Purpose
This article aims to evaluate the opioid prescribing habits of faculty at the University of Minnesota School of Dentistry, prior to and following implementation of an opioid-prescribing protocol for acute postsurgical pain.
Background
The misuse of prescription pain relievers is the second most common form of drug abuse behind marijuana. Drug overdose deaths have nearly tripled during 1999–2014 [
1]. The Centers for Disease Control and Prevention (CDC) reported 64,070 deaths from 2016 to 2017 related to opioids nationwide, constituting a 21% increase. Natural and semisynthetic opioids such as hydrocodone and oxycodone were responsible for 14,427 deaths (22.5%), preceding heroin (24.1%) and synthetics opioids (31.4%) [
2]. These facts led to the President of the United States declaring the opioid abuse epidemic a national health emergency on August 10, 2017.
The relationship between prescription opioids and opioid abuse has been well documented [
3,
4,
5,
6] and increased morphine milligram equivalents (MMEs) have been correlated to increased opioid-related death [
7]. While there has been recent data reporting that heroin is becoming a more common first opioid, use of prescription opioids remains a significant initiator of abuse [
8]. Dentists and oral surgeons are among the leading opioid prescribers and are responsible for the majority of prescriptions to minors. The vast majority (99.2%) of dentists report prescribing opioids for various procedures, the most frequent being hydrocodone (76.1%) and oxycodone (12.2%). The most correlated procedure is third molar extractions. A cohort study of 2,757,237 third molar extraction patients in the Medicaid database reported an average prescription MME of 120, representing 24 5-mg tablets of hydrocodone or 16 5-mg tablets of oxycodone [
9]. Another study reported an average of 20 tablets, with 20% of providers prescribing significantly more [
10]. Both studies noted significant variation in the MME prescribed. Patients report requiring three tablets within the first 24 hours for pain control, with an average total number of eight tablets required following extraction of third molars [
11].
It has been estimated that over half of all opioid medication prescribed following dental surgery goes unused [
12]. Unused medication can, unfortunately, contribute to abuse. This impact is reflected in reports that the majority of abused medications by teenagers are obtained from a parent’s medicine cabinet, and 75% of abusers obtain their opioids from a family member or an acquaintance [
5].
To improve postoperative pain management and reduce variance in opioid prescribing, the Department of Oral and Maxillofacial Surgery, University of Minnesota School of Dentistry introduced an opioid prescription protocol in February 2016 [
13]. This protocol was created in response to the Minnesota Legislature’s Opioid Prescribing Improvement Program (OPIP) released in March 2015 [
14]. The protocol guidelines were developed based on evidence that acute postoperative pain can be effectively managed with preoperative nonsteroidal anti-inflammatory drugs (NSAIDs) and a regimen of ibuprofen [
15,
16,
17].The University of Minnesota’s protocol calls for preand postoperative NSAIDs to be used as first-line analgesic therapy unless contraindicated. In cases when opioids are indicated, such as prolonged or difficult surgical procedures, providers should choose the lowest MME option that will adequately produce analgesia. Providers should consult the State Prescription Drug Monitoring Program (PDMP) prior to writing opioid prescriptions, as opioids should not be prescribed to patients who have a concurrent opioid prescription. Reasons for deviation from the guidelines are to be documented in the patient’s records. The protocol resembles the statement from the American Dental Association regarding the use of opioids for the treatment of dental pain [
18] as well as the CDC guidelines for opioid prescribing [
4].
Dentists have an opportunity to play a significant role in reducing access to opioid medications. Gaps in opioid training, implementation of mitigation strategies, consistent patient education, and the use of PDMP have been identified as possible targets [
19]. PDMPs have been proven to be successful in decreasing the number of opioid-related deaths [
20,
21]. The use of an opioid protocol to standardize prescribing habits can reduce the number of opioid prescriptions and decrease variance while allowing the provider autonomy in patient management. Acute postoperative pain remains a challenging problem that dentists and oral surgeons must address, with both undertreatment and overtreatment leading to serious consequences [
16,
22]. The goal of the opioid protocol is to educate dentists on evidence-based prescribing patterns and act as a guide on the treatment of dental pain.
Materials and Methods
This retrospective analysis compares the number of total opioid prescriptions and number of tablets per prescription in the previous 10 quarters prescribed by the University of Minnesota School of Dentistry. Prescription data were collected from institutional electronic health record software (Axium). All FDA (Food and Drug Administration) Schedule I, II, III, & IV opioids that were written within the University of Minnesota School of Dentistry were collected. The Divisions of Orthodontics and Pediatric Dentistry were not included as they do not use an electronic health record or report prescriptions in a searchable method. Data included the prescribing department, provider number, patient’s age, date of prescription, medication, dosage, and number of tablets. Departments with significant opioid prescriptions (n ≥ 100) were included in the analysis (Comprehensive Care, Endodontics, General Practice Residency, Operative, Oral Surgery, Periodontics, Prosthodontics). Departments with less than 100 prescriptions over all 10 quarters were not included in individual department analysis (Operative). Temporomandibular and Orofacial Pain Clinic data were also not included, as the majority of its opioid prescriptions were assumed to be for chronic pain management and not applicable for acute postoperative pain protocol. Only opioids prescribed in tablet form were included, as liquid form opioids were a small number and not statistically significant.
The opioid prescription protocol was introduced and accepted in February 2016 by the Clinical Affairs Committee. The protocol became a mandatory university policy immediately. Per protocol, departments were required to enroll in electronic prescribing (eRx) by their own discretion. Departmentof Oral and Maxillofacial Surgery was thefirstdepartment to implement electronic prescribing on October 1, 2016. All departments within the University of Minnesota were notified along the same timeline via email and through committee presentations of the policy and reasons for implementation. Education on the protocol was completed by Dr. Harold K. Tu, Director of the Department of Oral and Maxillofacial Surgery, for each clinical department including faculty, students, and residents. Training consisted of an educational lecture which was given to each department individually. Departments were allowed to enroll in eRx along their own timelines. The protocol was published to the University of Minnesota School of Dentistry Web site on January 18, 2018.
Data were collected under the specifications of IRB 1701M04361. Statistical analysis was completed in Statistical Package for the Social Sciences (SPSS, IBM ver. 25). Graphics were generated in Excel (Windows 2016). Of the total opioid prescriptions (n ¼ 8,257), 97.7% were included (n ¼ 8071) if complete. Prescriptions missing data were excluded from analysis (n ¼ 186). Averages displayed as the mean. Error bars reflect standard error due to normal distribution. Means compared by one-way ANOVA with p-value < 0.05 were considered significant.
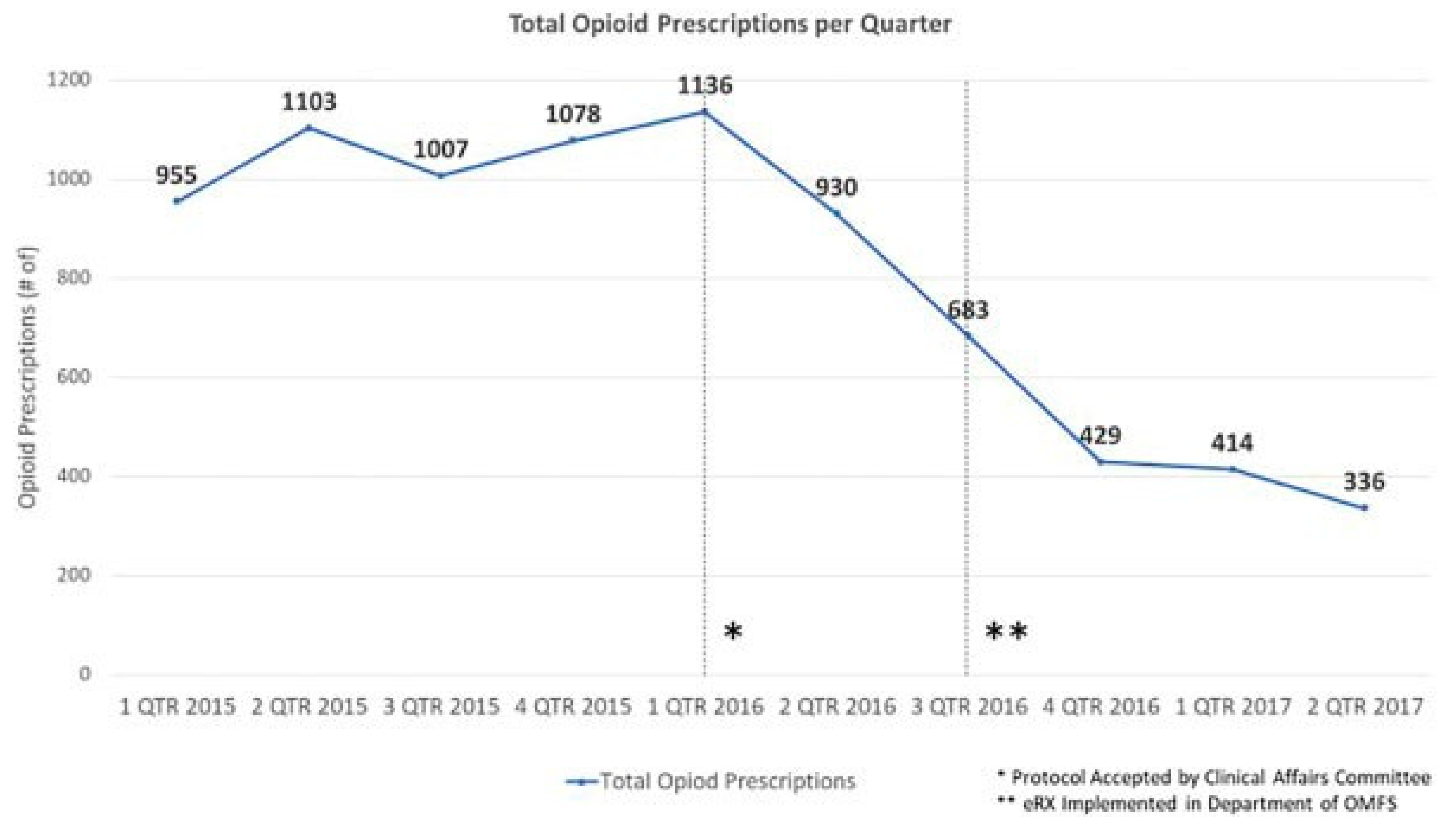
Figure 1.
Total number of opioid prescriptions written by the University of Minnesota School of Dentistry from January 1, 2015, to May 31, 2017 displayed by quarter.
Figure 1.
Total number of opioid prescriptions written by the University of Minnesota School of Dentistry from January 1, 2015, to May 31, 2017 displayed by quarter.
Results
The University of Minnesota School of Dentistry made 5,279 total opioid prescriptions across all departments in the five quarters prior to the introduction of the opioid protocol in February 2016. In the five quarters following implementation, 2,792 total opioid prescriptions were written, resulting in a 47.1% overall decrease in the number of prescriptions written. A decrease in the number of opioid prescriptions is observed beginning in the first quarter of 2016 (
Figure 1).
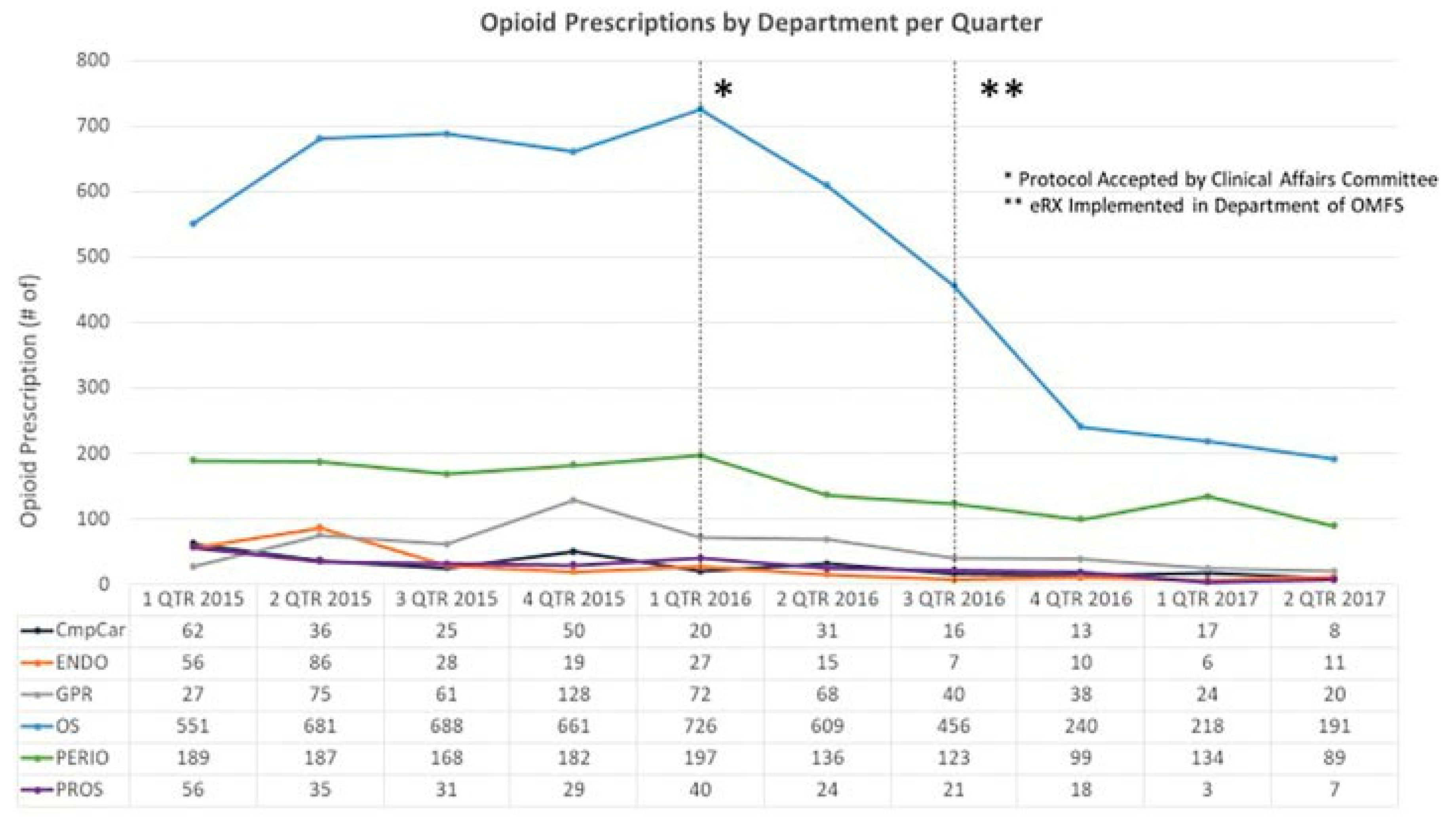
Department of Oral and Maxillofacial Surgery constituted an average 61.1% of all opioid prescriptions in the School of Dentistry. Periodontics (PERIO) followed second with 20.2%. The remaining departments prescribed less than 10% of the opioids as follows: General Practice Residency (GPR), 6.8%; Comprehensive Care (CmpCare), 3.4%; Prosthodontics (PROS), 3.1%; Endodontics (ENDO), 3.0%; and other, 2.0% (
Figure 2).
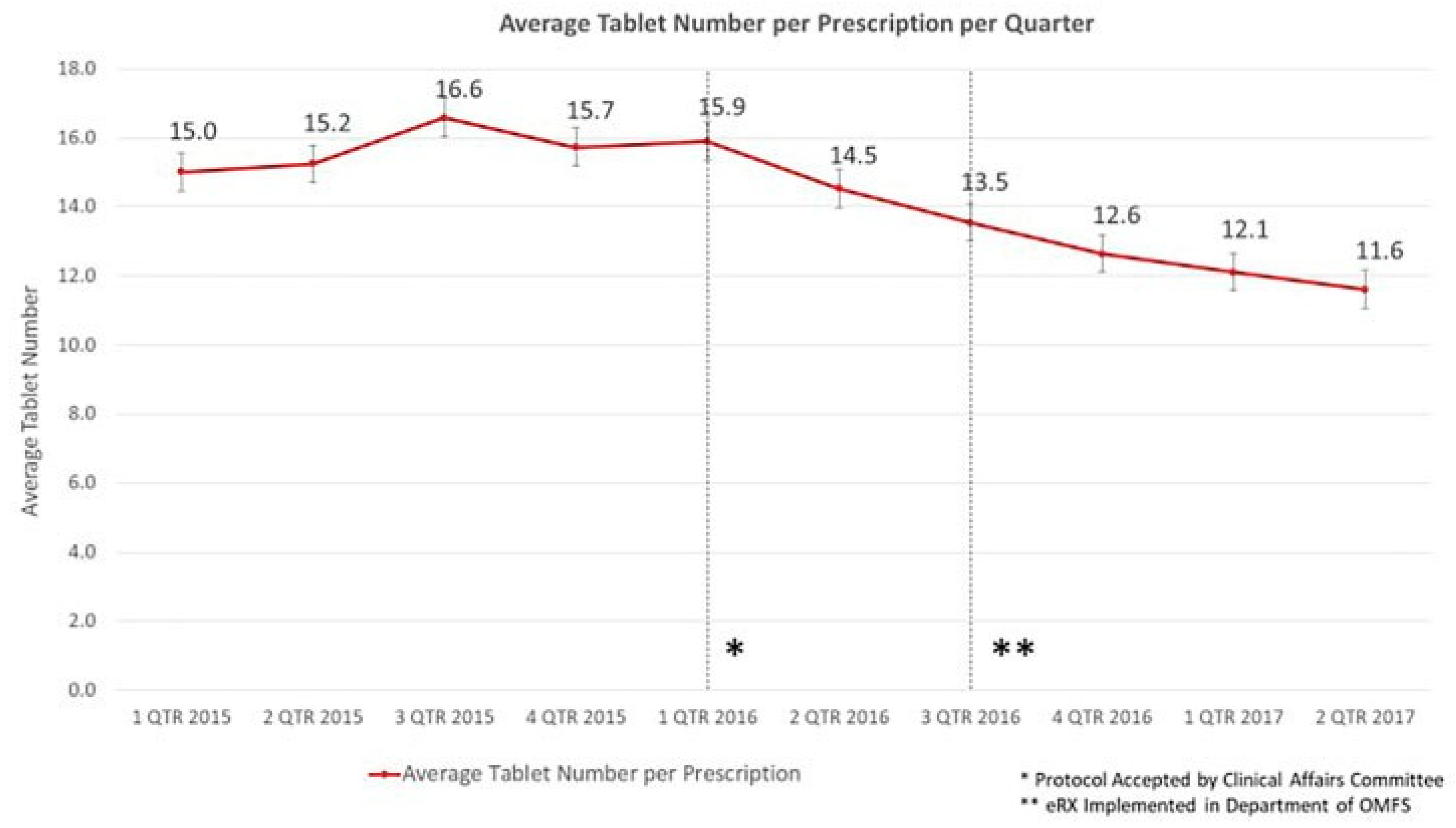
There was an overall decrease observed in the number of tablets prescribed per opioid prescription and the variance of tablet prescribed. The pre-protocol prescriptions averaged 16.3 tablets ( standard deviation [SD]: 10.72) and the post-protocol prescriptions averaged 13.2 tablets (SD: 6.3), an overall decrease of 17.9% (
p < 0.001). Variance decreased from 114.9 to 39.2 (F [17,800] ¼ 195.39,
p < 0.001). A linear decrease in average pill number per prescription was observed from the introduction of the opioid protocol (
Figure 3). The number of tablets prescribed per prescription varies by department (
Figure 4).
Figure 2.
Opioid prescriptions by department per quarter (n ≥ 100 prescriptions per quarter).
Figure 2.
Opioid prescriptions by department per quarter (n ≥ 100 prescriptions per quarter).
Figure 3.
Overall average number of tablets per prescription written by the University of Minnesota School of Dentistry from January 1, 2015, to May 31, 2017 displayed by quarter.
Figure 3.
Overall average number of tablets per prescription written by the University of Minnesota School of Dentistry from January 1, 2015, to May 31, 2017 displayed by quarter.
Percent opioid prescriptions of total prescriptions decreased following protocol (
Figure 5). All departments reported decreases in both opioid prescriptions and average number of tablets per prescription pre- and post-protocol implementation (
Figure 5). Comparing the 15 months preceding the protocol to the 15 months following, Endodontics reported a decrease in opioid prescriptions (77.3%) followed by Prosthodontics (61.6%), Comprehensive Care (56.0%), Oral and Maxillofacial Surgery (48.2%), General Practice Residency (47.7%), and Periodontics (37.1%). Department of Oral and Maxillofacial Surgery reported the greatest decrease in the number of tablets per prescription (22.8%) followed by General Practice Residency (21.1%), Endodontics (19.6%), Periodontics (18.9%), Prosthodontics (15.5%), and Comprehensive Care (9.9%). Refill prescriptions were negligible (
n ≤ 5) across all quarters.
Figure 4.
Average pill number per prescription by department per quarter (n ≤ 100 tablets per prescription).
Figure 4.
Average pill number per prescription by department per quarter (n ≤ 100 tablets per prescription).
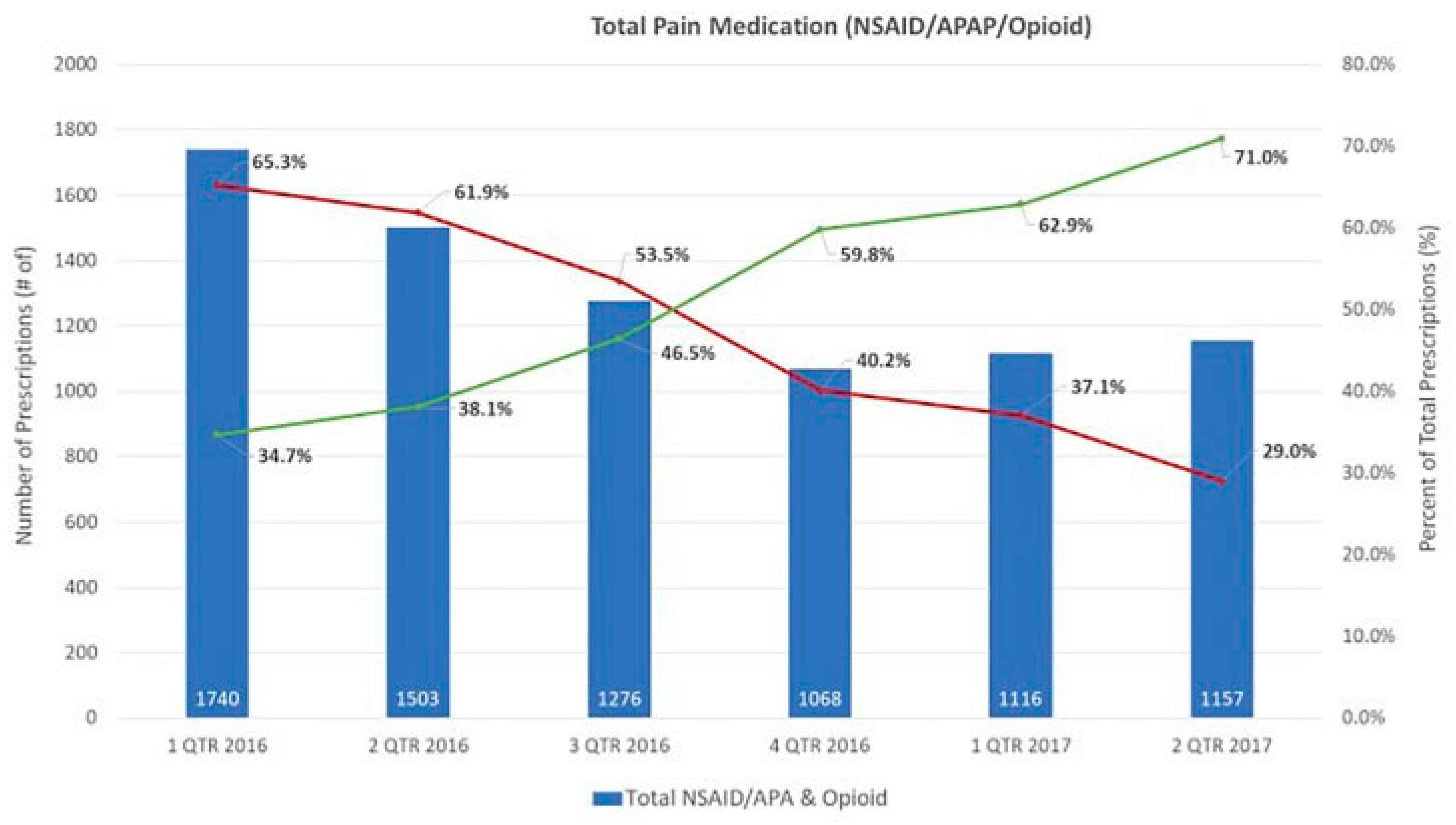
Figure 5.
Total prescriptions and total opioid prescriptions per quarter. Percentage of prescriptions which were opioids displayed per quarter.
Figure 5.
Total prescriptions and total opioid prescriptions per quarter. Percentage of prescriptions which were opioids displayed per quarter.
Faculty headcounts including adjuncts were reported to be 264 (October 2014), 266 (October 2015), and 251 (October 2016).
Discussion
In the five quarters following implementation of the protocol, there was an observed decrease in prescriptions for each quarter. Initially, decreases were more significant and have now started to level off. Average tablet number per prescription has also decreased significantly and a significant decrease in the variance of tabletsper prescriptionwas also noted. These results support the hypothesis that an opioid prescribing protocol can be successful in decreasing the total number of opioid prescriptions, the number of tablets dispensed per prescription, and prescriber variance while appropriately addressing acute postoperative pain. Anecdotally, no increase in after-hour calls or return visits for inadequate pain control was noted; further investigation is warranted.
Conclusion
The dental field has an opportunity to play a significant role in reducing access to opioid medications. Improving opioid prescribing education, implementation of mitigation strategies, consistent patient education, and the use of PDMPs have the potential to decrease variance in prescribing opioids in the community. The use of an opioid-prescribing protocol can help providers appropriately prescribe opioids with the goal to adequately treat postoperative pain and limit unused medication. The protocol was adopted by the clinical affairs committee in the first quarter of 2016 and an immediate decrease in the number of opioid prescriptions written was observed. This was likely due to the education that departments received regarding the protocol and the increased awareness of evidence-based dental pain management.
There was no significant decrease of opioid prescriptions in response to the OPIP in the first quarter of 2015. This legislation required providers to use the PDMP and set guidelines for safe opioid prescribing (OPIP 2016). A 12% decrease in schedule II opioids across Minnesota was reported from 2015 to 2016 (MN PMP). While it is possible that the OPIP legislation affected our results, the protocol is likely the significant contributor as decreases in prescriptions at the University were not observed until the third quarter of 2016, immediately following presentation and training on the prescribing protocol. The implementation of eRx (electronic prescribing), which acts similar to the PDMPs prescription database, as part of the prescribing protocol likely affected prescribing behavior; however, departments which had not yet enrolled in eRx reported similar decreases in prescriptions as those who did. Faculty turnover was negligible. These results highlight the need for a multisystem approach to help reduce the number of opioid prescriptions prescribed by the dental community, while still treating pain adequately.
The Opioid Prescribing Protocol implemented at the University of Minnesota School of Dentistry has shown that the adoption of a prescribing protocol could further help reduce the number of opioid prescriptions and number of tablets per prescription. An opioid-prescribing protocol guides dentists on appropriate and responsible opioid-prescribing patterns, and acts as a tool that they can utilize to compare their prescribing patterns with set guidelines found to be successful in managing acute postoperative pain. Providers increasingly elected to use NSAIDs as first-line postoperative analgesics following the protocol (
Figure 6). The decrease in opioid prescriptions accounted by a marked increase in NSAID prescriptions support our hypothesis. The significant decrease in variance also supports the efficacy of the protocol in educating providers. Implementing a specific opioid protocol for the treatment of postoperative pain can significantly decrease the number of opioid prescriptions, number of tablets per prescription, and prescriber variance in dental clinics.
Figure 6.
Total nonsteroidal anti-inflammatory drug (NSAID), (Acetaminophen) acetyl-para-aminophenol (APAP), and opioid prescriptions worth percent of NSAID/APAP prescriptions and opioid prescriptions per quarter.
Figure 6.
Total nonsteroidal anti-inflammatory drug (NSAID), (Acetaminophen) acetyl-para-aminophenol (APAP), and opioid prescriptions worth percent of NSAID/APAP prescriptions and opioid prescriptions per quarter.
Adequately managing acute postoperative pain requires, at times, the use of opioids. It has been our goal to develop guidelines that aid providers in discerning which procedures and patients require opioids for adequate postoperative pain management, the goal being to decrease the number of exposures to addictive medication. Our protocol was developed with the indications that NSAIDs and acetaminophen should be the first-line analgesic therapy when not contraindicated, as they have been shown to be effective in producing adequate postoperative analgesia. We were careful to allow for the use of opioids, but indications for the use of opioids as first line for acute postoperative pain requires documentation.
Poorly controlled postoperative pain is of great concern and our study closely monitored after-hour calls along with postoperative phone calls regarding pain management and the need for secondary prescriptions or secondary opioid medications. There has been no noticeable increase in after-hour calls or secondary prescriptions as of this date. The findings of the study suggest that unused opioids prescribed by dentists may be contributing to the national problems of misuse, abuse, diversion, and addiction. The protocol was met with acceptance throughout most of the practitioners within the School of Dentistry and from the public. There were concerns voiced about postoperative pain control and patients’ acceptance. This has not been observed, and in fact more and more patients, and parents of patients, have been asking to not have any opioids prescribed after the procedure.
Limitations of our study include those prescriptions not correctly entered in Axium along with human error. Only tablet-based prescriptions were included. While faculty turnover was limited, we cannot completely rule out the effect of changing faculty. It is also difficult to isolate other factors which would affect provider behavior, such as outside education, opioid awareness, etc. Demographic data were collected on a limited basis and could have altered results. While there are noted limitations, we believe the large samples size, long data range, and low p-values support the significance of the protocol’s effects on prescriber behavior at the University of Minnesota. Future research into the effect of PDMP on tablet averages and variance could substantiate the effectiveness of a PDMP. A survey of providers could offer insight into what prescribers report was the motivating factor behind change in behavior. Understanding which procedures were correlated with opioid decreases would help us appreciate which providers opted to prescribe an opioid less frequently. A study on patient satisfaction with education and pain treatment under the protocol could offer us more information on the efficacy of the protocol to manage pain effectively, compared with opioids.