Since its advent in the 1980s [
1], advanced three-dimensional (3D) computer technologies have transformed plastic surgery and other healthcare fields byadvancing surgical technique [
2,
3,
4]. With significant progress in computed tomographic (CT) imaging [
5] and the developmentof rigid biomaterials [
6,
7], specific advances have been seen in craniofacial reconstruction [
8,
9,
10]. Modern computer-aided virtual surgical planning, 3D modeling, and printed patient custom implants (PCIs) are now employed with some frequency to enhance the diagnostic analysis, anatomic orientation, patient consent, individualized planning, virtual and physical simulation, augmentation of tissues, and educational yield in craniofacial surgery [
2,
3,
4,
8,
9,
10].
There are multiple reports in the literature of the use of advanced 3D computer technology using PCIs for the reconstruction of orbital defects after trauma [
11,
12,
13], though few report cases of reoperative trauma [
11,
13], and none describe the simultaneous single-stage reconstruction of multiple associated periorbital defects. We present a reoperative case of complex posttraumatic orbital, zygomaticomaxillary complex, and frontal bone deformities, which was analyzed and repaired using 3D technology.
Case Study
This case was reviewed in accordance with ethical standards of clinical research as outlined by the University of Tennessee Institutional Review Board. A 50-year-old man presented to our craniofacial referral center 3 months after two failed attempts at open reduction and internal fixation of complex leftorbital, zygomatic, and frontal bonefractures sustained in a motorcycle accident. The patient reported debilitating diplopia, recurrent nausea when using both eyes, and was dependent on eye patch to perform his job as a welder. Preoperative evaluation demonstrated left enophthalmos, left lateral canthal displacement, lower eyelid ectropion, vertical orbital dystopia, and a laterally and inferiorly displaced, comminuted zygoma with multiple bone defects (
Figure 1 and
Figure 2). He displayed a drooping appearance in his left upper and midface combined with periorbital scarring. The patient’s primary therapeutic goal was correction of diplopia, but he also desired improvement in facial appearance.
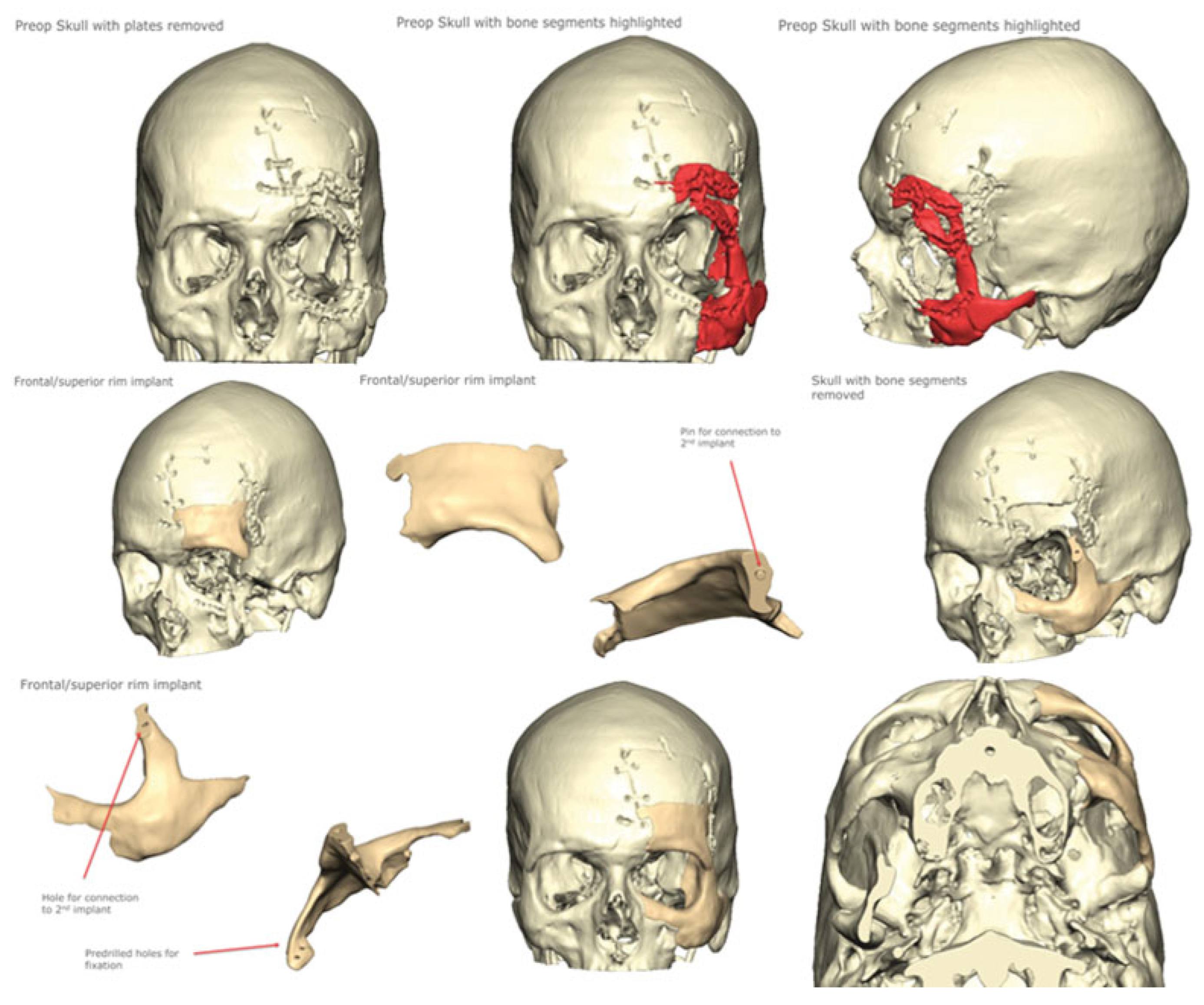
Advanced 3D computerized technology was employed for diagnostic assessment, preoperative planning, virtual surgical planning with computer-aided simulation of results, and fabrication of a PCI (KLS Martin, Inc.;, Jacksonville, FL;
Figure 1) [
14]. Our craniofacial protocol of CT images (1.5-mm-thickcuts) was transferred via secure cloud computing using a Digital Imaging and Communications in Medicine Image File (.dcm. “DICOM”). Virtual manipulation of these images during a computer-aided planning session was then conducted online with a biomedical computer engineering specialist. The PCI was designed by segmental mirroring [
11,
12,
13] of the contralateral periorbital anatomy to approximate the premorbid left orbit, zygoma, and frontal bone.
A two-part PCI with interlocking frontal and zygomatic segments was fabricated based on this mirrored image from polyether ether ketone (PEEK; ISO 10993 specifications) using an additive manufacturing method [
14]. Contoured radial titanium mesh designed by the senior author (L.S.) [
15,
16] was then rigidly secured to the implant with micro-screw fixation to the infraorbital rim to establish exact internal orbital symmetry compared with the opposite orbit. Prior to intraoperative placement, the radial mesh is removed with screw holes serving as an exact guide for orbital floor position. Physical simulation of the operation was conducted on a 3D-printed skull model fashioned from the preoperative craniofacial CT scan. The left periorbital bony defect was corrected by placement of the PCI preoperatively. The 3D model and PCI were then sterilized and used as guides intraoperatively to aid in the reconstruction.
Figure 1.
Virtual surgical planning process.
Figure 1.
Virtual surgical planning process.
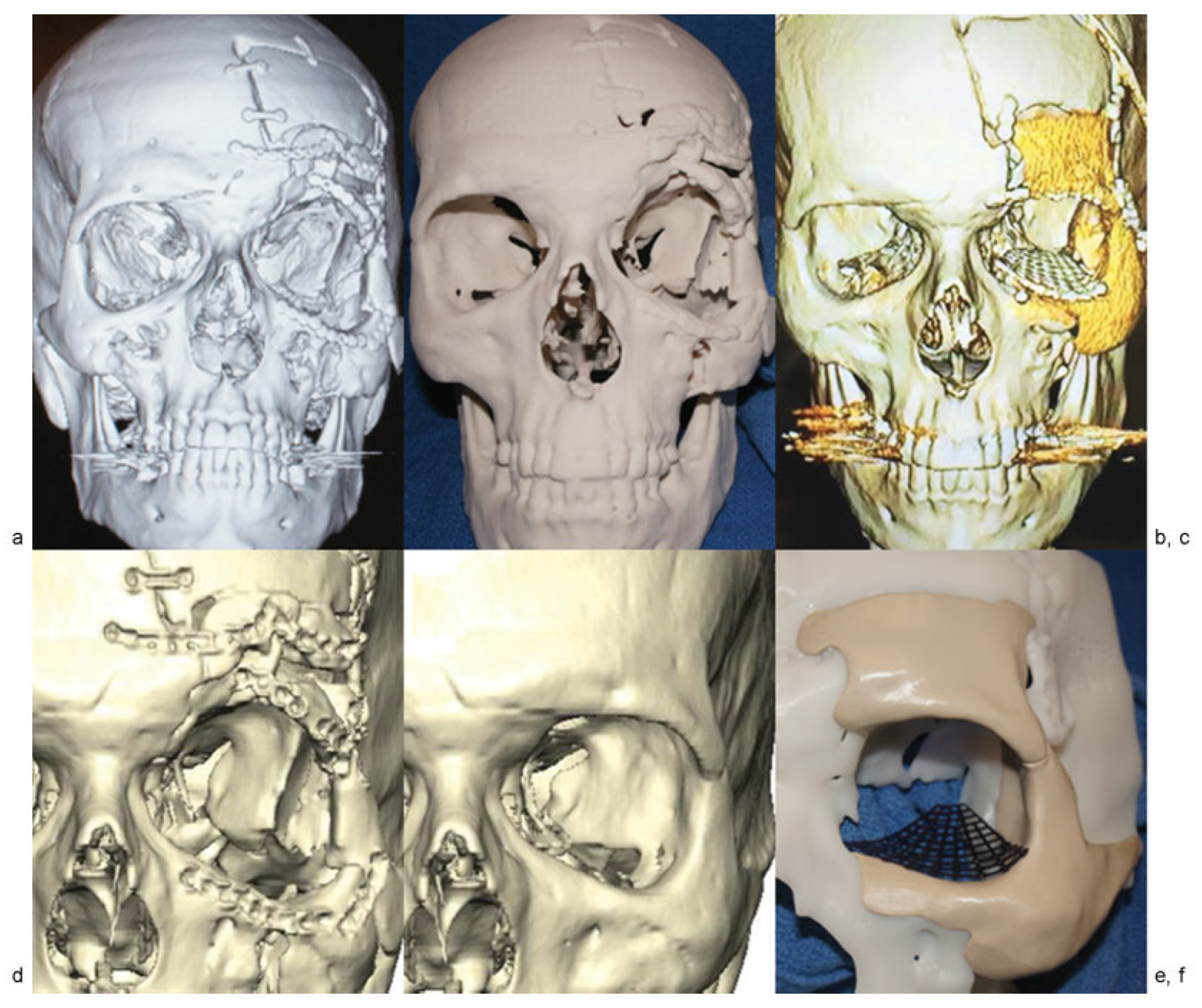
Figure 2.
(a–f) Before and after imaging, model, and custom implant.
Figure 2.
(a–f) Before and after imaging, model, and custom implant.
The patient underwent reopening of the previous bicoronal and lower eyelid incisions to provide sufficient exposure, which included complete takedown of the temporalis muscle, removal of multiple previous reduction plates, microscrews, and comminuted bone fragments. Owing to severe comminution with insufficient bone stock, portions of the left supraorbital frontal bone and body of the left zygoma were removed via debridement and osteotomy. The two piece PCI was inserted by positioning and rigidly fixing the supraorbital and frontal bone segment first. The zygomatic portion of the PCI was then locked in place to the frontal bone segment and rigidly secured to the patient’s native bone using lag screw and miniplate fixation. A contoured titanium mesh (formed and positioned preoperatively) was inserted to reconstruct the orbital floor and secured to the PCI’s infraorbital rim with micro-screws using predrilled holes as a guide. The cheek and eyelid soft tissue was then resuspended with multiple sutures to bone, and a lateral canthopexy was performed.
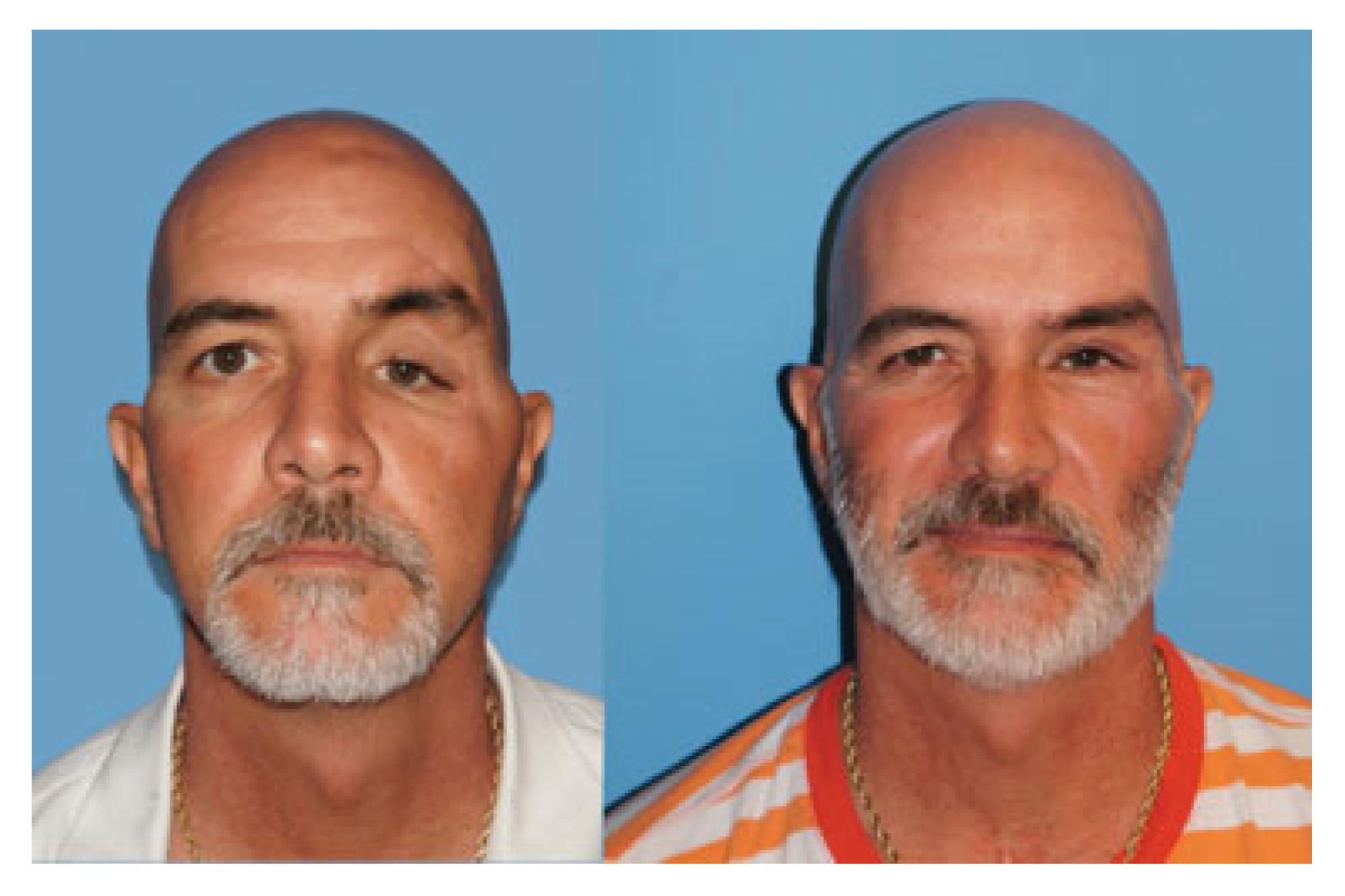
The postoperative course was uneventful, and the patient was discharged the following day. He subsequently underwent correction of traumatic left upper eyelid ptosis with plication of the levator tendon. Following the aforementioned procedures, the patient experienced complete resolution of his diplopia with correction of posttraumatic facial deformities (
Figure 3). He was able to discontinue use of the eye patch and resume normal work responsibilities without restrictions.
Discussion
We present a clinical case treated at a tertiary craniofacial referral center using advanced 3D computerized technology for the diagnostic assessment, preoperative planning, virtual surgical planning with computer-aided simulation of results, and fabrication of a PCI (KLS Martin, Inc.;
Figure 1) [
14]. This case illustrates the use of advanced 3D computer technology in the reconstruction of a complex orbital deformity after previous attempts at posttraumatic reduction. The employment of state-of-the-art computer planning and 3D modeling enhanced this patient’s preoperative planning by enabling the analysis and simulation of the operation in both the virtual and physical environment.
Figure 3.
Before and after photographs.
Figure 3.
Before and after photographs.
Owing to the reoperative nature of this case in the setting of deficient, comminuted native bone stock, we elected to use a PCI to reconstruct the left periorbital region, zygoma, and affected frontal cranium. The native bone was severely comminuted and displaced, including bone defects and multiple small deformed bone fragments. Multiple osteotomies, repositioning, and splint calvarial bone grafting were considered as an option. We chose the custom implant due to the irregular and deformed nature of the existing bone. The PCI avoided the time required to harvest and contour bone grafts with no chance of the resorption or remodeling of these grafts that can occur in the long term. Posttraumatic orbital reconstruction with 3D technology has been reported previously [
11,
12,
13], though not with simultaneous reconstruction of this degree of periorbital trauma with a PEEK PCI.
Previous authors have noted the utility of PEEK in craniofacial reconstruction, given its close approximation to the physical properties of human cortical bone [
6,
7]. While there is a risk of infection or extrusion of any alloplastic implant, we feel there are certain keys to its successful use. These implants should not be used if there is exposure to any sinus; autogenous bone grafts would then be our choice. Rigid fixation of the implant to existing stable bone is crucial, with normal or undamaged soft-tissue coverage key to long-term success. While long-term follow-up (10–20 years) is needed, the senior author has had excellent results following the aforementioned principles in short-term follow-up (4–5 years).
Blumer et al. [
11], Park et al. [
12], and Zhang et al. [
13], have also reported the use of segmental mirroring to reapproximate the orbital anatomy based on the unaffected contralateral side. There are inherent drawbacks to the use of advanced 3D computer technology, including increased cost, risks associated with the use of alloplastic biomaterials, and unexpected discrepancies between simulated and actual operative results [
2,
3,
4,
8,
9,
10]. This is a pitfall that may be encountered, as these highly precise PCIs are fitted among inherent technical challenges for accurate surgical placement. Custom osteotomy guides may be utilized, as needed, to optimize placement accuracy. This case required meticulous attention to detail to establish the appropriate fit between the implant and native bone with the use of a custom 3D skull model intraoperatively. The removal of bone fragments and PCI placement was tested on the model and did not require any recontouring intraoperatively. Both implants were rigidly fixed in place with screws and plates. There was no exposure to sinuses, and meticulous attention to soft-tissue redraping and suspension was performed. It is also important to note that the employment of 3D technology does not absolve the surgeon from the use of sound clinical principles in operative planning and execution. We have demonstrated that computerized virtual planning, 3D models, and PCI may safely enhance the planning, simulation, and execution of reoperative, posttraumatic periorbital reconstruction with excellent functional and aesthetic results.
Computer-aided 3D reconstruction is a burgeoning field in craniofacial surgery characterized by advanced technology for the optimal correction of a wide array of deformities [
8,
9,
10]. The current challenges faced by practitioners include the production of high-quality evidence to define criteria warranting the use of 3D technologies and standards of production of PCIs. Other issues to consider are the value of 3D reconstructive technologies in medical education, the optimal biomaterials for use in PCIs, and long-term outcomes of this approach [
2,
3,
4,
8,
9,
10,
17].
Conclusion
Modern 3D technology allows the surgeon to better analyze complex periorbital deformities and precisely plan surgical correction with the option of printing custom bone implants. These techniques were successfully applied in a reoperative case of debilitating diplopia after traumatic injury with excellent aesthetic and functional results. Further application of advanced 3D computer technology can potentially improve the results of severe periorbital traumatic reconstruction and warrants further study.
Note
This articlewas orally presented at the Southeastern Society of Plastic and Reconstructive Surgeons 59th Annual Scientific Meeting, Lake Buena Vista, Florida, 12 June 2016.