India has the highest fatality rates in road traffic accidents, 20 times that of a developed country. [
1] The situation in India is worsening and road traffic injuries have been increasing over the past 20 years. [
2] According to the report “Road Accidents in India 2015,” the number of injuries due to road traffic accidents rose to 500,279 in 2015 from 493,474 in 2014. Two-wheelers continue to be involved in maximum number of accidents (28.8%). However, more recent studies have shown that assault is now the most common cause of maxillofacial injuries in developed countries, and traffic accidents remain the most frequent cause in many developing countries. [
3,
4] Currently, there is a global trend for motorization, which in low- and middle-income countries is represented by an explosion in the use of twowheel vehicles. [
5] The use of crash helmets has been the subject of many studies, pointing out their efficiency in decreasing mortality and morbidity compared with motorcyclists who did not use this protective measure. [
6] According to the World Health Organization Statistical Information System (WHOSIS), Census Bureau and the Indian Ministry of Health, and the National Mortality Information System, mortality rates of motorcyclists was the highest in India as compared with 67 countries (8.6 deaths per 100,000 inhabitants).
The purpose of this study was to determine the role of helmet type and fixation on maxillofacial injuries among motorcycle accident patients.
Patients and Methods
This study was approved by the institutional review board and ethics committee according to the declaration of Helsinki. A written informed consent was obtained from the participants agreeing to be a part of the study.
Study Setting
The Department of Accident and Emergency—M.S. Ramaiah Teaching Hospital.
The Department of Accident and Emergency—M.S. Ramaiah Memorial Hospital.
The Department of Oral and Maxillofacial Surgery—Faculty of Dental Sciences, M.S. Ramaiah University of Applied Sciences.
Source of Data
Data were collected from all motorcycle crash victim/patients (rider/pillion) involved in a motorcycle crash accident attending the above-mentioned centers.
Study Period
A prospective clinical study was conducted for a period of 18 months extending from December 2015 till June 2017.
Sampling Frame
The sampling frame consisted of a motorcycle rider or a pillion who is involved in a road traffic accident, within the study region and during the study period. The sample size was calculated using the Open Source Epidemiologic Statistics for Public Health or OpenEpi Version 2.3.1.
Inclusion Criteria
All motorcyclists (rider or pillion).
All ethnic groups.
All age groups and gender.
All types and severity of maxillofacial injuries, involved in a motorcycle crash.
All types of accidents—high-speed as well as low-speed accidents.
Exclusion Criteria
Motorcyclists who discharged themselves from hospital care without a definitive diagnosis.
Patients who could not answer the questions, in case of loss of consciousness or death.
Resources Used
Data were collected with the help of a questionnaire, injury proforma, and crash information datasheet. The demographic data, crash characteristics, patients under the influence of alcohol, type of helmet, and if the chin strap was fastened or not, were evaluated and recorded with the help of the proforma questionnaire. The incidence and pattern of any skeletal injury was determined by dividing the face into three, that is, the upper face, the midface, and the lower face, and the fractures were noted. The type of soft-tissue injuries was analyzed as laceration, abrasion, contusion, and communication. Site of the soft-tissue injury was assessed as extraoral and intraoral injuries. Extraoral injuries were recorded by MCFONTZL system developed by Lee et al. [
9] Intraoral wounds were classified into six types—labial mucosa, sulcular mucosa, buccal mucosa, tongue, gingiva, and palatal mucosa.
The fastening of the chin straps of the helmets was recorded in all the patients and it was correlated with the type of helmet and the type and severity of injury occurring in the motorcycle accident cases.
Statistical Analysis
Statistical Package for Social Sciences (SPSS) for Windows Version 22.0 Released 2013 (IBM Corp., Armonk, NY) was used to perform statistical analyses. Descriptive analysis of all the explanatory and outcome parameters was done using frequency and proportions for categorical variables. Chisquared test was used to compare demographic, helmet types, collision types, and hard- and soft-tissue injuries with helmet-related characteristics (statistically significant if
p < 0.05;
Figure 1 and
Figure 2).
Results
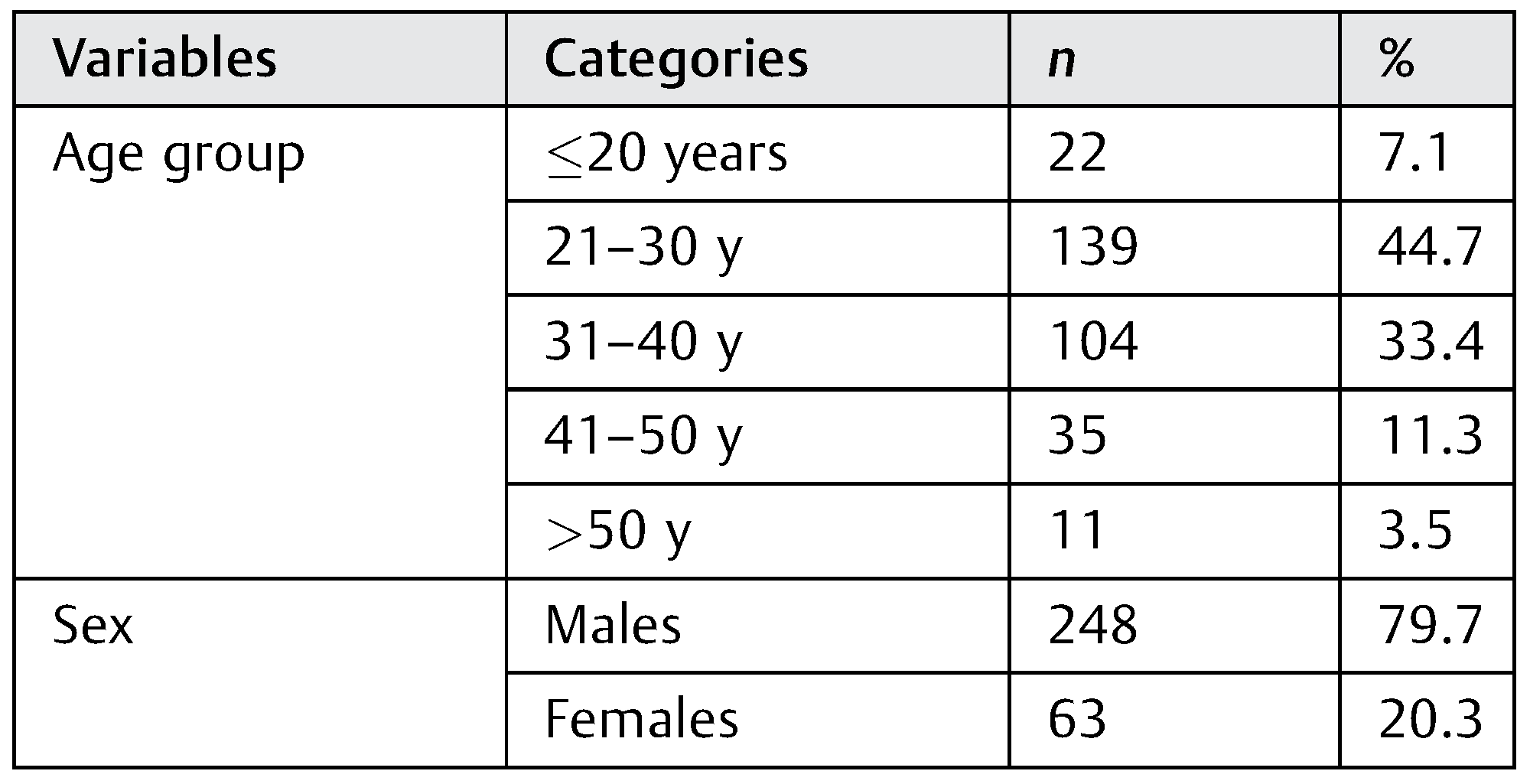
A total of 311 patients were evaluated in this study, who sustained facial injuries after the motorized two-wheeler accident: 248 were male and 63 were female; 234 patients were wearing a helmet at the time of the accident. Of these, 137 were open-face helmets (58.5%) and 97 were full-face helmets (41.5%). The percentage of male and female was 79.7 and 20.3%, respectively. The patients’ age ranged from 18 to 63 years (
Table 1).
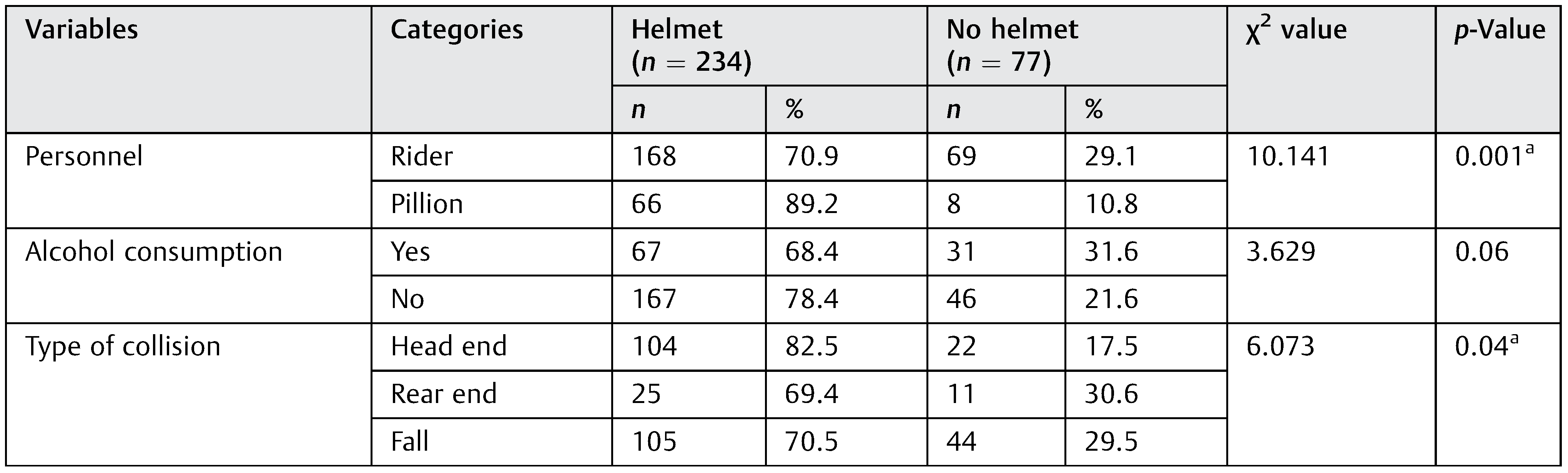
The numbers of riders sustaining facial injuries in the helmeted as well as the non-helmeted riders were significantly more as compared with the pillion (
p = 0.001). Riding under the influence of alcohol and its impact on the facial injuries at the time of a road traffic accident was also considered in this study, but the results were statistically insignificant. The type of collision was mostly head-ended collision and self-fall. The difference between the head end, rear end, and self-fall type of collisions was significantly more in helmeted riders as compared with non-helmeted riders. These results can be justified by the fact that the number of helmeted riders was significantly more than the non-helmeted riders in our study. Any kind of road traffic accidents with high-speed as well as low-speed collisions was taken into consideration for our study (
Table 2).
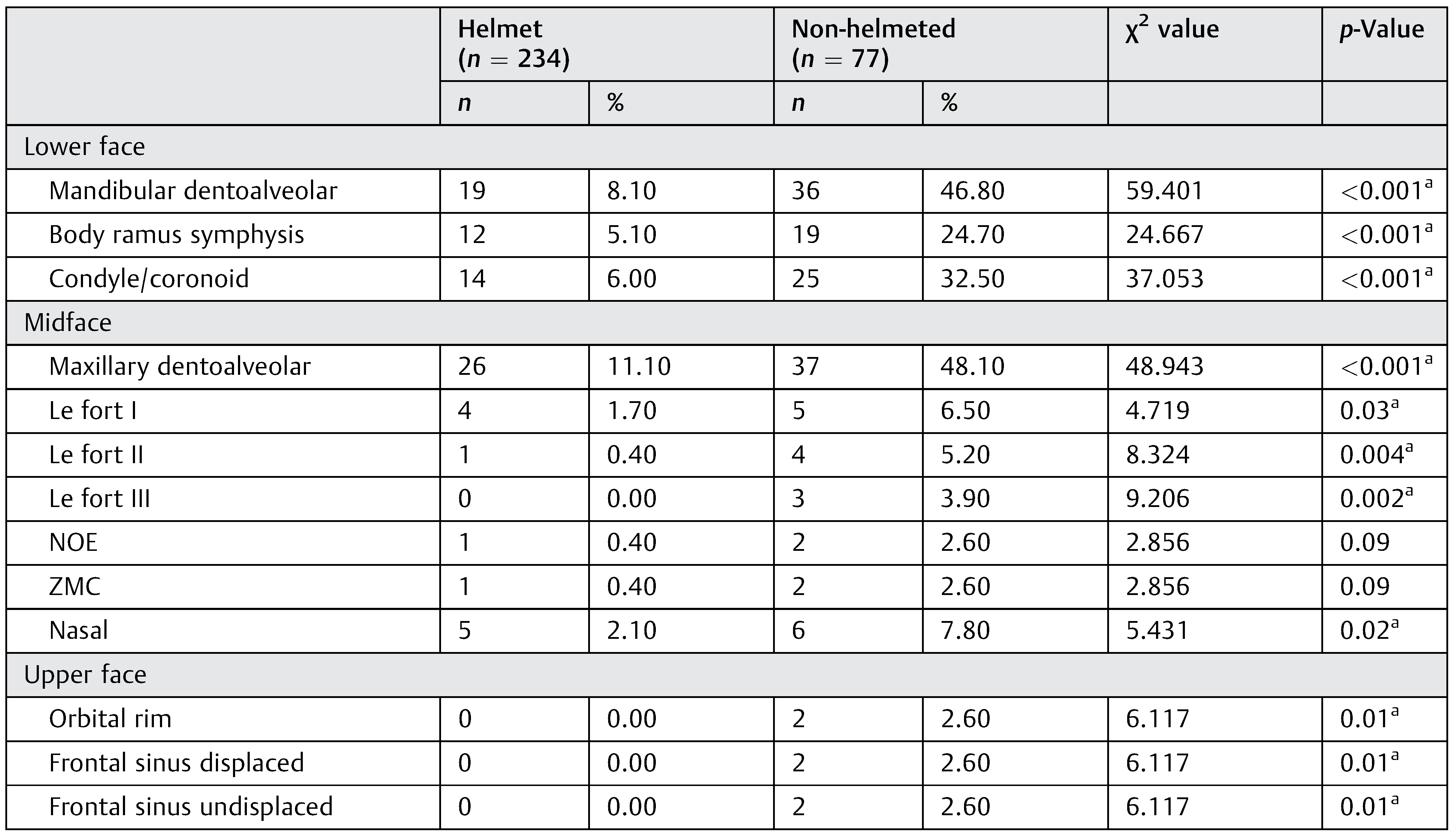
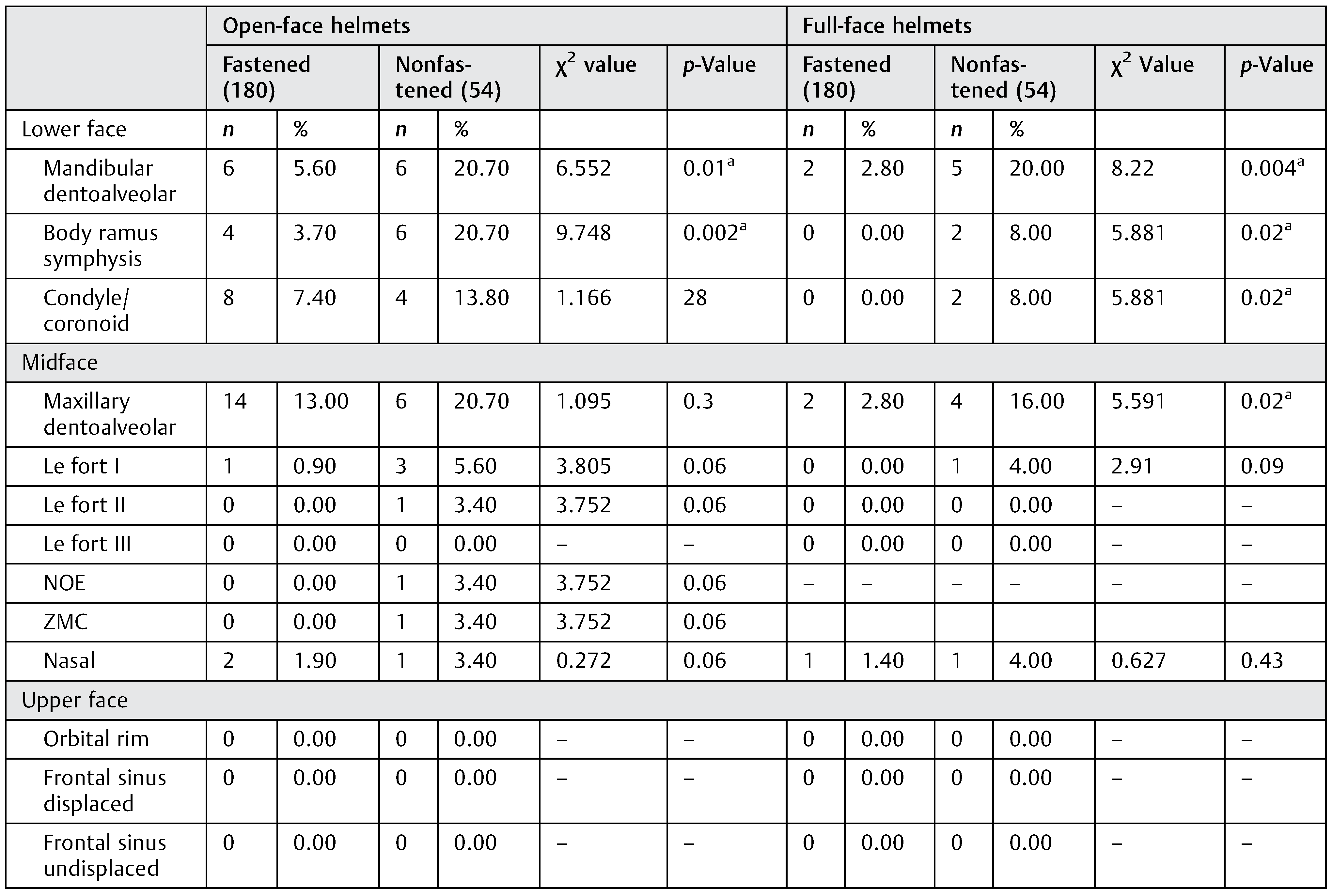
The type and pattern of injuries were evaluated in helmeted and non-helmeted riders, open- and full-face helmets, and fastened and nonfastened helmets. The number of subjects sustaining skeletal injuries was significantly more in non-helmeted group (
Table 3). If helmeted, the patients were subdivided into the types of helmet group (open-face helmet vs. full-face helmets). Helmeted subjects were also divided into fastening and nonfastening groups. Interestingly, there were no skeletal injuries in the upper face in helmeted subjects (
Table 4 and
Table 5).
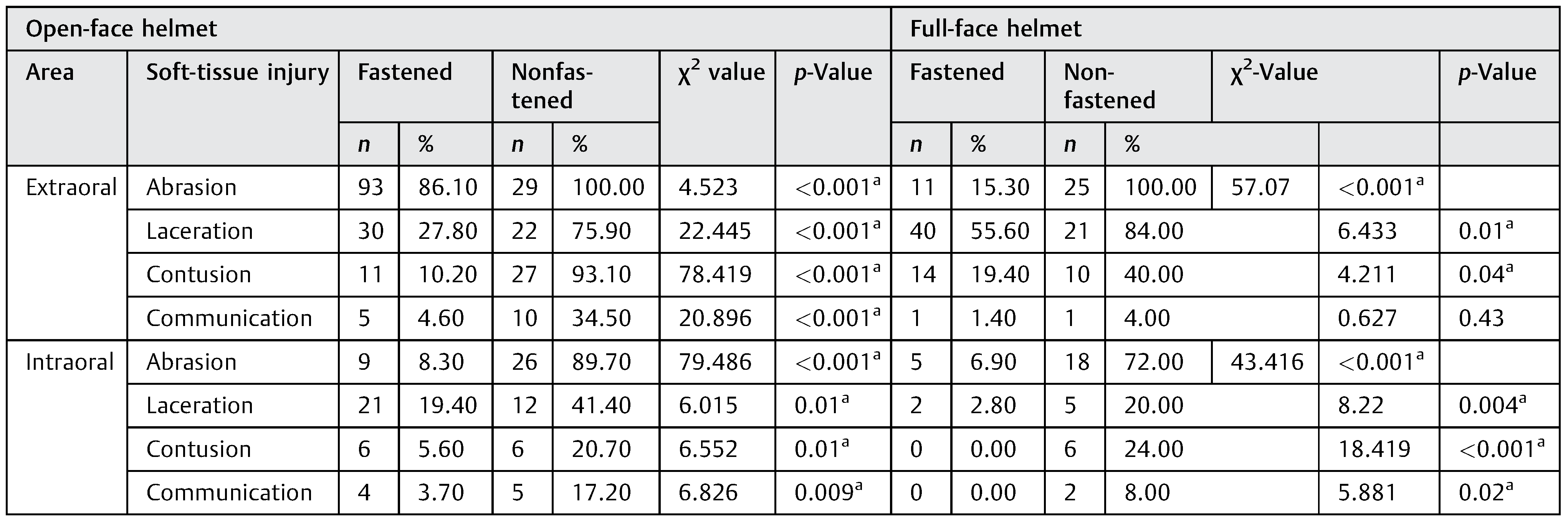
Skeletal injuries and the soft-tissue injuries were recorded separately. The maxillofacial skeletal injuries were recorded by dividing the face into three parts, whereas the soft-tissue injuries were subdivided into extraoral and intraoral injuries. The soft-tissue injuries were more in the nonfastened open helmet subjects. These differences were statistically significant (
Table 6).
Discussion
Maxillofacial injuries occurring from road traffic accidents is one of the most commonly encountered injuries by emergency departments worldwide. [
11] Trauma to the face needs special attention and a thorough evaluation during the primary stages of trauma care. The epidemiology of fractures is constantly influenced by the geographic area, population density, socioeconomic status, and cultural differences. [
12] Our unit being located in a semiurban locality had patients from various cultural differences and diverse socioeconomic strata and thus giving a wide range of results in this current study.
Most common age group to sustain maxillofacial injuries was 21 to 30, which accounted for 44.7% of the cases. This is in accordance with other studies conducted by several authors who have indicated a higher male to female ratio in road traffic accidents. [
6,
12,
13,
14,
15,
16] The incidence of injuries in male patients was significantly more as compared with that in females. This can be due to the fact that more numbers of male population ride two-wheelers in the city in general. The age group of 21 to 30 years was considered as the most common age group for the incidence of maxillofacial injuries. [
10,
12]
In this study, there were significantly more riders who sustained facial injuries after a motorized two-wheeler accident. The pillions sustained lesser number of injuries. The difference between the two groups was statistically significant. The literature of review indicates that the rider is more prone for sustaining facial injuries in a motorized two-wheeler accident. In a study conducted by Mallikarjuna and Krishnappa, 75.5% were riders and 24.3% were pillions. [
12] This can be attributed to the fact that the rider will face maximum impact during the collision, as he is in a more exposed front position. Also this study has taken into consideration solo riders who were riding without any pillions.
In our study, the collisions were recorded for low-speed as well as high-speed impacts. Head end collision and self-fall were the most common type of collision. Injuries sustained by non-helmeted riders during any kind of collision were significantly more in non-helmeted riders. The head end collisions and rear end collisions were comparable in a study conducted by Yu et al. [
7] These results were different from our study in which self-fall and head end collision type were more as compared with a rear end collision. Our study coincides with another study by Oginni et al. in which the most prominent collision type was head end. [
17]
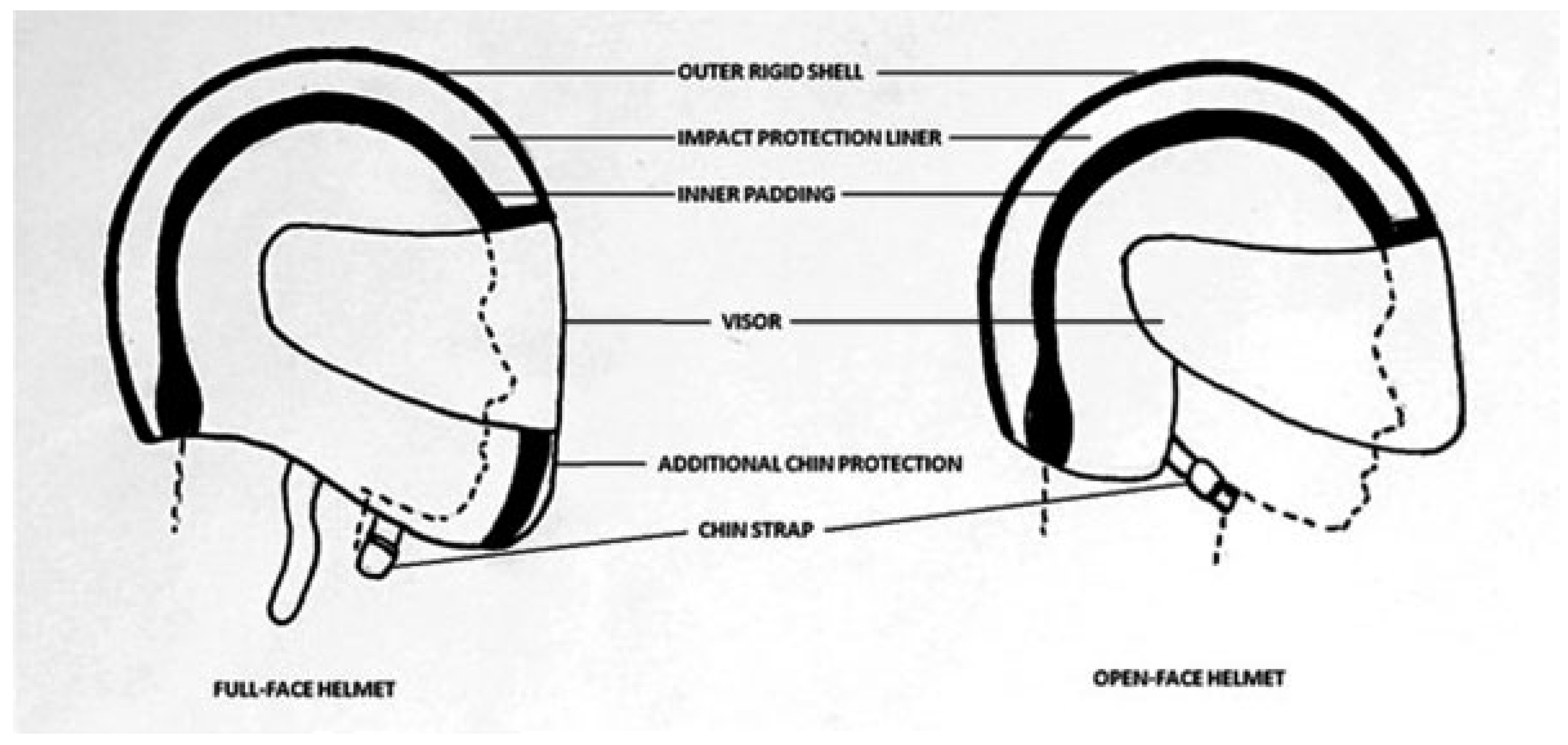
There were two types of helmets described in this study: an open-face helmet and a full-face helmet. An open-face helmet is a half helmet which has no protection of the face, whereas a full-face helmet has the protection of the face including the chin. In the literature review performed by Liu et al., it was found that full-face helmets were more effective than the open-face helmets. [
6] The same findings are substantiated by our study, in which the skeletal injuries as well as the soft-tissue injuries were much more in open-face helmets when compared with a full-face helmet.
Helmet fixation is a major issue among Asian motorcyclists. About one-third of Asian motorcycle riders were shown with poor fixation. [
7,
8,
18] If the helmet chin strap is not fastened or not fastened properly, the helmettends to slip-offat the time of impact, thus rendering incapable to protect the rider from maxillofacial injuries as well as head injuries. This factor has been well documented in our study in which the nonfastened helmet group sustained significantly more hard- and softtissue injuries as compared with a fastened helmet rider.
The motorcycle helmet rules which are not effective in some regions can be the defining cause of the facial injuries. There is a significant negative impact of relaxed motorcycle helmet laws leading to an increase in craniomaxillofacial injuries. [
19] After the application of the compulsory helmet law, which states mandatory helmet use for the rider as well as the pillion, the incidence of maxillofacial injuries as well as traumatic brain injuries has reduced considerably. [
20] Lack of adequate training coupled with poor law enforcement among motorcyclists may be the reason of the accidents. [
21]
The number of lower face fractures was more in the nonfastened group. This was statistically significant (p < 0.001). This can be described by the fact that the helmets slip off during the impact of the collision. This factor can also be attributed to the use of half-face helmets where there is no protection of the lower third of the face. The midface dentoalveolar fractures and the Le-Fort I fractures were significantly more in nonfastened group (p = 0.04 and 0.01, respectively).
Riders with loosely fastened helmets had an increased risk of head injury and were more than twice as likely to have brain injuries, compared with riders wearing properly fastened helmets. [
7] Non-helmeted motorcyclists were associated with 1.9 times higher risk of sustaining an open wound of the head and five times higher risk of intracranial injury, compared with those motorcyclists who used a helmet. [
18] Motorcyclists with poorly fixed helmet were five and four times as likely to sustain head and severe head injuries compared with those with firmly fixed helmets. [
8] These findings were in accordance with our study where motorcyclists with nonfastened helmets sustained significantly more hard- and soft-tissue injuries of the maxillofacial region. The amount of fractures sustained in the lower face in the open face fastened group was significantly less than the nonfastened group (
p = 0.01). The incidence of fractures was more in the nonfastened group of both the openand full-face helmets.
The extraoral abrasions, lacerations, contusions, and communications were significantly more in helmets with nonfastened chin straps when compared with fastened chin straps (p < 0.001). Similarly, intraoral abrasions (p < 0.001), lacerations, (p = 0.001), contusion (p = <0.001), and communications (p = 0.001) were significantly more in motorcyclists with nonfastened straps as compared with motorcyclists with fastened straps. The same is true about the open-face helmets as well as full-face helmets.
In most of the helmets, there is a visor, which is usually made of plastic or polycarbonate which tends to break at the time of the impact. This might result in soft-tissue injuries of the face, especially the mid-third and the lower third of the face. In the present study, the maximum number of softtissue injuries in the open-face helmet group was in the midthird and lower third of the face. Open-face helmets offer minimal to no protection of the mid-third and lower third of the face. A visor attached to the open-face helmet has no support or lock in the lower helmet. This might also contribute to the injuries of the face.
It can be concluded from our study that in case of a loosely fastened helmet or a nonfastened helmet, the incidence of injury is more in the open helmeted motorcyclists as compared with full-face helmet. But there were no fractures seen in the upper face in case ofopen-facehelmet, suggesting that anopenface helmet helps against upper face injury and head injuries.
Evidence from the literature showed that contributory factors to helmet ejection include improper chin strap fastening, failure of the fastening system, loose-fitting helmets, and high impact energy to the facial region causing dislocation or loss of support of the retentive system. One of the factors is the retention design. It was observed that a large number of motorcyclists who failed to fasten their helmets properly used helmets with double-D retention system. [
8]