Facial Fracture Patterns Associated with Traumatic Optic Neuropathy
Abstract
:Methods
Results
Discussion
Conclusion
Funding
Note
Acknowledgments
References
- Wang, B.H.; Robertson, B.C.; Girotto, J.A.; et al. Traumatic optic neuropathy: a review of 61 patients. Plast Reconstr Surg 2001, 107, 1655–1664. [Google Scholar] [CrossRef] [PubMed]
- Holt, G.R.; Holt, J.E. Incidence of eye injuries in facial fractures: an analysis of 727 cases. Otolaryngol Head Neck Surg 1983, 91, 276–279. [Google Scholar] [CrossRef] [PubMed]
- al-Qurainy, I.A.; Stassen, L.F.; Dutton, G.N.; Moos, K.F.; el-Attar, A. The characteristics of midfacial fractures and the association with ocular injury: a prospective study. Br J Oral Maxillofac Surg 1991, 29, 291–301. [Google Scholar] [PubMed]
- Yu-Wai-Man, P.; Griffiths, P.G. Steroids for traumatic optic neuropathy. Cochrane Database Syst Rev 2013, (06), CD006032. [Google Scholar] [CrossRef] [PubMed]
- Yu-Wai-Man, P.; Griffiths, P.G. Surgery for traumatic optic neuropathy. Cochrane Database Syst Rev 2005, (04), CD005024. [Google Scholar]
- Ropposch, T.; Steger, B.; Meço, C.; et al. The effect of steroids in combination with optic nerve decompression surgery in traumatic optic neuropathy. Laryngoscope 2013, 123, 1082–1086. [Google Scholar] [CrossRef] [PubMed]
- Joseph, M.P.; Lessell, S.; Rizzo, J.; Momose, K.J. Extracranial optic nerve decompression for traumatic optic neuropathy. Arch Ophthalmol 1990, 108, 1091–1093. [Google Scholar] [CrossRef] [PubMed]
- Bellamy, J.L.; Mundinger, G.S.; Flores, J.M.; et al. Facial fractures of the upper craniofacial skeleton predict mortality and occult intracranial injury after blunt trauma: an analysis. J Craniofac Surg 2013, 24, 1922–1926. [Google Scholar] [CrossRef] [PubMed]
- Cahan, M.A.; Fischer, B.; Iliff, N.T.; Clark, N.L.; Manson, P.N. Less common orbital fracture patterns: the role of computed tomography in the management of depression of the inferior oblique origin and lateral rectus involvement in blow-in fractures. J Craniofac Surg 1996, 7, 449–459. [Google Scholar] [CrossRef] [PubMed]
- Mundinger, G.S.; Dorafshar, A.H.; Gilson, M.M.; Mithani, S.K.; Manson, P.N.; Rodriguez, E.D. Blunt-mechanism facial fracture patterns associated with internal carotid artery injuries: recommendations for additional screening criteria based on analysis of 4,398 patients. J Oral Maxillofac Surg 2013, 71, 2092–2100. [Google Scholar] [CrossRef] [PubMed]
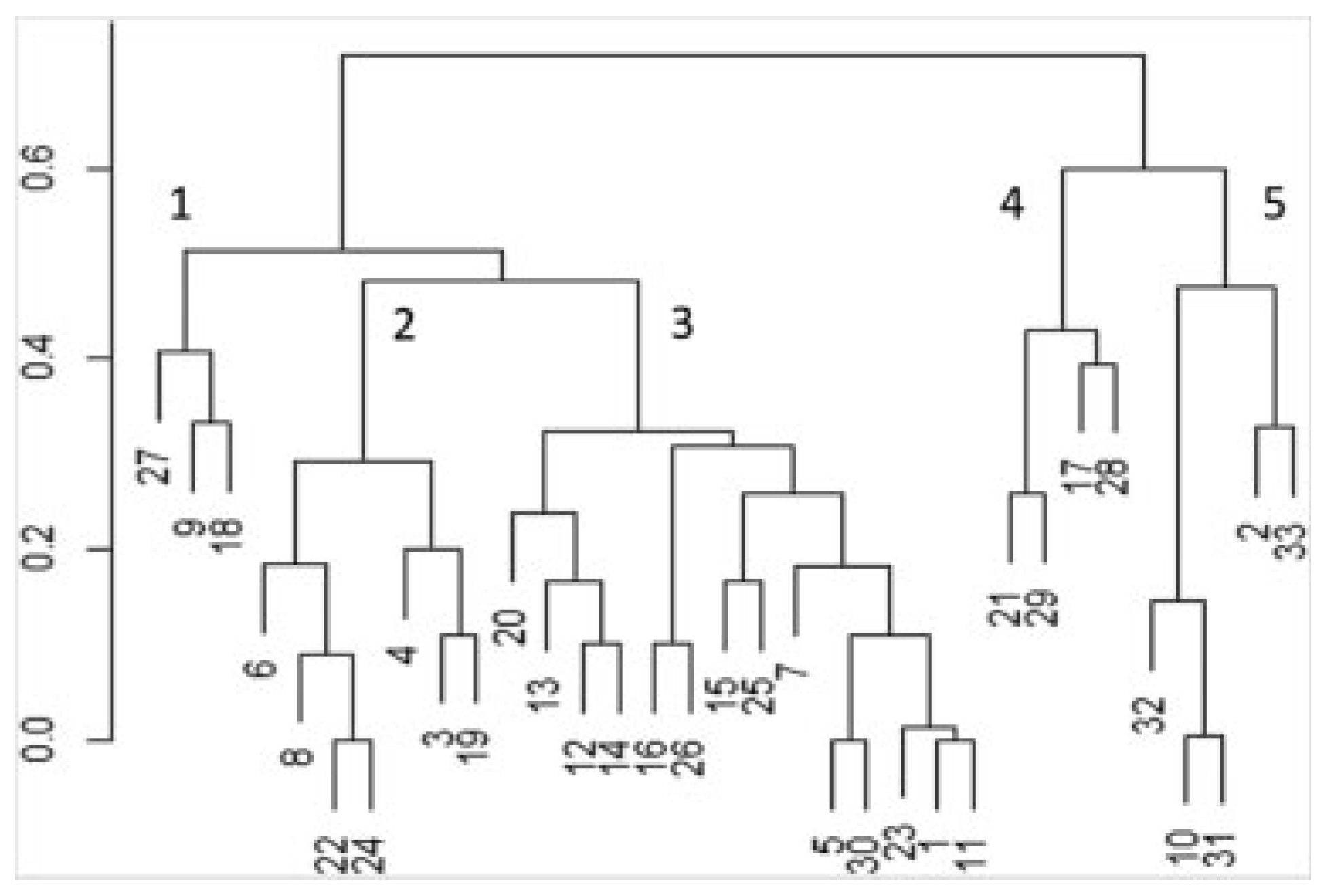
- Kaufman, L.; Rousseeuw, P. Finding Groups in Data: A Cluster Analysis; Wiley: New York, NY, USA, 1990. [Google Scholar]
- Maechler, M.; Rousseeuw, P.; Struyf, A.; Hubert, M.; Hornik, K. Cluster: Cluster Analysis Basics and Extensions. R package version 1.14.4. 2015.
- Kumaran, A.M.; Sundar, G.; Chye, L.T. Traumatic optic neuropathy: a review. Craniomaxillofac Trauma Reconstr 2015, 8, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Sosin, M.; De La Cruz, C.; Mundinger, G.S.; et al. Treatment outcomes following traumatic optic neuropathy. Plast Reconstr Surg 2016, 137, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Kim, J.H.; Hwang, K. The frequency of decreased visual acuity in orbital fractures. J Craniofac Surg 2015, 26, 1581–1583. [Google Scholar] [CrossRef] [PubMed]
- Amrith, S.; Saw, S.M.; Lim, T.C.; Lee, T.K. Ophthalmic involvement in cranio-facial trauma. J Craniomaxillofac Surg 2000, 28, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Tsai, H.H.; Jeng, S.F.; Lin, T.S.; Kueh, N.S.; Hsieh, C.H. Predictive value of computed tomography in visual outcome in indirect traumatic optic neuropathy complicated with periorbital facial bone fracture. Clin Neurol Neurosurg 2005, 107, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Magarakis, M.; Mundinger, G.S.; Kelamis, J.A.; Dorafshar, A.H.; Bojovic, B.; Rodriguez, E.D. Ocular injury, visual impairment, and blindness associated with facial fractures: a systematic literature review. Plast Reconstr Surg 2012, 129, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Ansari, M.H. Blindness after facial fractures: a 19-year retrospective study. J Oral Maxillofac Surg 2005, 63, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Vaca, E.E.; Mundinger, G.S.; Kelamis, J.A.; et al. Facial fractures with concomitant open globe injury: mechanisms and fracture patterns associated with blindness. Plast Reconstr Surg 2013, 131, 1317–1328. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.L.; Panje, W.R.; Gross, C.E. Optic nerve blindness following blunt forehead trauma. Ophthalmology 1982, 89, 445–455. [Google Scholar] [CrossRef] [PubMed]
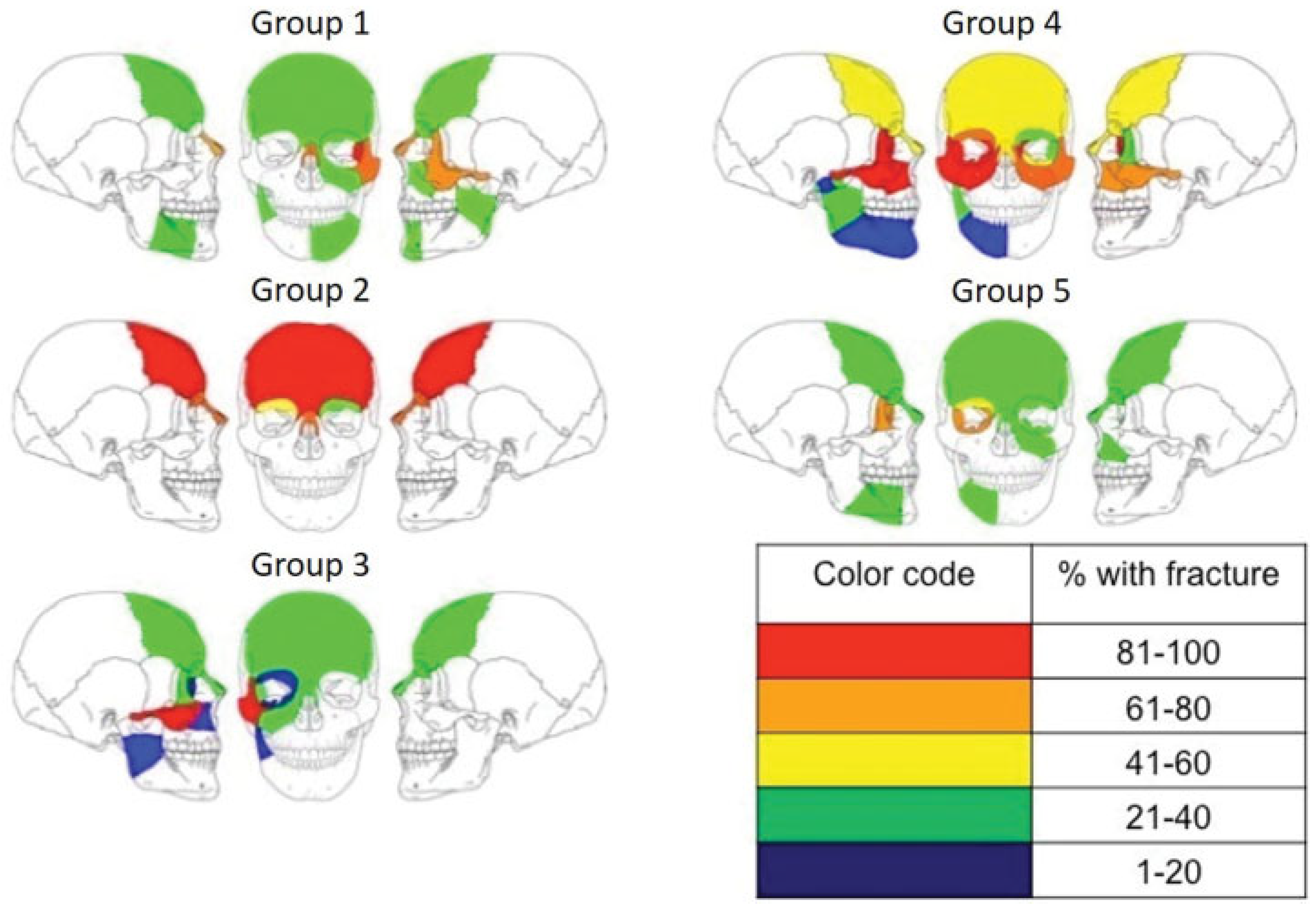
| 1 | 2 | 3 | 4 | 5 | Study (n = 33) | |
|---|---|---|---|---|---|---|
| Sex (% M) | 100% | 86% | 57% | 100% | 80% | 76% |
| Mean age | 18 | 28 | 37 | 22 | 52 | 34 |
| Side (% right) | 33% | 86% | 57% | 0% | 80% | 58% |
| Mechanism (% penetrating) | 100% | 14% | 36% | 100% | 60% | 45% |
| Mean number of fractures | 4.7 | 2.6 | 2.4 | 12.6 | 4.25 | 4.7 |
| Mean Glasgow Coma Scale | 15 | 11 | 10 | 9 | 7 | 10 |
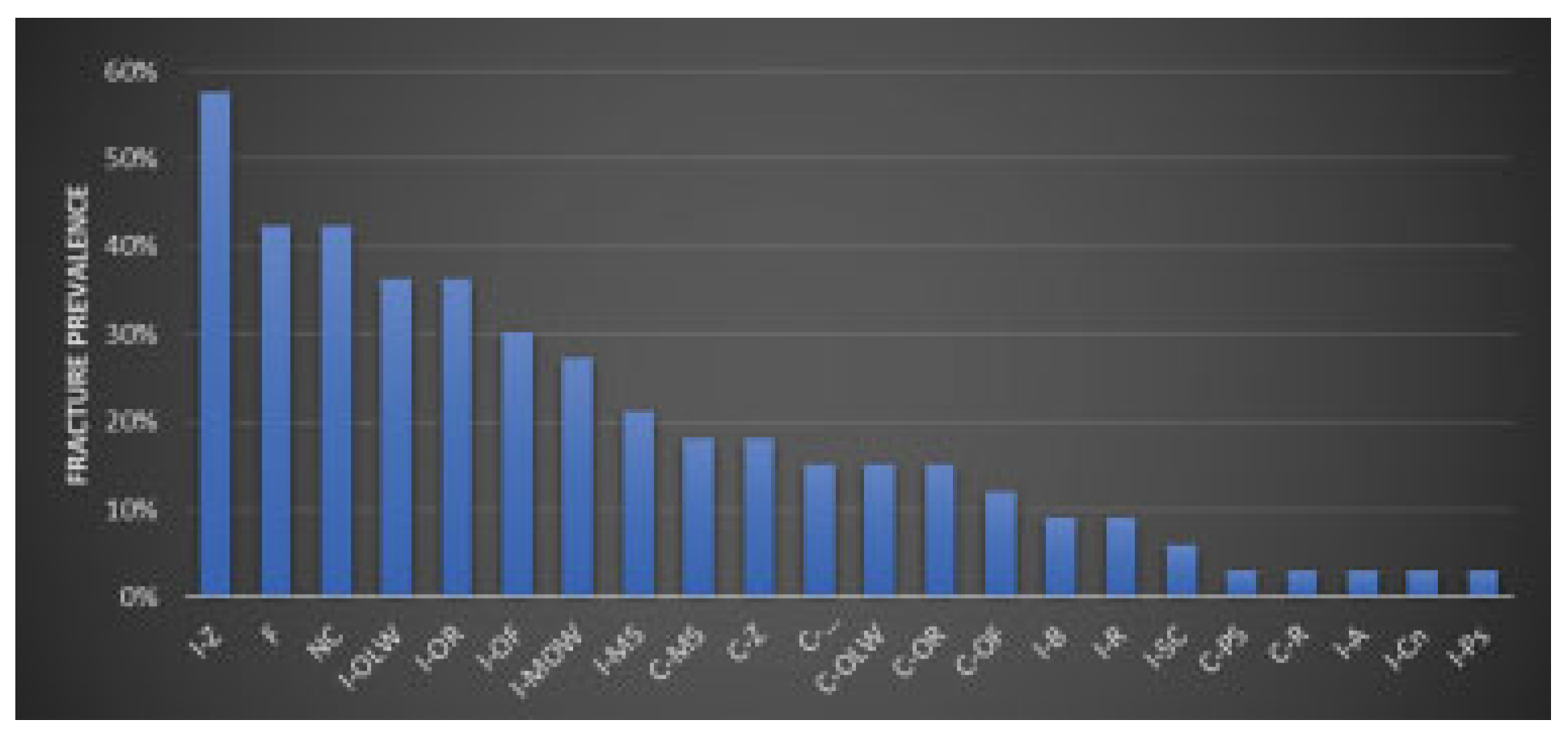
| Study (n = 33) | Total number of fractures | % with fracture | Bone | Number of fractures | % with fracture | Bone | Number of fractures | % with fracture | |
|---|---|---|---|---|---|---|---|---|---|
| Ipsilateral zygoma | I-Z | 19 | 58 | Clade I | Clade IV | ||||
| Frontal | F | 14 | 42 | C-OLW | 3 | 100 | C-MOW | 5 | 100 |
| Nasal combo | NC | 14 | 42 | NC | 2 | 67 | I-MOW | 5 | 100 |
| Ipsilateral orbital lateral wall | I-OLW | 12 | 36 | C-Z | 2 | 67 | I-MS | 5 | 100 |
| Ipsilateral orbital roof | I-OR | 12 | 36 | F | 1 | 33 | I-OF | 5 | 100 |
| Ipsilateral orbital floor | I-OF | 10 | 30 | C-MS | 1 | 33 | I-OLW | 5 | 100 |
| Ipsilateral medial orbital wall | I-MOW | 9 | 27 | C-OR | 1 | 33 | I-Z | 5 | 100 |
| Ipsilateral maxillary sinus | I-MS | 7 | 21 | C-Ps | 1 | 33 | C-MS | 4 | 80 |
| Contralateral maxillary sinus | C-MS | 6 | 18 | C-R | 1 | 33 | C-Z | 4 | 80 |
| Contralateral zygoma | C-Z | 6 | 18 | I-B | 1 | 33 | I-OR | 4 | 80 |
| Contralateral medial orbital wall | C-MOW | 5 | 15 | F | 3 | 60 | |||
| Contralateral orbital lateral wall | C-OLW | 5 | 15 | Clade II | NC | 3 | 60 | ||
| Contralateral orbital roof | C-OR | 5 | 15 | F | 6 | 86 | C-OF | 3 | 60 |
| Contralateral orbital floor | C-OF | 4 | 12 | NC | 5 | 71 | C-OLW | 2 | 40 |
| Ipsilateral body | I-B | 3 | 9 | I-OR | 4 | 57 | C-OR | 2 | 40 |
| Ipsilateral ramus | I-R | 3 | 9 | C-OR | 1 | 14 | I-R | 2 | 40 |
| Ipsilateral subcondyle | I-SC | 2 | 6 | I-Sc | 2 | 40 | |||
| Contralateral parasymphysis | C-PS | 1 | 3 | Clade III | I-A | 1 | 20 | ||
| Contralateral ramus | C-R | 1 | 3 | I-Z | 14 | 100 | I-B | 1 | 20 |
| Ipsilateral angle | I-A | 1 | 3 | I-OLW | 4 | 29 | I-Cn | 1 | 20 |
| Ipsilateral condyle | I-Cn | 1 | 3 | F | 3 | 21 | I-Ps | 1 | 20 |
| Ipsilateral parasymphysis | I-Ps | 1 | 3 | NC | 3 | 21 | |||
| Symphysis | S | 0 | 0 | I-MS | 2 | 14 | Clade V | ||
| Basilar | B | 0 | 0 | I-OF | 2 | 14 | I-MOW | 3 | 75 |
| Contralateral angle | C-A | 0 | 0 | I-OR | 2 | 14 | I-OF | 3 | 75 |
| Contralateral body | C-B | 0 | 0 | I-MOW | 1 | 7 | I-OLW | 3 | 75 |
| Contralateral coronoid | C-C | 0 | 0 | I-R | 1 | 7 | I-OR | 2 | 50 |
| Contralateral condyle | C-Cn | 0 | 0 | F | 1 | 25 | |||
| Contralateral subcondyle | C-Sc | 0 | 0 | NC | 1 | 25 | |||
| Ipsilateral coronoid | I-C | 0 | 0 | C-MS | 1 | 25 | |||
| C-OF | 1 | 25 | |||||||
| C-OR | 1 | 25 | |||||||
| I-B | 1 | 25 |
© 2018 by the author. The Author(s) 2018.
Share and Cite
Kelishadi, S.S.; Zeiderman, M.R.; Chopra, K.; Kelamis, J.A.; Mundinger, G.S.; Rodriguez, E.D. Facial Fracture Patterns Associated with Traumatic Optic Neuropathy. Craniomaxillofac. Trauma Reconstr. 2019, 12, 39-44. https://doi.org/10.1055/s-0038-1641172
Kelishadi SS, Zeiderman MR, Chopra K, Kelamis JA, Mundinger GS, Rodriguez ED. Facial Fracture Patterns Associated with Traumatic Optic Neuropathy. Craniomaxillofacial Trauma & Reconstruction. 2019; 12(1):39-44. https://doi.org/10.1055/s-0038-1641172
Chicago/Turabian StyleKelishadi, Shahrooz S., Matthew R. Zeiderman, Karan Chopra, Joseph A. Kelamis, Gerhard S. Mundinger, and Eduardo D. Rodriguez. 2019. "Facial Fracture Patterns Associated with Traumatic Optic Neuropathy" Craniomaxillofacial Trauma & Reconstruction 12, no. 1: 39-44. https://doi.org/10.1055/s-0038-1641172
APA StyleKelishadi, S. S., Zeiderman, M. R., Chopra, K., Kelamis, J. A., Mundinger, G. S., & Rodriguez, E. D. (2019). Facial Fracture Patterns Associated with Traumatic Optic Neuropathy. Craniomaxillofacial Trauma & Reconstruction, 12(1), 39-44. https://doi.org/10.1055/s-0038-1641172



