The Preventive Role of Exercise on the Physiological, Psychological, and Psychophysiological Parameters of Coronavirus 2 (SARS-CoV-2): A Mini Review
Abstract
:1. Introduction
2. Search Strategy
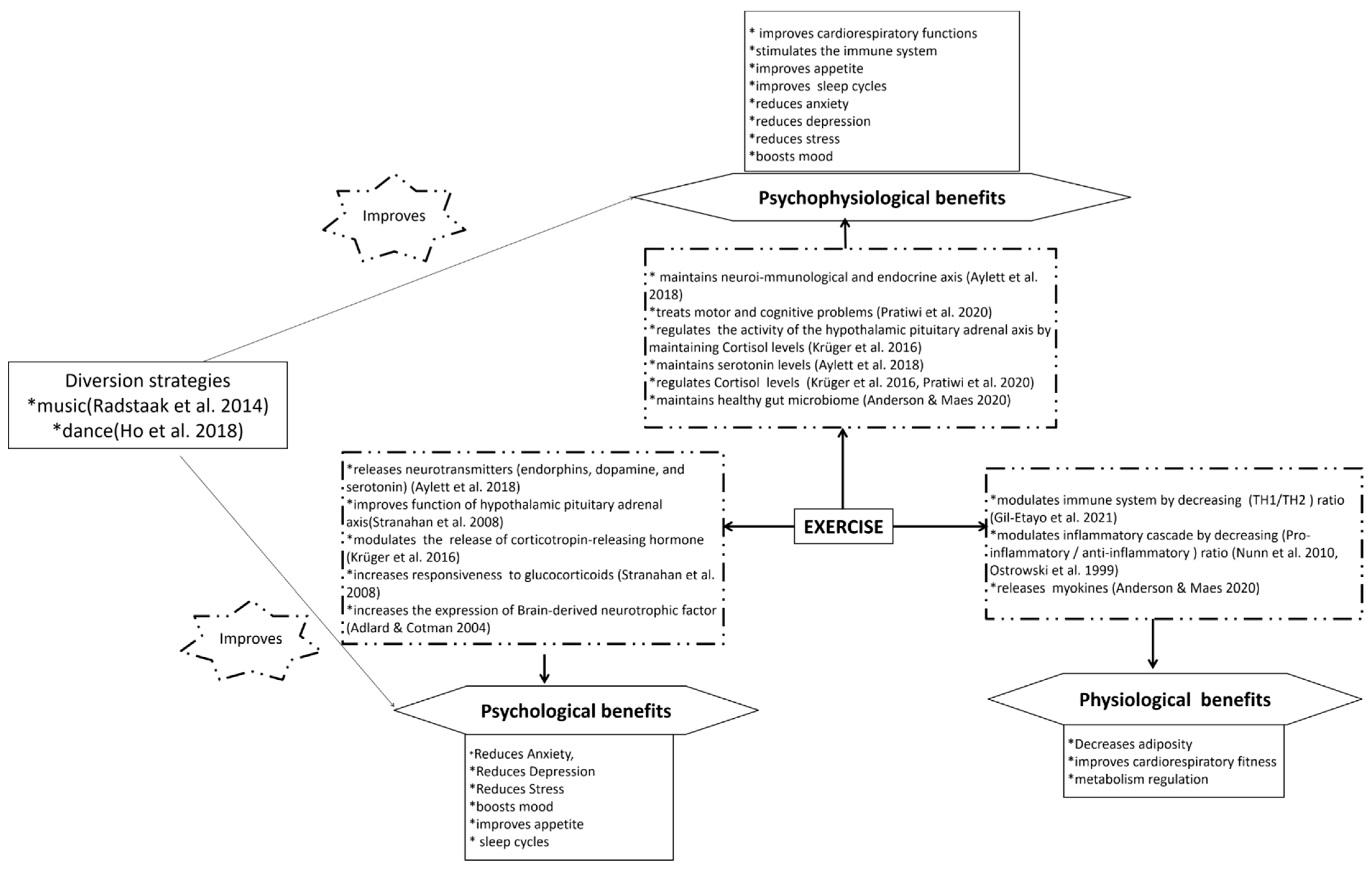
3. Physiological Effects of COVID-19 and Its Management by Exercise
4. Psychological Effects of COVID-19 and Its Management by Exercise
5. Psychophysiological Effects of COVID-19 and Its Management by Exercise
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Adhikari, Sasmita Poudel, Sha Meng, Yu-Ju Wu, Yu-Ping Mao, Rui-Xue Ye, Qing-Zhi Wang, Chang Sun, Rozelle Scott, Hein Raat, Huan Zhou, and et al. 2020. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infectious Diseases of Poverty 9: 29. [Google Scholar] [CrossRef] [Green Version]
- Adlard, P. A., and C. W. Cotman. 2004. Voluntary exercise protects against stress-induced decreases in brain-derived neurotrophic factor protein expression. Neuroscience 124: 985–92. [Google Scholar] [CrossRef]
- Anderson, George, and Michael Maes. 2020. Gut Dysbiosis Dysregulates Central and Systemic Homeostasis via Suboptimal Mitochondrial Function: Assessment, Treatment and Classification Implications. Current Topics in Medicinal Chemistry 20: 524–39. [Google Scholar] [CrossRef]
- Anon. 2020. US Census Bureau, Household Pulse Survey. Available online: https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/ (accessed on 3 September 2021).
- Arvidsdotter, Tina, Bertil Marklund, Sven Kylén, Charles Taft, and Inger Ekman. 2016. Understanding persons with psychological distress in primary health care. Scandinavian Journal of Caring Sciences 30: 687–94. [Google Scholar] [CrossRef]
- Aylett, Elizabeth, Nicola Small, and Peter Bower. 2018. Exercise in the treatment of clinical anxiety in general practice–a systematic review and meta-analysis. BMC Health Services Research 18: 559. [Google Scholar] [CrossRef] [PubMed]
- Blair, Steven N. 1996. Influences of Cardiorespiratory Fitness and Other Precursors on Cardiovascular Disease and All-Cause Mortality in Men and Women. JAMA Journal of the American Medical Association 276: 205. [Google Scholar] [CrossRef] [PubMed]
- Blumenthal, James A., Michael A. Babyak, P. Murali Doraiswamy, Lana Watkins, Benson M. Hoffman, Krista A. Barbour, Steve Herman, W. E. Craighead, A. L. Brosse, R. Waugh, and et al. 2007. Exercise and Pharmacotherapy in the Treatment of Major Depressive Disorder. Psychosomatic Medicine 69: 587–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bohlken, Jens, Friederike Schömig, Matthias R. Lemke, Matthias Pumberger, and Steffi G. Riedel-Heller. 2020. COVID-19-Pandemie: Belastungen des medizinischen Personals. Psychiatrische Praxis 47: 190–97. [Google Scholar] [CrossRef]
- Brock, David W., Brian A. Irving, Barbara Gower, and Gary R. Hunter. 2011. Differences emerge in visceral adipose tissue accumulation after selection for innate cardiovascular fitness. International Journal of Obesity 35: 309–12. [Google Scholar] [CrossRef] [Green Version]
- Carek, Peter J., Sarah E. Laibstain, and Stephen M. Carek. 2011. Exercise for the Treatment of Depression and Anxiety. The International Journal of Psychiatry in Medicine 41: 15–28. [Google Scholar] [CrossRef]
- Choi, Edmond Pui Hang, Bryant Pui Hung Hui, and Eric Yuk Fai Wan. 2020. Depression and Anxiety in Hong Kong during COVID-19. International Journal of Environmental Research and Public Health 17: 3740. [Google Scholar] [CrossRef] [PubMed]
- Church, Timothy S., Conrad P. Earnest, Angela M. Thompson, Elisa Priest, Ruben Q. Rodarte, Travis Sanders, Robert Ross, and Steven N. Blair. 2010. Exercise without Weight Loss Does Not Reduce C-Reactive Protein. Medicine and Science in Sports and Exercise 42: 708–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clemente-Suárez, Vicente Javier, Athanasios A. Dalamitros, Ana Isabel Beltran-Velasco, Juan Mielgo-Ayuso, and Jose Francisco Tornero-Aguilera. 2020. Social and Psychophysiological Consequences of the COVID-19 Pandemic: An Extensive Literature Review. Frontiers in Psychology 11: 3077. [Google Scholar] [CrossRef] [PubMed]
- Dinas, P. C., Y. Koutedakis, and A. D. Flouris. 2011. Effects of exercise and physical activity on depression. Irish journal of Medical Science 180: 319–25. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, Joseph E., Steven N. Blair, John M. Jakicic, Melinda M. Manore, Janet W. Rankin, and Bryan K. Smith. 2009. Appropriate Physical Activity Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults. Medicine and Science in Sports and Exercise 41: 459–71. [Google Scholar] [CrossRef] [PubMed]
- Dumas, Alexia, Lucie Bernard, Yannick Poquet, Geanncarlo Lugo-Villarino, and Olivier Neyrolles. 2018. The role of the lung microbiota and the gut-lung axis in respiratory infectious diseases. Cellular Microbiology 20: e12966. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Esch, Tobias, Jorg Duckstein, Justus Welke, and Vittoria Braun. 2007. Mind/body techniques for physiological and psychological stress reduction: Stress management via Tai Chi training—A pilot study. Medical Science Monitor 13: CR488–CR497. [Google Scholar]
- Flynn, Michael G., Brian K. McFarlin, and Melissa M. Markofski. 2007. State of the Art Reviews: The Anti-Inflammatory Actions of Exercise Training. American Journal of Lifestyle Medicine 1: 220–35. [Google Scholar] [CrossRef] [Green Version]
- Franklin, Barry A., and Peter A. McCullough. 2009. Cardiorespiratory Fitness: An Independent and Additive Marker of Risk Stratification and Health Outcomes. Mayo Clinic Proceedings 84: 776–79. [Google Scholar] [CrossRef] [Green Version]
- García-Fernández, Lorena, Verónica Romero-Ferreiro, Sergio Padilla, Pedro David López-Roldán, María Monzó-García, and Roberto Rodriguez-Jimenez. 2021. Gender differences in emotional response to the COVID-19 outbreak in Spain. Brain Behavior 11: e01934. [Google Scholar] [CrossRef]
- Gerber, Markus, and Uwe Pühse. 2009. Review Article: Do exercise and fitness protect against stress-induced health complaints? A review of the literature. Scandinavian Journal Public Health 37: 801–19. [Google Scholar] [CrossRef]
- Gil-Etayo, Francisco Javier, Patricia Suàrez-Fernández, Oscar Cabrera-Marante, Daniel Arroyo, Sara Garcinuño, Laura Naranjo, and Daniel E. Pleguezuelo. 2021. T-Helper Cell Subset Response Is a Determining Factor in COVID-19 Progression. Frontiers in Cellular and Infection Microbiology 11: 79. [Google Scholar] [CrossRef]
- Haskell, William L., I-Min Lee, Russell R. Pate, Kenneth E. Powell, Steven N. Blair, Barry A. Franklin, Caroline A. Macera, Gregory W. Heath, Paul D. Thompson, and Adrian Bauman. 2007. Physical Activity and Public Health. Medicine and Science in Sports and Exercise 39: 1423–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawryluck, Laura, Wayne L. Gold, Susan Robinson, Stephen Pogorski, Sandro Galea, and Rima Styra. 2004. SARS Control and Psychological Effects of Quarantine, Toronto, Canada. Emerging Infectious Diseases 10: 1206–12. [Google Scholar] [CrossRef]
- Ho, Rainbow Tin Hung, Adrian Ho Yin Wan, Friendly So Wah Au-Yeung, Phyllis Hau Yan Lo, Pantha Joey Chung Yue Siu, Cathy Pui Ki Wong, Winnie Yuen Han Ng, Irene Kit Man Cheung, Siu Man Ng, Cecilia Lai Wan Chan, and et al. 2014. The psychophysiological effects of Tai-chi and exercise in residential Schizophrenic patients: A 3-arm randomized controlled trial. BMC Complementary and Alternative Medicine 14: 364. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, Rainbow Tin Hung, Ted C. T. Fong, Wai Chi Chan, Joseph S. K. Kwan, Patrick K. C. Chiu, Joshua C. Y. Yau, and Linda C. W. Lam. 2018. Psychophysiological Effects of Dance Movement Therapy and Physical Exercise on Older Adults With Mild Dementia: A Randomized Controlled Trial. The Journals of Gerontology: Series B. [Google Scholar] [CrossRef] [PubMed]
- Hou, Fengsu, Fengying Bi, Rong Jiao, Dan Luo, and Kangxing Song. 2020. Gender differences of depression and anxiety among social media users during the COVID-19 outbreak in China:a cross-sectional study. BMC Public Health 20: 1648. [Google Scholar] [CrossRef] [PubMed]
- Hu, Shaojuan, Lorelei Tucker, Chongyun Wu, and Luodan Yang. 2020. Beneficial Effects of Exercise on Depression and Anxiety During the COVID-19 Pandemic: A Narrative Review. Frontiers in Psychiatry 11: 1217. [Google Scholar] [CrossRef]
- Janke, Kellie L., Tara P. Cominski, Eldo V. Kuzhikandathil, Richard J. Servatius, and Kevin C. H. Pang. 2015. Investigating the Role of Hippocampal BDNF in Anxiety Vulnerability Using Classical Eyeblink Conditioning. Frontiers in Psychiatry 6. [Google Scholar] [CrossRef] [Green Version]
- Jayakody, Kaushadh, Shalmini Gunadasa, and Christian Hosker. 2014. Exercise for anxiety disorders: Systematic review. British Journal of Sports Medicine 48: 187–96. [Google Scholar] [CrossRef]
- Jeong, Hyunsuk, Hyeon Woo Yim, Yeong-Jun Song, Moran Ki, Jung-Ah Min, Juhee Cho, and Jeong-Ho Chae. 2016. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiology and Health 38: e2016048. [Google Scholar] [CrossRef]
- Jones, Elizabeth A. K., Amal K. Mitra, and Azad R. Bhuiyan. 2021. Impact of COVID-19 on Mental Health in Adolescents: A Systematic Review. International Journal of Environmental Research and Public Health 18: 2470. [Google Scholar] [CrossRef]
- Jose, Ricardo J., and Ari Manuel. 2020. COVID-19 cytokine storm: The interplay between inflammation and coagulation. The Lancet Respiratory Medicine 8: e46–e47. [Google Scholar] [CrossRef]
- Kandola, Aaron, Gemma Lewis, David P. J. Osborn, Brendon Stubbs, and Joseph F. Hayes. 2020. Depressive symptoms and objectively measured physical activity and sedentary behaviour throughout adolescence: A prospective cohort study. The Lancet Psychiatry 7: 262–71. [Google Scholar] [CrossRef] [Green Version]
- Keely, Simon, Nicholas J. Talley, and Philip M. Hansbro. 2012. Pulmonary-intestinal cross-talk in mucosal inflammatory disease. Mucosal Immunology 5: 7–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khawam, Elias, Hassan Khouli, and Leo Pozuelo. 2020. Treating acute anxiety in patients with COVID-19. Cleveland Clinic Journal of Medicine. [Google Scholar] [CrossRef] [PubMed]
- Krüger, Karsten, Frank-Christoph Mooren, and Christian Pilat. 2016. The Immunomodulatory Effects of Physical Activity. Current Pharmaceutical Design 22: 3730–48. [Google Scholar] [CrossRef] [PubMed]
- Lee, Hyun Suk, and Junga Lee. 2021. Applying Artificial Intelligence in Physical Education and Future Perspectives. Sustainability 13: 351. [Google Scholar] [CrossRef]
- Levkovich, Inbar, and Shiri Shinan-Altman. 2021. The impact of gender on emotional reactions, perceived susceptibility and perceived knowledge about COVID-19 among the Israeli public. International Health. [Google Scholar] [CrossRef] [PubMed]
- Markus, Regina P., Pedro A. Fernandes, Gabriela S. Kinker, Sanseray da Silveira Cruz-Machado, and Marina Marçola. 2018. Immune-pineal axis—Acute inflammatory responses coordinate melatonin synthesis by pinealocytes and phagocytes. British Journal of Pharmacology 175: 3239–50. [Google Scholar] [CrossRef] [Green Version]
- Mikkelsen, K., L. Stojanovska, M. Polenakovic, M. Bosevski, and V. Apostolopoulos. 2017. Exercise and mental health. Maturitas 106: 48–56. [Google Scholar] [CrossRef] [PubMed]
- Morres, Ioannis D., Antonis Hatzigeorgiadis, Afroditi Stathi, Nikos Comoutos, Chantal Arpin-Cribbie, Charalampos Krommidas, and Yannis Theodorakis. 2019. Aerobic exercise for adult patients with major depressive disorder in mental health services: A systematic review and meta-analysis. Depression Anxiety 36: 39–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Narici, Marco, Giuseppe De Vito, Martino Franchi, Antonio Paoli, Tatiana Moro, Giuseppe Marcolin, Bruno Grassi, Lucrezia Zuccarelli, Biolo Gianni, Filippo Giorgio Di Girolamo, and et al. 2021. Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: Physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures. European Journal of Sport Science 21: 614–35. [Google Scholar] [CrossRef]
- Nieman, David C., Dru A. Henson, Melanie D. Austin, and Victor A. Brown. 2005. Immune Response to a 30-Minute Walk. Medicine and Science in Sports and Exercise 37: 57–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nunn, Alistair V., Geoffrey W. Guy, James S. Brodie, and Jimmy D. Bell. 2010. Inflammatory modulation of exercise salience: Using hormesis to return to a healthy lifestyle. Nutrition & Metabolism 7: 87. [Google Scholar] [CrossRef] [Green Version]
- Ostrowski, Kenneth, Thomas Rohde, Sven Asp, Peter Schjerling, and Bente Klarlund Pedersen. 1999. Pro- and anti-inflammatory cytokine balance in strenuous exercise in humans. The Journal of physiology 515: 287–91. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, Bente K., and Mark A. Febbraio. 2012. Muscles, exercise and obesity: Skeletal muscle as a secretory organ. Nature Reviews Endocrinology 8: 457–65. [Google Scholar] [CrossRef] [PubMed]
- Petzold, Moritz Bruno, Jens Plag, and Andreas Ströhle. 2020. Umgang mit psychischer Belastung bei Gesundheitsfachkräften im Rahmen der COVID-19-Pandemie. Nervenarzt 91: 417–21. [Google Scholar] [CrossRef] [Green Version]
- Phillips, Ashley. 2021. Artificial Intelligence-enabled Healthcare Delivery and Digital Epidemiological Surveillance in the Remote Treatment of Patients during the COVID-19 Pandemic. American Journal of Medical Research 8: 30. [Google Scholar] [CrossRef]
- Poirier, Paul, and Jean-Pierre Després. 2001. Exercise In Weight Management of Obesity. Cardiology Clinics 19: 459–70. [Google Scholar] [CrossRef]
- Pratiwi, Prita Indah, Qiongying Xiang, and Katsunori Furuya. 2020. Physiological and Psychological Effects of Walking in Urban Parks and Its Imagery in Different Seasons in Middle-Aged and Older Adults: Evidence from Matsudo City, Japan. Sustainability 12: 4003. [Google Scholar] [CrossRef]
- Radstaak, Mirjam, Sabine A. E. Geurts, Jos F. Brosschot, and Michiel A. J. Kompier. 2014. Music and Psychophysiological Recovery from Stress. Psychosomatic Medicine 76: 529–37. [Google Scholar] [CrossRef] [PubMed]
- Raghavendra, Rao M., H. S. Vadiraja, Raghuram Nagarathna, H. R. Nagendra, M. Rekha, N. Vanitha, and K. S. Gopinath. 2009. Effects of a Yoga Program on Cortisol Rhythm and Mood States in Early Breast Cancer Patients Undergoing Adjuvant Radiotherapy: A Randomized Controlled Trial. Integrative Cancer Therapies 8: 37–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rebar, Amanda L., Robert Stanton, David Geard, Camille Short, Mitch J. Duncan, and Corneel Vandelanotte. 2015. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychology Review 9: 366–78. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, Diane L., J. R. Garay, S. L. Deamond, Maura K. Moran, W. Gold, and R. Styra. 2008. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiology & Infection 136: 997–1007. [Google Scholar] [CrossRef]
- Rogers, Rob. 2021. Internet of Things-based Smart Healthcare Systems, Wireless Connected Devices, and Body Sensor Networks in COVID-19 Remote Patient Monitoring. American Journal of Medical Research 8: 71. [Google Scholar] [CrossRef]
- Rosa Rimes, Ridson, Marcos de Souza Moura Antonio, Murilo Khede Lamego, Alberto Souza de Sa Filho, Joao Manochio, Flavia Paes, and Mauro Giovanni Carta. 2015. Effects of Exercise on Physical and Mental Health, and Cognitive and Brain Functions in Schizophrenia: Clinical and Experimental Evidence. CNS Neurological Disorders-Drug Targets (Formerly Current Drug Targets-CNS & Neurological Disorders) 14: 1244–54. [Google Scholar] [CrossRef] [Green Version]
- Saeed, Sy Atezaz, Karlene Cunningham, and Richard M. Bloch. 2019. Depression and Anxiety Disorders: Benefits of Exercise, Yoga, and Meditation. American Family Physician 99: 620–27. [Google Scholar]
- Schuch, Felipe B., Davy Vancampfort, Justin Richards, Simon Rosenbaum, Philip B. Ward, and Brendon Stubbs. 2016. Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. Journal of Psychiatric Research 77: 42–51. [Google Scholar] [CrossRef] [Green Version]
- Serafini, Gianluca, Bianca Parmigiani, Andrea Amerio, Andrea Aguglia, Leo Sher, and Mario Amore. 2020. The psychological impact of COVID-19 on the mental health in the general population. QJM An International Journal of Medicine 113: 531–37. [Google Scholar] [CrossRef]
- Shimizu, Kazuhiro, Fuminori Kimura, Takayuki Akimoto, Takao Akama, Kai Tanabe, Takahiko Nishijima, Shinya Kuno, and Ichiro Kono. 2008. Effect of moderate exercise training on T-helper cell subpopulations in elderly people. Exercise Immunology Review 14: 24–37. [Google Scholar]
- Song, Qing-Hua, Guo-Qing Shen, Rong-Mei Xu, Quan-Hai Zhang, Ming Ma, Yan-Hua Guo, Xin-Ping Zhao, and Yu-Bing Han. 2014. Effect of Tai Chi exercise on the physical and mental health of the elder patients suffered from anxiety disorder. International Journal of Physiology, Pathophysiology and Pharmacology 6: 55–60. [Google Scholar] [PubMed]
- Stebbing, Justin, Anne Phelan, Ivan Griffin, Catherine Tucker, Olly Oechsle, Dan Smith, and Peter Richardson. 2020. COVID-19: Combining antiviral and anti-inflammatory treatments. The Lancet Infectious Diseases 20: 400–2. [Google Scholar] [CrossRef]
- Stefan, Norbert, Andreas L. Birkenfeld, Matthias B. Schulze, and David S. Ludwig. 2020. Obesity and impaired metabolic health in patients with COVID-19. Nature Reviews Endocrinology 16: 341–42. [Google Scholar] [CrossRef] [Green Version]
- Stonerock, Gregory L., Benson M. Hoffman, Patrick J. Smith, and James A. Blumenthal. 2015. Exercise as Treatment for Anxiety: Systematic Review and Analysis. Annals of Behavioral Medicine 49: 542–56. [Google Scholar] [CrossRef] [Green Version]
- Stranahan, Alexis M., Kim Lee, and Mark P. Mattson. 2008. Central Mechanisms of HPA Axis Regulation by Voluntary Exercise. Neuromolecular Medicine 10: 118–27. [Google Scholar] [CrossRef] [Green Version]
- Ströhle, Andreas. 2009. Physical activity, exercise, depression and anxiety disorders. Journal of Neural Transmission 116: 777–84. [Google Scholar] [CrossRef]
- Stubbs, Brendon, Davy Vancampfort, Simon Rosenbaum, Joseph Firth, Theodore Cosco, Nicola Veronese, Giovanni A. Salum, and Felipe B. Schuch. 2017. An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: A meta-analysis. Psychiatry Research 249: 102–8. [Google Scholar] [CrossRef]
- Tan, Tricia, Bernard Khoo, Edouard G. Mills, Maria Phylactou, Bijal Patel, Pei C. Eng, and Layla Thurston. 2020. Association between high serum total cortisol concentrations and mortality from COVID-19. Lancet Diabetes Endocrinology 8: 659–60. [Google Scholar] [CrossRef]
- Vanuytsel, Tim, Sander Van Wanrooy, Hanne Vanheel, Christophe Vanormelingen, Sofie Verschueren, Els Houben, Shadea Salim Rasoel, J. Tόth, L. Holvoet, R. Farré, and et al. 2014. Psychological stress and corticotropin-releasing hormone increase intestinal permeability in humans by a mast cell-dependent mechanism. Gut 63: 1293–99. [Google Scholar] [CrossRef] [PubMed]
- Vogelzangs, N., A. T. F. Beekman, P. De Jonge, and B. W. J. H. Penninx. 2013. Anxiety disorders and inflammation in a large adult cohort. Translational Psychiatry 3: e249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Meizi, Julien S. Baker, Wenjing Quan, Siqin Shen, Gusztáv Fekete, and Yaodong Gu. 2020. A Preventive Role of Exercise Across the Coronavirus 2 (SARS-CoV-2) Pandemic. Frontiers in Physiology 11: 572718. [Google Scholar] [CrossRef] [PubMed]
- Wang, Minghuan, Caihong Hu, Qian Zhao, Renjie Feng, Qing Wang, Hongbin Cai, and Zhenli Guo. 2021. Acute psychological impact on COVID-19 patients in Hubei: A multicenter observational study. Translational Psychiatry 11: 133. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. 2021. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 15 September 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baker, J.S.; Cole, A.; Tao, D.; Li, F.; Liang, W.; Jiao, J.; Gao, Y.; Supriya, R. The Preventive Role of Exercise on the Physiological, Psychological, and Psychophysiological Parameters of Coronavirus 2 (SARS-CoV-2): A Mini Review. J. Risk Financial Manag. 2021, 14, 476. https://doi.org/10.3390/jrfm14100476
Baker JS, Cole A, Tao D, Li F, Liang W, Jiao J, Gao Y, Supriya R. The Preventive Role of Exercise on the Physiological, Psychological, and Psychophysiological Parameters of Coronavirus 2 (SARS-CoV-2): A Mini Review. Journal of Risk and Financial Management. 2021; 14(10):476. https://doi.org/10.3390/jrfm14100476
Chicago/Turabian StyleBaker, Julien S., Alistair Cole, Dan Tao, Feifei Li, Wei Liang, Jojo Jiao, Yang Gao, and Rashmi Supriya. 2021. "The Preventive Role of Exercise on the Physiological, Psychological, and Psychophysiological Parameters of Coronavirus 2 (SARS-CoV-2): A Mini Review" Journal of Risk and Financial Management 14, no. 10: 476. https://doi.org/10.3390/jrfm14100476
APA StyleBaker, J. S., Cole, A., Tao, D., Li, F., Liang, W., Jiao, J., Gao, Y., & Supriya, R. (2021). The Preventive Role of Exercise on the Physiological, Psychological, and Psychophysiological Parameters of Coronavirus 2 (SARS-CoV-2): A Mini Review. Journal of Risk and Financial Management, 14(10), 476. https://doi.org/10.3390/jrfm14100476







