Comparative Evaluation of Clinical and Radiological Outcomes of Retromandibular Transparotid and Transoral Endoscopic-Assisted Approach for Surgical Management of Mandibular Subcondylar Fractures
Abstract
:Introduction
Patients and Methods
Inclusion criteria
- Patients in the age group of 18-60 years.
- Noncomminuted laterally displaced unilateral subcondylar fractures with more than 2 mm overlap and/or >10◦ angulation with or without other concomitant fractures of mandible and with sufficient dentition to reproduce the occlusion.
- Bilateral mandibular condylar fractures where only one side warranted open reduction.
- The time gap between the day of trauma to admission in the hospital should be <3 weeks.
- Subject consent to participate.
Exclusion criteria
- Patients with a history of uncontrolled diabetes mellitus, prolonged steroid therapy, compromised immunity, and associated bone pathology.
- Intracapsular condylar fracture, undisplaced fractures of mandibular condyle, comminuted mandibular condylar fracture, concomitant pan facial or midface fracture, and history of previous mandibular fractures or osteotomies.
- The tendency for keloid formation and those with contused lacerated wounds, abrasions or avulsive soft tissue injuries around the area of extra-oral incision, and presence of preinjury or postinjury facial nerve palsy.
- Occlusion: in the postoperative period: 0: intact, 1: altered occlusion which could be adjusted with intermaxillary elastics and intermaxillary fixation (IMF), 2: altered occlusion could not be adjusted by intermaxillary elastics or IMF and required reoperation.
- Scar: Stony Brook scar assessment scale[12] was used (0: worst and 5: best). Three blinded observers individually rated the scar. The interobserver reliability test was done to see the strength of agreement between raters.
- Surgical ease was evaluated by the time taken for surgery and also by a variable fracture severity score (FS), which correlated the severity of fracture and time taken during surgery. This included a preoperative score of mandibular mobility index, loss of ramus height, and degree of displacement (FS: 0-3 = Less Severe, 4-5 = Moderately Severe, 6-7 = Very Severe).
- Facial nerve injury: House Brackman facial nerve grading scale was used (0: Normal, 1: Normal, 2: Slight Dysfunction, 3: Moderate Dysfunction, 4: Moderately Severe Dysfunction, 5: Severe Dysfunction, 6: Total Paralysis).[9]
- Time elapsed since the day of trauma and time taken for surgery were correlated for the association. Similarly, the presence of multiple fractures of the mandible and postoperative occlusion were evaluated for the association.
Radiographic Assessment
Statistical Analysis
Surgical Procedure
The Retromandibular Transparotid Approach
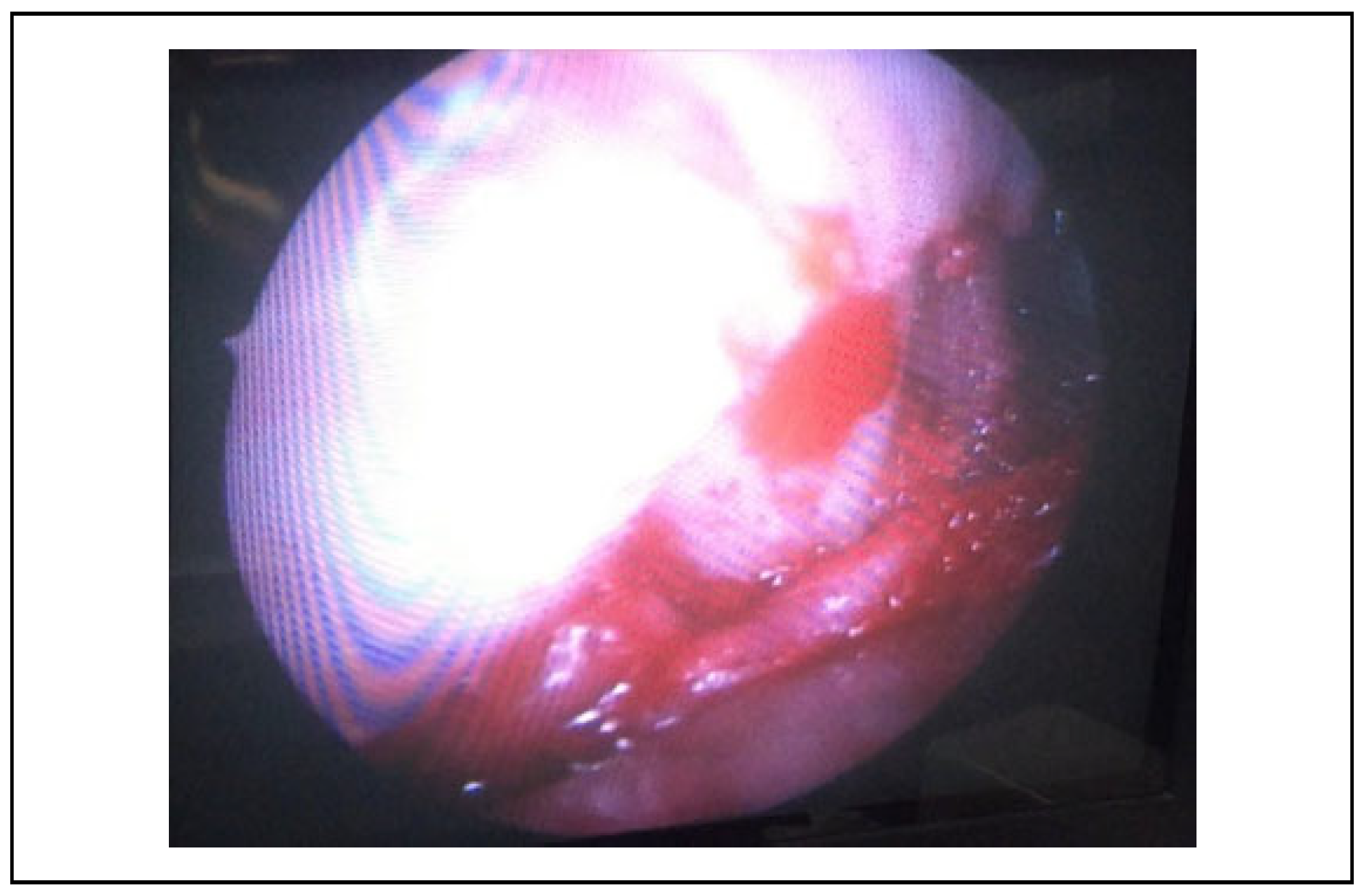
Endoscopic-Assisted Transoral Open Reduction and Internal Fixation
Results
Demographic Results
Clinical Results
- Helkimo dysfunction index. This is a systematic tool to assess the functional status of temporomandibular joint (TMJ) and quantifies the dysfunction present and allows for correlation between the patient symptoms and clinical finding.
- Occlusion. Preoperative occlusion was deranged in all 20 cases.
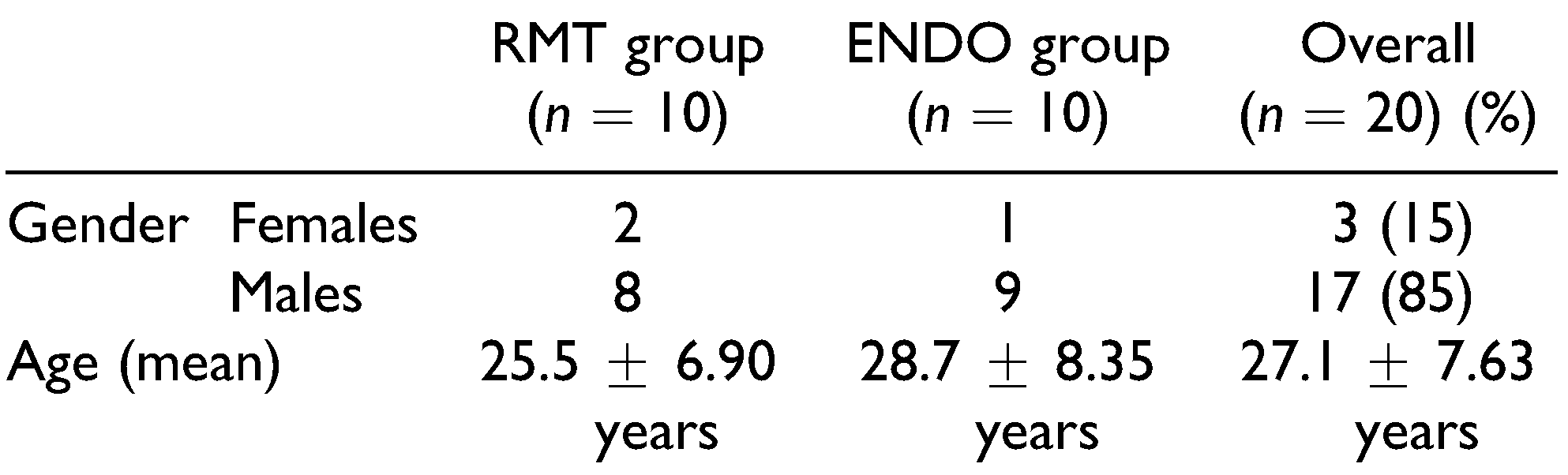 |
- Scar. For the RMT group, three blinded observers individually rated the scars. Based on the 95% confident interval of the ICC estimate, there was a statistically significant agreement between raters, ICC = .801 (95% CI, 0.949 to 5.292), P = .001. The strength of agreement was classified as very good reliability. A repeated measure ANOVA test showed that the scar assessment scale significantly got better over time F(1.68) = 35.335, P < .001.
- Surgical ease. The mean time taken in RMT group was 63.5±12.48 minutes, whereas the mean operative time taken in ENDO group was 196.6 ± 48.9 minutes. The mean operating time for ORIF by RMT approach was 3 times faster than the ENDO (P < .001). An attempt was made to see if the severity of fracture positively correlated with the amount of time taken for surgery. A fracture severity score (FS) was developed and showed no statistically significant difference between the groups (P = .811). Only 2 patients in ENDO group experienced a surgical or technical complication during the procedure where the fracture fragments were grossly overlapped and for reduction, a supplementary incision was given near the lower border to facilitate the reduction (Table 4).
 |
- Facial nerve injury. Temporary facial nerve weakness was an innate complication of the RMT approach, especially of the marginal mandibular and buccal branches. At the end of 6 months follow-up, recovery of the facial nerve damage was noted in 5 (P = .003) out of 6 patient in RMT group and in ENDO group only 1 patient had facial nerve weakness, which recovered fully at the end of 6 months. There was a significant improvement in grades over time (P = .001) for both groups.
- Correlation between parameters. Spearman’s correlation showed no relation between number of fractures and postoperative occlusion at 1 month, 3 months, and 6 months for both the groups (r = .320, P = .192; r = .223, P = .092, and r = .122, P = .568, respectively). Whereas a moderate relation was found between time elapsed since trauma to surgery and time took for surgery (r = .458), which was statistically significant (P = .042). This means that the delay in instituting treatment increased the time taken during surgery.
 |
 |
| Mean + SD (◦) | Pre-op | 1 month | 3 month | 6 month | |
|---|---|---|---|---|---|
| Degree of displacement | RMT group (n = 9) | 18.0 + 11.0 | 3.6 + 3.7 | 2.6 + 3.3 | 1.4 + 1.66 |
| ENDO group (n = 9) | 19.7 + 11.91 | 3.6 + 4.1 | 2.6 + 2.3 | 1.2 + 1.71 | |
| Overall (n = 18) | 18.8 + 11.17 | 3.6 + 3.8 | 2.6 + 2.7 | 1.3 + 1.6 | |
| P values (A vs B) | 0.762 | 1.0 | 1.0 | 0.784 | |
| P values (over time) | P > .001 |
- Complications. During the follow-up period, surgical complications like formation of salivary fistula, sialocele, Frey’s syndrome, infection were not encountered in any of the cases.
Radiographic Results
Discussion
| Mean + SD (mm) | Pre-op | 1 month | 3 month | 6 month | |
|---|---|---|---|---|---|
| Loss of ramus height | RMT group (n = 9) | 4.30 + 2.9 | 2.30 + 1.4 | 1.90 + 1.5 | 1.70 + 1.4 |
| ENDO group (n = 9) | 3.90 + 2.2 | 1.70 + 1.4 | 1.60 + 1.7 | 0.80 + 1.5 | |
| Overall (n = 18) | 4.10 + 2.5 | 2.00 + 1.4 | 1.75 + 1.6 | 1.25 + 1.5 | |
| P values (A vs B) | .734 | .357 | .690 | .192 | |
| P values (over time) | P > .001 |
- (a)
- Consider design and use of instruments which may facilitate 3D control of the condylar fragment postreduction while at the same time not interfering with the optical cavity.
- (b)
- Coronoidectomy may allow a direct visualization of the condylar fracture site when transoral route is adopted.
Conclusion
Funding
Conflicts of Interest
References
- Al-Moraissi, E.; Ellis, E. Surgical treatment of adult mandibular condylar fractures provides better outcomes than closed treatment: a systematic review and meta-analysis. J Oral and Maxillofac Surg. 2015, 73, 482–493. [Google Scholar] [CrossRef] [PubMed]
- Zachariades, N.; Mezitis, M.; Mourouzis, C.; Papadakis, D.; Spanou, A. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J Oral and Maxillofac Surg. 2006, 34, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Villarreal, P.; Monje, F.; Junquera, L.; Mateo, J.; Morillo, A.; Gonza´lez, C. Mandibular condyle fractures: determinants of treatment and outcome. J Oral and Maxillofac Surg. 2004, 62, 155–163. [Google Scholar] [CrossRef]
- Mueller, R.; Czerwinski, M.; Lee, C.; Kellman, R. Condylar fracture repair: use of the endoscope to advance traditional treatment philosophy. Facial Plast Surg Clin North Am 2006, 14, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E.; McFadden, D.; Simon, P.; Throckmorton, G. Surgical complications with open treatment of mandibular condylar process fractures. J Oral and Maxillofac Surg. 2000, 58, 950–958. [Google Scholar] [CrossRef]
- Kanno, T.; Sukegawa, S.; Tatsumi, H.; et al. The retromandibular transparotid approach for reduction and rigid internal fixation using two locking miniplates in mandibular condylar neck fractures. Int J Oral Maxillofac Surg. 2014, 43, 177–184. [Google Scholar] [CrossRef]
- Kanno, T.; Sukegawa, S.; Tatsumi, H.; et al. Does a retromandibular transparotid approach for the open treatment of condylar fractures result in facial nerve injury? J Oral and Maxillofac Surg. 2016, 74, 2019–2032. [Google Scholar] [CrossRef]
- Schmelzeisen, R.; Cienfuegos-Monroy, R.; Scho¨n, R.; Chen, C.; Cunningham, L.; Goldhahn, S. Patient benefit from endoscopically assisted fixation of condylar neck fractures—a randomized controlled trial. J Oral and Maxillofac Surg 2009, 67, 147–158. [Google Scholar] [CrossRef]
- Shi, D.; Patil, P.; Gupta, R. Facial nerve injuries associated with the retromandibular transparotid approach for reduction and fixation of mandibular condyle fractures. J Oral and Maxillofac Surg. 2015, 43, 402–407. [Google Scholar] [CrossRef]
- Kokemueller, H.; Konstantinovic, V.; Barth, E.; et al. Endoscopeassisted transoral reduction and internal fixation versus closed treatment of mandibular condylar process fractures—a prospective double-center study. J Oral and Maxillofac Surg. 2012, 70, 384–395. [Google Scholar] [CrossRef]
- Suhas, S.; Ramdas, S.; Lingam, P.; Kumar, H.; Sasidharan, A.; Aadithya, R. Assessment of temporomandibular joint dysfunction in condylar fracture of the mandible using the Helkimo index. Indian J Plastic Surg. 2017, 50, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Singer, A.; Arora, B.; Dagum, A.; Valentine, S.; Hollander, J. Development and validation of a novel scar evaluation scale. Plast Reconstr Surg. 2007, 120, 1892–1897. [Google Scholar] [CrossRef]
- Singh, V.; Bhagol, A.; Goel, M.; Kumar, I.; Verma, A. Outcomes of open versus closed treatment of mandibular subcondylar fractures: a prospective randomized study. J Oral and Maxillofac Surg. 2010, 68, 1304–1309. [Google Scholar] [CrossRef] [PubMed]
- Ghezta, N.; Bhardwaj, Y.; Rani, P.; Ram, R. Efficacy of retromandibular transparotid approach for the management of extracapsular subcondylar mandibular fractures using 2-mm titanium miniplates: a prospective clinical study. J Oral and Maxillofac Surg. 2016, 74, 1613–1621. [Google Scholar] [CrossRef]
- Nogami, S.; Takahashi, T.; Yamauchi, K.; et al. Clinical comparison between the retromandibular approach for reduction and fixation and endoscope-assisted open reduction and internal fixation for mandibular condyle fractures. J Craniofac Surg. 2012, 23, 1815–1818. [Google Scholar] [CrossRef]
- Chrcanovic, B. Surgical versus non-surgical treatment of mandibular condylar fractures: a meta-analysis. Int J Oral and Maxillofac Surg. 2015, 44, 158–179. [Google Scholar] [CrossRef] [PubMed]
- Haug, R.H.; Brandt, M. Traditional versus endoscope-assisted open reduction with rigid internal fixation (ORIF) of adult mandibular condyle fractures: a review of the literature regarding current thoughts on management. J Oral and Maxillofac Surg. 2004, 62, 1272–1279. [Google Scholar] [CrossRef]
- Bhutia, O.; Kumar, L.; Jose, A.; Roychoudhury, A.; Trikha, A. Evaluation of facial nerve following open reduction and internal fixation of Subcondylar fracture through retromandibular transparotid approach. Br J Oral and Maxillofac Surg. 2014, 52, 236–240. [Google Scholar] [CrossRef]
- Manisali, M.; Amin, M.; Aghabeigi, B.; Newman, L. Retromandibular approach to the mandibular condyle: a clinical and cadaveric study. Int J Oral and Maxillofac Surg. 2003, 32, 253–256. [Google Scholar] [CrossRef]
- Snyder, S.K.; Cunningham, L.L. The biology of open versus closed treatment of condylar fractures. Atlas Oral Maxillofac Surg Clin North Am. 2017, 25, 35–46. [Google Scholar] [CrossRef]
- Choi, K.-Y.; Yang, J.-D.; Chung, H.-Y.; Cho, B.-C. Current concepts in the mandibular condyle fracture management part II: open reduction versus closed reduction. Arch Plast Surg 2012, 39, 301. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.H. Comparison of computed tomography imaging before and after functional treatment of bilateralcondylar fractures in adults. Int J Oral and Maxillofac Surg. 1996, 25, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Sandler, N.A.; Andreasen, K.H.; Johns, F.R. The use of endoscopy in the management of Subcondylar fractures of the mandible: a cadaver study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999, 88, 529–531. [Google Scholar] [CrossRef] [PubMed]





© 2020 by the author. The Author(s) 2020.
Share and Cite
Sinha, A.; Natarajan, S. Comparative Evaluation of Clinical and Radiological Outcomes of Retromandibular Transparotid and Transoral Endoscopic-Assisted Approach for Surgical Management of Mandibular Subcondylar Fractures. Craniomaxillofac. Trauma Reconstr. 2021, 14, 90-99. https://doi.org/10.1177/1943387520949099
Sinha A, Natarajan S. Comparative Evaluation of Clinical and Radiological Outcomes of Retromandibular Transparotid and Transoral Endoscopic-Assisted Approach for Surgical Management of Mandibular Subcondylar Fractures. Craniomaxillofacial Trauma & Reconstruction. 2021; 14(2):90-99. https://doi.org/10.1177/1943387520949099
Chicago/Turabian StyleSinha, Ajit, and Srivalli Natarajan. 2021. "Comparative Evaluation of Clinical and Radiological Outcomes of Retromandibular Transparotid and Transoral Endoscopic-Assisted Approach for Surgical Management of Mandibular Subcondylar Fractures" Craniomaxillofacial Trauma & Reconstruction 14, no. 2: 90-99. https://doi.org/10.1177/1943387520949099
APA StyleSinha, A., & Natarajan, S. (2021). Comparative Evaluation of Clinical and Radiological Outcomes of Retromandibular Transparotid and Transoral Endoscopic-Assisted Approach for Surgical Management of Mandibular Subcondylar Fractures. Craniomaxillofacial Trauma & Reconstruction, 14(2), 90-99. https://doi.org/10.1177/1943387520949099



