A Hemangioma of the Zygomatic Bone: Management Ensuring Good Reconstructive and Aesthetic Results
Abstract
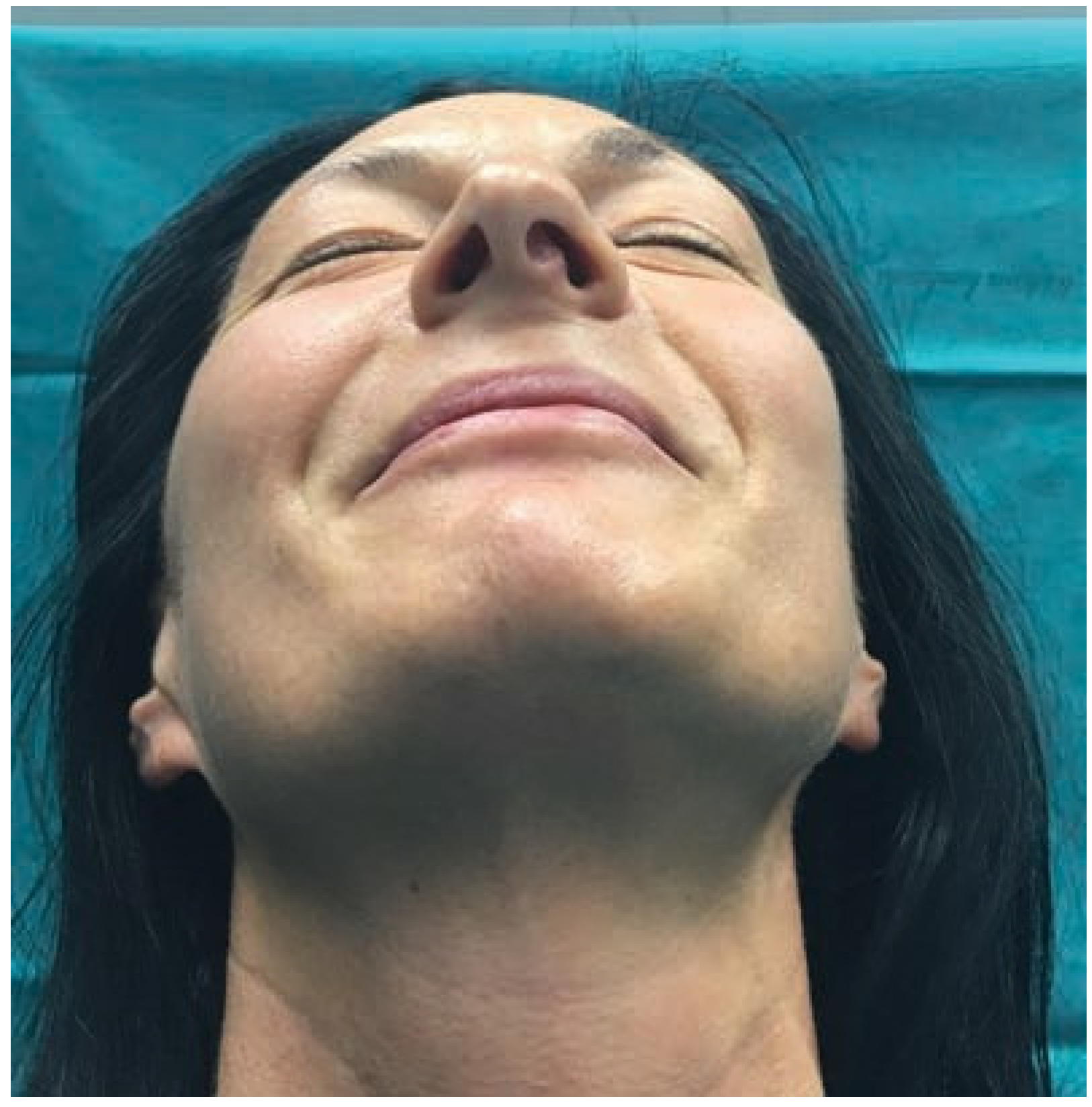
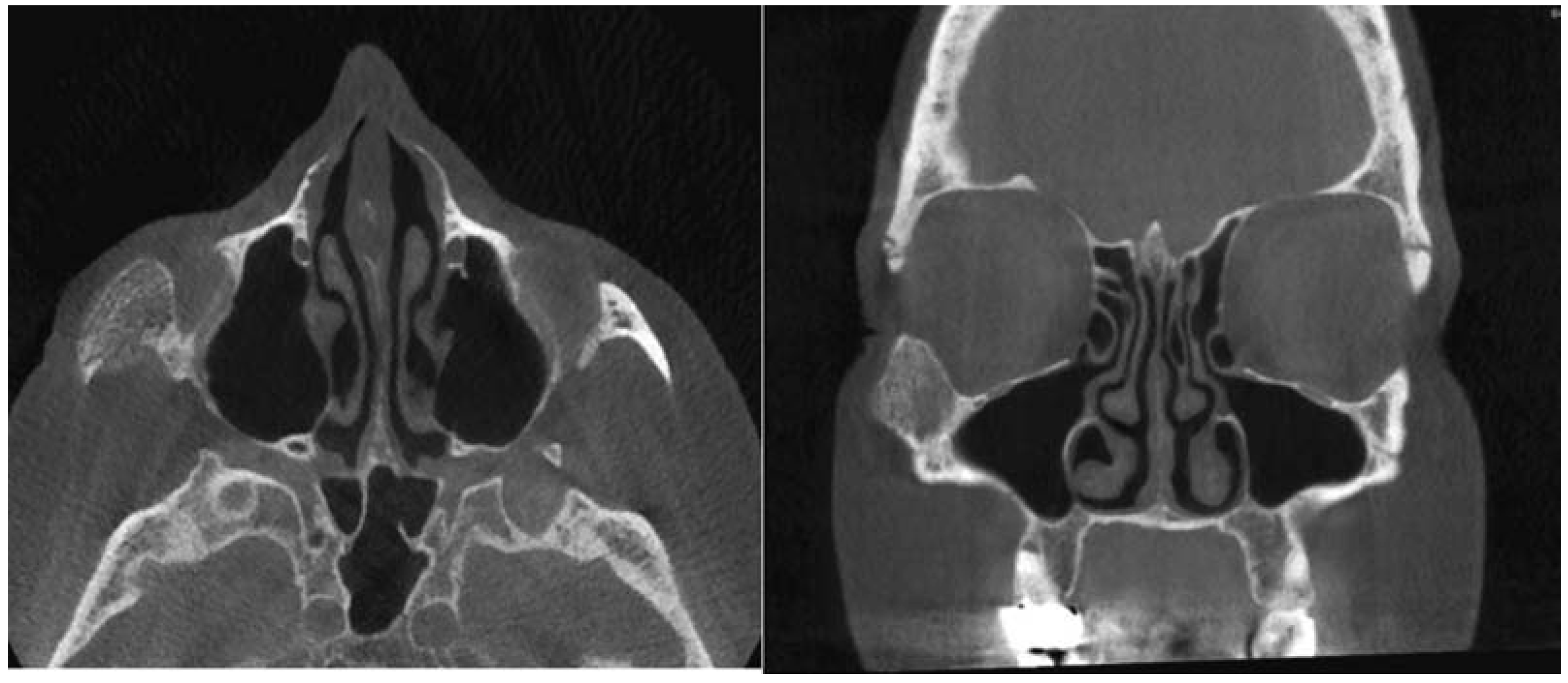
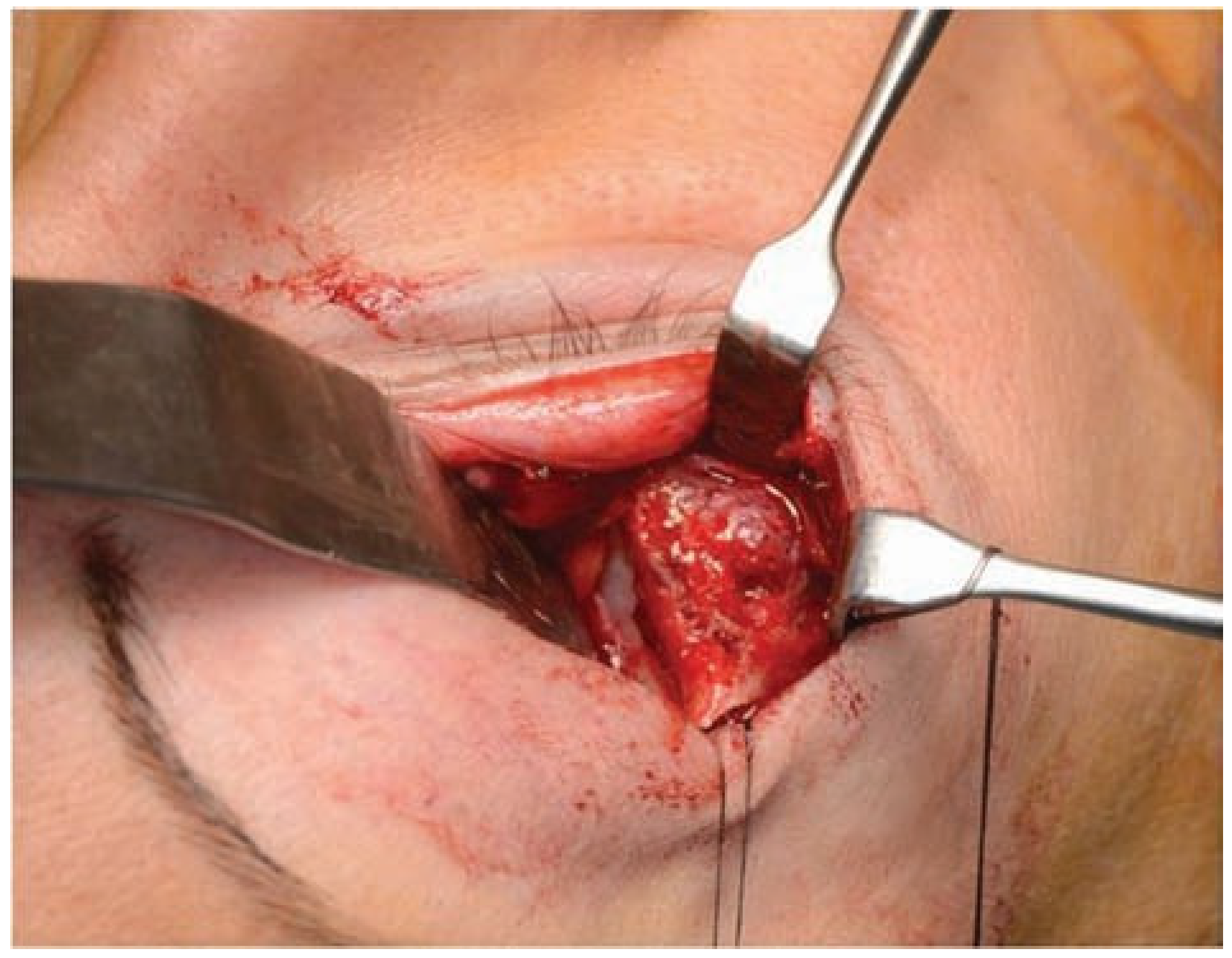
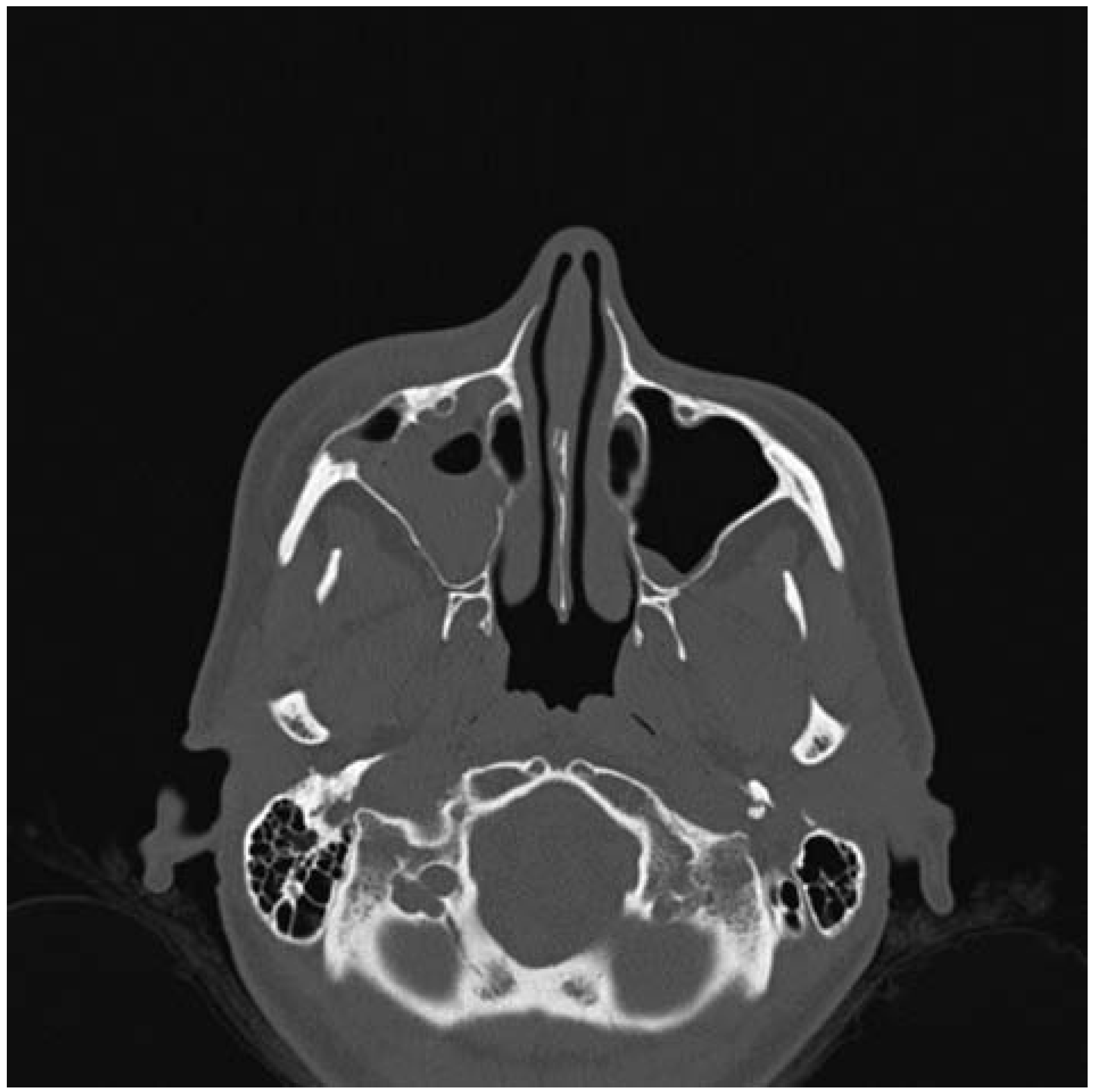
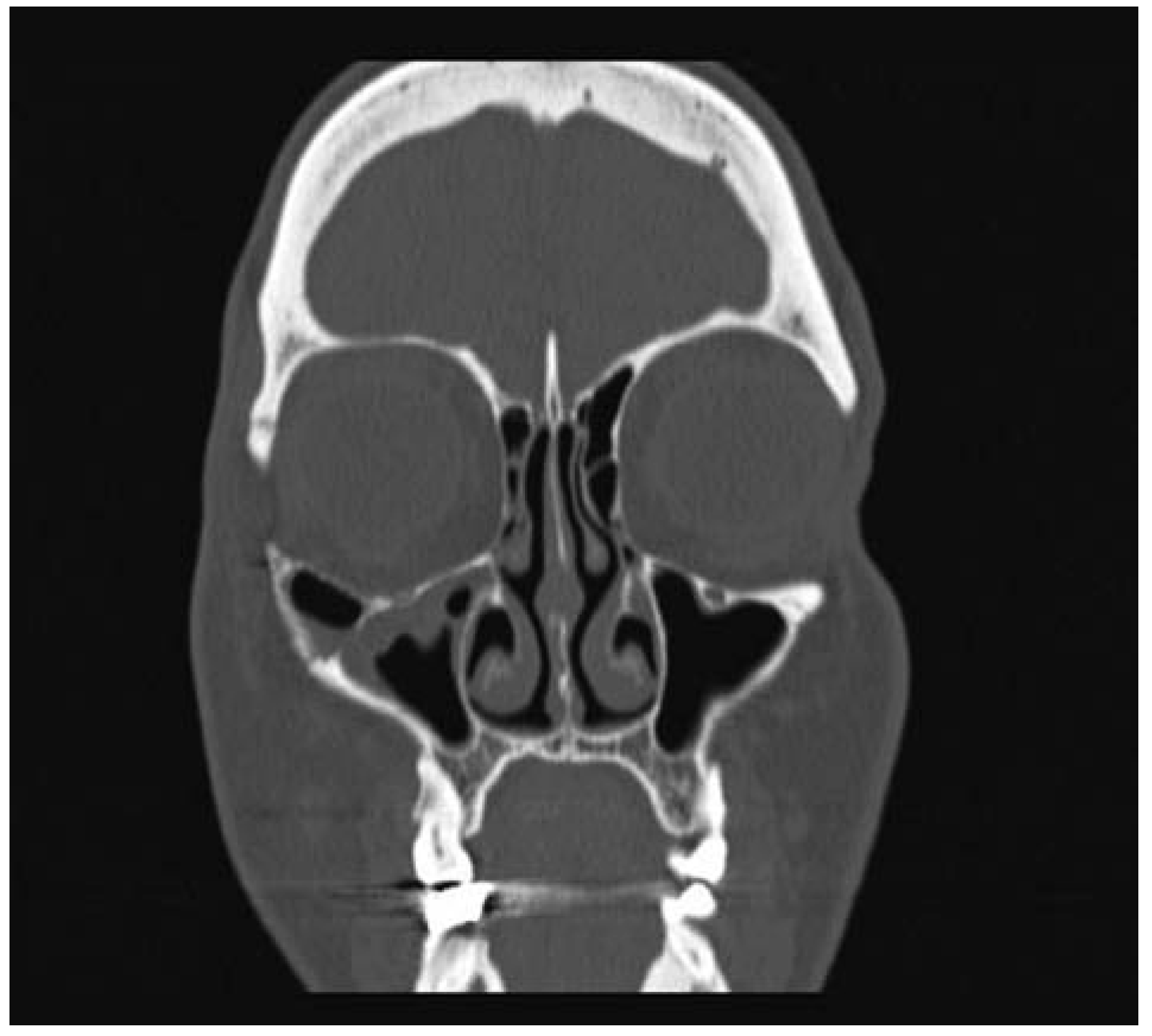
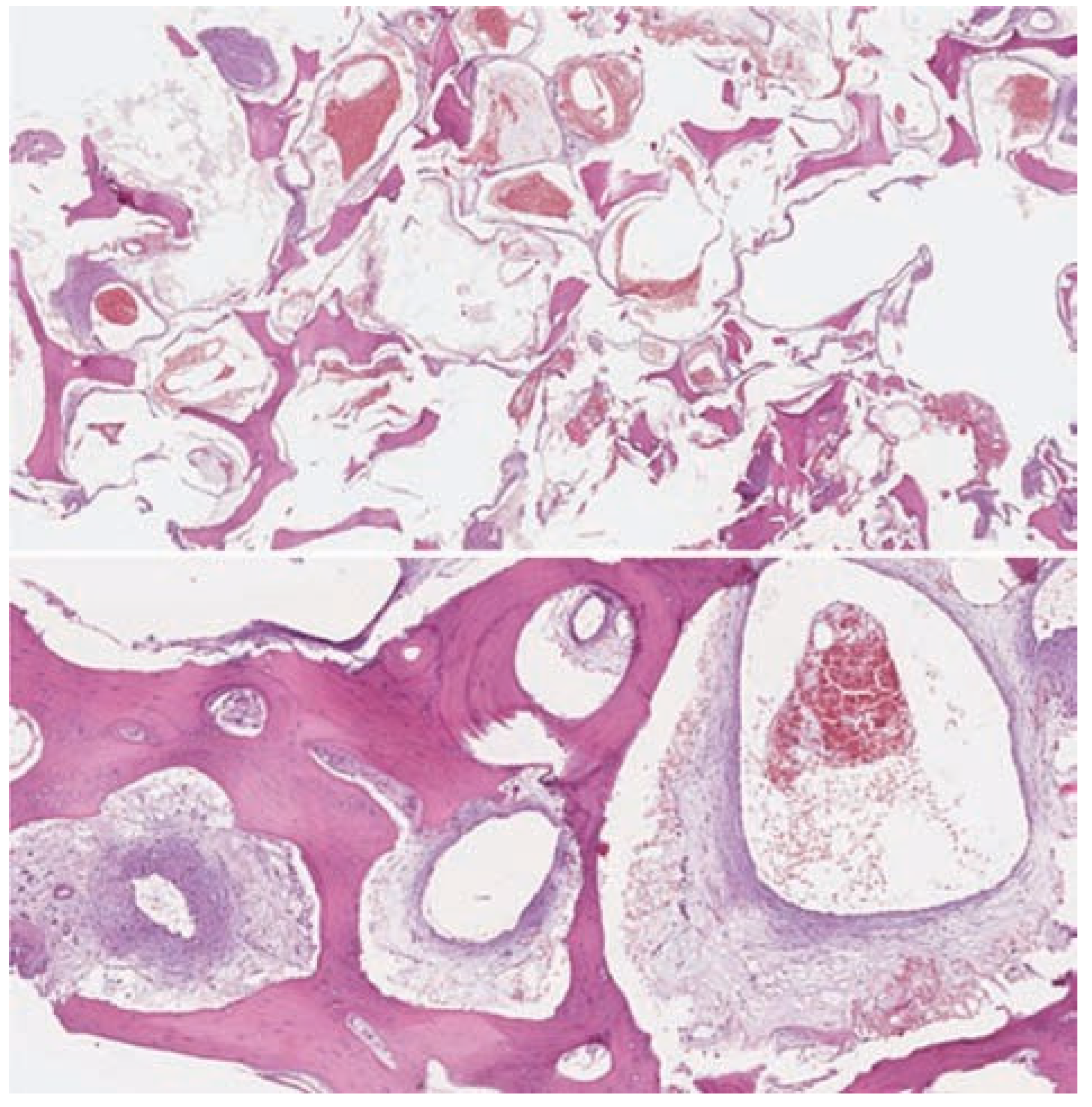
:Case Presentation
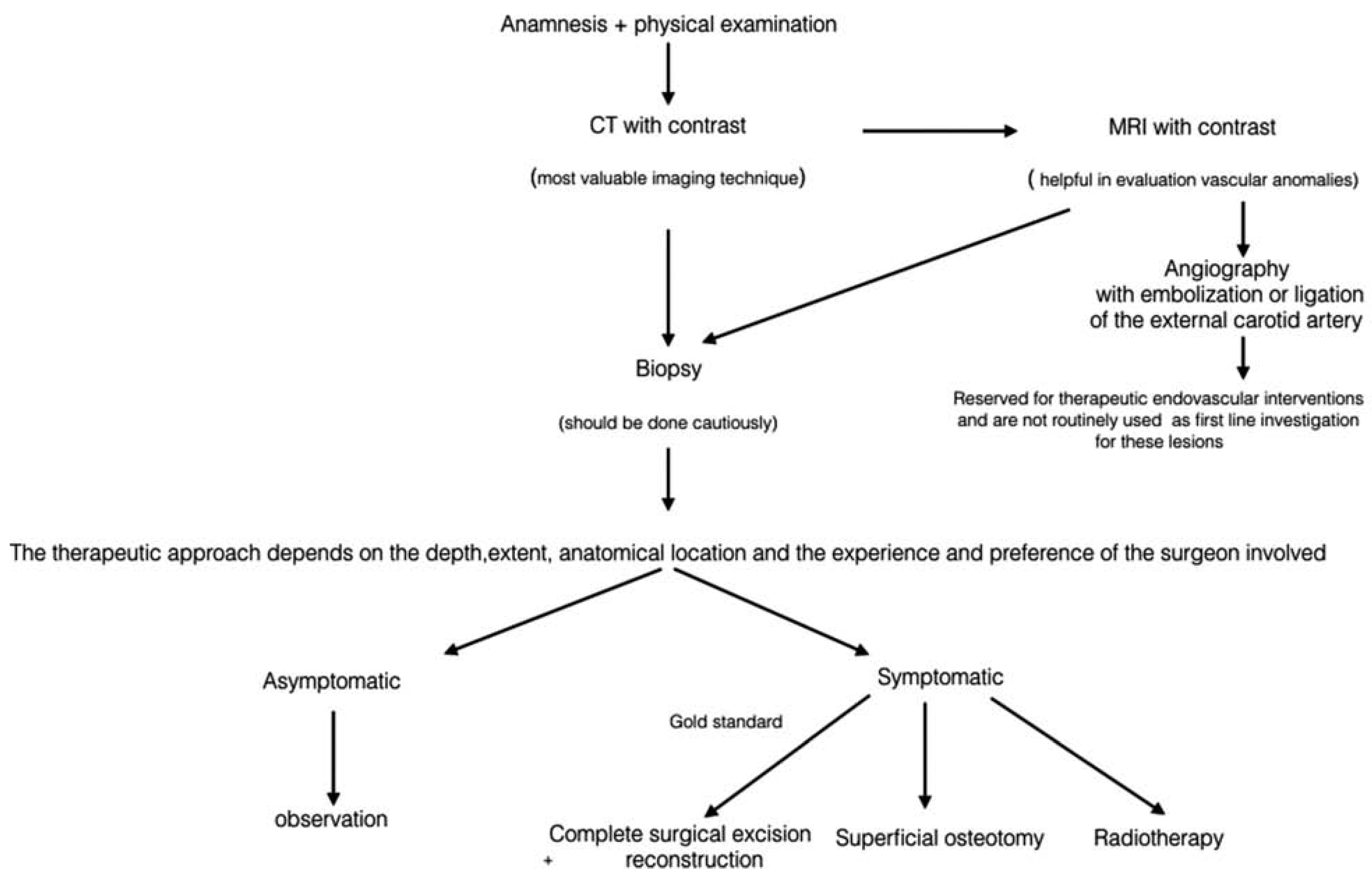
Discussion
Conclusions
Note
References
- Srinivasan, B.; Ethunandan, M.; Van der Horst, C.; Markus, A.F. Intraosseous ‘haemangioma’ of the zygoma: More appropriately termed a venous malformation. Int J Oral Maxillofac Surg 2009, 38, 1066–1070. [Google Scholar] [CrossRef]
- Yu, M.S.; Kim, H.C.; Jang, Y.J. Removal of a nasal bone intraosseous venous malformation and primary reconstruction of the surgical defect using open rhinoplasty. Int J Oral Maxillofac Surg 2010, 39, 394–396. [Google Scholar]
- Wassef, M.; Vanwijck, R.; Clapuyt, P.; Boon, L.; Magalon, G. Vascular tumours and malformations, classification, pathology and imaging [in French]. Ann Chir Plast Esthet 2006, 51, 263–281. [Google Scholar] [PubMed]
- Moore, S.L.; Chun, J.K.; Mitre, S.A.; Som, P.M. Intraosseous hemangioma of the zygoma: CT and MR findings. AJNR Am J Neuroradiol 2001, 22, 1383–1385. [Google Scholar] [PubMed]
- Kim, T.H.; Lim, E.J.; Lee, J.K.; Lee, J.G.; Han, M.H. Intraosseous hemangioma of the middle turbinate misdiagnosed as a nasal polyp. Case Rep Otolaryngol 2014, 2014, 217349. [Google Scholar]
- Dhupar, V.; Yadav, S.; Dhupar, A.; Akkara, F. Cavernous hemangioma– uncommon presentation in zygomatic bone. J Craniofac Surg 2012, 23, 607–609. [Google Scholar] [PubMed]
- Toynbee, J. An account of two vascular tumors developed in the substance of bone. Lancet 1845, 2, 676. [Google Scholar]
- Schofield, A.L. Primary hemangioma of the malar bone. Br J Plast Surg 1950, 3, 136–140. [Google Scholar]
- Mulliken, J.B.; Glowacki, J. Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. Plast Reconstr Surg 1982, 69, 412–422. [Google Scholar] [CrossRef]
- Mulliken, J.B.; Fishman, S.J.; Burrows, P.E. Vascular anomalies. Curr Probl Surg 2000, 37, 517–584. [Google Scholar]
- Enjolras, O.; Mulliken, J.B. Vascular tumors and vascular malformations (new issues). Adv Dermatol 1997, 13, 375–423. [Google Scholar]
- Enjolras, O.; Wassef, M.; Chapot, R. (Eds.) Introduction: ISSVA classification. In Color Atlas of Vascular Tumors and Vascular Malformations; Cambridge University Press: New York, NY, 2007; pp. 1–11. [Google Scholar]
- Kaya, B.; Işılgan, S.E.; Cerkez, C.; Otrakçı, V.; Serel, S. Intraosseous cavernous hemangioma: A rare presentation in maxilla. Eplasty 2014, 14, e35. [Google Scholar] [PubMed]
- Park, B.H.; Hwang, E.; Kim, C.H. Primary intraosseous hemangioma in the frontal bone. Arch Plast Surg 2013, 40, 283–285. [Google Scholar] [PubMed]
- Aykan, A.; Keleş, M.K.; Bayram, Y.; et al. Hemangioma of the zygomatic bone. J Craniofac Surg 2016, 27, e200–e202. [Google Scholar] [PubMed]
- Liu, J.K.; Burger, P.C.; Harnsberger, H.R.; Couldwell, W.T. Primary intraosseous skull base cavernous hemangioma. Skull Base 2003, 13, 219–228. [Google Scholar]
- Cheng, N.C.; Lai, D.M.; Hsie, M.H.; Liao, S.L.; Chen, Y.B. Intraosseous hemangiomas of the facial bone. Plast Reconstr Surg 2006, 117, 2366–2372. [Google Scholar]
- Warman, S.; Myssiorek, D. Hemangioma of the zygomatic bone. Ann Otol Rhinol Laryngol 1989, 98 (Pt 1) Pt 1, 655–658. [Google Scholar]
- Razek, A.A. Imaging appearance of bone tumors of the maxillofacial region. World J Radiol 2011, 3, 125–134. [Google Scholar] [PubMed]
- Gonçalves, F.G.; Rojas, J.P.; Hanagandi, P.B.; et al. Case report: Periorbital intraosseous hemangiomas. Indian J Radiol Imaging 2011, 21, 287–290. [Google Scholar]
- Ramchandani, P.L.; Sabesan, T.; Mellor, T.K. Intraosseous vascular anomaly (haemangioma) of the zygoma. Br J Oral Maxillofac Surg 2004, 42, 583–586. [Google Scholar]
- Firooznia, H.; Golimbu, C.; Rafii, M.; Rauchning, W.; Weinreb, J. MRI and CT of the musculoskeletal system; Mosby: St. Louis, MO, 1992; p. 63. [Google Scholar]
- Dogan, S.; Kocaeli, H.; Sahin, S.; Korfali, E.; Saraydaroglu, O. Large cavernous hemangioma of the frontal bone. Neurol Med Chir (Tokyo) 2005, 45, 264–267. [Google Scholar] [PubMed]
- Top, H.; Aygit, C.; Sarikaya, A.; Karaman, D.; Firat, M.F. Evaluation of maxillary sinus after treatment of midfacial fractures. J Oral Maxillofac Surg 2004, 62, 1229–1236. [Google Scholar] [PubMed]
- Marshak, G. Hemangioma of the zygomatic bone. Arch Otolaryngol 1980, 106, 581–582. [Google Scholar] [PubMed]
- Clauser, L.; Meneghini, F.; Riga, M.; Rigo, L. Haemangioma of the zygoma. Report of two cases with a review of the literature. J Craniomaxillofac Surg 1991, 19, 353–358. [Google Scholar]
- Konior, R.J.; Kelley, T.F.; Hemmer, D. Intraosseus zygomatic hemangioma. Otolaryngol Head Neck Surg 1999, 121, 122–125. [Google Scholar]
- Ethunandan, M.; Mellor, T.K. Haemangiomas and vascular malformations of the maxillofacial region–a review. Br J Oral Maxillofac Surg 2006, 44, 263–272. [Google Scholar]


© 2017 by the author. The Author(s) 2017.
Share and Cite
Bocchialini, G.; Castellani, A.; Bozzola, A.; Rossi, A. A Hemangioma of the Zygomatic Bone: Management Ensuring Good Reconstructive and Aesthetic Results. Craniomaxillofac. Trauma Reconstr. 2017, 10, 332-336. https://doi.org/10.1055/s-0036-1594274
Bocchialini G, Castellani A, Bozzola A, Rossi A. A Hemangioma of the Zygomatic Bone: Management Ensuring Good Reconstructive and Aesthetic Results. Craniomaxillofacial Trauma & Reconstruction. 2017; 10(4):332-336. https://doi.org/10.1055/s-0036-1594274
Chicago/Turabian StyleBocchialini, Gabriele, Andrea Castellani, Anna Bozzola, and Alessandro Rossi. 2017. "A Hemangioma of the Zygomatic Bone: Management Ensuring Good Reconstructive and Aesthetic Results" Craniomaxillofacial Trauma & Reconstruction 10, no. 4: 332-336. https://doi.org/10.1055/s-0036-1594274
APA StyleBocchialini, G., Castellani, A., Bozzola, A., & Rossi, A. (2017). A Hemangioma of the Zygomatic Bone: Management Ensuring Good Reconstructive and Aesthetic Results. Craniomaxillofacial Trauma & Reconstruction, 10(4), 332-336. https://doi.org/10.1055/s-0036-1594274


