Abstract
Study Design: This article was a technical note. Objective: To demonstrate the utilization of virtual surgical planning for surgical splint (VSPSS) fabrication. The VSPSS was used as an intraoperative assisting and guiding tool for reduction and/or fixation of treatment of comminuted maxillomandibular fractures. Methods: The presented technical note showed the fabrication process that began with data acquisition and presurgical planning using virtual surgical planning (VSP). The VSPSS was designed and fabricated after the fractures were reduced digitally in VSP. In the operating room, the VSPSS was seated to guide reduction and/or allow satisfactory fixation in three different situations. Results: Postoperative radiographs showed an acceptable reduction of the fractures. All patients had stable and repeatable occlusion postoperatively. Conclusions: The VSPSS is a feasible tool for surgeons to assist in the comminuted maxillomandibular fracture management, decrease operating time, and improve fracture stability.
Introduction
Comminuted facial fractures are common in maxillofacial trauma and generally caused by impact from high-energy mechanisms, for example, caused by motor vehicle collisions (MVCs) and gunshot wounds. Maxillary fractures reported 20%,[1] and mandibular fractures reported 5% to 7%[2] as being comminuted. Most of them are difficult to treat and still remain a challenge for surgeons due to the variability of fragmentation. Reduction and stabilization of these fractures are also delicate. Treatment modalities of comminuted maxillary and mandibular fractures include closed reduction, and open reduction and internal fixation (ORIF) using plates/and or screws. ORIF came into general use in comminuted fracture treatment because it minimizes sequestrum formation and allows postoperative function at the same time. However, not all comminuted fractures are amenable to this treatment, closed reduction techniques preferred in some cases such as severe fragmentation and soft tissue disruption (Figure 1).[2,3,4]
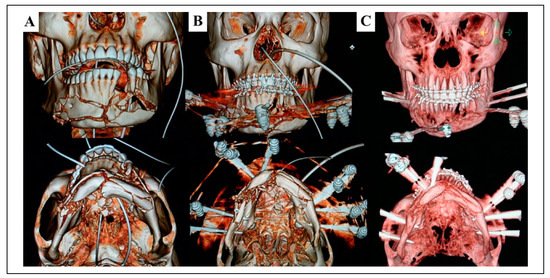
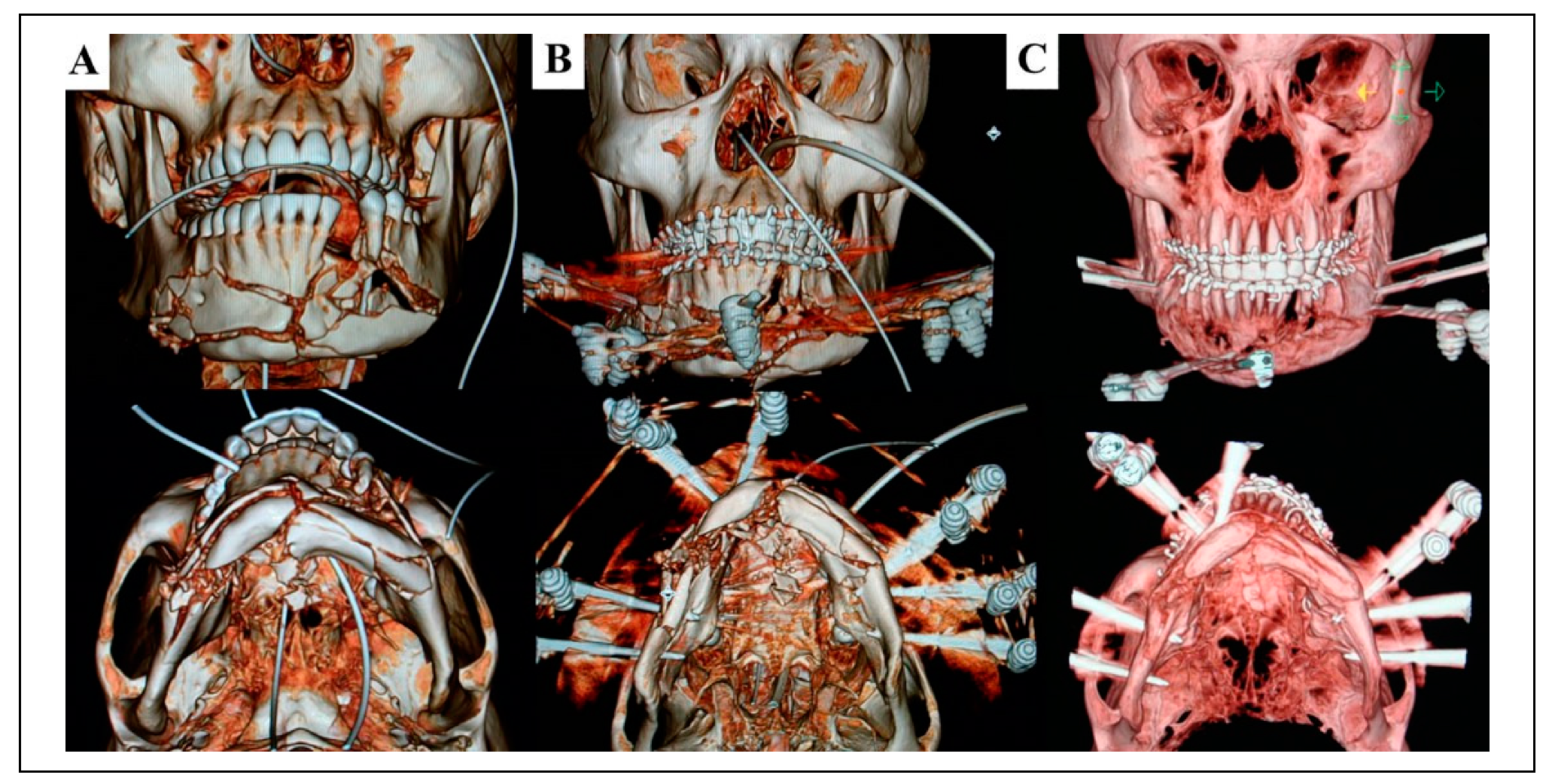
Figure 1.
3DCT showed comminuted mandibular fractures treated with closed reduction using MMF and external pin fixation. (A) Multiple bone fragmentation. (B) MMF and external pin fixation used for reduction and stabilization of the segments. (C) Three-month postoperative 3DCT showed acceptable bone alignment and healing. MMF indicates maxillomandibular fixation; 3DCT, three-dimensional computed tomography.
Surgical splints are fabricated to establish proper preinjury occlusion in managing jaw fractures in the following situations: edentulous or missing a significant number of teeth; fracture in the child with deciduous dentition; severely displaced and comminuted fractures of the palate, maxilla, or mandible that are difficult to obtain and maintain bony reduction. These splints assist in the anatomical reduction of bony segments, immobilize and maintain the reduction before or during maxillomandibular fixation (MMF) or ORIF application, and act as stabilization during bone healing period.[5,6,7] Traditionally, when we consider splint for treatment of maxillomandibular fractures, an impression will be taken of the upper and lower jaws. After pouring the impression, the models will be sectioned at the fracture sites, reduced, and waxed together in the ideal position. This technique will not allow surgeons to review the alignment of the reduced jaw fractures because only portions of dentoalveolar fractures are registered and speculated for the previous patient’s occlusion. Then splints will be fabricated on the reduced models.[5,6,7,8]
Recently, virtual or computer-aided surgery has evolved over time and gained popularity in craniomaxillofacial surgery: craniofacial reconstruction, orbital reconstruction, tumor resection, maxillomandibular reconstruction, orthognathic surgery, dental/craniofacial implant, traumatology, temporoman-dibular joint surgery, and others.[9,10,11,12,13,14,15,16] The main advantages of this computer technology are the possibilities for preoperative planning, improvement in precision with predicted outcome, reduction in surgical time, and better patient satisfaction than conventional methods.[10,11,12,13,14,15,16,17,18] The use of virtual surgery for the treatment of maxillary and mandibular fractures commonly involve presurgical planning and three-dimensional (3D) printing, contour model/surgical guide for cutting or drilling/Gunning splint/occlusal splint/plate or mesh, and fabrication for its use in surgical procedures.[12,14,16,17,19,20,21,22,23,24,25,26,27]
To our knowledge, there are no published reports describing the use of virtual surgery and surgical splint-assisted reduction and fixation for treatment of comminuted maxillomandibular fractures. The purpose of this present study is to demonstrate the utilization of virtual surgical planning for surgical splint (VSPSS) fabrication in comminuted maxillomandibular fractures to eliminate the need for impression and model surgery. Then the VSPSS is used as an intraoperative assisting and guiding tool to alleviate the level of a complex jaw fractures and aid in reduction and/or fixation.
Methods
Data Acquisition and Presurgical Planning
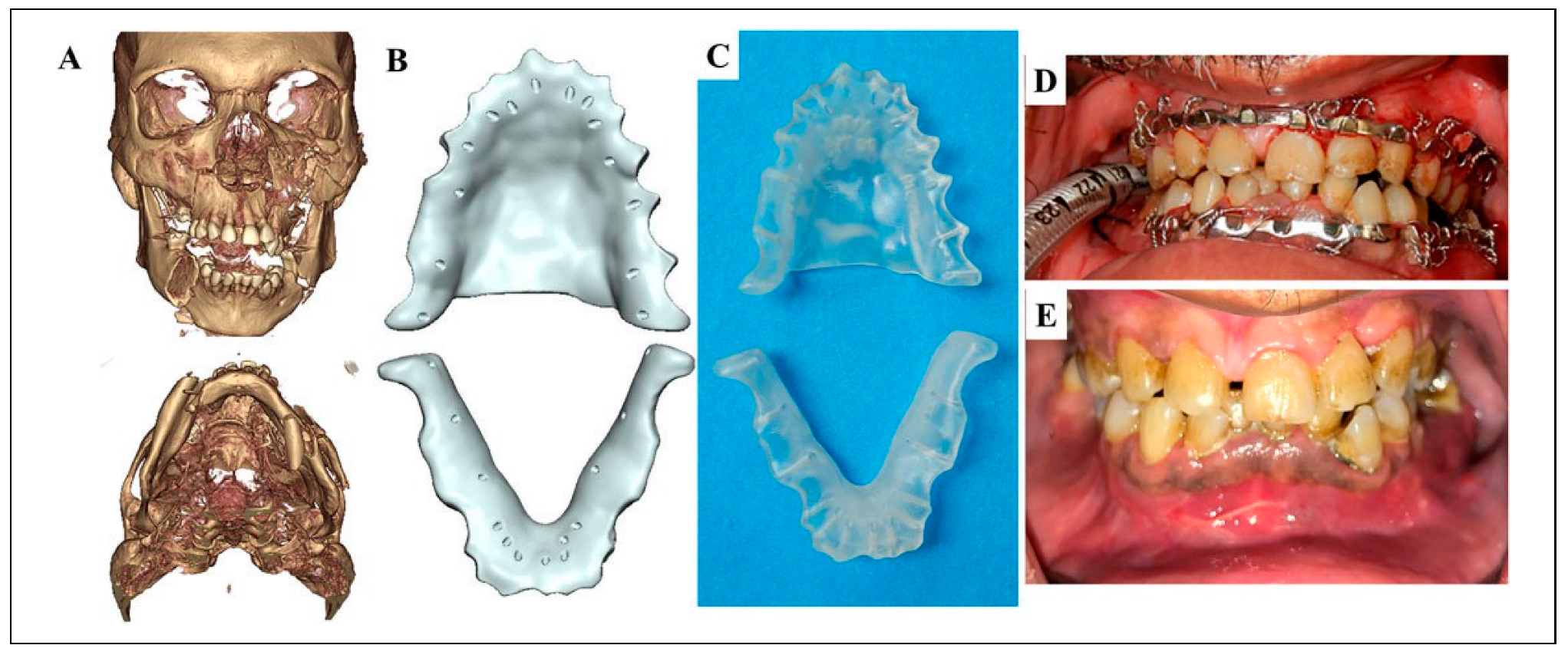
All patients received a medical computed tomography (CT) scan (slice thickness of 1 mm) of the craniofacial area. After the oral and maxillofacial surgery service was consulted, we completed the patient evaluation and generated the treatment plan. If a surgical splint was the treatment of choice, the images were processed as a data file in the Digital Imaging and Communication in Medicine (DICOM) format and submitted to a commercial vendor for virtual surgical planning (VSP) using the IPS CaseDesigner Software (KLS Martin group, Jacksonville, Florida, USA). A web-based planning session between the oral and maxillofacial surgeons and the biomedical engineer from the modeling company was scheduled. During the live meeting, the fractured and displaced bony segments were moved and aligned virtually by an engineer guided by the surgeons. The maxillary and/or mandibular VSPSS were constructed and seated digitally after the virtual reduction had been completed and confirmed by surgeons. Surgeons designed the desired shape, thickness, and location of the splint holes in VSP (Figure 2). The VSPSS outline was below the height of contour of the teeth to prevent occlusal interferences and displacement of the surgical splint when circumdental wires were applied. The thickness was 2 to 3 mm for adequate strength. The 1.5-mm diameter holes were put at interdental area for passing interdental wires. The VSPSS was fabricated by utilizing 3D printing technology. The data of final designed VSPSS were exported as a stereolithography (STL) file to a 3D printer, and then the VSPSS was printed using a biocompatible resin. The material was added layer by layer until a perfect anatomical fit was created. The patient-specific VSPSS was shipped to the surgeons and available for use 3-5 days after the meeting.
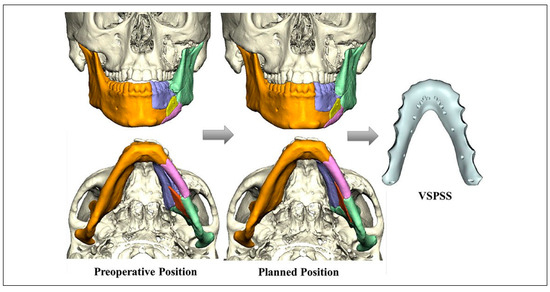
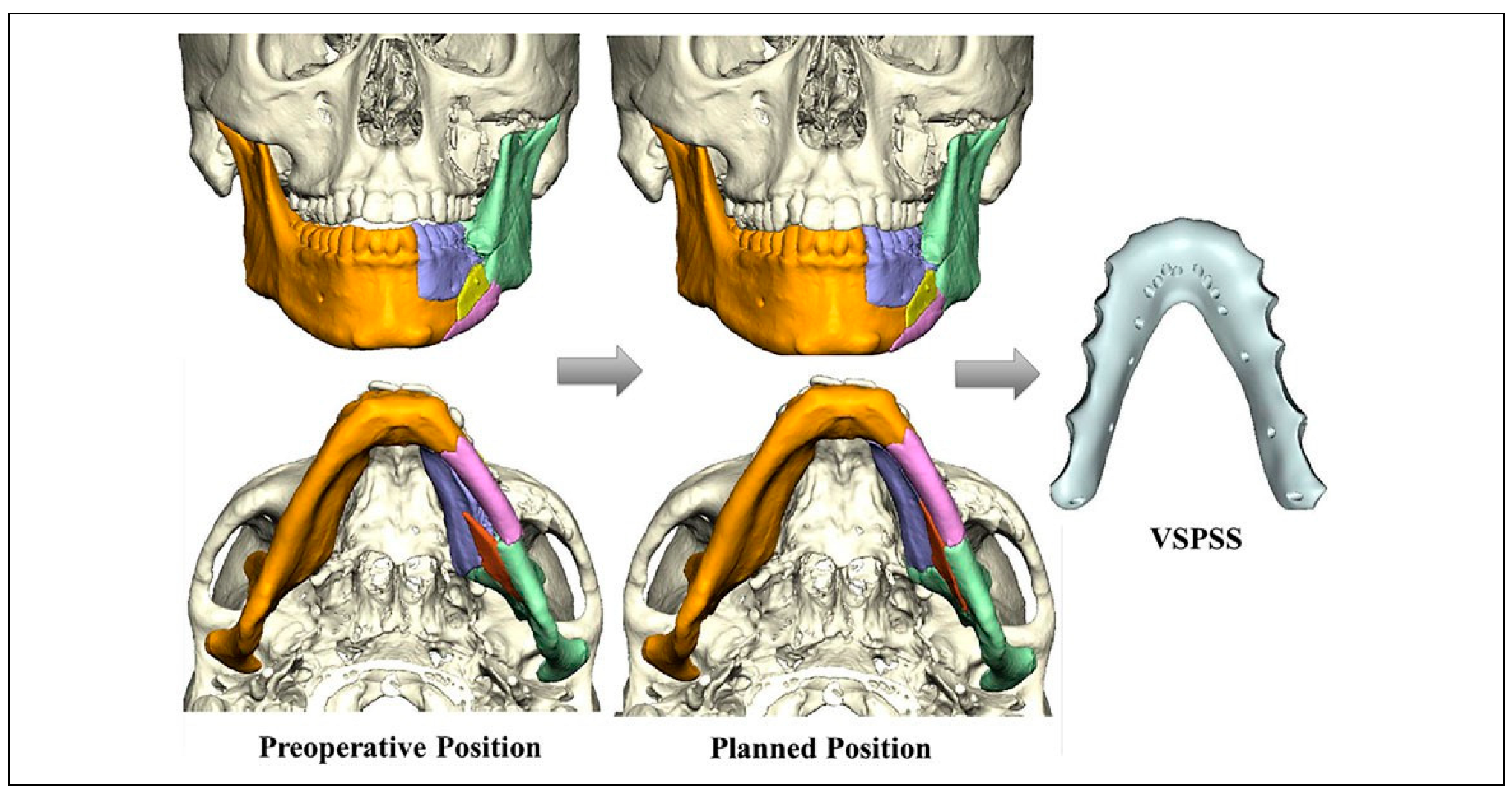
Figure 2.
VSP used for preoperative planning and virtual reduction of fractured segments to planned position, then the VSPSS was designed and prepared for fabrication. VSP indicates virtual surgical planning; VSPSS, virtual surgical planning for surgical splint.
Surgical Procedure
Episode 1: Work injury. A 23-year-old male presented after an excavator accident with comminuted left maxillary and mandibular fractures, teeth numbers 14, 15, and 19 were broken and involved the fractures. Due to the severely displaced and comminuted mandibular fracture combined with a minimally comminuted maxillary fracture (Figure 3A), the use of MMF for closed reduction alone was not sufficient so we decided to use the mandibular VSPSS for assisted reduction and stabilization. After the VSP web session and mandibular VSPSS fabrication were finished, the patient underwent repair of the comminuted fractures with closed reduction (Figure 3B to D). The mandibular VSPSS was seated into correct position with respect to the remaining teeth and secured with circumdental wires. Arch bar application was performed on both dental arches, then MMF was placed with stable occlusion and no complications. MMF was removed 2 weeks after surgery. Then, arch bars and VSPSS were removed 8 weeks after surgery (Figure 3E to H).
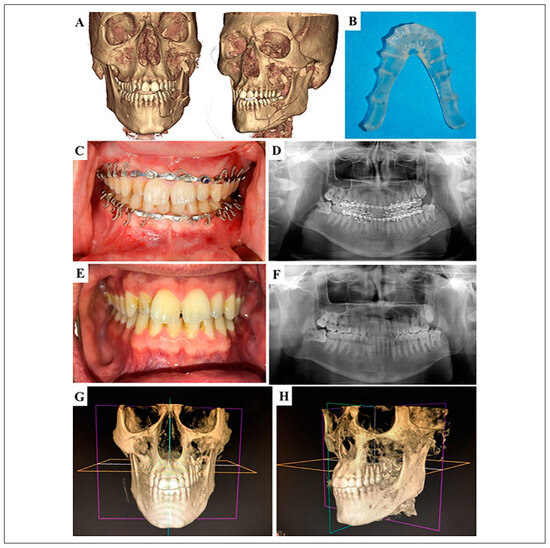
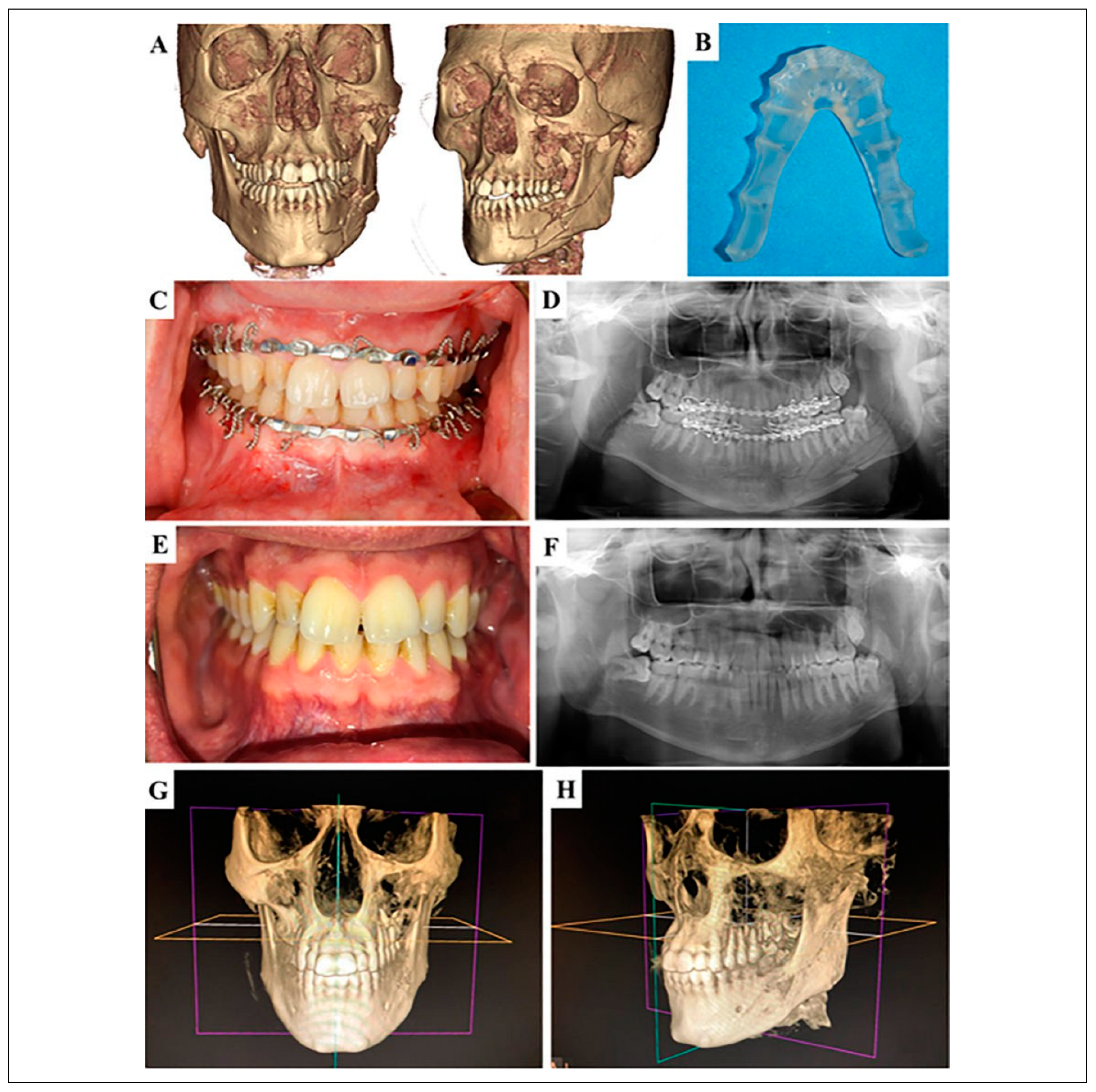
Figure 3.
(A) Preoperative 3DCT scan demonstrated comminuted fracture of left maxilla and mandible. (B) Mandibular VSPSS fabricated from virtual surgery. (C) Intraoperative occlusion after VSPSS and arch bars application. (Note: The mandibular VSPSS was placed at the lingual aspect of the mandible.) (D) Postoperative panoramic X-ray showed proper reduction of fractured segments. (E) Three-month postoperative occlusion showed maximum intercuspation and (F) the panoramic X-ray showed normal bone healing. (G) and (H) Six-month postoperative 3D-CBCT showed satisfactory bone alignment and healing. CBCT indicates cone-beam computed tomography; 3DCT, three-dimensional computed tomography; VSPSS, virtual surgical planning for surgical splint.
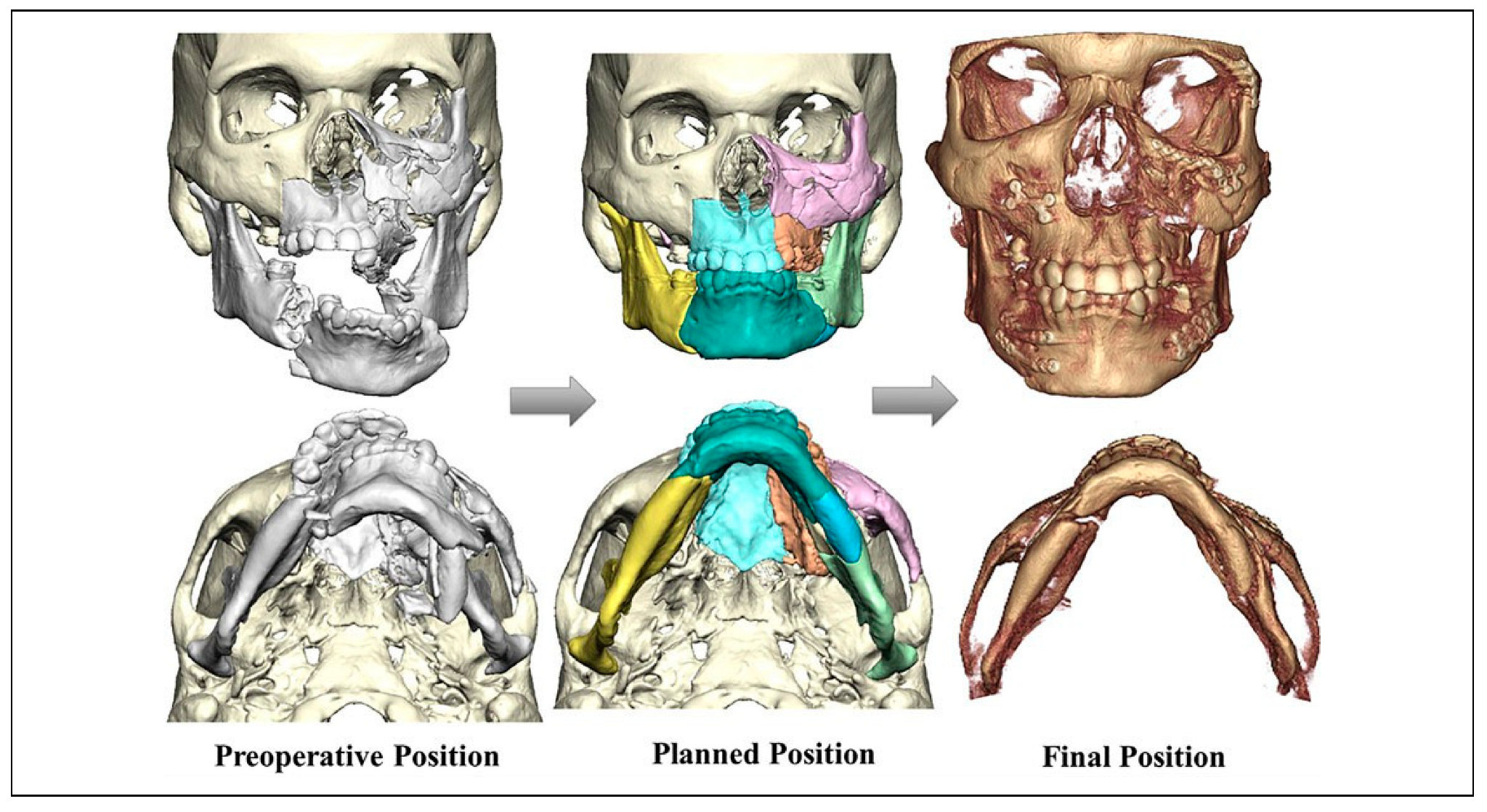
Episode 2: Gunshot wound. A 36-year-old male with a self-inflicted gunshot wound (SIGSW) to the submental region resulted in extensive soft tissue loss in the floor of the mouth, detachment of genioglossus muscle, multiple severely displaced and comminuted fractures of the maxilla and mandible, and poor remaining dentition (Figure 4A). Initially, the patient was taken to the operating room for tracheostomy, examination, wash out, and wound dressing. Then, VSP was used to plan the second surgery and fabricate the VSPSS. Because the patient had gross bone fragmentation and soft tissue disruption, surgical exposure for standard ORIF would have detached more vital soft tissue. Therefore, to minimize the risks of necrosis and nonunions conservative treatment was more amenable. There were not sufficient teeth between comminuted fracture segments to facilitate MMF, therefore skeletal wiring, and external pin fixation was planned in conjunction with VSPSS to provide a means of stable fixation in the mandible. External pin fixation was considered to maintain spatial relationships of mandibular segments that supplement bone and soft tissue healing. For the second surgery, the plan was to undergo closed reduction for comminuted fractures with VSPSS, skeletal wiring, and external pin fixation. Firstly, the mandibular VSPSS was placed and secured with circumdental and circummandibular wiring, respectively. Secondly, the maxillary VSPSS was used to reduce and stabilize the palate and maxillary fractures. This splint was secured with circumdental and bilateral circumzygomatic wiring, respectively. Finally, the external pin fixation was applied to control the severely unstable mandible (Figure 4B and C). All wounds were irrigated with copious normal saline mixing with bacitracin again, genioglossus muscle was resuspended with the mandibular VSPSS, then a pressure dressing was applied to the submental region. The skeletal and circumdental wires, maxillary and mandibular VSPSS, and external pin fixator were removed 3 months after surgery (Figure 4D and E).
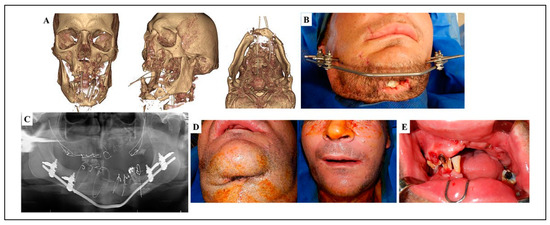
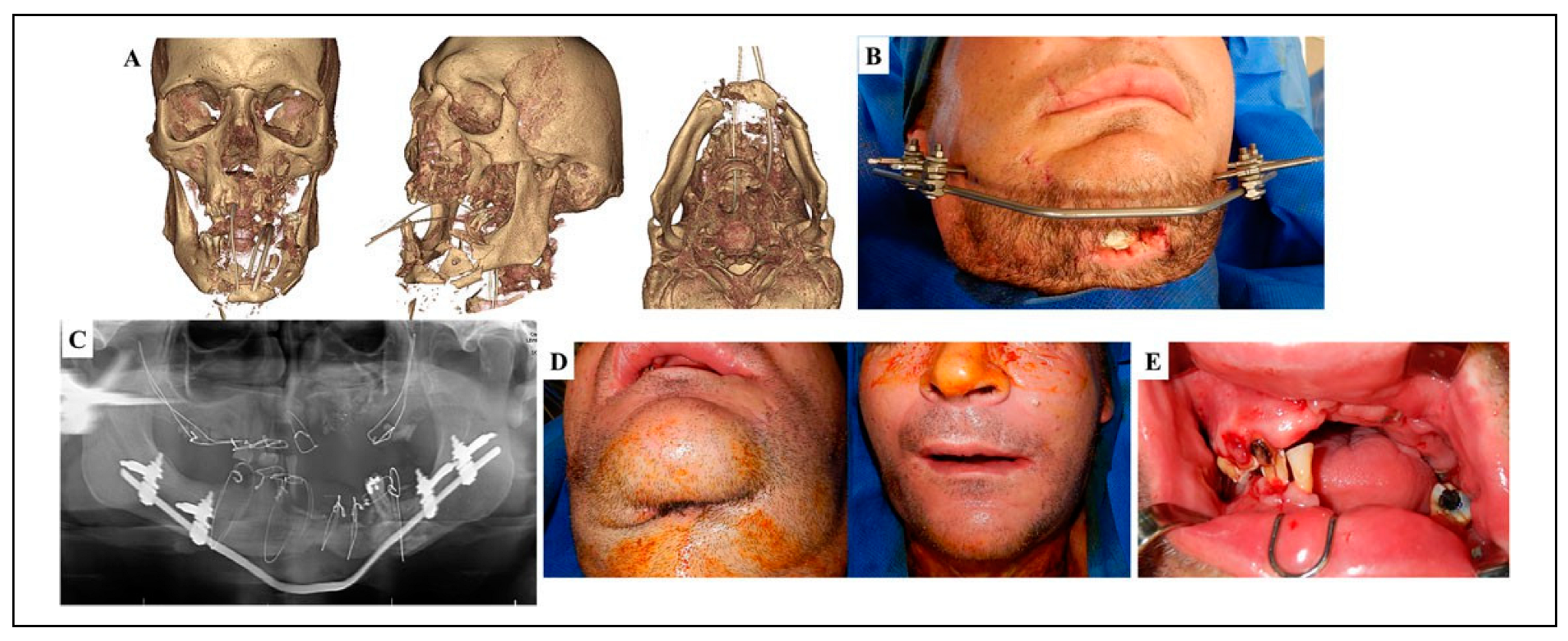
Figure 4.
(A) Preoperative 3DCT scan demonstrated grossly comminuted maxillary and mandibular fractures. Poor remaining dentition and unstable occlusion were also showed. (B) The external pin fixator was placed using a titanium bar and soft tissue injury at submental region from SIGSW. (C) Postoperative panoramic X-ray showed acceptable bone alignment. (D) Three-month after the surgery, the patient had a complete soft tissue closure at submental region and facial symmetry. (E) Three-month postoperative occlusion. 3DCT indicates three-dimensional computed tomography; SIGSW, self-inflicted gunshot wound.
Episode 3: Motor vehicle collision. A 53-year-old male presented with multiple injuries after MVC. Craniofacial CT scan demonstrated multiple facial fractures consisted of left zygomaticomaxillary complex fracture, left orbital floor fracture, nasal bone fracture, LeFort I fracture and comminuted fracture of left maxilla, and bilateral comminuted fractures of body of the mandible (Figure 5A). Because the patient had multiple facial fractures, ORIF was the preferred treatment to achieve form and function. VSP with fabrication of maxillary and mandibular VSPSS was chosen due to the severity of the comminution and the VSPSS ability to assist in reduction, reinforce the arch bar stability, and prevent segment displacement during application of plates and screws in this case (Figure 5B and C). After the patient was stable, the patient underwent closed reduction of the nasal bone fractures, ORIF assisted with maxillary and mandibular VSPSS for the maxilla and mandible, and ORIF with plates and screws for the other facial fractures. Surgery was started in the maxilla where the VSPSS was seated and secured with circumdental wires and then arch bars were placed. Next, the same procedure was performed on the mandible and MMF with occlusion was applied. Incisions in the buccal vestibule were made at the right and left body to expose the fracture sites. We found most of the segments were reduced with VSPSS properly, other segments were identified and reduced in an anatomical position. Two 2.0-mm miniplates and one 2.0-mm 3D plate with monocortical screws (KLS Martin group, Freiburg, Germany) were fixated at the right and left mandibular bodies, respectively. Then, attention was turned to the right maxilla, exposure and fixation with a 1.5-mm miniplate and monocortical screws was completed. Left zygomaticomaxillary complex fracture was treated with ORIF and a 1.5-mm miniplate and monocortical screws at left lateral orbital rim and infraorbital rim. Left orbital floor fracture was reconstructed with a biodegradable plate. MMF was removed to allow postoperative function. Arch bars and VSPSS were removed 8 weeks after the surgery (Figure 5D and E).
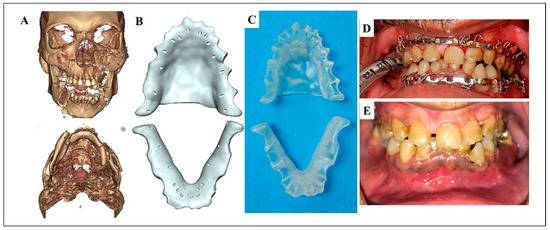
Figure 5.
(A) Preoperative 3DCT scan showing multiple facial fractures. (B) Maxillary and mandibular VSPSS designed by using VSP. (C) Maxillary and mandibular VSPSS fabricated from virtual surgery. (D) Intraoperative occlusion after VSPSS and arch bar application. (E) Three-month postoperative occlusion showed occlusal harmony. 3DCT indicates three-dimensional computed tomography; VSP virtual surgical planning; VSPSS, virtual surgical planning for surgical splint.
Results
All VSPSSs were seated satisfactorily. The postoperative recovery was uneventful. The cone-beam CT scan (CBCT) or panoramic radiograph was used to evaluate postoperatively. It showed a satisfied reduction of the fractures (Figure 6). All patients had stable and repeatable occlusion.
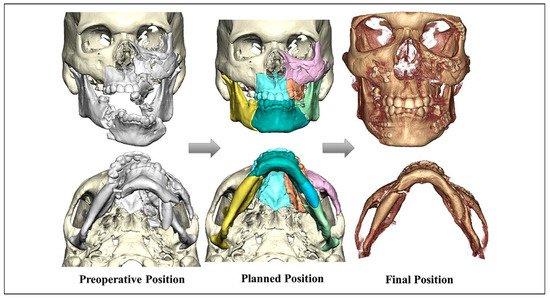
Figure 6.
Demonstrating satisfactory bony reduction after using VSPSS-assisted reduction and fixation. VSPSS indicates virtual surgical planning for surgical splint.
Discussion
Historically, surgical splints required an inconvenient and difficult procedure to take impressions of excessively mobilize fracture segments. Difficulties included dealing with soft tissue damage, management of endotracheal tubes, or patients with multiple injuries require care from multiple teams. This procedure occurred bedside, in the operating room, or dental unit.[5,7] Complications included more soft tissue injury or tooth loss from impression taking.
In addition, the time spent and technical skills required in dental model surgery and fabrication of splints caused traditional splints to be underutilized by surgeons in the management of jaw fractures. Currently, advances in diagnostic imaging, computer-aided design and computer-aided manufacturing (CAD/CAM), and digital technology has changed, the way presurgical planning can be accomplished. VSP has taken a more central role for oral and maxillofacial surgeons to improve treatment outcomes.[10,11,18] There are some studies showing the use of VSP to create occlusal splints,[19] Gunning splints,[23] and wing-splints[27] in treatment of mandibular fractures. This study reported the use of VSP to fabricate the VSPSS-assisted reduction and/or fixation. Wang et al.[23] stated that this technology can be an efficient and reliable method used to fabricate splints that are functionally similar to the conventional splints. Our study agreed with Wang et al.[23] in terms of VSPSS efficiency of fabrication and functionality. Using VSP and VSPSS, the surgeon can create the appropriate treatment plan without hindrance by patient pain, swelling, hemorrhage, or endotracheal intubation. Moreover, VSP and VSPSS help us to plan and reduce the fractured segments accurately, eliminate dental impression taking in the operating room, and reduce operating time.
To achieve optimal reduction and stabilization of facial fractures, one must carefully analyze many factors of a given case before selecting one of the many well-known techniques for repair. ORIF is a common treatment modality of facial fractures, but closed reduction continues to be used for treatment of maxillary and mandibular fractures under the appropriate circumstance. Management of facial fractures requires an individualized treatment plan for each patient and fracture type. Grossly comminuted fractures are a relative indication for closed reduction to avoid devitalizing the bone fragments.[2,3,4,8] This article reported patients with complex jaw fractures which challenged the manipulation and outcome of function and esthetic harmony. VSPSS was chosen to assist the complicated reduction and/or fixation either in patients with adequate or inadequate dentition. Cohen et al.[5] reported a satisfactory to excellent restoration of occlusion and no complications occurred as a direct result of the surgical splints.
The occlusion is the strategic key and goal to start guiding the reduction of comminuted fractures. Once occlusion is set and stabilized by fitting with VSPSS, alveolar bone and soft tissue around the teeth would be molded and conformed to the closer anatomical position by a closed reduction technique of VSPSS. Regarding VSPSS fabrication during a web-based planning session, the fractured and displaced bony segments are moved and aligned virtually to an appropriate anatomical reduction. With a virtual surgical plan, VSPSS is an extra tool to assist during operation. Although some small pieces of comminuted fractures are impossible to completely reduce, these could act as bone grafting with minimal devascularized subperiosteum comparing with the ones of an opened technique. These would allow to assist in reduction and fixation of the comminuted mandibular and maxillary fractures. VSPSS can be used alone or combined with other treatment methods when indicated.[5,6,8] It can reinforce the arch bar stability and prevent fracture segments rotation and distraction before and during application of arch bars and/or plates and screws.[5,6] Because of its ability in anatomical reduction assistance of fractures,[5,6,7] it is a tool that changes complex jaw fractures to less complicated fractures. Consequently, the effort needed for reduction is decreased, wide surgical exposure needed for ORIF is also decreased, and accuracy of the treatment is increased. Besides comminuted factures of maxilla and mandible, dentoalveolar fractures is also an indication for this splint.[6] It helps to bind all the teeth into a single unit, realign and firmly stabilize dentoalveolar segments. The VSPSS should be applied 4 to 6 weeks; however, individual surgeon could consider removing the surgical splint depending on fracture stability.[6,8] Even though the VSPSS seems to have several benefits for manipulation and reduction of maxillomandibular fractures, it could be a limitation if the bone and soft tissue discontinuity is too extensive. In this case, the composite flap could be considered.[2,26,28]
There are the other limitations of VSPSS use that should be considered. First, the amount of time required for virtual surgery and manufacturing of surgical splints may be an issue in treatment trauma patients. Nevertheless, it takes about 3 to 5 days to get the surgical splints in our practice, which is acceptable period for maxillary or mandibular fracture management.[3,29] At this time, patients start to have decreased swelling and are more clinically stable to undergo surgery. Second, there could be a steep learning curve between surgeons and biomedical engineers in term of design and fabrication of VSPSS. For example, the design of VSPSS boundaries could be similar to those of dentures. The hole location for passing wires should be simplified and used for surgeons. Regarding circumdental wire application, a 1.5-mm diameter hole should be placed in horizontal direction at interdental area. This would facilitate surgeon ability to pass a wire from either the buccal or lingual directions. This problem can be overcome with clear communication with the VSPSS design engineer.
Conclusion
The present study demonstrates a patient-specific VSP fabricated splint used to reduce, fixate, and stabilize the complex comminuted fractures of the maxilla and mandible. VSPSS is a feasible tool for surgeons to supplement their treatment of comminuted maxillomandibular fractures, decrease operating time, and improve fracture stability.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Acknowledgments
The authors thank Dr Cameron J. Walsh, Department of Oral and Maxillofacial Surgery, University of Alabama at Birmingham, who performed English proofreading.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
This study was approved by the University of Alabama at Birmingham Institutional Review Board (IRB-150219014).
References
- Patil, R.S.; Kale, T.P.; Kotrashetti, S.M.; Baliga, S.D.; Prabhu, N.; Issrani, R. Assessment of changing patterns of Le Fort fracture lines using computed tomography scan: an observational study. Acta Odontol Scand. 2014, 72, 984–988. [Google Scholar]
- Alpert, B.; Tiwana, P.S.; Kushner, G.M. Management of comminuted fractures of the mandible. Oral Maxillofac Surg Clin North Am. 2009, 21, 185–192. [Google Scholar] [PubMed]
- Gentile, M.A.; Tellington, A.J.; Burke, W.J.; Jaskolka, M.S. Management of midface maxillofacial trauma. Atlas Oral Maxillofac Surg Clin North Am. 2013, 21, 69–95. [Google Scholar]
- Ellis, E., 3rd; Muniz, O.; Anand, K. Treatment considerations for comminuted mandibular fractures. J Oral Maxillofac Surg. 2003, 61, 861–870. [Google Scholar] [PubMed]
- Cohen, S.R.; Leonard, D.K.; Markowitz, B.L.; Manson, P.N. Acrylic splints for dental alignment in complex facial injuries. Ann Plast Surg. 1993, 31, 406–412. [Google Scholar] [PubMed]
- Chidyllo, S.A.; Jacobs, J.S. Applications of dental splints with regard to modern techniques of rigid fixation. J Craniofac Surg. 1994, 5, 136–141. [Google Scholar] [CrossRef]
- Konas, E.; Tuncbilek, G.; Kayikcioglu, A.; Akcan, C.A.; Kocadereli, I.; Mavili, M.E. Splint-assisted reduction of comminuted or complex maxillofacial fractures. J Craniofac Surg. 2011, 22, 1471–1475. [Google Scholar]
- Blitz, M.; Notarnicola, K. Closed reduction of the mandibular fracture. Atlas Oral Maxillofac Surg Clin North Am. 2009, 17, 1–13. [Google Scholar]
- Bell, R.B. Computer planning and intraoperative navigation in cranio-maxillofacial surgery. Oral Maxillofac Surg Clin North Am. 2010, 22, 135–156. [Google Scholar]
- Louvrier, A.; Marty, P.; Barrabe, A.; et al. How useful is 3D printing in maxillofacial surgery? J Stomatol Oral Maxillofac Surg. 2017, 118, 206–212. [Google Scholar]
- Jacobs, C.A.; Lin, A.Y. A new classification of three-dimensional printing technologies: systematic review of three-dimensional printing for patient-specific craniomaxillofacial surgery. Plast Reconstr Surg. 2017, 139, 1211–1220. [Google Scholar] [PubMed]
- Levine, J.P.; Patel, A.; Saadeh, P.B.; Hirsch, D.L. Computer-aided design and manufacturing in craniomaxillofacial surgery: the new state of the art. J Craniofac Surg. 2012, 23, 288–293. [Google Scholar] [CrossRef]
- Gelesko, S.; Markiewicz, M.R.; Bell, R.B. Responsible and prudent imaging in the diagnosis and management of facial fractures. Oral Maxillofac Surg Clin North Am. 2013, 25, 545–560. [Google Scholar] [CrossRef]
- Castro-Núñez, J.; Shelton, J.M.; Snyder, S.; Sickels, J.V. Virtual surgical planning for the management of severe atrophic mandible fractures. Craniomaxillofac Trauma Reconstr. 2018, 11, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Morrison, C.S.; Taylor, H.O.; Collins, S.; Oyelese, A.; Sullivan, S.R. Use of intraoperative computed tomography in complex craniofacial trauma: an example of on-table change in management. Craniomaxillofac Trauma Reconstr. 2014, 7, 298–301. [Google Scholar] [CrossRef] [PubMed]
- Thor, A. Preoperative planning of virtual osteotomies followed by fabrication of patient specific reconstruction plate for secondary correction and fixation of displaced bilateral mandibular body fracture. Craniomaxillofac Trauma Reconstr. 2016, 9, 188–194. [Google Scholar] [CrossRef]
- Li, P.; Tang, W.; Liao, C.H.; Tan, P.Y.; Zhang, J.K.; Tian, W.D. Clinical evaluation of computer-assisted surgical technique in the treatment of comminuted mandibular fractures. J Oral Maxillofac Surg Med Pathol. 2015, 27, 332–336. [Google Scholar]
- Martelli, N.; Serrano, C.; van den Brink, H. , et al. Advantages and disadvantages of 3-dimensional printing in surgery: a systematic review. Surgery. 2016, 159, 1485–1500. [Google Scholar] [CrossRef]
- Tepper, O.M.; Sorice, S.; Hershman, G.N.; Saadeh, P.; Levine, J.P.; Hirsch, D. Use of virtual 3-dimensional surgery in post-traumatic craniomaxillofacial reconstruction. J Oral Maxillofac Surg. 2011, 69, 733–741. [Google Scholar]
- Wagner, J.D.; Baack, B.; Brown, G.A.; Kelly, J. Rapid 3-dimensional prototyping for surgical repair of maxillofacial fractures: a technical note. J Oral Maxillofac Surg. 2004, 62, 898–901. [Google Scholar] [CrossRef]
- Kokosis, G.; Davidson, E.H.; Pedreira, R.; Macmillan, A.; Dorafshar, A.H. The use of computer-aided design and manufacturing in acute mandibular trauma reconstruction. J Oral Maxillofac Surg. 2018, 76, 1036–1043. [Google Scholar] [PubMed]
- Sinha, P.; Skolnick, G.; Patel, K.B.; Branham, G.H.; Chi, J.J. A 3-dimensional-printed short-segment template prototype for mandibular fracture repair. JAMA Facial Plast Surg. 2018, 20, 373–380. [Google Scholar] [PubMed]
- Wang, H.D.; Frost, C.; Cusano, A.; Dorafshar, A.H. Management of bilateral edentulous mandible fractures through an intraoral approach using CAD/CAM technology: a case report. J Oral Maxillofac Surg. 2018, 76, e1–e1056. [Google Scholar]
- Ma, J.L.; Ma, L.M.; Wang, Z.F.; Zhu, X.J.; Wang, W.J. The use of 3D-printed titanium mesh tray in treating complex comminuted mandibular fractures: a case report. Medicine (Baltimore). 2017, 96, 1–5. [Google Scholar]
- el-Gengehi, M.; Seif, S.A. Evaluation of the accuracy of computer-guided mandibular fracture reduction. J Craniofac Surg. 2015, 26, 1587–1591. [Google Scholar]
- Khatib, B.; Cuddy, K.; Cheng, A.; et al. Functional anatomic computer engineered surgery protocol for the management of self-inflicted gunshot wounds to the maxillofacial skeleton. J Oral Maxillofac Surg. 2018, 76, 580–594. [Google Scholar]
- Lee, J.-W.; Choi, B.-J.; Nam, O.-H.; Kwon, Y.-D. Minimal invasive treatment using patient-specific template for mandibular fractures in children: “Wing-splint” by CAD/CAM technology. Br J Oral Maxillofac Surg. 2016, 54, 1140–1141. [Google Scholar]
- Peleg, M.; Sawatari, Y. Management of gunshot wounds to the mandible. J Craniofac Surg. 2010, 21, 1252–1256. [Google Scholar]
- Meara, D.J.; Jones, L.C. Controversies in maxillofacial trauma. Oral Maxillofac Surg Clin North Am. 2017, 29, 391–399. [Google Scholar]
© 2020 by the authors. The Authors 2020.