Abstract
Traumatic orbital roof fractures are rare and are managed nonoperatively in most cases. They are typically associated with severe mechanisms of injury and may be associated with significant neurologic or ophthalmologic compromise including traumatic brain injury and vision loss. Rarely, traumatic encephalocele or pulsatile exophthalmos may be present at the time of injury or develop in delayed fashion, necessitating close observation of these patients. In this article, we describe two patients with minimally displaced blow-in type orbital roof fractures that were later complicated by orbital encephalocele and pulsatile exophthalmos, prompting urgent surgical intervention. We also suggest a management algorithm for adult patients with orbital roof fractures, emphasizing careful observation and interdisciplinary management involving plastic surgery, neurosurgery, and ophthalmology.
Orbital roof fractures are relatively uncommon, with singleinstitution estimates ranging from 1 to 9% of facial fractures [1,2,3,4,5]. Because frontal and paranasal sinuses prevent direct transmission of forces from the superior orbital rim to the orbital roof, orbital roof fractures tend to occur with high-energy mechanisms and are typically accompanied by injuries to surrounding structures [1,2,3,4,5,6,7,8,9,10]. In particular, there may be significant ophthalmologic and neurologic injuries, including globe rupture, optic neuropathy, retrobulbar hematoma, extraocular muscle entrapment, pulsatile exophthalmos, and severe traumatic brain injury with or without cerebrospinal fluid (CSF) leak and brain herniation [1,2,3,7,9,11]. Early diagnosis and surgical intervention, when indicated, have been shown to be effective in managing orbital roof fractures and minimizing their long-term sequelae [1,3,7,8,9]. However, the majority of orbital roof fractures are successfully managed nonoperatively if they are minimally displaced [2,3,12]. In this article, we present two cases of minimally displaced orbital roof fractures that were initially managed nonoperatively but were later complicated by pulsatile exophthalmos and orbital encephalocele, requiring urgent operative intervention. We also suggest a management algorithm for orbital roof fractures in adults.
Case 1
A 66-year-old woman presented to the emergency department (ED) after being struck by a bicyclist. She had a transient loss of consciousness after striking her head on the ground and complained of headache, neck pain, and nausea and vomiting. She was agitated and oriented only to self, with a Glasgow Coma Scale (GCS) of 14 (E4V4M6). She was noted to have dysphasia and bilateral periorbital ecchymoses without visual or extraocular movement deficits. Pupils were equal, round, and reactive to light, and visual fields were full. The patient declined detailed examination by the ophthalmology team. No CSF rhinorrhea was seen. Computed tomographic (CT) scan revealed bilateral minimally displaced blow-in orbital roof fractures (Figure 1a,b), left subdural hematoma with a 3-mm midline shift (Figure 1c), and a left retrobulbar hemorrhage (Figure 1d). She also had a minimally displaced occipital fracture and bifrontal cerebral parenchymal contusions. There were no other facial fractures or pneumocephalus. The patient received levetiracetam and a hypertonic saline bolus before being admitted to the trauma intensive care unit for monitoring. Her intracranial pressure was managed medically, including head of bed elevation, blood pressure control, and continuous infusion of hypertonic saline. She received hourly neurological examinations.
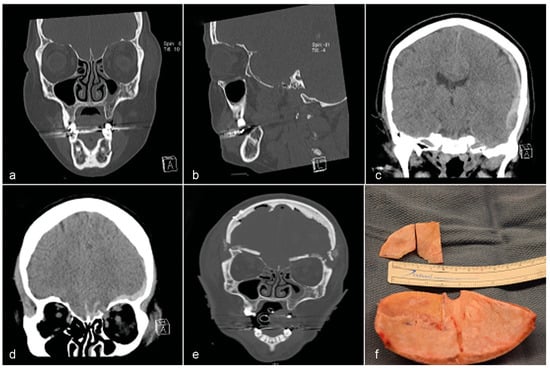
Figure 1.
CT scan of Patient 1: face, head, and brain with 1 mm slices. (a) Coronal view of bilateral minimally displaced orbital roof fractures. (b) Sagittal view of the left orbital roof fracture, which was more depressed than the right. (c) Coronal view of the left subdural hematoma (SDH) with 3 mm midline shift. (d) Coronal view of the left orbital encephalocele. (e) Coronal view of the bilateral orbital roof repair with split calvarial bone grafts. (f) Intraoperative picture of split calvarial bone grafts from the inner table of the patient’s frontal bone.
On hospital day 3, the patient was noted to be more dysphasic, combative, and intermittently following commands, with a GCS of 13 (E4V3M6). She developed bilateral pulsatile exophthalmos, with the left more pronounced than the right (Supplemental video). A repeat CT scan was performed, showing stable bony orbital roof fractures and an increased midline shift of 4 mm. Because of her worsening neurological status and pulsatile exophthalmos, the patient was taken emergently to the operating room for evacuation of the subdural hematoma and repair of the orbital roof defects and dural lacerations. Through a coronal incision, a bifrontal craniotomy was performed and she was found to have bilateral, unstable orbital roof blow-in fractures with extensive comminution and small bone fragments, dural lacerations, and orbital meningoencephaloceles. The orbital roof fractures were reconstructed with split calvarial bone grafts anchored with titanium screws, corticocancellous bone graft, and a vascularized pericranial flap (Figure 1e,f). Her pulsatile exophthalmos resolved immediately after surgery. She was later discharged to a rehabilitation facility with her mental status back at baseline and no focal neurologic or visual deficits.
Case 2
A 48-year-old man presented to the ED after falling approximately 25 feet off a ladder onto the pavement. He had transient loss of consciousness at the scene. Upon arrival, he had a 45-s episode of grand mal seizures and was intubated for airway protection. On exam, he was opening his eyes spontaneously and following commands in all four extremities with a GCS of 11T (E4V1M6). He was noted to have bilateral periorbital edema and ecchymoses without visual or extraocular movement deficits. Pupils were equal, round, and reactive to light, and visual fields were full. CT scan showed minimally displaced bilateral orbital roof blow-in fractures, comminuted frontal skull fractures involving the orbital rim, anterior and posterior tables of the frontal sinus, and facial fractures (Figure 2a, b). He had bilateral frontal contusions, a small right frontal subdural hematoma and traumatic subarachnoid hemorrhage (Figure 2c). No orbital encephalocele was noted. He was treated with levetiracetam and a hypertonic saline bolus. The patient was admitted to the trauma intensive care unit for monitoring.
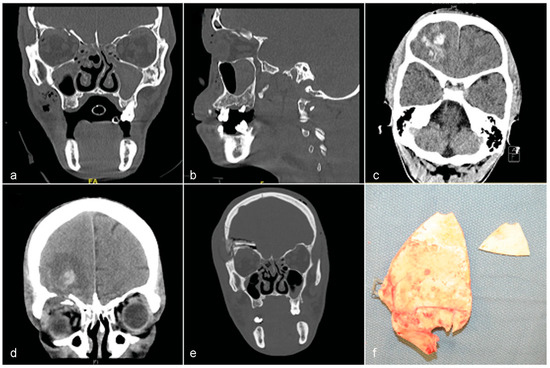
Figure 2.
CT scan of Patient 2: face, head, and brain with 1 mm slices. (a) Coronal view of bilateral minimally displaced orbital roof fractures. (b) Sagittal view of the comminuted right orbital roof fracture, which was more depressed than the left. (c) Axial view of the right frontal lobe contusion. (d) Coronal view of the right orbital encephalocele with right frontal lobe contusion and worsening fracture displacement, on hospital day 4. (e) Coronal view of the right orbital roof repair with split calvarial bone graft. (f) Intraoperative picture of split calvarial bone graft from the inner table of the patient’s right frontal bone.
On hospital day 4, the patient was noted to have pulsatile exophthalmos of the right eye. He remained awake and alert. A repeat head CT with angiogram revealed proptosis of the right globe, increased fracture displacement, and an orbital encephalocele (Figure 2d), without evidence of a carotid-cavernous fistula (CCF). The patient was taken to the operating room for bifrontal craniotomy and was found to have a right unstable blow-in fracture with extensive comminution and small bone fragments, dural laceration, and orbital meningoencephalocele. The frontal sinus and orbital fractures were repaired with a split calvarial bone graft anchored with titanium screws. The traumatic orbital encephalocele was reduced and the subdural hematoma was evacuated. The CSF leak was repaired with a vascularized pericranial flap (Figure 2e,f). An external ventricular drain was placed and mannitol was given intraoperatively. The patient recovered well from surgery without visual or neurologic deficits.
Discussion
Orbital roof fractures occur most commonly with a highenergy impact, such as a motor vehicle collision or a fall [1,2,6,8,10]. Depending on the direction of displacement, orbital roof fractures can be classified as “blow-in” or “blow-out,” with the latter being more common [2,6]. Blow-in type fractures present with signs and symptoms consistent with decreased orbital volume, including exophthalmos, diplopia, and restricted extraocular movements [2,6]. These fractures may be severe enough to allow for an orbital encephalocele. Blow-out type fractures result in an increase in orbital volume, and enophthalmos is commonly seen [2]. The majority of orbital roof fractures are associated with other facial fractures, most commonly involving ethmoidal and frontal sinuses and the medial orbital wall and least commonly involving the mandible [1,8,10].
Because of their location, orbital roof fractures are often associated with serious ophthalmologic or neurologic injuries that, if recognized, must be urgently addressed. These injuries include globe rupture, optic neuropathy, retrobulbar hematoma, extraocular muscle entrapment, pulsatile exophthalmos, and severe traumatic brain injury with or without CSF leak and brain herniation [1,2,3,7,9,11]. The exact incidence of these complications is not known, especially that of orbital encephaloceles, which are documented almost exclusively in isolated case reports [13,14,15].
CT scan with thin slices remains the imaging modality of choice in the evaluation of orbital roof fractures and surgical planning [9]. For patients with significant craniofacial fractures, we advocate for 1 mm coronal, sagittal, and axial views and three-dimensional reconstruction (Figure 3). This practice allows for optimal detection of orbital roof fractures and associated intracranial and ophthalmologic injuries. Magnetic resonance imaging (MRI) is superior in diagnosing intraorbital soft-tissue injuries such as encephalocele and optic neuropathy, but it is limited by long study time, relative insensitivity to bony fragments and wood and glass foreign bodies, and potential to cause further damage in cases of ferromagnetic foreign bodies [16].
Pulsatile exophthalmos may result from other causes, such as traumatic and nontraumatic CCF [17,18], aortic regurgitation [19], intracranial [20] and intraosseous [21] arteriovenous malformations, and sphenoid wing dysplasia with temporal lobe herniation in neurofibromatosis [22]. A CT angiogram, as performed in one of our patients, can be obtained to rule out CCF.
The management of orbital roof fractures should follow standard Advanced Trauma Life Support (ATLS) protocols and begin by first addressing life-threatening injuries. Multidisciplinary assessment by plastic surgeons/otolaryngologists/craniomaxillofacial surgeons, neurosurgeons, and ophthalmologists provides the best evaluation of all possible neurologic and ophthalmologic complications and should be obtained where possible [1]. Most authors agree that emergent repair is indicated when there is significant ophthalmologic or neurologic compromise [1,2,3,7,9,11]. Serial imaging and clinical examination is required to assess progression of intracranial processes and intracranial pressure [23,24]. Our management algorithm for orbital roof fractures in adults is outlined in Figure 3.
Management of orbital roof fractures is reported to be nonoperative in 71 to 90% of cases [1,3,7]. Antonyshyn et al. operated on all blow-in type orbital roof fractures [6]. Minimally displaced fractures are commonly managed conservatively, whereas moderately to severely displaced fractures are often managed operatively. However, some authors argue that the degree of displacement alone does not predict development of serious complications [1]. In one case series of four patients with significantly displaced blow-in or blow-out orbital roof fractures but without serious neurologic or visual compromise at presentation, the authors noted healing of fractures without sequelae [25]. They postulated that the equilibrium between intraorbital and intracranial pressures led to their resolution [25]. Nevertheless, this equilibrium can be disturbed with increasing intracranial pressures or dural laceration, or both, in the setting of a minimally displaced but unstable orbital roof due to extensive comminution, as seen in both patients we present.
When operative intervention is indicated, there are several surgical approaches and reconstruction options available to the surgeon. Subcranial approach through a superior blepharoplasty incision is appropriate when there are no intracranial injuries. If there is intracranial injury, the repair can be achieved through a coronal incision and frontal craniotomy. Once adequate exposure is obtained, the fracture can be reduced and stabilized or reconstructed. Autologous bone grafts, titanium mesh, or alloplasts such as polytetrafluoroethylene have been shown to provide successful stabilization or reconstruction [2].
In this article, we present two adults with minimally displaced orbital roof fractures that were monitored, but later required operative repair due to the development of pulsatile exophthalmos and orbital meningoencephalocele. These cases emphasize the importance of close observation by an experienced multidisciplinary team for all orbital roof fractures, regardless of their degree of displacement (Video 1).
Video 1: Supplemental video of patient in Case 1 which demonstrates pulsatile exophthalmos.
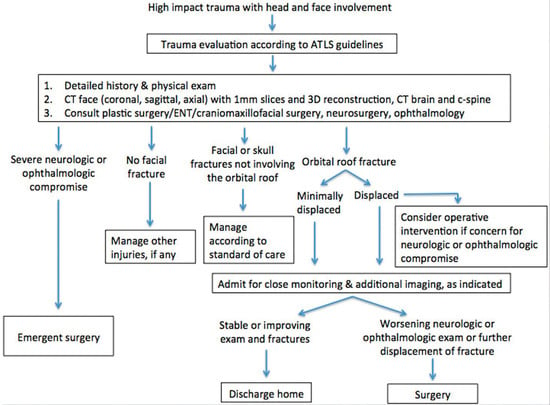
Figure 3.
A suggested management algorithm for orbital roof fractures in adults.
References
- Cossman, J.P.; Morrison, C.S.; Taylor, H.O.; Salter, A.B.; Klinge, P.M.; Sullivan, S.R. Traumatic orbital roof fractures: Interdisciplinary evaluation and management. Plast Reconstr Surg 2014, 133, 335e–343e. [Google Scholar] [CrossRef] [PubMed]
- Haug, R.H.; Van Sickels, J.E.; Jenkins, W.S. Demographics and treatment options for orbital roof fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002, 93, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.W.; Bae, T.H.; Kim, W.S.; Kim, H.K. Early reconstruction of orbital roof fractures: Clinical features and treatment outcomes. Arch Plast Surg 2012, 39, 31–35. [Google Scholar] [CrossRef]
- Martello, J.Y.; Vasconez, H.C. Supraorbital roof fractures: A formidable entity with which to contend. Ann Plast Surg 1997, 38, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, W.G. Displaced orbital roof fractures: Presentation and treatment. Plast Reconstr Surg 1991, 87, 657–661. [Google Scholar] [CrossRef]
- Antonyshyn, O.; Gruss, J.S.; Kassel, E.E. Blow-in fractures of the orbit. Plast Reconstr Surg 1989, 84, 10–20. [Google Scholar] [CrossRef]
- Fulcher, T.P.; Sullivan, T.J. Orbital roof fractures: Management of ophthalmic complications. Ophthal Plast Reconstr Surg 2003, 19, 359–363. [Google Scholar]
- Piotrowski, W.P.; Beck-Mannagetta, J. Surgical techniques in orbital roof fractures: Early treatment and results. J Craniomaxillofac Surg 1995, 23, 6–11. [Google Scholar]
- Righi, S.; Boffano, P.; Guglielmi, V.; Rossi, P.; Martorina, M. Diagnosis and imaging of orbital roof fractures: A review of the current literature. Oral Maxillofac Surg 2015, 19, 1–4. [Google Scholar]
- Scholsem, M.; Scholtes, F.; Collignon, F.; et al. Surgical management of anterior cranial base fractures with cerebrospinal fluid fistulae: A single-institution experience. Neurosurgery 2008, 62, 463–469, discussion 469–471. [Google Scholar]
- Penfold, C.N.; Lang, D.; Evans, B.T. The management of orbital roof fractures. Br J Oral Maxillofac Surg 1992, 30, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Bolling, J.P.; Wesley, R.E. Conservative treatment of orbital roof blow in fracture. Ann Ophthalmol 1987, 19, 75–76. [Google Scholar]
- Antonelli, V.; Cremonini, A.M.; Campobassi, A.; Pascarella, R.; Zofrea, G.; Servadei, F. Traumatic encephalocele related to orbital roof fractures: Report of six cases and literature review. Surg Neurol 2002, 57, 117–125. [Google Scholar] [CrossRef]
- Jaiswal, M.; Sundar, I.V.; Gandhi, A.; Purohit, D.; Mittal, R.S. Acute traumatic orbital encephalocele: A case report with review of literature. J Neurosci Rural Pract 2013, 4, 467–470. [Google Scholar] [CrossRef] [PubMed]
- Mokal, N.J.; Desai, M.F. Titanium mesh reconstruction of orbital roof fracture with traumatic encephalocele: A case report and review of literature. Craniomaxillofac Trauma Reconstr 2012, 5, 11–18. [Google Scholar] [CrossRef]
- Lee, H.J.; Jilani, M.; Frohman, L.; Baker, S. CT of orbital trauma. Emerg Radiol 2004, 10, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Lewis, A.I.; Tomsick, T.A.; Tew, J.M., Jr. Management of 100 consecutive direct carotid-cavernous fistulas: Results of treatment with detachable balloons. Neurosurgery 1995, 36, 239–244, discussion 244–245. [Google Scholar] [CrossRef]
- Liang, W.; Xiaofeng, Y.; Weiguo, L.; Wusi, Q.; Gang, S.; Xuesheng, Z. Traumatic carotid cavernous fistula accompanying basilar skull fracture: A study on the incidence of traumatic carotid cavernous fistula in the patients with basilar skull fracture and the prognostic analysis about traumatic carotid cavernous fistula. J Trauma 2007, 63, 1014–1020. [Google Scholar] [CrossRef]
- Ashrafian, H. Pulsatile pseudo-proptosis, aortic regurgitation and 31 eponyms. Int J Cardiol 2006, 107, 421–423. [Google Scholar] [CrossRef]
- Ding, D.; Liu, K.C. Orbital venous congestion: Rare manifestation of an intracranial arteriovenous malformation. J Clin Neurosci 2014, 21, 522–524. [Google Scholar] [CrossRef]
- Park, E.S.; Jung, Y.J.; Yun, J.H.; Ahn, J.S.; Lee, D.H. Intraosseous arteriovenous malformation of the sphenoid bone presenting with orbital symptoms mimicking cavernous sinus dural arteriovenous fistula: A case report. J Cerebrovasc Endovasc Neurosurg 2013, 15, 251–254. [Google Scholar] [PubMed]
- Dale, E.L.; Strait, T.A.; Sargent, L.A. Orbital reconstruction for pulsatile exophthalmos secondary to sphenoid wing dysplasia. Ann Plast Surg 2014, 72, S107–S111. [Google Scholar] [CrossRef] [PubMed]
- Bratton, S.L.; Chestnut, R.M.; Ghajar, J.; et al. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons; Joint Section on Neurotrauma and Critical Care, AANS/CNS. Guidelines for the management of severe traumatic brain injury. VIII. Intracranial pressure thresholds. J Neurotrauma 2007, 24 (Suppl. S1), S55–S58. [Google Scholar] [PubMed]
- Chesnut, R.M.; Temkin, N.; Carney, N.; et al. Global Neurotrauma Research Group. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med 2012, 367, 2471–2481. [Google Scholar]
- Stam, L.H.; Wolvius, E.B.; Schubert, W.; Koudstaal, M.J. Natural course of orbital roof fractures. Craniomaxillofac Trauma Reconstr 2014, 7, 294–297. [Google Scholar]
© 2016 by the author. The Author(s) 2016.