One of the most demanding aspects of dental and surgical practice is the management of the patient who has suffered alveolar process trauma. The major problem in the treatment of alveolar process fractures is difficulty in the adequate achievement of anatomical reduction and immobilization. Various treatment modalities for the stabilization of fractured alveolar process segment, which are in practice and mentioned in the literature, include the splinting method consisting of wiring techniques such as Essig’s wiring, figure-of-eight wiring, arch bar, wire reinforced composite splint, acid-etched brackets and arch wire splint, custom-made cast metal trauma splint with lingual access holes, fiber splint (multilayer), ribbon splint, self-drilling bone screws with stabilizing wires, and plates.[
1] Although these techniques provide an effective treatment of these fractures, their efficacy may be questionable in terms of patient compliance, comfort, longer duration, and treatment predictability.
In some cases, traditional fixation of the fractured piece is not possible as the teeth needed for splinting may be missing; therefore, in such cases, lag screw fixation becomes useful. Originally described by Brons et al[
2] and then by Niederdellmann et al,[
3] lag screw fixation has been available in the armamentarium of surgeons for many years. Krenkel[
4] has described the lag screw technique for fixation of the fracture of the mandibular condyles. The main purpose of the study is to evaluate the stability of the alveolar process fractures of the maxilla and mandible using lag screw osteosynthesis.
Materials and Methods
A simple nonrandomized and observational study was conducted at the Department of Oral and Maxillofacial Surgery, from August 2014 to March 2017. The Institutional Review Board and the Local Ethical Committee had approved the study. The study followed the criteria as declared by Helsinki. In this study, 20 adult patients without any systemic complications, who strictly met the inclusion criteria, were included.
The inclusion criteria were patients with oblique alveolar process fracture of maxilla or mandible alone or in combination with other facial fractures, patients aged between 7 and 62 years without involving the tooth buds, and patients who consented for the surgical treatment and postoperative follow-up. The exclusion criteria were patients with primary dentition with underlying tooth buds in the fractured alveolus; patients who could not be followed up postoperatively over a minimum period of 3 months; and patients with facial fractures with infection and a history of diabetes, uncontrolled hypertension, prolonged steroid therapy, compromised immunity, or associated bone pathologic features; alcoholics; and patients with fracture older than 7 days.
The diagnosis was made on the basis of the clinical examination findings and radiographic interpretation. Routine investigations were performed. All patients provided informed consent before participating in this study. To remove the bias, a single surgeon had operated on all the patients under standard aseptic conditions and protocol. A 2.0-mm titanium screws were used for the mandibular alveolar process fracture and 1.5-mm titanium screws were used for the maxillary alveolar process fracture.
The Technique of Placement
A 2.0-mm transgingival lag screw placement was done under general or local anesthesia depending on the case. Following carefully closed repositioning and anatomical evaluation, a 1.6-mm-diameter bur was used to drill a hole through the gingiva, perpendicular to the broken fragment (cis-cortical) and the alveolar process (transcortical). This process of placement of the lag screw in the fractured segments prevents the most complication of the lag screw placement, that is, fracture of the outer cortex as soon as compression. Moreover, we need to diligently handle the cis-cortical (broken) fragment. A larger, 2.0-mm-diameter bur was used to enlarge the holes in the fractured alveolar fragment. The fragment may be temporally fixed by hand or retention forceps. The screw length was measured with a depth gauge. A 2.0-mm titanium screw was driven into the bone, bicortically through the gingiva in a compression manner, similar to onlay grafts. Care was taken to maintain the original alignment of the fractured piece. The procedure was repeated until the adequate number of screws is inserted. The use of at least two screws is recommended to achieve adequate 3D stability. In all cases, antibiotics were administered for 5 days as per need. Postoperative instructions included good oral hygiene and the use of mouth rinse with 0.2% chlorhexidine gluconate (
Figure 1, Figure 2, Figure 3 and Figure 4).
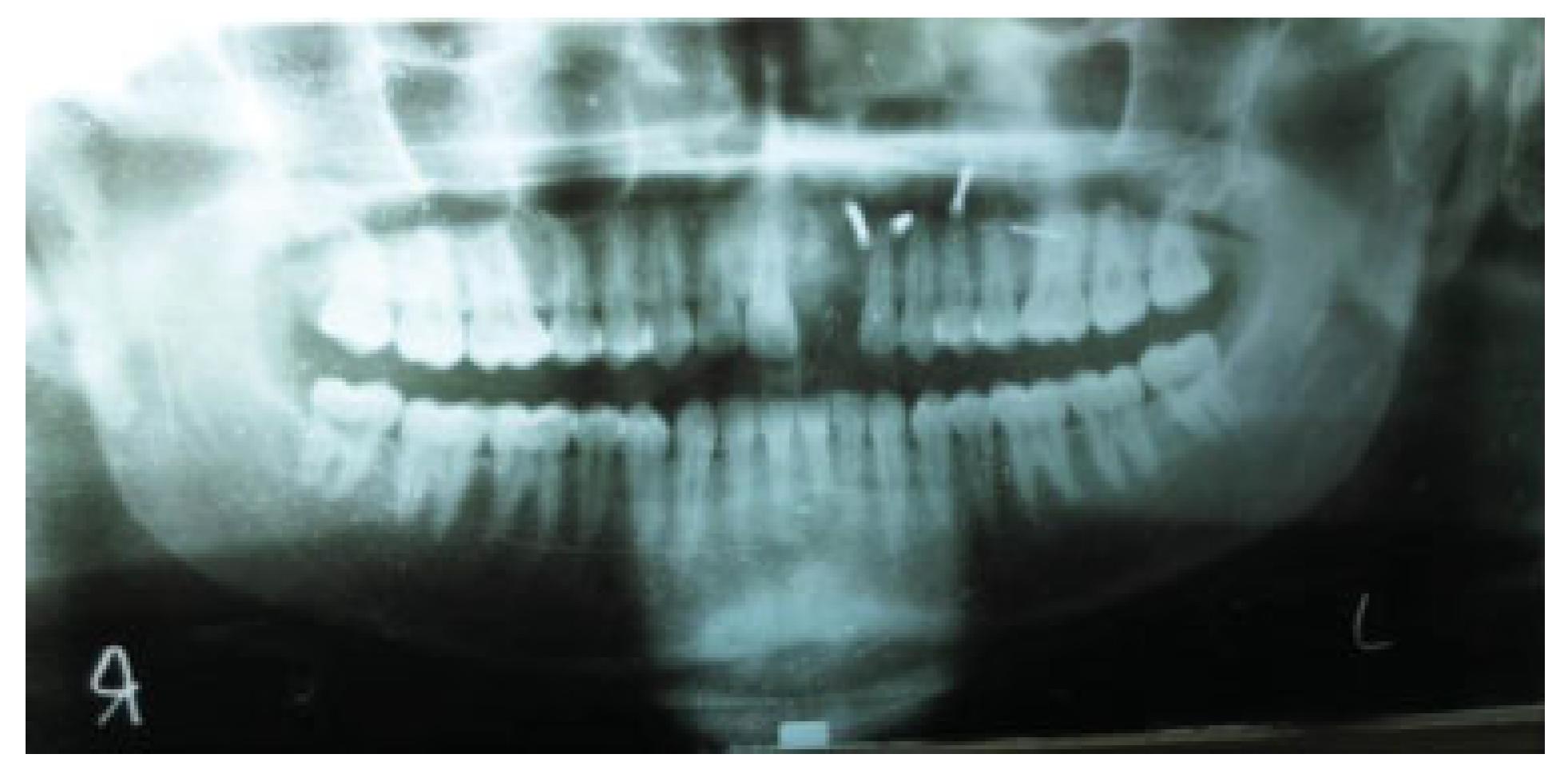
Follow-up of all cases was done for a minimum period of 3 months. Follow-up was done as day −1 (preoperative day), day 1 on operative day, day 10 (10th postoperative day), day 30 (30th postoperative day), and day 90 (90th post-operative day). Orthopantomograms (OPG) were taken on all follow-up visits.
The transgingival lag screws were removed under local anesthesia, 3 months after osteosynthesis. The mucosa covering the screws or adjacent to it was infiltrated with 1 mL 2% lignocaine hydrochloride with 1:80,000 adrenaline.
All cases were evaluated for the following parameters on all follow-up visits.
Fracture stability was evaluated by mechanical manipulation of the alveolar process in all three dimensions: bucco lingual, mesiodistal, and upward–downward directions. The fracture was considered stable if movement was absent in all three dimensions. The fracture was considered unstable if movement was present in any of the dimensions.
Anatomical reduction was initially assessed by evaluating the functional occlusion in the centric relation of the patient during the postoperative follow-up visits. It was also evaluated by taking pretreatment and postoperative radiographs (OPG) for a period of 3 months on prescribed follow-ups. It was considered positive if overlapping between the fractured fragments was seen in radiographs, and it was considered negative if overlapping was absent.
Bone loss and resorption were assessed by taking a series of radiographs (OPG) for a period of 3 months on prescribed follow-ups. Bone loss was considered positive if bone volume became less on follow-up OPGs and it was considered negative if bone volume remained the same radiographically. Tooth loss was assessed clinically and radiographically on postoperative follow-ups. Tooth loss was considered positive if several teeth in the fractured alveolar process became less, and it was considered negative if the number of teeth remained same.
Wound infection should have pus discharge which has to be positive for bacterial growth and culture.
Statistical Analysis
The obtained data were analyzed statistically using IBM SPSS Statistics Windows, version 20.0 (IBM Corp, Armonk, NY). Descriptive analysis was done and the data were presented in the form of frequency and percentage to analyze efficacy of transgingival lag screw fixation in alveolar process fracture.
Discussion
The aim of the contemporary treatment of alveolar process fracture includes reestablishing the original occlusion and providing the uncompromised function with natural esthetics. Alveolar process fracture has a great psychological impact on the patient due to fear of losing tooth or teeth which more commonly affect the anterior region. Early diagnosis and management of alveolar process fracture will help in the maintenance of good occlusion. The earlier the hard- and soft-tissue injuries are treated, the better are the chances of good healing. Alveolar process trauma usually results from falls, playground accidents, bicycle accidents, athletic injuries, motor vehicle accidents, abuse and domestic violence, assaults, and altercations.
Oikarinen and Kassila[
5] reported that the frequency and nature of dentoalveolar injuries vary and are largely dependent on the cause, gender, and age of the patient. Barde et al[
6] investigated the epidemiology of mandible fractures in India and found the highest incidence in the age group of 21 to 30 years and a male:female ratio of 3.7:1.34. The most common etiological factor was found to be RTA by the study of Kotrashetti and Singh.[
7] In our study too, RTA was the most common factor (65%) responsible for alveolar process fractures and a majority of patients were in the age group 7 to 20 years (8 patients out of 20 patients, 40%). Lag screw osteosynthesis is a method that provides the advantages of stable internal fixation. Lag screw osteosynthesis can be defined as the stable union of two bone fragments under pressure with the help of screws inserted in lag fashion.[
3,
6]
The lag screw technique was first introduced to maxillofacial surgery by Brons and Boering[
2] in 1970 for mandibular fractures. Ideally, the length of fracture surface should be greater or equal to the mandibular height, a condition that is satisfied in the oblique surface fractures.
According to Ardary et al,[
8] the ultimate stability of screw fixation depends on the number of screws used, the method of screw placement, bicortical placement of the screws, and the holding power of the screws, which is affected by cortical bone thickness. The stability of this kind of osteosynthesis relies solely on compression between the fragments. In a study performed by Hyde et al,[
9] 10% of patients required elastic traction during the postoperative period for the first 10 days to achieve their premorbid occlusion. In our study, no elastics were used and number of screws was two or three, which provided sufficient bone compression for uneventful healing. Long back in 1976, Hovland and Gutmann[
10] had put forth a splinting technique for fixation of luxated or avulsed teeth which was atraumatic. The splint consisted of direct-bonded, mesh-backed, stainless steel orthodontic brackets attached by elastic ligatures to a piece of SS wire, but then this technique is not suitable for the alveolar process fracture in which multiple teeth are lost. Oikarinen and Kassila,[
5] in one of their review articles on splinting of teeth, had written extensively on the versatility of wire-composite splints. The wire-composite splint meets most of the principles of modern tooth fixation. Flexible splints allow normal masticatory stimulus, hence prevents and eliminates small resorption areas and promotes pulpal healing and can be kept for a longer time. And for alveolar block fracture, they suggested the same splint, but instead of 0.3-mm-thick stainless steel wire 0.5-mm-thick stainless steel wire should be used. But again, these splints were not suitable for cases where multiple teeth loss was present or which had large edentulous space.[
4] Some of the patients, who had lost three lower anterior teeth, were successfully treated with our method of fixation by the transgingival lag screw.
In a study performed by Nyárády et al,[
11] the transgingival screw was used as an alternative method to splinting and traditional plate osteosynthesis. In spite of other facial fractures, lag screw can be used for the alveolar process fractures along with the fractures of maxillofacial skeleton without affecting the other treatment modalities for the same. The transgingival lag screw technique in the management of alveolar process fracture is easy and quick to use, and flap reflection for osteosynthesis of alveolar process is not necessary. However, in cases of gingival lacerations, stripping of flap may further reduce the blood supply; therefore, going transgingivally without further manipulation of alveolar process fracture is advised. The technique is also recommended for alveolar process fractures when the blood supply is jeopardized and dental splinting is not possible. Ngassapa et al,[
12] in their experimental study, compared the reaction of periodontium to Merkx prefabricated arch bar splint and Obwegeser’s continuous loop wiring, and they recorded that both the splints had a significant amount of plaque accumulation except that the Merkx splint had more plaque comparatively, and there was marginal alveolar bone resorption. With the use of a lag screw for alveolar process fracture, we can anticipate good periodontium health without any disease or marginal bone loss, as there will be minimal or no plaque retention around the lag screw. A study conducted by Nyárády et al[
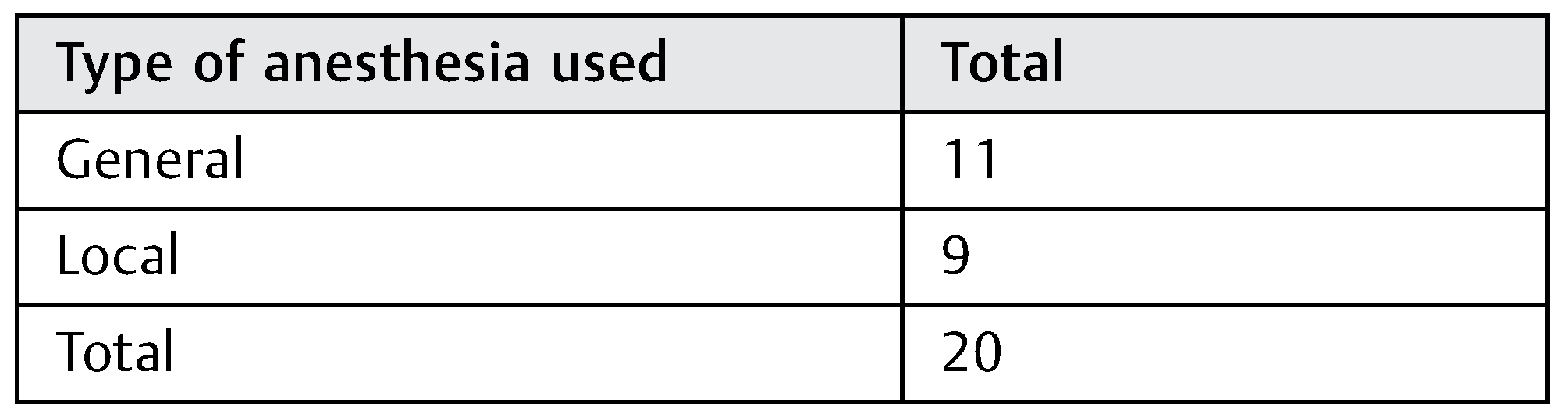
11] indicates that lag screw fixation whether done under general or local anesthesia had the same results. Our study also indicates that lag screw fixation whether done under general or local anesthesia had the same results. All patients recovered uneventfully. Kotrashetti and Singh[
7] did the assessment of inter-fragmentary mobility and showed this to be present in 20% of cases of lag screw fixation used for mandible fracture, and the mobility was absent by the second postoperative follow-up. Nyárády et al[
11] used transgingival lag screw to treat patients with alveolar process fracture and recorded no bone loss and no tooth loss in the surgical area, and broken bone was also not resorbed.
All the fractures were anatomically reduced after lag screw fixation. In our study too, all the fractures were absolutely stable after lag screw fixation and all the fractured alveolar process showed the anatomical reduction after lag screw fixation. We also evaluated bone loss, tooth loss, and bone resorption during the study and found no tooth loss, no marked bone loss, and no bone resorption in any of the follow-ups in any of our cases. Zachariades et al[
13] encountered an infection rate that varied between 1% for those fractures treated with in the first week and 4% for those treated within a second week or later. Another factor that contributes to the infection was poor local conditions. None of the fractures got infected in our study. Coburn et al[
14] reported some complications with traditional lag such as fracture of the screws on insertion, iatrogenic damage to teeth and teeth root causing loss and bony sequestra formation. Ellis and Ghali[
15] reported a common complication during lag screw placement which is the fracture of outer cortex of the segment once the compression starts, but no such complication was seen in our study. The advantages of using a lag screw instead of plates are less implant material, lower costs, a simpler technique, and limited surgical exposure. Since then, the compression screw technique has been widely used.[
16,
17,
18]
Lag screws were also used in the midface area by Pribtkin et al.[
19] Screws and implants have been introduced through the mucosa without complications for a long time. Fracture of the alveolar process is a common injury, comprising 2 to 8% of all craniofacial injuries. Often, nearby soft tissue and teeth are damaged making the situation more severe and thus bone grafting or advanced prosthetic techniques are required for rehabilitation. In our study, the outcome was good in all cases. No further augmentation was needed. The transgingival introduction of lag screws for stabilizing the broken fragments did not interfere with the compromised blood supply of the alveolar process. The inserted implants were minimal. The flapless operation shortens the operation time.
In our study, the oral hygiene could be maintained adequately, as no bulky arch bars were used, and no splinting was done in any of the 20 alveolar process fracture treated. With time, the understanding and management of alveolar process fracture have evolved tremendously to the present day transgingival closed reduction and fixation using titanium-osteosynthesis screws which are minimally traumatic, equally effective, and less time consuming, best suited for the world in which time is most respected and priceless.
The major limitation of this study is the small sample size. Further research is required in the future to validate the applicability of the lag screw as a routine procedure for the alveolar process fracture patients.