option if intubation is difficult due to body habitus or poor visualization of laryngeal structures.[9] Considerations such as positioning the patient in a slightly upright manner, using a supraglottic airway (SGA) in place of mask ventilation, and using a laryngoscope with a modified handle can be important additional strategies.[10,11]
Traumatic displacement of teeth or dental appliances may cause difficulty with ventilation or produce complete airway obstruction. A high index of suspicion must be maintained for displaced teeth into the airway in patients with missing or fractured teeth in the setting of poor ventilation or oxygen saturation in a patient with an otherwise secure upper aiway.[12] Even the presence of excessive facial hair can interfere with ventilation as well as securing an endotracheal tube.[13] Facial hair may impair the seal between a ventilation mask and the face, and if intubation is required, the common technique of securing the endotracheal tube by taping across the jaw is not ideal. To account for these variabilities in how a maxillofacial trauma patient may present, alternative techniques for stabilizing a tube into position will be discussed below.
Soft tissue swelling and bleeding (facial lacerations, epistaxis, oropharyngeal hemorrhage, etc.) may themselves cause respiratory distress or may obscure anatomy and preclude straightforward intubation. Facial fractures are common after maxillofacial trauma in addition to soft tissue injury and pattern may vary based on mechanism.[14,15] These injuries can be categorized into 3 groups depending on the bone(s) involved: upper face (involving frontozygomatic processes, sinuses, or frontal bone fractures), middle face (involving zygomatic arch, nasal bone, orbital floor, naso-orbital-ethmoid, or maxillary fractures), and lower face (involving mandibular fractures). Retrodisplaced midface fractures may obstruct the nasopharyngeal airway, mandibular fractures may release anterior attachments of the tongue base leading to prolapse and airway obstruction, and fracture of the hyoid or laryngeal cartilage may directly obstruct the airway and present a risk for further damage if intubation is attempted. Complications resulting from trauma may hinder the placement of an endotracheal tube and necessitate emergent surgical intervention.
In the prehospital environment, the primary goal of rescue teams treating craniomaxillofacial trauma patients is to establish an airway in any way possible. However, once the patient has been stabilized, the airway obtained in the field may need to be adjusted to facilitate facial reconstructive surgery. Otolaryngologists and maxillofacial surgeons are in a unique position to provide care for these patients, being able to provide both reconstruction of soft tissue injuries and facial fractures as well as effective options for management of the upper airway. As experts in laryngotracheal surgery, otolaryngologists often play a key role in securing the airway in the management of facial fractures in both the acute and delayed repair settings. During planned fracture repair, surgeons and anesthesiologists must collaborate to determine a precise airway plan due to the inherent conflict of a need for a secure airway and a need for surgical access to the face. Airway management interventions utilized in the operating room must fulfill a unique set of criteria, including (1) ease of execution to minimize the time and training experience needed to establish the airway, (2) streamlined design to avoid having bulky obstacles obstructing the surgical field, and (3) durability to prevent dislodgement during surgery.
With these goals in mind, our principal aim is to work toward establishing a more uniform approach to the intraoperative management of difficult, trauma-related airways. In this study, we review current techniques, present case examples of select patients to demonstrate various techniques for stabilizing the airway in key situations, and propose emergent and intraoperative algorithms for securing the difficult airway in maxillofacial trauma patients undergoing head and neck surgery. Photographs of the stabilized airway are included to demonstrate the strengths and pitfalls of each method and to better illustrate the desired outcome of the maneuver.
Materials and Methods
Following Institutional Review Board approval at Penn State Milton S. Hershey Medical Center, a literature review was conducted to synthesize already published guidelines for airway management in maxillofacial trauma patients. Independent searches of the PubMed and MEDLINE databases were performed from January 1, 2019 to February 1, 2019. Articles from the period of 2008 to 2018 were collected. All studies which described both airway management and maxillofacial trauma using the Boolean method and relevant search term combinations, including “maxillofacial,” “trauma,” and “airway,” were considered. All languages were included in the search algorithm, but only studies in English were selected for analysis. International journals translated to English and full-length original articles were assessed for data extraction eligibility. This material was supplemented with targeted searches to address specific needs identified in writing this comprehensive review. References of all publications reviewed were also reviewed for potential inclusion criteria. A qualitative synthesis of the studies was employed to integrate study results. Duplicated articles and abstracts were excluded. Further exclusion criteria included articles that exclusively described a single patient case presentation, non-English language articles, articles involving animal research, or proof of concept articles focused on the development of a novel biomedical device for airway management.
Following the literature review, a retrospective evaluation of various techniques of securing the airway in our maxillofacial trauma patients was also performed. Only selective patients who presented with trauma necessitating complex airway management were included to create the case series. Analysis was performed exclusively on a qualitative basis using intraoperative photographs to demonstrate the efficacy of each described method for securing the airway. As part of our retrospective review, patients were included if they underwent maxillofacial trauma operative repair requiring complex airway stabilization from January 1, 2019 to June 1, 2019. Written informed consent for use of intraoperative photographs in the study was obtained from all patients. Patient photographs were deidentified and collected.
Results
Our systematic review utilizing the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria is depicted in Figure 1. A total of 452 relevant articles in total were identified. Of these 452 search results, only 256 articles were published between the years 2008 and 2018. Of the 256 relevant articles published within the span of 2008 to 2018, 94 studies were excluded due to either being written in a non-English language (n = 10) or describing an animal study (n = 84). The total number of studies screened was 162, and of these, 63 were further excluded due to either not having the full article text available for review (n = 8) or describing a patient presentation as a case report (n = 55). The eligibility analysis reviewed 99 articles, and of these, 15 were further excluded due to the articles not being published in a MEDLINE database journal (n = 15). The qualitative analysis included 84 total articles. Of these, the subject matter for 68 articles was deemed inappropriate for the literature review due to either describing a specific biomedical airway device or a novel technique (n = 8), describing a specific mechanism of trauma in a specific subset of the population (n = 9), relating to a specific complication of facial surgery as a whole (n = 22), or focusing on general airway considerations in surgical patients without maxillofacial trauma (n = 29). The remaining 16 articles were included in the literature review. Due to variability in study design and concept, meaningful synthesis of data in the form of a meta-analysis was not possible. For example, the articles surveyed do not provide data on outcomes of using various methods for securing an endotracheal tube. The articles are also inconsistent in the population they report on (ie, pediatric vs adult patients), and the intubation technique they focus on. The following discussion represents a consolidation of all currently described airway management techniques in the facial trauma patient, and the authors’ proposed treatment algorithm for use of these techniques.
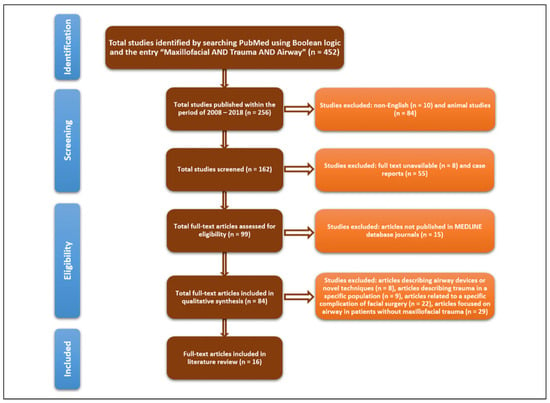
Figure 1.
PRISMA flow diagram depicting the process of selecting studies for the literature review.
Discussion
Emergent Airway Management
The American Society of Anesthesiologists defines a difficult airway as a situation in which a trained medical professional experiences difficulty with ventilation, intubation, or both.[16] For the acute management of difficult airways in patients presenting with maxillofacial trauma, factors that may hinder ventilation or intubation include mandibular fractures, prolapse of the tongue, and blood or vomitus in the pharynx. When a patient presents with altered level of consciousness (as defined by a score of <8 on the Glasgow Coma Scale) and the details of stomach contents are unknown, Rapid Sequence Induction (RSI) is the ideal form of airway management. RSI involves the rapid, simultaneous administration of sedative and neuromuscular blocking agents to induce unconsciousness and muscular paralysis. RSI is used in trauma airway management when the patient is at high risk for aspiration, such as when the patient is obtunded or the patient’s fasting status is unknown. If a cervical spine injury is suspected in a patient, stabilize the patient first using manual in-line stabilization (MILS). Although it has long been employed as a standard of care for managing acute trauma patients, applying MILS in the maxillofacial trauma scenario can restrict jaw opening and tongue displacement, which can make intubation via direct laryngoscopy challenging. However, if done properly, MILS can immobilize the head and neck to prevent aggravation of cervical spine injury while leaving the mandible free for airway access, thus improving the trauma patient’s likelihood of recovery. A flow chart of these factors is shown in Figure 2.
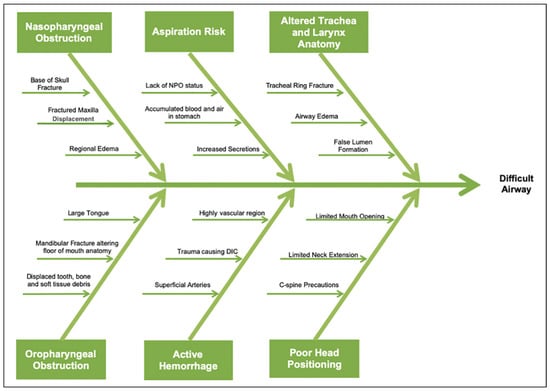
Figure 2.
Factors contributing to a difficult airway in craniomaxillofacial trauma.
Basic tenets of airway management should be followed. In the emergent setting, if no obvious airway foreign bodies are noted in the oral cavity or oropharynx (including fractured teeth or environmental foreign bodies), then bag mask ventilation may be attempted and used to provide oxygenation while a more definitive airway is obtained. An oral or nasal airway may be used as an adjunct. If unable to provide adequate ventilation, advanced airway devices such as an SGA device (eg, laryngeal mask airway or intubating laryngeal mask airway) may provide adequate ventilation while a more secure airway is planned.
In trauma patients who experience tongue base collapse or posterior displacement of the tongue due to mandibular trauma, a tongue retraction maneuver should be attempted and flexible fiber-optic assistance or video laryngoscopy (eg, GlideScope; Verathon) should be used to intubate the patient. Our preferred method for tongue retraction in maxillofacial trauma patients is with a towel clamp (Figure 3). Control of significant hemorrhage from the head and neck should be secondary to securing an airway in the trauma patient. If significant bleeding is present and precludes visualization, an assistant should provide suction and pressure during intubation when possible. Once the airway is secure, necessary measures such as oropharyngeal or nasal packing may be instituted to achieve hemostasis.

Figure 3.
Retraction of tongue using a towel clamp to decrease soft tissue obstruction of the oropharynx in maxillofacial trauma. Alternatively, a penetrating towel clamp can be used.
When ventilation and intubation fail, or in an acutely decompensating patient, a surgical airway should be obtained; options include a cricothyroidotomy or tracheostomy. When evaluating trauma patients in respiratory distress, the presence of severe panfacial fractures, extensive soft tissue injury, and/or laryngotracheal injury should prompt physicians to have a low threshold to institute a surgical airway.
Acute Airway Algorithm
In the emergent setting, the airway is obtained by the rescue team by any means necessary, and algorithms exist to guide airway selection. Once a tube is secured, the airway must be stabilized. Additionally, in an acute (non-emergent) or planned reconstructive setting, many factors must be considered in selecting the appropriate airway and method of securing it. The acute airway algorithm in Figure 4 demonstrates the steps that can be taken to troubleshoot obstacles that arise in the process of securing the difficult airway in the context of maxillofacial trauma.
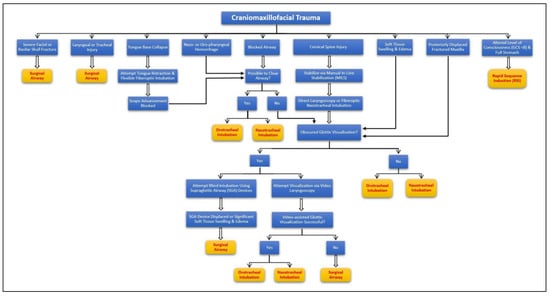
Figure 4.
The proposed algorithm for approaching acute airway management.
Intraoperative Airway Management
When performing a procedure on maxillofacial trauma patients, full access to the surgical site must be maintained while securing the airway. Although a tracheostomy can always position the airway away from the operative field, many simple maneuvers can be instituted and may help to avoid the need for a tracheostomy and the associated risks and complications.[17,18]
Orotracheal Intubation
Several laryngoscopic modalities are available to the surgical team for guiding orotracheal intubation, including direct laryngoscopy, video-assisted laryngoscopy, flexible indirect laryngoscopy, and fiber-optic intubation.[19,20] A meta-analysis by Pieters et al evaluating the efficacy of using laryngoscopy in difficult airway scenarios showed increased first-attempt success and better glottic visualization using video-assisted laryngoscopy versus direct laryngoscopy.[21] As previously mentioned, standard orotracheal intubation may limit access to the lower third of the patient’s face for reconstructive surgery. To prevent interference with the surgical field, techniques do exist that also utilize the oral route. One such option is to use a retromolar intubation technique, in which an endotracheal tube is advanced through the gap in the teeth created by missing or impacted third molars (Figure 5).[22] Retromolar intubation also affords a route to the airway in patients with trismus or patients requiring intraoperative mandibulomaxillary fixation (MMF).[23,24,25] Of note, if a surgeon plans on performing MMF during the case, consideration must be taken for resecuring an airway that becomes dislodged intraoperatively, as this may require expedient removal of the MMF to visualize and replace a dislodged endotracheal tube.

Figure 5.
Demonstration of retromolar intubation. (Image reprinted with permission from Jaisani MR, Pradhan L, Bhattarai B, Sagtani A. Intubation Techniques: Preferences of Maxillofacial Trauma Surgeons. J Maxillofac Oral Surg. 2015;14(2):501-505).
Any airway management intervention performed through the oral route needs to be securely anchored to prevent accidental extubation during surgery. The easiest method for securing an orotracheal tube is to tape the tube away from the surgical field. However, if the patient has extensive facial hair or if taping will interfere with surgical access, the tube may be sutured through the cheek, buccal mucosa, lip, gums, or circumdentally (Figure 6).

Figure 6.
Demonstration of an anchored endotracheal tube by (A) suturing the tube to the lip and (B and C) fixing the tube circumdentally.
Nasotracheal Intubation
Orotracheal intubation may not be ideal for surgical access, particularly in cases of mandibular trauma. When trauma to the midface is limited and displaced septal or nasal bone fractures requiring reduction are not present, nasotracheal intubation is a viable option to maintain the airway.[26] When standard nasotracheal intubation is complicated by the presence of blood or secretions in the nasal passages, or by variations in patient anatomy, image-guided nasotracheal intubation, including fiber-optic-guided, lightwandguided intubation, and newer video-assisted laryngoscopy techniques, can be used.[25,27] It is best to first position the nasotracheal tube cephalically toward the head of the bed to remove it from the surgical field. The tube can be anchored by taping it across the forehead, or by suturing it through the nasal septum and placing a Merocel (Medtronic Inc.), between the tube and soft tissue triangle to prevent necrosis of the nasal tip (Figure 7).[28,29]
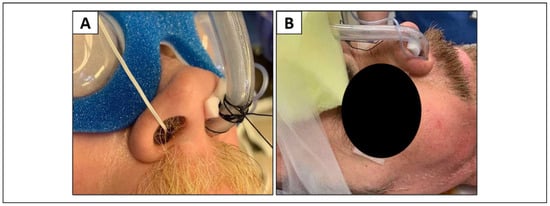
Figure 7.
Demonstration of an anchored nasotracheal tube by (A) securing the tube to the septum with 3-0 silk suture with a Merocel pack in place and (B) taping the tube to the forehead with a Merocel pack in place.
Submental Intubation
In situations where unfettered access to the upper, middle, and lower third of the face is required, such as patients with panfacial fractures, submental intubation may be utilized.
This is a surgical airway obtained by an incision in the submental region and into the floor of the mouth. The oral endotracheal tube is passed through this small incision in the submental triangle.[30] The tube can be secured by suturing it through subcutaneous tissue at the exterior incision site or intraorally through the buccal mucosa or circumdentally (Figure 8).

Figure 8.
Demonstration of submental intubation with endotracheal tube secured to the skin at the exterior incision site with a 3-0 silk purse-string suture.
The advantage of routing the endotracheal tube under the mandible is full access to the entire facial skeleton can be acquired. Additionally, submental intubation is a safe, simple, and aesthetic alternative to other invasive airway techniques, including tracheostomy.[30,31] Perhaps the biggest benefit of submental intubation is that it involves fewer overall complications (0-3%) than other surgical methods of establishing the airway.[30,32] The potential complication profile resulting from submental intubation would include wound infection, facial or lingual nerve damage, salivary gland damage, hypertrophic scar or keloid formation, and oral mucocele.[30] Additionally, the potential increased risk for pneumomediastinum, pneumothorax, or upper airway stenosis (tracheomalacia, A-frame deformity, subglottic stenosis) with tracheostomy are avoided by submental intubation. There is also evidence that this procedure is more cost-effective than tracheostomy, particularly when accounting for aftercare and need for future decannulation.[33,34,35,36]
Tracheostomy
Tracheostomy may be preferred in the setting of severe facial trauma or expected prolonged intubation. The preferred method is via an open approach, although a percutaneous tracheostomy may be performed.[37] In the context of maxillofacial trauma, a tracheostomy affords an airway that is routed entirely clear of the surgical field and is very secure despite extensive manipulation of the head including repositioning, drilling, and so on. Additionally, tracheostomy is ideal if a patient is to be ventilated for a prolonged period of time following surgery.[37] Complications of tracheostomy include pneumomediastinum/pneumothorax, posterior tracheal wall injury, subglottic stenosis, and tracheomalacia as well as the rare but life-threatening tracheoinnominate fistula.[32,38,39,40,41] In a multi-institutional study of the use of tracheostomy procedure, analysis of 1175 patients having undergone tracheostomy tube placement for any cause revealed complication rates of 1.4%, 5.6%, and 7.1% for intraoperative, early postoperative, and late postoperative complications, respectively.[42]
Percutaneous dilational tracheostomy (PDT) is accomplished using a modified Seldinger technique and is often performed with the aid of bronchoscopy.[37] PDT offers several benefits over the traditional open tracheostomy, primarily because it can be performed at the bedside: PDT has been reported to be quicker to perform, with less associated financial costs, and decreased bleeding and infection risks.[37] However, the success of PDT is dependent on surgeon experience and patient factors, and overall may lead to higher rates of post-tracheostomy tracheal stenosis.[43] Therefore, the decision of whether to pursue an open, surgical tracheostomy versus a PDT should be based upon patient selection as well as surgeon comfort and experience.
Tracheostomy tubes may be secured with a commercial tracheostomy tube holder, a commercial tracheostomy tie, a commercial tracheostomy soft collar, and/or sutured directly to the neck skin as an anchor. Suturing the tracheostomy plate is advised postoperatively until the first tracheostomy tube change to prevent accidental decannulation and false passage.
Intraoperative Airway Algorithm
The intraoperative algorithm for securing the difficult airway proposed in Figure 9 attempts to account for variability in injury type and patient factors. For soft tissue injuries without underlying facial or basilar skull fractures, intubation can proceed via either nasotracheal or orotracheal route.[44] In cases of comminuted basilar skull fracture, blind nasotracheal intubation is contraindicated. Accidental intracranial penetration has been reported when advancing an endotracheal tube through the nasopharynx, leading to catastrophic neurological damage and death.[22] However, if the nasotracheal route is selected in skull base trauma, direct visualization over a fiber-optic scope is recommended.[45] For fractures of the upper face including orbital and nasal fractures, orotracheal intubation is a safe and reliable option that would not interfere with the fracture reduction surgery. For fractures of the midface, the method used to manage the airway depends on whether there is a comminuted fracture. If a severely comminuted fracture is present requiring multiple sites of surgical access for repair, a submental intubation or tracheostomy is preferred. For fractures of the lower face, which most commonly affect the mandible, the method of airway management depends on whether MMF is required. If MMF is not required, then orotracheal intubation is the preferred route and the tube may be placed in a retromolar position. However, if MMF is required for fracture reduction, then either nasotracheal intubation, submental intubation, or tracheostomy can be used.
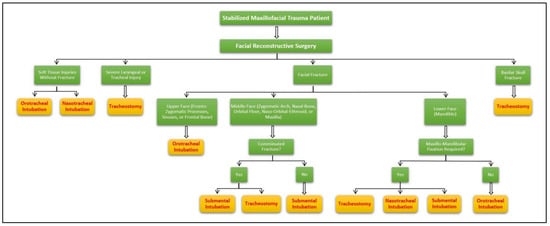
Figure 9.
Proposed algorithm for securing the difficult airway intraoperatively.
Conclusion
Otolaryngologists are uniquely posed to collaborate with the anesthesia team in providing insight on the difficult airway access of a maxillofacial trauma patient from both a reconstructive and surgical airway standpoint. Modifications can be made to standard endotracheal and surgical airway techniques to prevent interference with the surgical field and minimize risk for accidental extubation. The proposed algorithms can be used to guide airway management in patients with maxillofacial trauma in both the acute, emergent setting and during reconstructive procedures.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Allareddy, V.; Allareddy, V.; Nalliah, R.P. Epidemiology of facial fracture injuries. J Oral Maxillofac Surg. 2011, 69, 2613–2618. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.Y.; Khoo, W.X.; Hing, E.C.; et al. An algorithm for the management of concomitant maxillofacial, laryngeal, and cervical spine trauma. Ann Plast Surg. 2016, 77 (Suppl. S1), S36–S38. [Google Scholar] [CrossRef]
- Cook, T.M.; MacDougall-Davis, S.R. Respiration and the airway: complications and failure of airway management. Br J Anaesth 2012, 109 (Suppl. S1), 68–85. [Google Scholar] [CrossRef]
- Cook, T.M. Strategies for the prevention of airway complications—a narrative review. Anaesthesia. 2018, 73, 93–111. [Google Scholar] [CrossRef] [PubMed]
- Horton, C.L.; Brown, C.A., 3rd.; Raja, A.S. Trauma airway management. J Emerg Med. 2014, 46, 814–820. [Google Scholar] [CrossRef]
- Reich, W.; Surov, A.; Eckert, A.W. Maxillofacial trauma— underestimation of cervical spine injury. J CranioMaxillofac Surg. 2016, 44, 1469–1478. [Google Scholar] [CrossRef]
- DeAngelis, A.F.; Barrowman, R.A.; Harrod, R.; Nastri, A.L. Review article: maxillofacial emergencies: maxillofacial trauma. Emerg Med Australas. 2014, 26, 530–537. [Google Scholar] [CrossRef]
- Kovacs, G.; Sowers, N. Airway management in trauma. Emerg Med Clin North Am. 2018, 36, 61–84. [Google Scholar] [CrossRef] [PubMed]
- Klucka, J.; Stourac, P.; Stoudek, R.; Toukalkova, M.; Harazim, H.; Kosinova, M. Controversies in pediatric perioperative airways. Biomed Res Int 2015, 2015, 368761. [Google Scholar] [CrossRef]
- Kristensen, M.S. Airway management and morbid obesity. Eur J Anaesthesiol. 2010, 27, 923–927. [Google Scholar] [CrossRef]
- Mosier, J.M.; Joshi, R.; Hypes, C.; Pacheco, G.; Valenzuela, T.; Sakles, J.C. The physiologically difficult airway. West J Emerg Med. 2015, 16, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.N.; Botros, D.B.; Groban, L.; Bryan, Y.F. Anatomic and physiopathologic changes affecting the airway of the elderly patient: implications for geriatric-focused airway management. Clin Interv Aging 2015, 10, 1925–1934. [Google Scholar] [PubMed]
- Tuzuner-Oncul, A.M.; Kucukyavuz, Z. Prevalence and prediction of difficult intubation in maxillofacial surgery patients. J Oral Maxillofac Surg. 2008, 66, 1652–1658. [Google Scholar] [CrossRef]
- Ghosh, R.; Gopalkrishnan, K. Facial fractures. J Craniofac Surg. 2018, 29, e334–e340. [Google Scholar] [CrossRef]
- Erdmann, D.; Follmar, K.E.; Debruijn, M.; Bruno, A.D.; Jung, S.H.; Edelman, D. A retrospective analysis of facial fracture etiologies. Ann Plast Surg. 2008, 60, 398–403. [Google Scholar] [CrossRef]
- Apfelbaum, J.L.; Hagberg, C.A.; Caplan, R.A.; et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on management of the difficult airway. Anesthesiology. 2013, 118, 251–270. [Google Scholar] [PubMed]
- Akulian, J.A.; Yarmus, L.; Feller-Kopman, D. The role of cricothyrotomy, tracheostomy, and percutaneous tracheostomy in airway management. Anesthesiol Clin. 2015, 33, 357–367. [Google Scholar] [CrossRef]
- Morris, L.L.; Whitmer, A.; McIntosh, E. Tracheostomy care and complications in the intensive care unit. Crit Care Nurse. 2013, 33, 18–30. [Google Scholar] [CrossRef]
- Misirlioglu, G.; Sen, O. Comparison of GlideScope video laryngoscopy and Macintosh laryngoscope in ear-nose and throat surgery. Irish J Med Sci. 2016, 185, 729–733. [Google Scholar] [CrossRef]
- Evans, S.W.; McCahon, R.A. Management of the airway in maxillofacial surgery: part 1. Br J Oral Maxillofac Surg. 2018, 56, 463–468. [Google Scholar] [CrossRef]
- Pieters, B.M.A.; Maas, E.H.A.; Knape, J.T.A.; van Zundert, A.A.J. Videolaryngoscopy vs. direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways: a systematic review and meta-analysis. Anaesthesia. 2017, 72, 1532–1541. [Google Scholar] [CrossRef] [PubMed]
- Kellman, R.M.; Losquadro, W.D. Comprehensive airway management of patients with maxillofacial trauma. Craniomaxillofac Trauma Reconstr. 2008, 1, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Truong, A.T.; Truong, D.T. Retromolar flexible fiber-optic orotracheal intubation: a novel alternative to nasal intubation and tracheostomy in severe trismus. Head Neck. 2015, 37, 423–424. [Google Scholar] [CrossRef] [PubMed]
- Vidya, B.; Cariappa, K.M.; Kamath, A.T. Current perspectives in intra operative airway management in maxillofacial trauma. J Maxillofac Oral Surg. 2012, 11, 138–143. [Google Scholar] [CrossRef][Green Version]
- Jaisani, M.R.; Pradhan, L.; Bhattarai, B.; Sagtani, A. Intubation techniques: preferences of maxillofacial trauma surgeons. J Maxillofac Oral Surg. 2015, 14, 501–505. [Google Scholar] [CrossRef][Green Version]
- Chauhan, V.; Acharya, G. Nasal intubation: a comprehensive review. Indian J Crit Care Med. 2016, 20, 662–667. [Google Scholar] [CrossRef]
- Kwak, H.K.; Lee, S.Y.; Lee, S.Y.; Cho, S.H.; Kim, H.S.; Kim, J.Y. McGrath video laryngoscopy facilitates routine nasotracheal intubation in patients undergoing oral and maxillofacial surgery: a comparison with Macintosh laryngoscopy. J Oral Maxillofac Surg. 2016, 74, 256–261. [Google Scholar] [CrossRef]
- Singh, R.; Sood, N.; Kerai, S.; Puri, A. Use of Merocel® aids in prevention of nasal pressure ulcers following nasal intubation: case series of 33 patients. Indian J Anaesth. 2017, 61, 513–515. [Google Scholar]
- Rastogi, S.; Bhutia, T.; Singh, A.; Arun, P. Nasal ala pressure sores following head and neck reconstructive surgery: a retrospective analysis from a tertiary cancer hospital. Indian J Anaesth. 2017, 61, 74–76. [Google Scholar] [CrossRef]
- Szantyr, A.; Szuta, M.; Zapala, J. Airway management using submental intubation in head and neck surgery. Folia Med Cracov. 2016, 56, 79–85. [Google Scholar]
- Kaiser, A.; Semanoff, A.; Christensen, L.; Sadoff, R.; DiGiacomo, J.C. Submental intubation: an underutilized technique for airway management in patients with panfacial trauma. J Craniofac Surg. 2018, 29, 1349–1351. [Google Scholar] [CrossRef] [PubMed]
- Lima, S.M.; Asprino, L.; Moreira, R.W.; de Moraes, M. A retrospective analysis of submental intubation in maxillofacial trauma patients. J Oral Maxillofac Surg. 2011, 69, 2001–2005. [Google Scholar] [CrossRef] [PubMed]
- Singaram, M.; Ganesan, I.; Kannan, R.; Kumar, R. Evaluation of safety and usefulness of submental intubation in panfacial trauma surgery. J Korean Assoc Oral Maxillofac Surg. 2016, 42, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Kita, R.; Kikuta, T.; Takahashi, M.; et al. Efficacy and complications of submental tracheal intubation compared with tracheostomy in maxillofacial trauma patients. J Oral Sci. 2016, 58, 23–28. [Google Scholar] [CrossRef]
- Kumar, R.R.; Vyloppilli, S.; Sayd, S.; Thangavelu, A.; Joseph, B.; Ahsan, A. Submental intubation: alternative short-term airway management in maxillofacial trauma. J Korean Assoc Oral Maxillofac Surg. 2016, 42, 151–156. [Google Scholar] [CrossRef]
- Jin, H.; Patil, P.M. Midline submental intubation might be the preferred alternative to oral and nasal intubation in elective oral and craniomaxillofacial surgery when indicated. J Oral Maxillofac Surg. 2015, 73, 39–46. [Google Scholar] [CrossRef]
- Freeman, B.D. Tracheostomy update: when and how. Crit Care Clin. 2017, 33, 311–322. [Google Scholar] [CrossRef]
- Barak, M.; Bahouth, H.; Leiser, Y.; Abu El-Naaj, I. Airway management of the patient with maxillofacial trauma: review of the literature and suggested clinical approach. Biomed Res Int 2015, 2015, 724032. [Google Scholar] [CrossRef]
- Fernandez-Bussy, S.; Mahajan, B.; Folch, E.; Caviedes, I.; Guerrero, J.; Majid, A. Tracheostomy tube placement: early and late complications. J Bronchology Interv Pulmonol. 2015, 22, 357–364. [Google Scholar] [CrossRef]
- Singh, T.; Sankla, P.; Smith, G. Tracheostomy or delayed extubation after maxillofacial free-flap reconstruction? Br J Oral Maxillofac Surg. 2016, 54, 878–882. [Google Scholar] [CrossRef]
- Patel, R.S.; McCluskey, S.A.; Goldstein, D.P.; et al. Clinicopathologic and therapeutic risk factors for perioperative complications and prolonged hospital stay in free flap reconstruction of the head and neck. Head Neck. 2010, 32, 1345–1353. [Google Scholar] [CrossRef] [PubMed]
- Halum, S.L.; Ting, J.Y.; Plowman, E.K.; et al. A multi-institutional analysis of tracheotomy complications. Laryngoscope. 2012, 122, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Lerner, A.D.; Yarmus, L. Percutaneous dilational tracheostomy. Clin Chest Med. 2018, 39, 211–222. [Google Scholar] [CrossRef] [PubMed]
- Jazayeri-Moghaddas, O.P.; Tse, W.; Herzing, K.A.; Markert, R.J.; Gans, A.J.; McCarthy, M.C. Is nasotracheal intubation safe in facial trauma patients? Am J Surg. 2017, 213, 572–574. [Google Scholar] [CrossRef] [PubMed]
- Mittal, G.; Mittal, R.K.; Katyal, S.; Uppal, S.; Mittal, V. Airway management in maxillofacial trauma: do we really need tracheostomy/submental intubation. J Clin Diagn Res. 2014, 8, 77–79. [Google Scholar] [CrossRef]
© 2020 by the author. The Author(s) 2020.