In recent years, basketball has become the second most popular sport in the United States, second to only American football. [
1] In recent years, football has seen a decline in popularity amongst Americans with concerns over chronic traumatic encephalopathy and shortened career longevity. [
2] Basketball, however, has seen a gradual rise, with television ratings growing proportionally higher than other sports. [
2] In total, 31% of adults 30 to 49 years of age report actively playing basketball, with an estimated 23.4 million people, higher than any sport. [
3,
4] It is feasible that basketball may soon become the most popular sport in the United States.
Basketball-related injuries have been described in the literature, but most studies focus on injuries of the lower extremity. [
5] Previous studies investigating basketball-related facial injuries have been conducted, however, to a limited degree. [
6,
7,
8,
9] Despite this, an increased awareness of facial trauma-related injuries has led to the use of facial protection in many sports. [
10] For example, we have seen prominent players wearing face masks while recovering from injury, including Kobe Bryant, LeBron James, and Richard “Rip” Hamilton, who wore it permanently after multiple nasal fractures. [
11] Players have missed playing time due to mandibular and orbital fractures, as well as, lacerations, abrasions, and contusions. This type of trauma has not escaped the public eye. [
12]
The epidemiological data on these types of injuries as well as strategies to help mitigate them have not been well described. Describing the data on basketball-related facial trauma will allow for recommendations and adaptations to reduce future injury and devise protocols for more efficient and effective treatment. Therefore, our primary objectives were to determine the incidence of basketball-related facial injuries and further describe their patterns in regard to age, mechanism of injury, and degree of injury.
Materials and Methods
An analysis of basketball-related facial trauma was conducted using the National Electronic Injury Surveillance System (NEISS). The NEISS is a database under the United States Consumer Product Safety Commission that collects information from approximately 100 emergency departments (EDs). This database presents demographics (age, gender, and ethnicity), medical injury information (diagnosis, injury type, and injury location), and a small description of the event. The data are extrapolated to give a national representative sample.
Using the methods described in similar studies, the NEISS was accessed in July 2018 and searched for basketball-related head and facial injuries from the previous 3 years (2015–2017). [
10,
13] Data surrounding each event were collected including age (further stratified into age groups: 0–5, 6–11, 12–18, 19–34, and >35 years of age), injury type (laceration, fracture, abrasion/contusion, dental, concussion, other/unspecified), injury location (mandibular, maxillary, nasal, orbital, frontal bone/skull), and mechanism of injury (collision, fall, elbow, direct basketball trauma, other/unspecified). Injuries that occurred while not playing basketball, including injury while assembling a basketball hoop, a fight that occurred during a basketball game, or injury as a result of assault with a basketball, were excluded from the analysis. Injuries with an ambiguous description (i.e., “facial injury”) were also excluded from the analysis. Finally, injuries not related to facial trauma (i.e., concussions) were also excluded from the analysis.
Chi-squared testing (χ2) was performed to compare categorical variables, with a Bonferroni correction applied in posttest analysis within multimatrix sets, using IBM SPSS 25th version statistical software (Armonk, New York). Statistical significance was set for p-value less than 0.05 (p < .05).
NEISS is a public anonymized database, the nature of which qualifies as nonhuman subject research. Per Drexel University’s (Philadelphia, Pennsylvania) institutional review board (IRB) policy, this research is exempt from IRB review.
Results
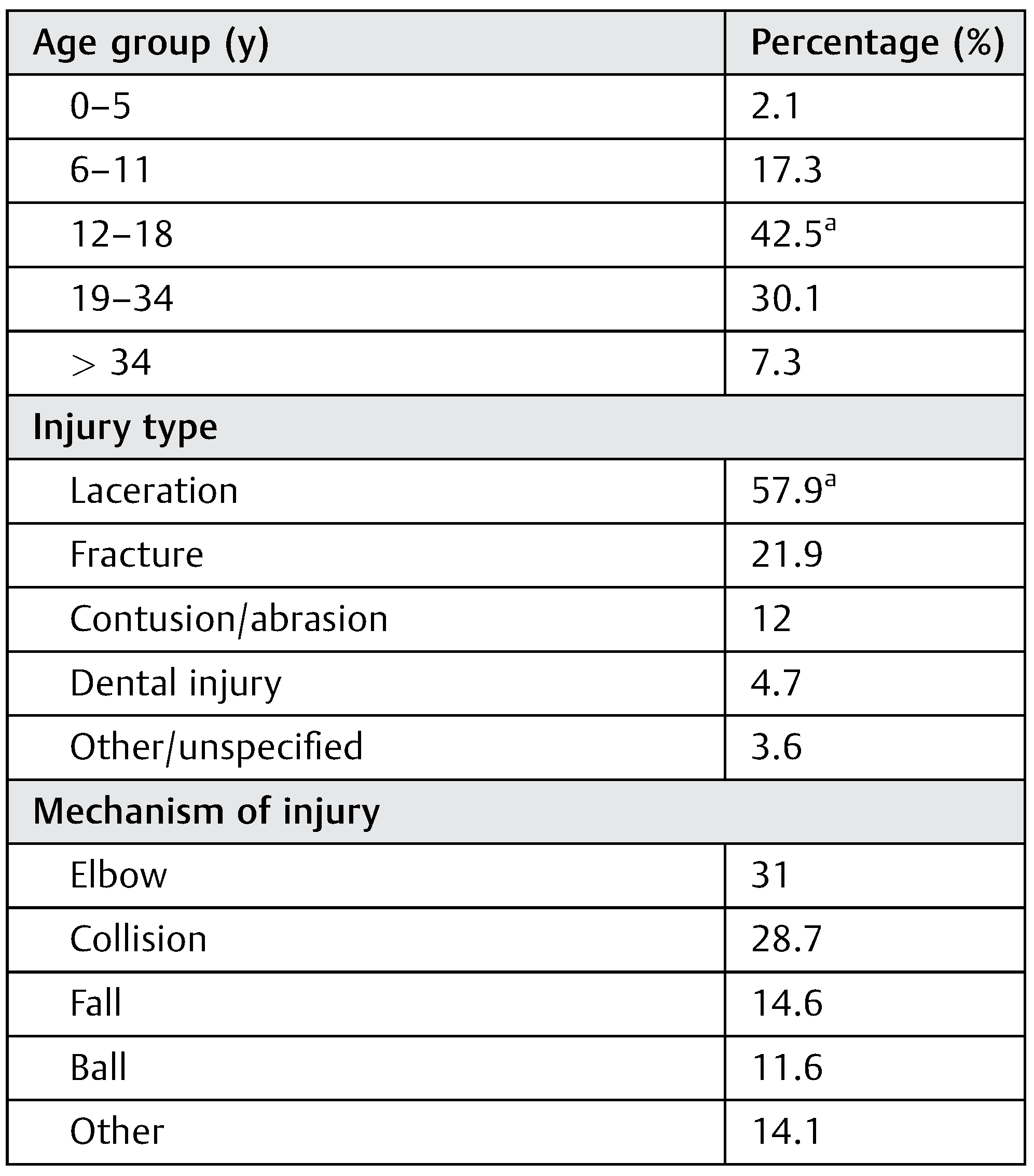
From 2015 to 2017, 8,977 basketball-related facial trauma ED visits were recorded in the database, with an estimated 234,887 visits occurring nationally. After exclusion criteria, a total of 4,578 ED visits were included in the study. Adolescents (age group: 12–18 years) incurred the most injuries, comprising 42.5% of the sample (
p < .001). The smallest incidence was in the 0 to 5 year age group, with an incidence of 2.1%. With respect to types of injuries incurred, lacerations accounted for the majority (57.8%;
p < .001). Dental injuries represented a small minority (4.7%), while the “other” category served the smallest group (3.6%). “Other” encompassed head and neck strain and sprain, dislocation, and hematoma. Mechanism of injury included elbow to the face (31%), collision with another player (28.7%), fall (14.6%), and direct basketball trauma (11.6%). The other/unspecified category (14.1%) had a greater occurrence than direct basketball trauma but could not be extrapolated to more specific data (
Table 1).
Type of injury appeared to have an effect on injury location. In regard to fracture, the nasal bone was the most common location (76.1%,
p < 0.001), while orbital and frontal bone fractures were the lowest (4.7 and 1.8%, respectively,
p < 0.001). With respect to lacerations, both orbital and mandibular had the highest occurrences (36.2 and 34.5% respectively,
p < 0.001), while frontal had the lowest (10.8%,
p < 0.001). Finally, the nasal region accounted for the most contusions and abrasions (29.6%,
p < 0.001), while the mandibular and maxillary areas were affected the least (10.8% and 10.3%,
p < 0.001 and
p = 0.02, respectively) (
Table 2).
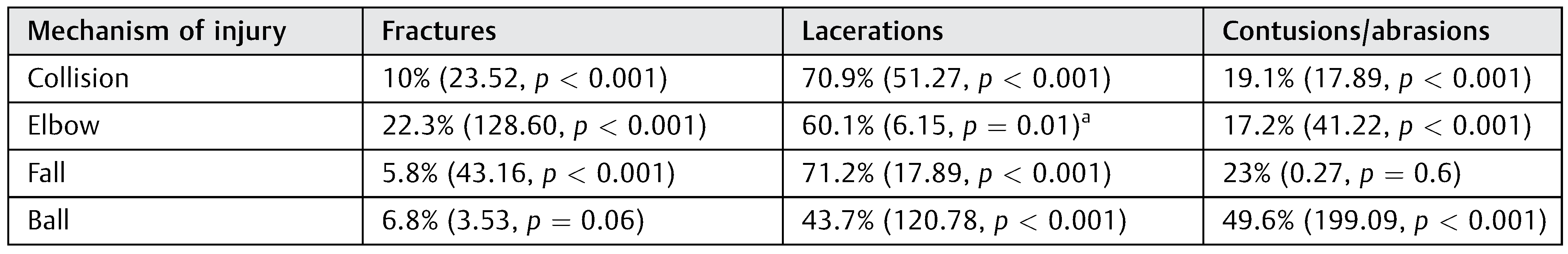
Mechanism of injury yielded significant differences in type of injury. Elbows to the face were the most likely type of injury to lead to a facial fracture (22.3%,
p < 0.001), while direct ball trauma was most likely to lead to a facial abrasion/contusion (49.6%,
p < 0.001). Collisions and falls were most likely to lead to lacerations, at 71.2 and 70.9% respectively (both:
p < 0.001).
Table 3 encompasses the full results.
Mechanisms in which varying age groups suffered injury were stratified as well. Collision with another player and elbow to the face were amongst the highest mechanisms to cause facial injury. One outlier was the 0- to 5-year-old age group, where collision was lowest at 9.5% (
p < 0.001) and falling down was the highest at 54.8% (
p < 0.001); the highest of any mechanism of injury in any age group.
Table 4 encompasses full data.
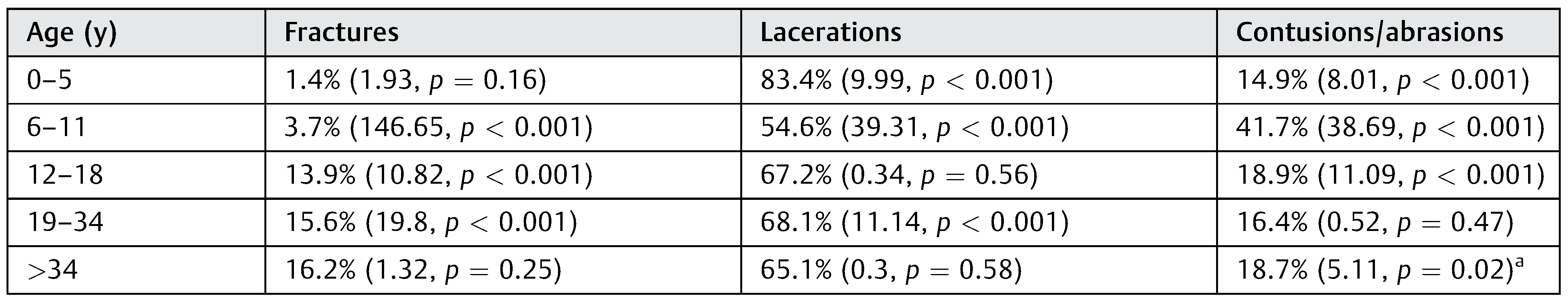
In terms of injuries most likely to occur in certain age groups, lacerations were the majority of injuries for all age groups. This was especially true for the 0 to 5-year-old age group, where lacerations were 83.4% (
p < 0.001) of the injuries suffered while fractures were relatively less common (1.4%,
p = 0.16). Fracture rates were highest in the age groups 12 to 18, 19 to 34, and 35 and up, while the 6 to 11-year-old age group had a significantly larger contusion/abrasion rate in comparison to the other groups (41.7%,
p < 0.001). Comprehensive data are enclosed in
Table 5.
Discussion
With basketball gaining increasing popularity, it is imperative to reach a comprehensive understanding of injuries related to the sport. Although previous studies have led to an improvement inplayer safety, further understanding can result in more efficient changes. Currently, the use of mouth guards have helped to reduce dental injuries. [
14,
15] The face mask has also shown promising data, but its utility and practicality have come under question in previous studies, citing collegiate athletes’ reluctance to use some facial safety equipment. [
15]
Overall, adolescents (age group: 12–18 years) incurred the most injuries, comprising 42.5% of the cohort in this study. Although previous studies did not further categorize patients into age groups, individuals under the age of 18 years accounted for the majority of soccer-, baseball-, and hockeyrelated injuries. [
10,
13,
16]
Our data showed the large majority of facial fractures to involve the nasal bone, suggesting a reemphasis on preventative methods or refinement of the face mask. This further supports other studies which have identified the nasal bone as the most commonly fractured bone in soccer, hockey, and baseball. [
10,
12,
16] The most concerning sequela of nasal bone fractures is cerebrospinal fluid leak with secondary brain infection. Although other facial fractures were less frequent, they come with complications including compromised airway, nerve injury, permanent deformity, and susceptibility to primary soft-tissue infections, osteomyelitis, and secondary brain infection. Therefore, further preventative methods are needed. [
17]
Lacerations were found to comprise the vast majority of injuries reported. It is also possible that this is underreported, as some patients may elect self-care for this type of injury. Regardless, it seems that mechanisms in preventing fractures can also be applied to laceration prevention. In addition, rates of contusions/abrasions with lacerations can be reduced if there are efforts to improve protection against fractures. These efforts are important overall because lacerations are the most common injury reported in other sports including soccer, baseball, and hockey. [
10,
12,
16] Lacerations were especially a major problem for the youngest age group (0–5 years), while abrasions/contusions were more likely to occur in the second youngest age group (6–11 years). Simultaneously, these two groups experienced lower fracture rates. The three remaining age groups (12–18, 19–34, and >34 years) had similar rates of injury. The insignificant fracture results were likely influenced by a much smaller sample size in the 0 to 5 and >34 year age groups. It may be necessary to obtain a greater power in our study for more reliable and conclusive results.
Children in the 0 to 5 year age group experienced falls as their primary mechanism of injury. This is likely due immature neurological balance, muscle strength, and bone formation, leading to an increased lack of coordination, functional strength, and reaction time. [
18] A potential solution for this is have children play on static, low impact surfaces, such as fixed, built-in carpeting, rather than traditional concrete street hoops or indoor hardwood floor to lessen fall impact. In contrast to the 0 to 5 year age group, all other groups had similar rates of injury mechanism, with collisions and elbows as the leading causes of injury. Protecting vulnerable areas with a face mask is one potential solution. A relatively smaller impact solution in regard to orbital injuries could be protective eye wear, especially in those who wear glasses. [
19] Making sure nails are cut short may also help lessen the impact of getting poked in the eye or small cuts on the face, and other parts of the body, that result from longer nails. [
20]
Another possible safety measure is to adjust the material of the ball. In our study, ball-to-face impact accounted for the majority of facial abrasions/contusions and a minority of overall injury mechanism. Ball-related injuries serving as a minority for mechanism of fracture is consistent with previous research. In organized sports, individuals are more likely to sustain a facial fracture from a ball in baseball, rugby, and soccer. [
21] In 2006, the National Basketball Association (NBA) attempted to change the material that basketballs were produced, from leather to synthetic microfiber. This ultimately failed due to player pushback on its functionality. However, it did result in a temporary transition from the leather material that manufacturers currently use to a softer material, with opportunity for future change. [
22] These changes have also been advocated across different sports previously, but further implementation and observation is needed to draw conclusions. [
23]
Unfortunately, due to the nature NEISS reporting, information was unavailable in terms of complications, resolutions, and detailed hospital course, limiting the potential for a more in-depth analysis. There was also limited information regarding the context of injury, such as if the fall occurred on hardwood or concrete, what safety equipment, if any, was used, size of the court, number of players on the court, or context of the game, such as friendly pickup, shooting around with friends, or an organized game for a league, as these all may play an effect. As discussed, the data may also skewed in terms of reporting. Abrasions and small lacerations do not always necessitate a hospital visit therefore these injuries may be underreported. Similarly, fractures may not always present to the ED for acute management and instead might have an initial outpatient visit, especially in children.
Previous research indicates that outside of orbital fractures and life-threatening injuries, there are no set guidelines on facial trauma management. This is attributed to a lack of evidence, preferences of different clinicians, fracture complexity, and varying hospital resources. [
24] Previous research indicates that various facial fractures sustained during sports, treated both operatively and nonoperatively, normally result in a full return to sports within a 3-week period. However, certain operative approaches were associated with longer recovery times, sometimes greater than the 3-week recovery period, due to the complexity of repair. [
25] Therefore, further investigation regarding an evidence-based approach to treatment is needed.
Additionally, further research may be necessary to examine rates of injury with current safety equipment versus a control. This can be further stratified to how likely a player is to wear the current equipment. From there, recommendations can be made to redesign for increasing practicality. Additional research is also necessary to correlate hospital course and patient presentation. Understanding typical presentations as they relate to specific injury mechanisms and varying context can help expedite clinical decision making as well as patient education.