Despite being the largest and strongest bone of the facial skeleton, its protrusion makes mandible the most vulnerable to fractures. [
1] Its susceptibility to trauma can easily be analyzed by studies put forth by different authors. [
2] Mandibular fractures have been found to occupy a significant percentage of all maxillofacial injuries, as studies put forth by Gassner et al. and Tanaka et al. observed that mandibular fractures account for 24.3 and 68.6% of maxillofacial trauma, respectively. [
3,
4] Biomechanical properties of the mandible, position during injury, overlying soft tissue, force properties (direction, intensity, location of point, and impact), and the teeth present are some of the range of factors, which decide the pattern of mandibular condyle and angle fractures. [
2]. The most common sites of fracture of the mandible are condyle (29.1%), angle (24.5%), symphysis (22%), and body (16%). However, there is a broad variation seen in how these findings translate in different researches because statistics put forth by Ogundare et al. suggested angle fractures to have the highest incidence at 36%. [
5] Meisami et al. provided statistics to prove that condylar and angle fractures have almost equal weightage in sites of mandible (25–33%). [
6]
However, clinical data have suggested a decreased incidence of condylar fractures in cases with present M3, concluding that when the fragility of the angle increases, the condyle is spared.
In contrast, recent studies have proven increased likelihood of condyle fractures in the absence of impacted mandibular third molars or a completely erupted one. However, the absence also tends to decrease the frequency of angle fractures. The segment where the ramus of the mandible meets the condyle is responsible for indirectly transmitting impact forces toward the condyle due to the difference in rigidity, which is higher in the ramus as compared with condyle.
In our study, an effort has been made to prove and draw conclusions from the hypothesis of the relationship between third molar and angle and condylar fractures of the mandible using variables such as type of impaction, severity of impaction, injury mechanism, position of third molar, and the root development.
Materials and Methods
A retrospective study was conducted on 280 patients who were treated for mandibular angle and condyle fractures in our Craniofacial Unit from 2010 to 2017. Research ethics committee approved the study.
Records and panoramic radiographs of all patients treated for mandibular condylar and angular fractures were analyzed and a correlation was established based on the following:
Distribution of mandibular fractures (angle and condyle) by gender and age.
Relationship between the presence of mandibular third molars and mandibular angle and condyle fractures.
Relationship between mandibular third molar position and mandibular angle and condyle fractures.
Relationship between angulation of mandibular third molars and mandibular angle and condyle fractures.
Relationship between the root development of mandibular third molars and mandibular angle and .condyle fractures.
The inclusion criteria for angle fractures involved (1) patients who had sustained isolated unilateral angle fractures, (2) patients whose complete information was available, and (3) cases which helped evaluate the influence of the presence and position of a mandibular third molar in mandibular angle fracture. The exclusion criteria involved (1) patients whose information was incomplete, (2) cases that reported fractures during third molar extractions, (3) cases that reported fractures during orthognathic surgeries due to bad splits involving third molars, (4) pathological fractures due to lesions involving third molars, and (5) patients with underlying bone metabolism disorders (osteopenia, osteoporosis).
The inclusion criteria for condyle fractures involved (1) patients who had sustained unilateral condyle fractures with or without associated concomitant mandibular fractures and (2) patients whose complete information was available. The exclusion criteria for condyle fractures involved (1) incomplete information, (2) presence of concomitant ankylosis of temporomandibular joint in condylar injuries, and (3) Condylar fractures previously treated surgically in other hospitals.
The primary predictor variable was presence/absence of impacted mandibular third molar. The secondary predictor variables taken into account were age and sex of patients followed by determination of impaction depth and eruption space of third molars using the classification system of Pell and Gregory.
The outcome variable was angle fracture or condyle fracture of mandible (presence or absence).
The statistical analysis was performed using SPSS Statistics software (SPSS Inc., Chicago, IL). Statistical significance was determined using the chi-squared tests.
Results
A total of 280 patients were considered for our retrospective study. The patients evaluated had been diagnosed with angle and condyle fractures and were admitted in our craniofacial unit for the treatment of the same.
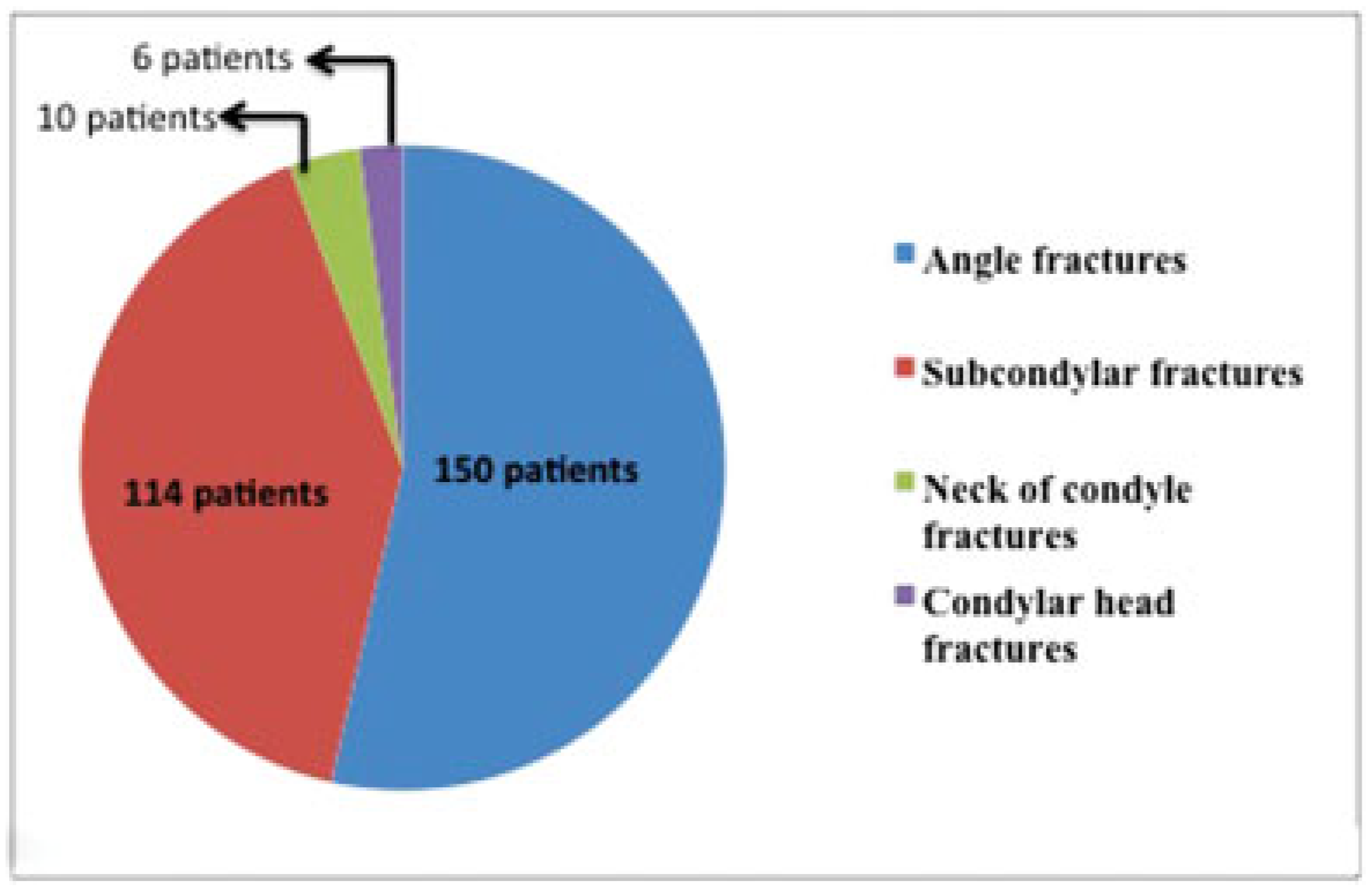
Of the total, 150 patients were of angle fractures occupying 53.6% of the sample set and 130 were of condyle fractures, constituting 46.4% of the sample (
Figure 1).
Subcondylar fractures accounted for 87.6% of the condyle fractures, whereas condylar head and neck fractures composed of 7.6 and 4.6%, respectively.
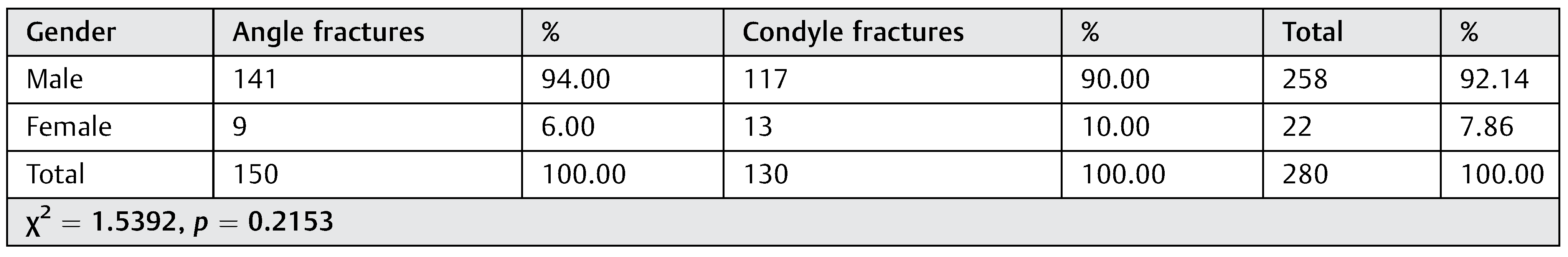
Gender and Distribution of Mandibular Angle and Condyle Fractures
Of the total, 141 male patients (94%) and 9 female patients (6%) were diagnosed with angle fracture of the mandible.
Of the condyle fractures, 117 were male patients (90%) and 13 were female patients (10%;
Figure 2,
Table 1). However, the
p-value was found to be statistically insignificant and this variable could not be used to establish a predilection of mandibular fractures based on the sex of the patients.
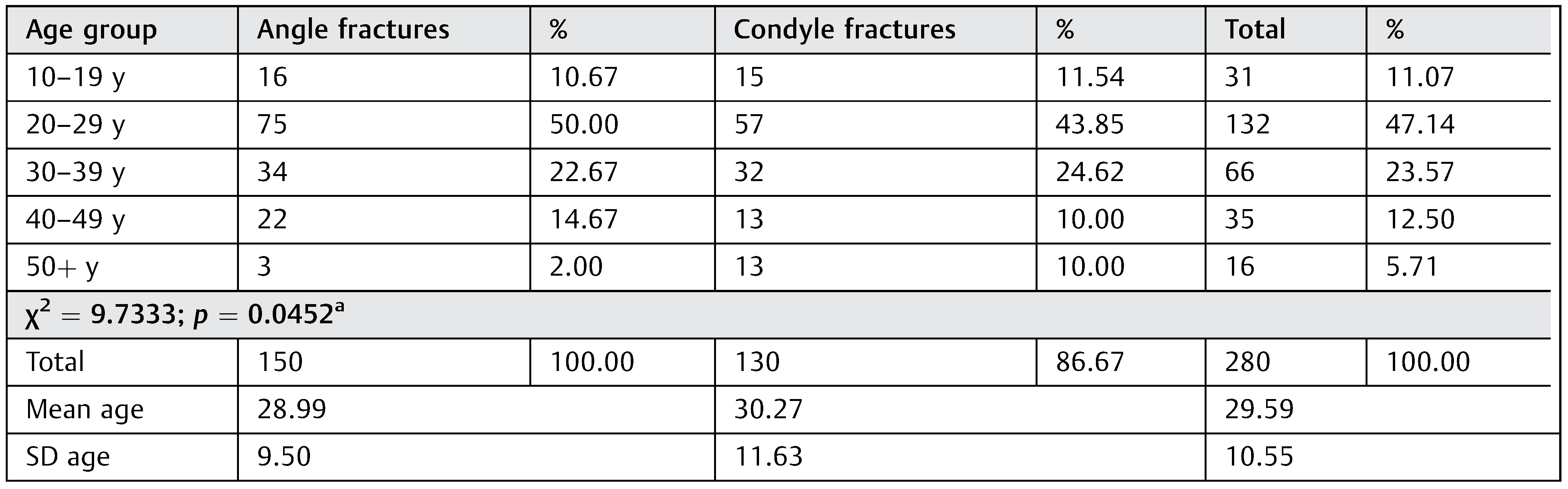
Age and Distribution of Mandibular Angle and Condyle Fractures
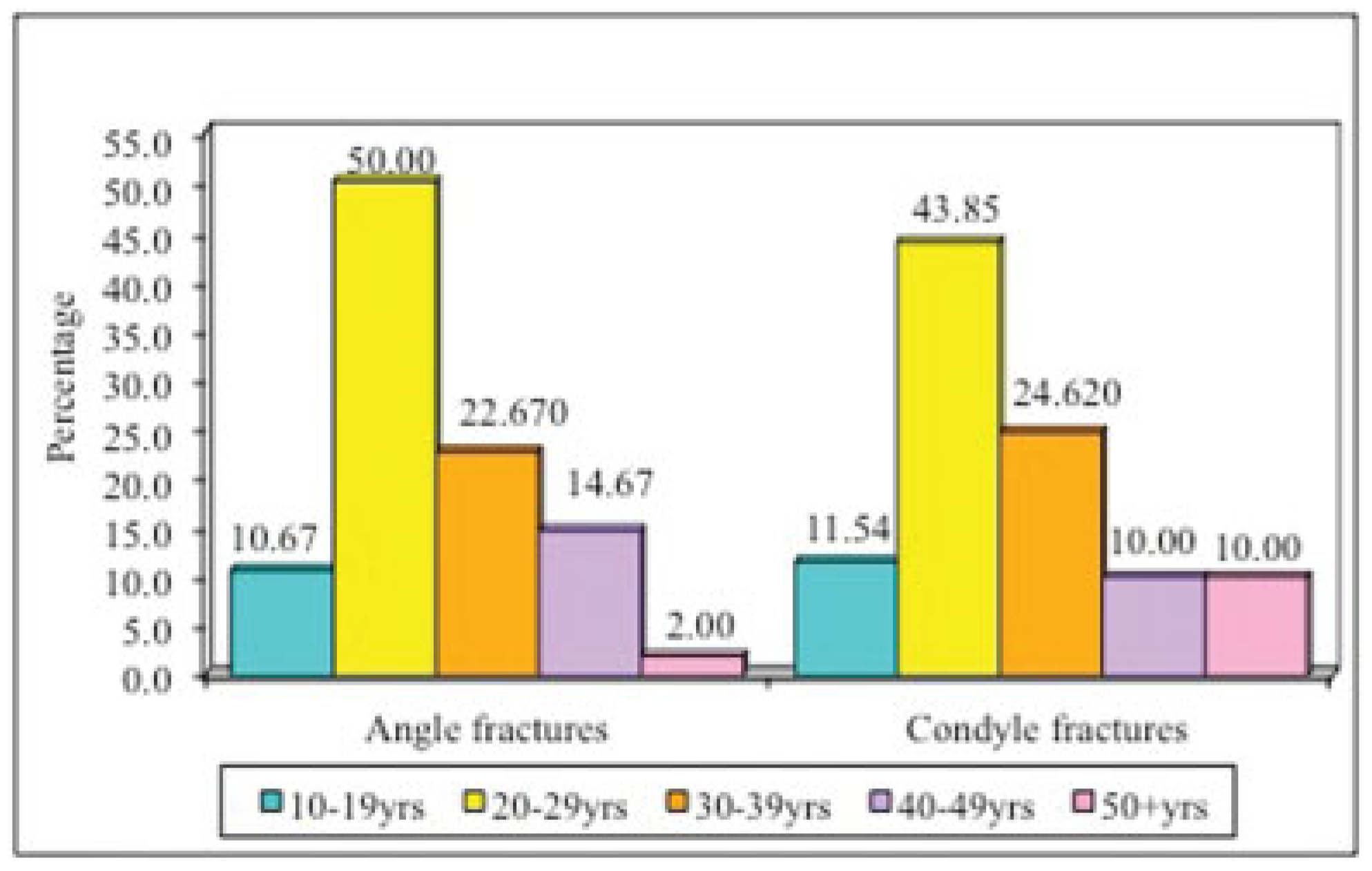
Among the angle fractures, the highest incidence was observed in patients 20 to 29 years age group (75 patients; 50%) followed by 30 to 39 years (34 patients; 22.67%), 40 to 49 years (22 patients; 14.67%), 10 to 19 years (16 patients; 10.67%), and older than 50 years age bracket (3 patients; 2%), respectively.
Among the condyle fractures, the highest incidence was observed in patients 20 to 29 years age group (57 patients; 43.85%) followed by 30 to 39 years (32 patients; 24.62%), 10 to 19 years (15 patients; 11.54%), 40 to 49 years (13 patients, 10%), and older than 50 years age bracket (13 patients, 10%), respectively.
The highest incidence for both the fractures was seen in 20 to 29 years age group and the mean ages calculated for both angle and condyle fractures were 28.99 and 30.27 years, respectively (
Figure 3;
Table 2).
Etiology or Cause of Fracture and Distribution of Mandibular Angle and Condyle Fractures
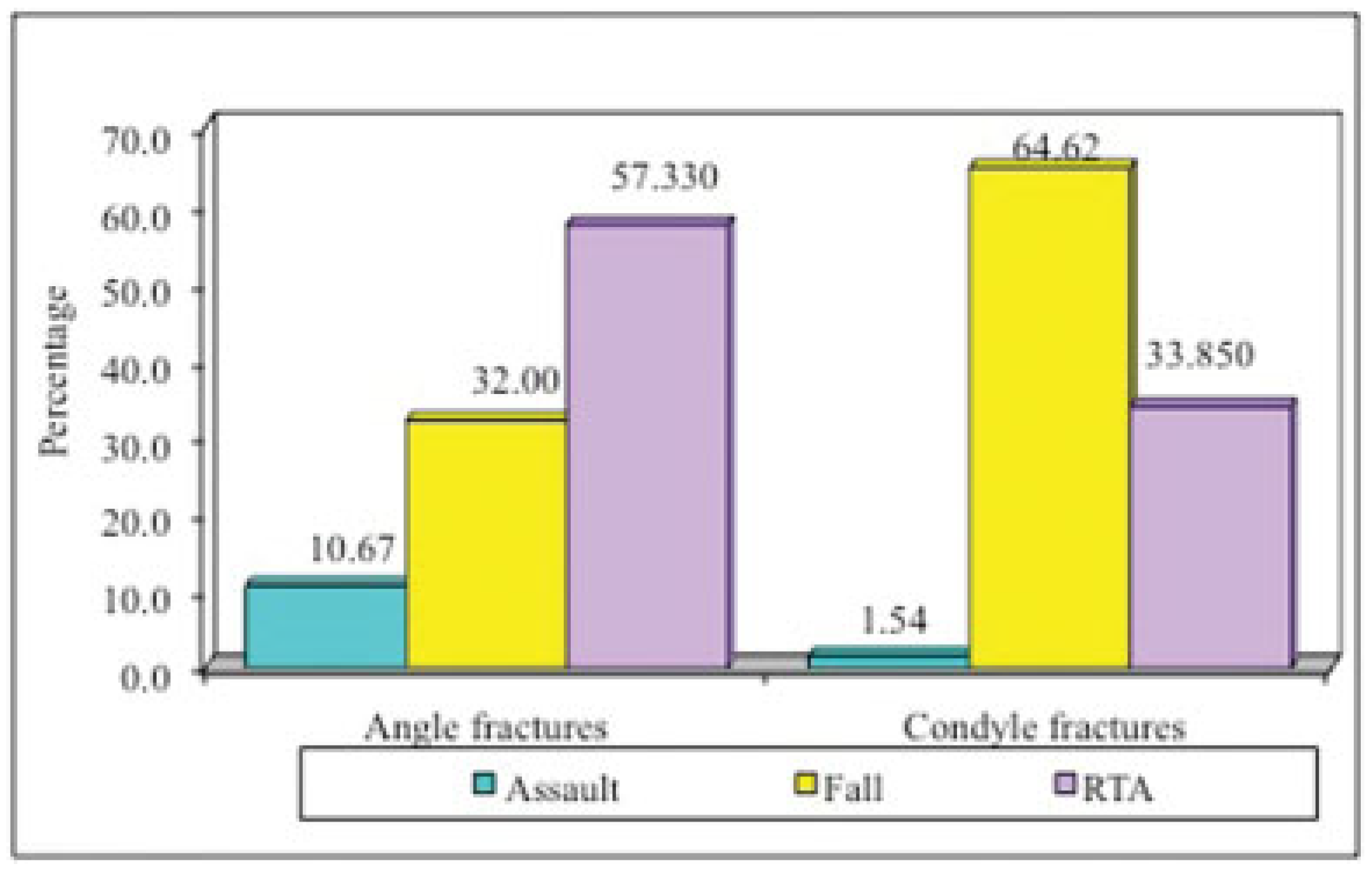
Among the angle fractures, road traffic accident had the highest incidence of etiology and was seen in 86 patients (57.33%). The other causes of trauma were fall and assault which were seen in 48 (32%) and 16 (10.67%) patients, respectively.
Among the condyle fractures, fall was the most common cause of fracture (84 patients; 64.62%). Road traffic accident (44 patients; 33.85%) was the second most common etiology followed by assault (2 patients; 1.54% [
Figure 4,
Table 3]).
Relationship between Presence and Absence of Mandibular Third Molar and Angle and Condyle Fractures
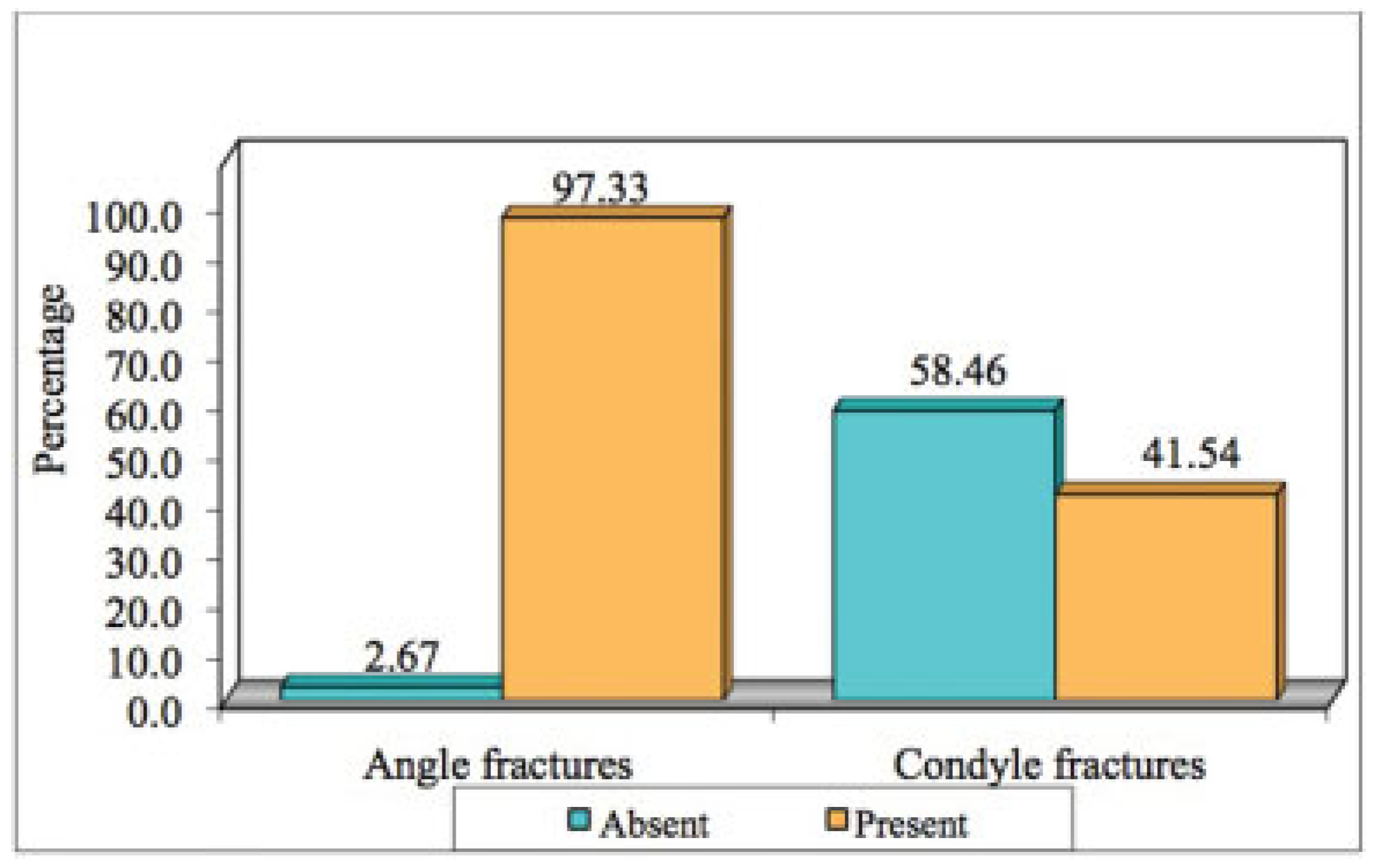
Of the mandibular angle fractures, 146 patients (97.33%) had mandibular third molars and 4 patients (2.67%) did not have third molars. The presence of a mandibular third molar in angle fractures was statistically and significantly higher than in patients who did not have them.
Of the condyle fractures, 76 patients (58.46%) had absence of mandibular third molars, whereas 54 patients (41.54%) had third molars. The absence of a mandibular third molar in condylar fractures was statistically and significantly higher than in patients where third molars were present (
Figure 5,
Figure 6,
Figure 7 and
Figure 8;
Table 4).
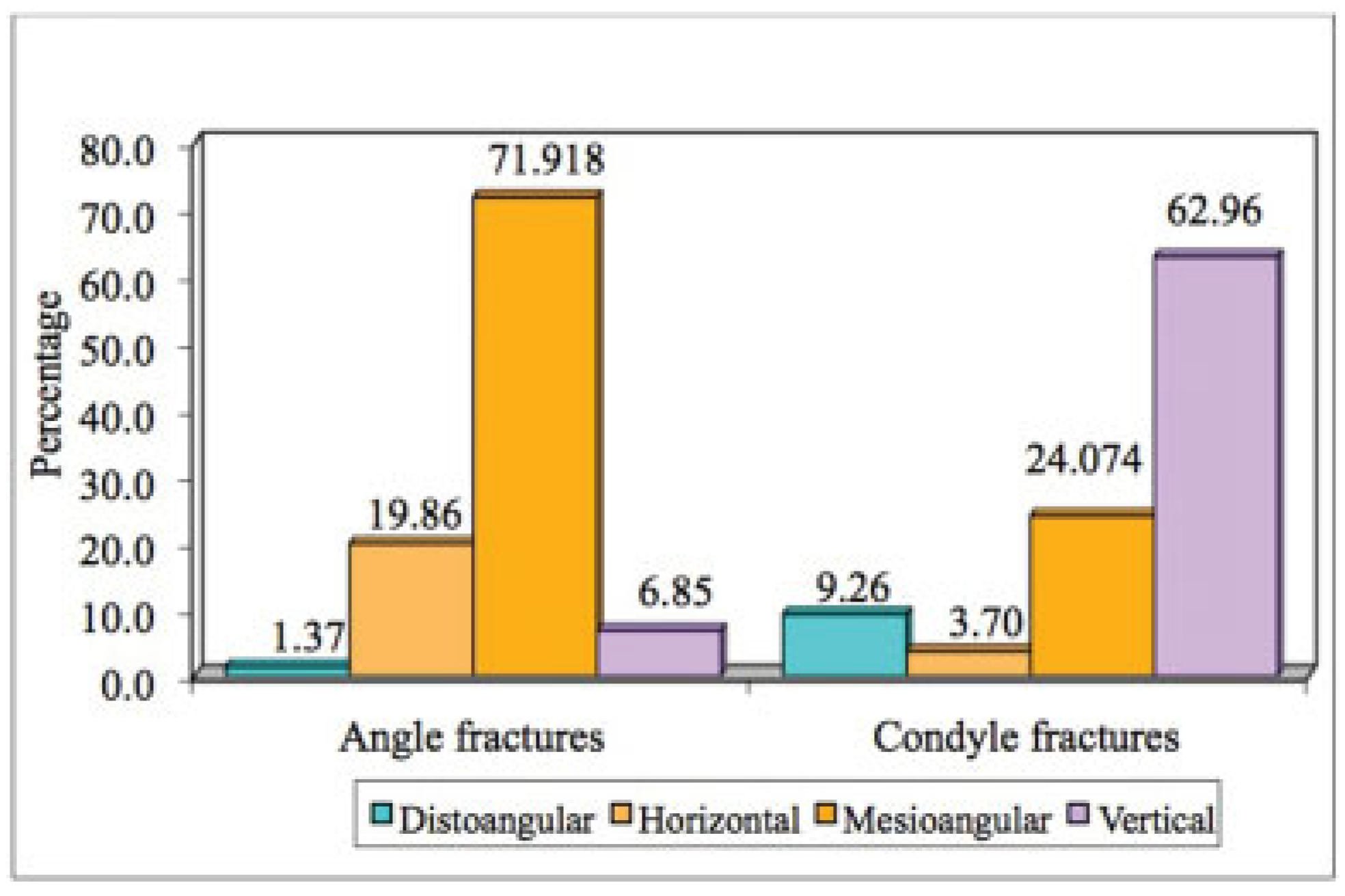
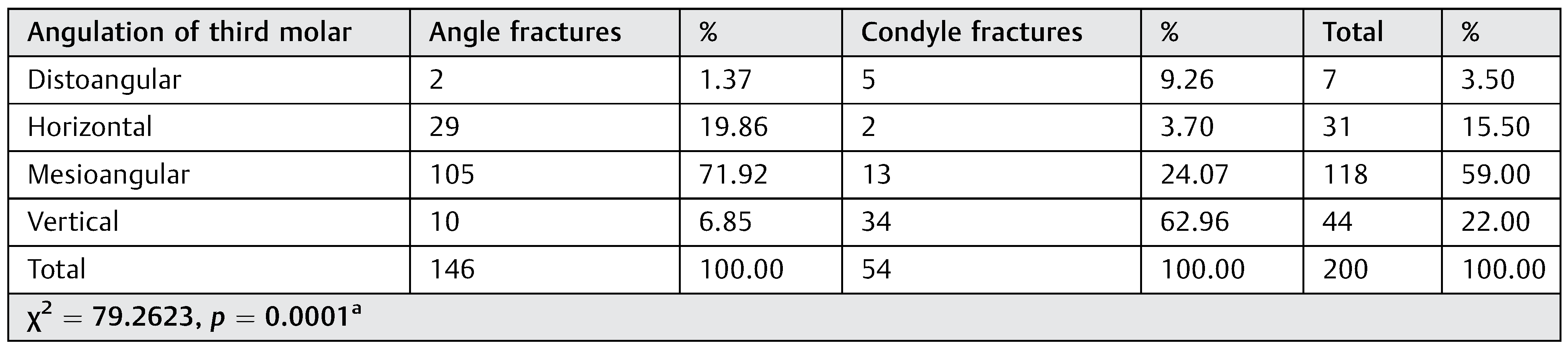
Relationship between Mandibular Third Molar Angulation and Mandibular Angle and Condyle Fractures
Of the 146 mandibular angle fracture patients who had a lower third molar, the highest incidence was seen in mesioangular angulation (105 patients; 71.92%) followed by horizontal angulation (29 patients; 19.86%), vertical angulation (10 patients; 6.85%), and distoangular angulation (2 patients; 1.37%), respectively.
Of the 54 mandibular condyle fracture patients, who had a lower third molar, the highest incidence was seen in vertical angulation (34 patients; 62.96%) followed by mesioangular angulation (13 patients; 24.07%), distoangular angulation (5 patients; 9.26%), and horizontal angulation (2 patients; 3.70% [
Figure 9,
Figure 10 and
Figure 11;
Table 5]), respectively.
Relationship between Mandibular Third Molar Position and Mandibular Angle and Condyle Fractures
Of the 146 mandibular angle fracture patients, who had a lower third molar, position with the highest incidence was seen in class II position B (94 patients; 64.38%) followed by class I position B (27 patients; 18.49%), class I position A (15 patients; 10.27%), class II position A (8 patients; 5.48%), class II position C (1 patient; 0.68%), and class III position B (1 patient; 0.68%), respectively.
Of the 54 mandibular condyle fracture patients, who had a lower third molar, position with highest incidence was seen in class I position A (48 patients; 88.89%) followed by class II position A (3 patients; 5.56%), class I position B (2 patients; 3.70%), and class II position B (1 patient; 1.85%), respectively (
Figure 12;
Table 6).
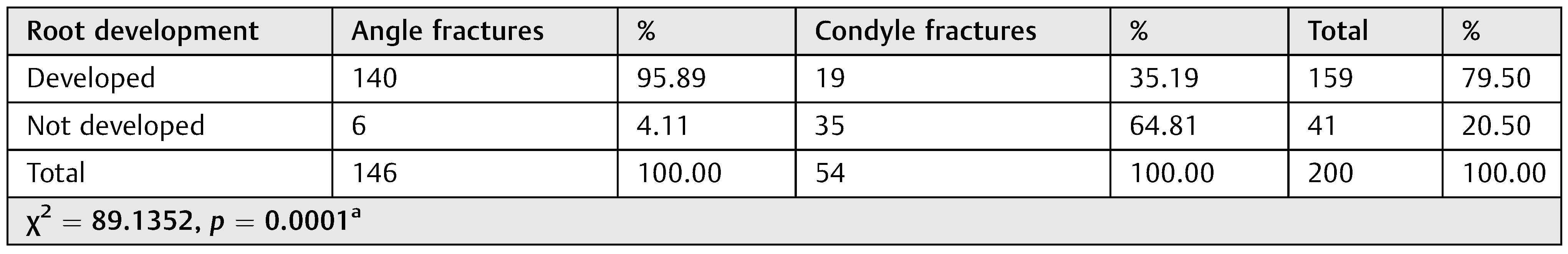
Relationship between Root Development of Mandibular Third Molar and Mandibular Angle and Condyle Fractures
Based on root development of the mandibular third molars, mandibular angle fractures were more frequent when the mandibular third molar had a developed root (140 patients; 95.89%). Mandibular condyle fractures were more frequent when roots were not yet completely developed (35 patients; 64.81% [
Figure 13 and
Figure 14;
Table 7]).
Discussion
A broad variation is seen in factors and variables governing mandibular angle and condyle fractures. Determinants such as direction, severity and impact of force, the presence of soft-tissue bulk, occlusal loading pattern, biomechanical characteristics such as bone density mass, and anatomic structures creating weak areas are accountable for mandibular fractures to occur. [
6,
10] Many studies have been put forth proving the increased risk of mandibular angle fractures due to the presence of an impacted third molar; however, there is scanty evidence and low emphasis on the distribution of angle and condyle fractures on the basis of age of the patient, sex, etiology of the trauma, presence and position of third molar, and development of roots. [
6,
11,
12]
In our study, gender of the patient was considered a variable, as all the patients who were operated from 2010 to 2017 were taken into consideration. However, as per statistics,
p-value was found to be 0.2153 (
p < 0.05), which was statistically insignificant, hence failing to establish a relationship between the sex of the patient and mandibular fractures. In many studies, male predilection has been seen over females for mandibular fractures. A similar male inclination was found in studies put forth by Busuito et al. (1986), Eriksson and Willmar (1987), Fridrich et al. (1992), Oji (1999), Ogundare et al., Sirimaharaj and Pyungtanasup (2008), and Bormann et al. (2009). [
5,
13] Majority of the fractures were found in men, mostly due to higher physical activity and their involvement in road traffic accidents. However, studies performed by Barde et al. and Subhasharaj et al. (2008) revealed a male:female ratio of 3.7:1 and 5.1:1, respectively, proving an increase in the trend of female involvement in mandibular trauma too. [
14]
Since direct trauma was one of the most common causes, age of the patient was taken into consideration as a variable. In our study, among the angle and condyle fractures, the highest incidence was observed in patients of 20 to 29 years age group. The mean age for both angle and condyle fractures was within 20 to 29 years age bracket. The social activity of young adults makes them more prone to trauma as compared with children, middle aged, and elderly persons. [
13]
In our study, the incidence of both angle and condyle fractures was highly affected by the age of the patients. However, our results were not complementary to those of Patil, who depicted that mandibular fractures were more prevalent among the older generations. [
15] Similar deductions were also made by Duan and Zhang. [
16]
Etiology or the cause of trauma was one of the variables of our study. We found that road traffic accidents were more responsible for angle fractures as falls were for condyle fractures. The most common cause of mandibular fractures in today’s day and age is road traffic accident, followed by violence or assaults as per Chrcanovic et al. [
13] According to Duan and Zhang, the highest incidence for mandibular fractures is seen in patients who were in road traffic accidents (44%), followed by assault (24%), fall (18%), and others. [
16] Our group A (angle fractures) results were contradicted by findings of Mah et al., who found assault or being struck by an object to be a more relevant cause of fracture; however, their results complemented our group B (condyle fractures) etiology which was followed by road traffic accidents. [
1] Tiwari et al. put forth that road traffic accidents were responsible for both angle and condyle fractures attributing up to 25% of patients with erupted mandibular third molars and 42% without third molars. [
17] Zhu et al. depicted two groups—one with unerupted third molars in which assault was a major etiological factor (41.6%) and the other without third molars in which assaults occupied 37.6% of the factors. [
12]
The statistical significance found in our results in relation to the presence and absence of impacted mandibular third molars and angle and condyle fractures was similar to the one found in a study by Mah et al. [
1] Reitzik et al. found that mandibular angle fractures were frequent in monkeys with impacted third molars due to the presence of only 60% strength as compared with a mandible without third molars. [
18] Tevepaugh and Dodson established that mandibular angle fractures were 3.8 times more likely to occur in the presence of a mandibular third molar than in the absence of the same. [
8] A similar result was established by Safdar and Meechan, Tiwari et al., and Halmos et al. [
11,
17,
19] The frequency of condyle fractures was found more in patients with absence of mandibular third molars or the ones who did not have impacted ones (79% erupted) as put forth by Zhu et al., Duan and Zhang, and Iida et al. [
12,
16,
20] However, study of Ugboko et al. conflicted with most of the researches and depicted that third molars were not a predisposing factor for angle fractures. [
21] Thus, prophylactic extractions of symptom-free mandibular third molars may strengthen the angle region, but at the same time the force generated may fracture the mandible elsewhere, especially the condyle. [
17] A theory that the presence of a mandibular third molar tends to reduce the cross-section area of the angle which in turn reduces the tensile strength of the bone, encouraging the propagation of fracture along the path of least resistance, was supported by Safdar and Meechan and Ma’aita and Alwrikat, [
11,
22] but was in conflict with Wolujewicz, Tevepaugh and Dodson, and Lee and Dodson who failed to establish this relation. [
8,
23,
24] Another interesting finding in different studies was the protective effect which the presence of third molars had on the condyle of the mandible and a similar effect which absence had on the angle of the mandible. [
25,
26]
The angulation of the mandibular third molar is also known to have a profound effect on the site of mandibular fracture, complementary to our results. Our results were supported by studies of Revanth et al. and Fuselier et al. for the group A (angle fracture) patients, who also found mesioangular impactions more prevalent. [
27,
28] Thangavelu et al. analyzed and validated the importance of angulation of M3s to the risk of angle and condyle fractures of the mandible. The most common angulation among angle fractures was mesioangular, which supported our data, but their finding of distoangular impactions among condyle fractures contradicted our results. [
29] Similarities were found in group B (condyle fractures), in which results put forth by Mah et al. and Patil matched our findings but conflicted with results of group A (angle fractures). Horizontal impaction was a relevant finding in the former’s study while vertical impaction was common in the latter’s study. [
1,
15] A similar conflict was also found with the result of Ma’aita and Alwrikat who found vertical and distoangular impactions more prominent among angle fractures. [
20,
22] Duan and Zhang compared vertical and horizontal positions for both angle and condyle fractures and found partially erupted third molars more prevalent among angle fractures and completely erupted third molars more common among condyle fractures for both the angulations. [
16]
As put forth by a prominent section of authors, the angle and condyle fracture patterns are influenced not only by the presence or absence but also by the position of third molars. Our results were statistically significant and complemented the study put forth by Mah et al., who also proved that class II position B was prevalent among angle fractures, while absence of third molar (class 0 position 0) and class I position A was one of the key reasons for condyle fractures to occur. [
1] Iida et al. supported the fact that class I was most responsible for mandibular fractures but unerupted third molars with class II position B and class III were accountable for the fractures to occur at the angle region, hence supporting our results for the same. [
20] Safdar and Meechan put forth the hypothesis that the amount of bony space occupied by an unerupted third molar can establish a direct relationship between the relative loss of bony integrity and weakness of that area of bone. Hence, proving that more deeply an impaction is seated, the more chances are of an angle fracture to occur. [
11] Lee and Dodson put forth the theory that a class III impaction or the deepest impaction was 50% less likely to cause a fracture of the angle than a partially erupted tooth, proving the concept that continuity of cortical bone plays an essential role in maintaining the integrity of the mandible. [
24] A similar theory was also suggested by Meisami et al. [
6] According to Halmos et al., there is a variable amount of risk depending on the position of third molar, the risk being greater in Pell and Gregory’s classes I and II and positions A and B. [
19] We confirm the results of Thangavelu et al., who also contemplated that highest incidence of angle fracture was found in class II position B and position A was more common among condyle fractures. [
29] However, Tevepaugh and Dodson failed to hypothesize the relationship between angle fracture and mandibular third molar. [
1,
8] Specifically, for condylar fractures, Duan and Zhang found class 0 to have a higher incidence followed by class I which supported our study; however, position C was more prominent as compared with position A, which contradicted our findings. [
16] Wolujewicz et al. also contradicted different studies stating that the presence of third molar does have an effect on the angle and condyle fractures, but the position is not a predisposing factor. [
23]
Finite element analysis studies have taken the front row in determining the forces acting around the different parts of the mandible and the concentration of stresses associated with them. Cho and Kim developed a three-dimensional (3D) finite element model study to determine the dynamic loads acting on different sites of the mandible to determine the stress concentration. They concluded that mandibular angle and the neck of the condyle were the most vulnerable to fractures due to concentration of load. They put forth that angle of the mandible is of reduced quality due to roots of the third molar and because the condyle automatically links this region to the upper skull, it also becomes a fracture site in the mandible. [
30]
A similar finite model study was performed by Antic et al., who generated three mandibular models from computed tomographic scans—one with an erupted third molar, one with partially impacted M3, and one without any M3. They were inflicted with a frontal and a lateral blow. The calculation of Von misses and principle stresses was performed. They concluded that angle region with impacted M3 showed highest stress in front blow and over the condylar region without M3. Similar finding was deduced with the lateral blow. [
2]
Bezerra et al. also performed a 3D finite model element study and found that the presence of a mandibular third molar resulted in greater stress concentration at the angle of mandible, whereas a similar effect was seen over the neck of the condyle on absence of M3. The conclusion drawn from their study was more of an anatomical and structural deduction; primary and secondary stresses were both responsible for angle and condyle fractures. [
31]
A recent meta-analysis performed by Armond et al., in which observational studies were included and 704 articles on mandibular third molars with angle fractures were assessed. They concluded that there was a positive connection between the presence of an impacted M3 and angle fracture (case–control studies: odds ratio [OR], 3.27). [
25,
26]
The third molar positions most favorable to angle fracture according to Pell and Gregory’s classification was class II position B, which is complementary to our results. The protective factors for angle fractures were class I position A.
A similar meta-analysis, with same number of observational cases, was performed for condyle fractures too. The deduction was that presence of a mandibular third molar reduced the risk of condyle fractures (case–control studies: OR 0.30). The assessment of all studies regarding condyle fractures proved that class I position A, as per Pell and Gregory’s classification, [
32] was the most favorable position for condyle fractures, which is similar to our results. Class II position B acts as protective factors for condyle fractures. [
25,
26]
The developed roots of the mandibular third molar were also taken as a determinant for the angle and condyle fracture pattern. Similar results were found by a retrospective study performed by Mah et al. who proved that condylar fractures were mostly associated with tooth germs or undeveloped roots, while horizontal impactions were a more common etiology for angle fractures due to the completely developed ones, hence concluding that mandibular angle and condyle fractures were significantly affected by the presence of third molar and continuity of cortical bone at the angle. [
1]
Irrespective of the conclusions drawn from our study, more research is still required to comprehensively examine the direction of strength and external force application, the quality of bone of the mandible, and the correlation between these factors and mandible angle and condyle fractures.