The Effect of Deep Vein Thrombosis Prophylaxis on Bleeding in Periorbital Surgery in Trauma Patients
Abstract
:Materials and Methods
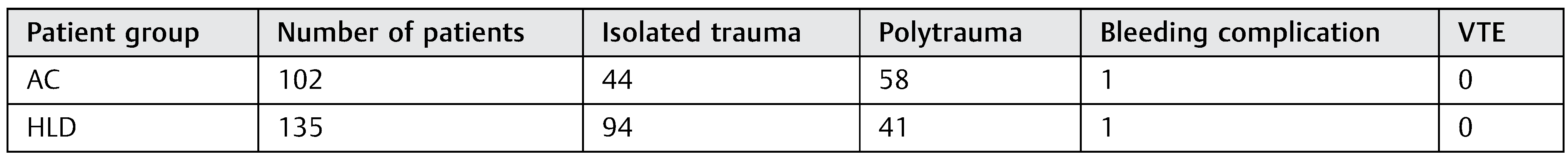
Results
Discussion
Conflicts of Interest
References
- O’Donnell, M.; Weitz, J.I. Thromboprophylaxis in surgical patients. Can J Surg 2003, 46, 129–135. [Google Scholar] [PubMed]
- Norwood, S.H.; McAuley, C.E.; Berne, J.D.; et al. A potentially expanded role for enoxaparin in preventing venous thromboembolism in high risk blunt trauma patients. J Am Coll Surg 2001, 192, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Geerts, W.H.; Jay, R.M.; Code, K.I.; et al. A comparison of low-dose heparin with low-molecular-weight heparin as prophylaxis against venous thromboembolism after major trauma. N Engl J Med 1996, 335, 701–707. [Google Scholar] [CrossRef]
- Louis, S.G.; Sato, M.; Geraci, T.; et al. Correlation of missed doses of enoxaparin with increased incidence of deep vein thrombosis in trauma and general surgery patients. JAMA Surg 2014, 149, 365–370. [Google Scholar] [CrossRef]
- Bandle, J.; Shackford, S.R.; Sise, C.B.; Knudson, M.M.; CLOTT Study Group. Variability is the standard: The management of venous thromboembolic disease following trauma. J Trauma Acute Care Surg 2014, 76, 213–216. [Google Scholar] [CrossRef]
- Gould, M.K.; David, G.; Sherry, W.; et al. Prevention of VTE in nonorthopedic surgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012, 141 (Suppl. S2), e227S. [Google Scholar] [CrossRef] [PubMed]
- Jamal, B.T.; Diecidue, R.J.; Taub, D.; Champion, A.; Bilyk, J.R. Orbital hemorrhage and compressive optic neuropathy in patients with midfacial fractures receiving low-molecular weight heparin therapy. J Oral Maxillofac Surg 2009, 67, 1416–1419. [Google Scholar] [CrossRef] [PubMed]
- Weitz, J.I. Low-molecular-weight heparins. N Engl J Med 1997, 337, 688–698. [Google Scholar] [PubMed]
- Levine, M.N.; Hirsh, J.; Gent, M.; et al. Prevention of deep vein thrombosis after elective hip surgery. A randomized trial comparing low molecular weight heparin with standard unfractionated heparin. Ann Intern Med 1991, 114, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Dolovich, L.R.; Ginsberg, J.S.; Douketis, J.D.; Holbrook, A.M.; Cheah, G. A meta-analysis comparing low-molecular-weight heparins with unfractionated heparin in the treatment of venous thromboembolism: Examining some unanswered questions regarding location of treatment, product type, and dosing frequency. Arch Intern Med 2000, 160, 181–188. [Google Scholar] [PubMed]
- Heit, J.A.; Silverstein, M.D.; Mohr, D.N.; Petterson, T.M.; O’Fallon, W.M.; Melton, L.J., III. Risk factors for deep vein thrombosis and pulmonary embolism: A population-based case-control study. Arch Intern Med 2000, 160, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Ho, K.M.; Burrell, M.; Rao, S.; Baker, R. Incidence and risk factors for fatal pulmonary embolism after major trauma: A nested cohort study. Br J Anaesth 2010, 105, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Barrera, L.M.; Perel, P.; Ker, K.; Cirocchi, R.; Farinella, E.; Morales Uribe, C.H. Thromboprophylaxis for trauma patients. Cochrane Database Syst Rev 2013, CD008303. [Google Scholar] [CrossRef] [PubMed]
 |
 |
© 2019 by the author. The Author(s) 2019.
Share and Cite
Woernley, T.C.; Maida, B.; Melville, J.; Marchena, J.; Demian, N. The Effect of Deep Vein Thrombosis Prophylaxis on Bleeding in Periorbital Surgery in Trauma Patients. Craniomaxillofac. Trauma Reconstr. 2019, 12, 271-273. https://doi.org/10.1055/s-0039-1683915
Woernley TC, Maida B, Melville J, Marchena J, Demian N. The Effect of Deep Vein Thrombosis Prophylaxis on Bleeding in Periorbital Surgery in Trauma Patients. Craniomaxillofacial Trauma & Reconstruction. 2019; 12(4):271-273. https://doi.org/10.1055/s-0039-1683915
Chicago/Turabian StyleWoernley, Timothy Charles, Blake Maida, James Melville, Jose Marchena, and Nagi Demian. 2019. "The Effect of Deep Vein Thrombosis Prophylaxis on Bleeding in Periorbital Surgery in Trauma Patients" Craniomaxillofacial Trauma & Reconstruction 12, no. 4: 271-273. https://doi.org/10.1055/s-0039-1683915
APA StyleWoernley, T. C., Maida, B., Melville, J., Marchena, J., & Demian, N. (2019). The Effect of Deep Vein Thrombosis Prophylaxis on Bleeding in Periorbital Surgery in Trauma Patients. Craniomaxillofacial Trauma & Reconstruction, 12(4), 271-273. https://doi.org/10.1055/s-0039-1683915



