Surgical Management of Traumatic Meniscus Injuries
Abstract
:1. Introduction
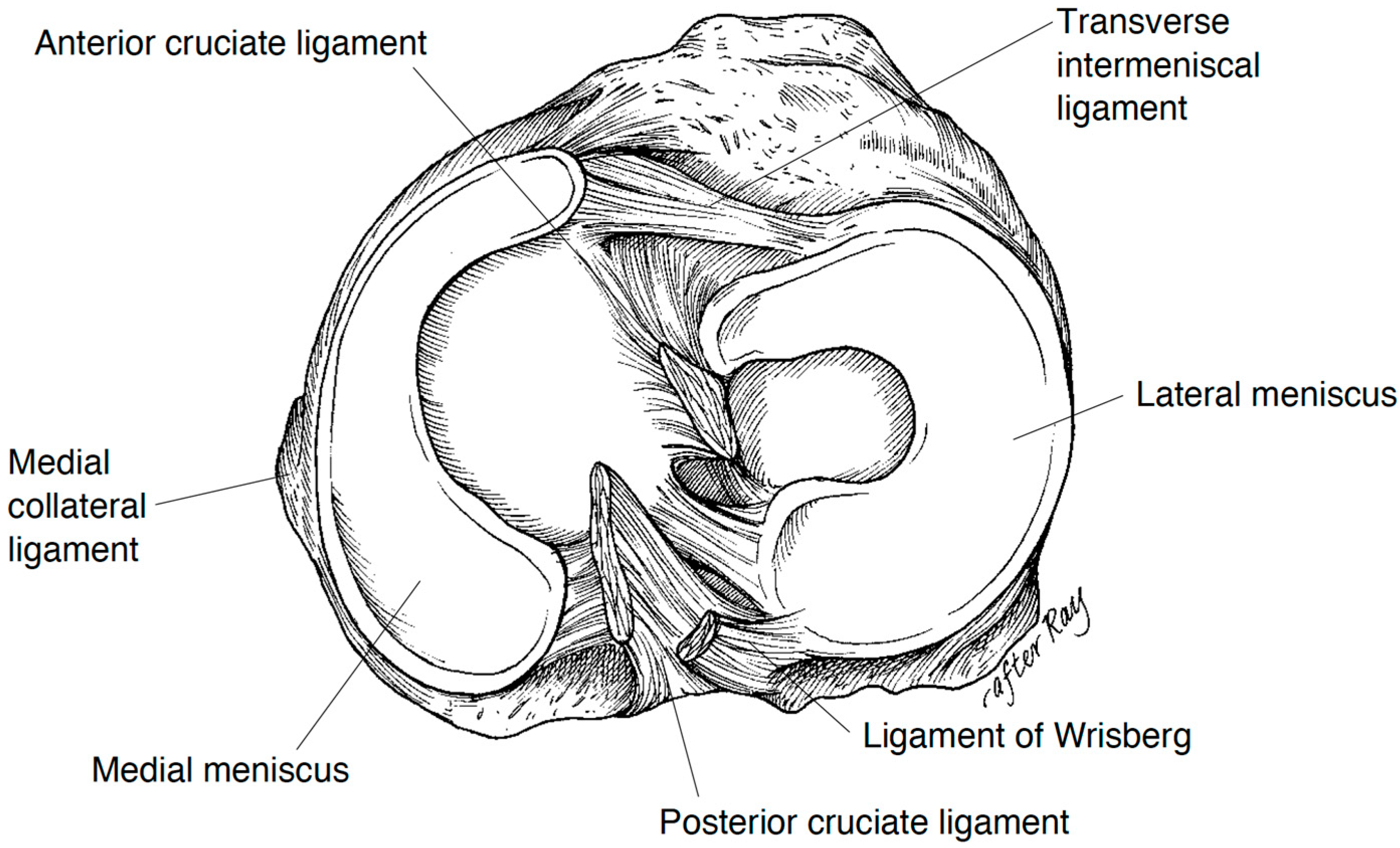
1.1. Anatomy of the Menisci
1.2. Clinical Biomechanics of the Menisci
2. Injury Mechanism and Classification of Traumatic Meniscus Tears
2.1. Epidemiology of Traumatic Meniscus Tears
2.2. Injury Mechanism of Traumatic Meniscus Tears
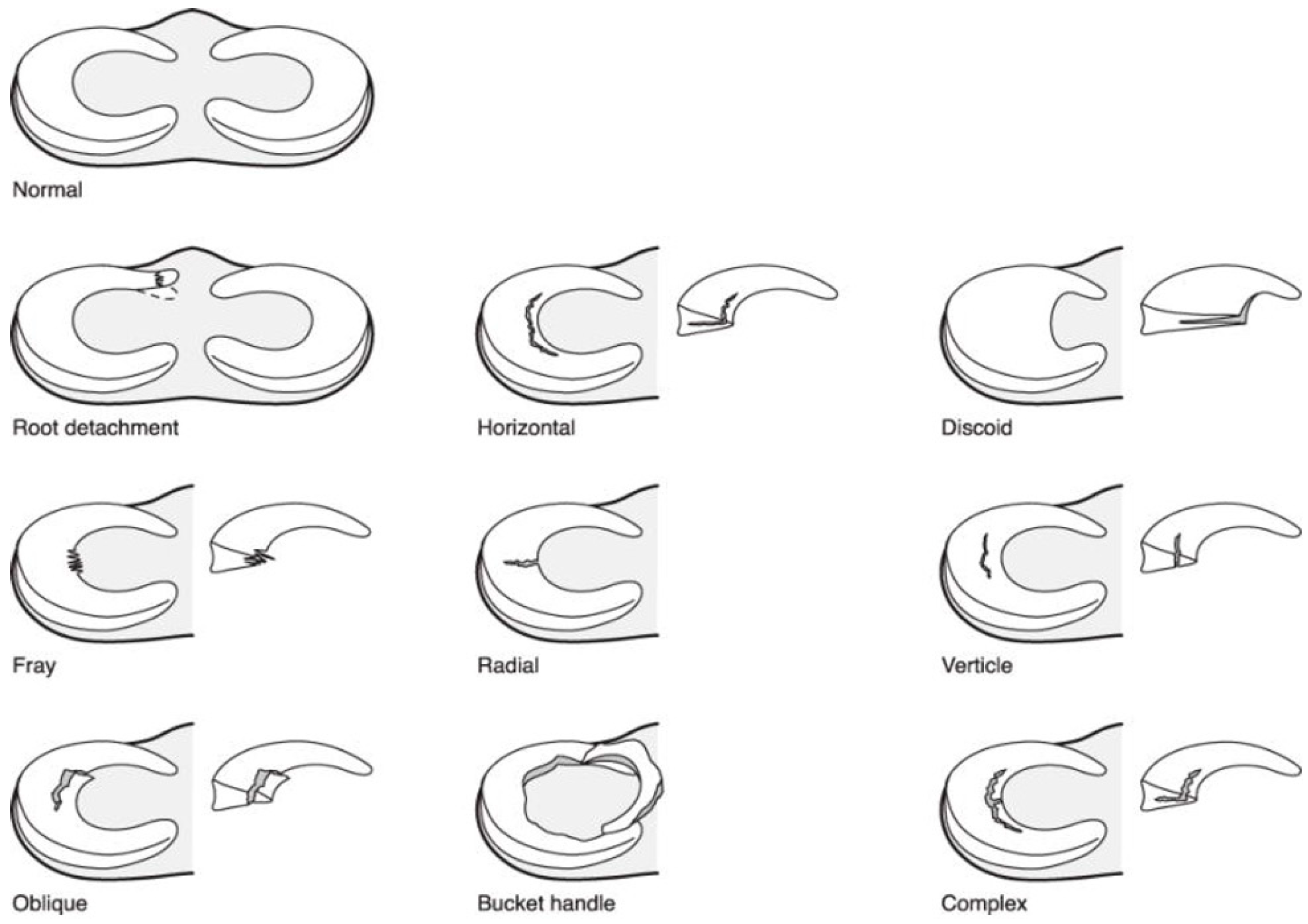
2.3. Classification of Meniscus Tears
2.4. The Discoid Meniscus
3. Surgical Management of Meniscus Tears
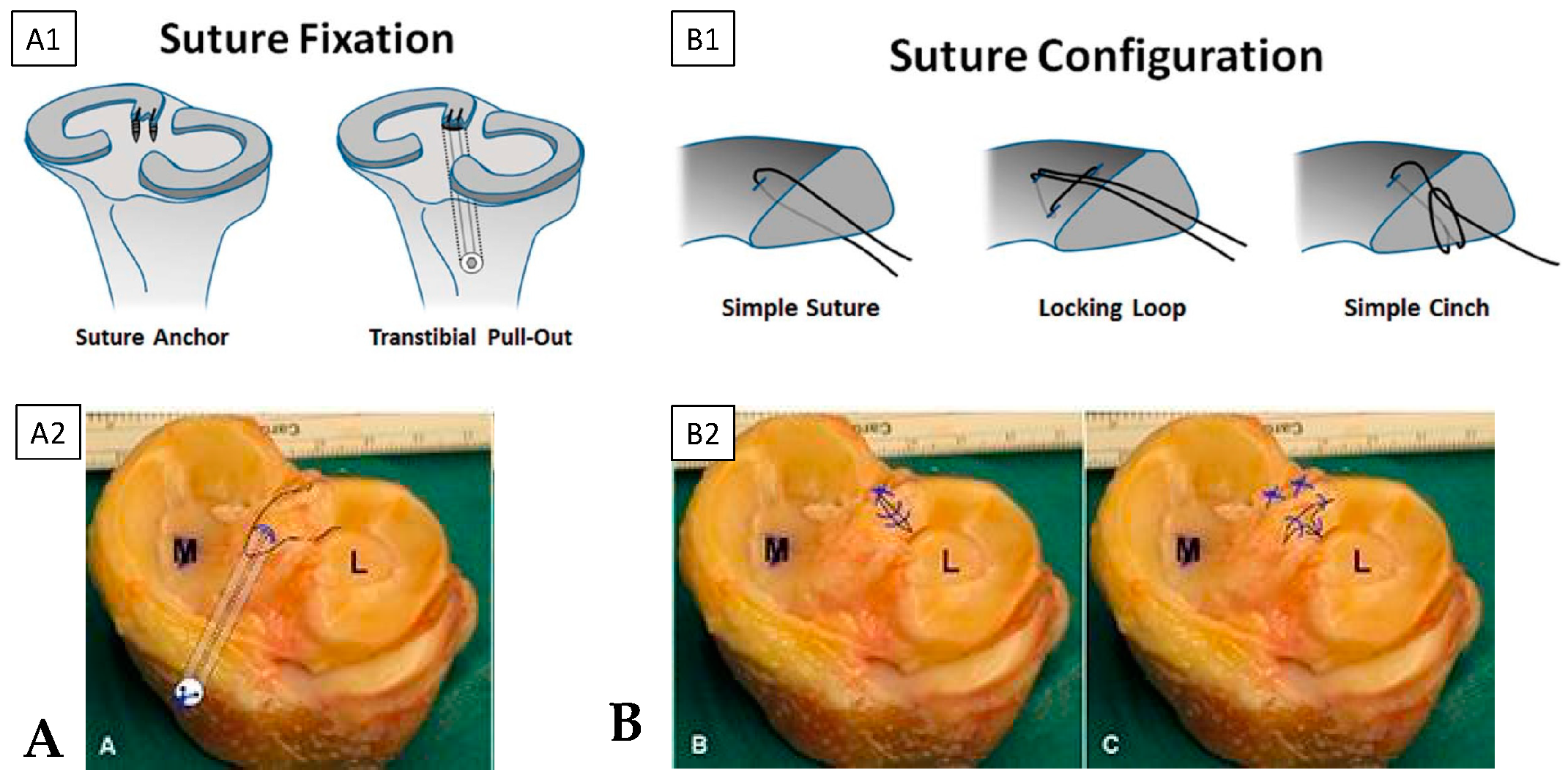
3.1. Surgical Techniques for Meniscus Repair
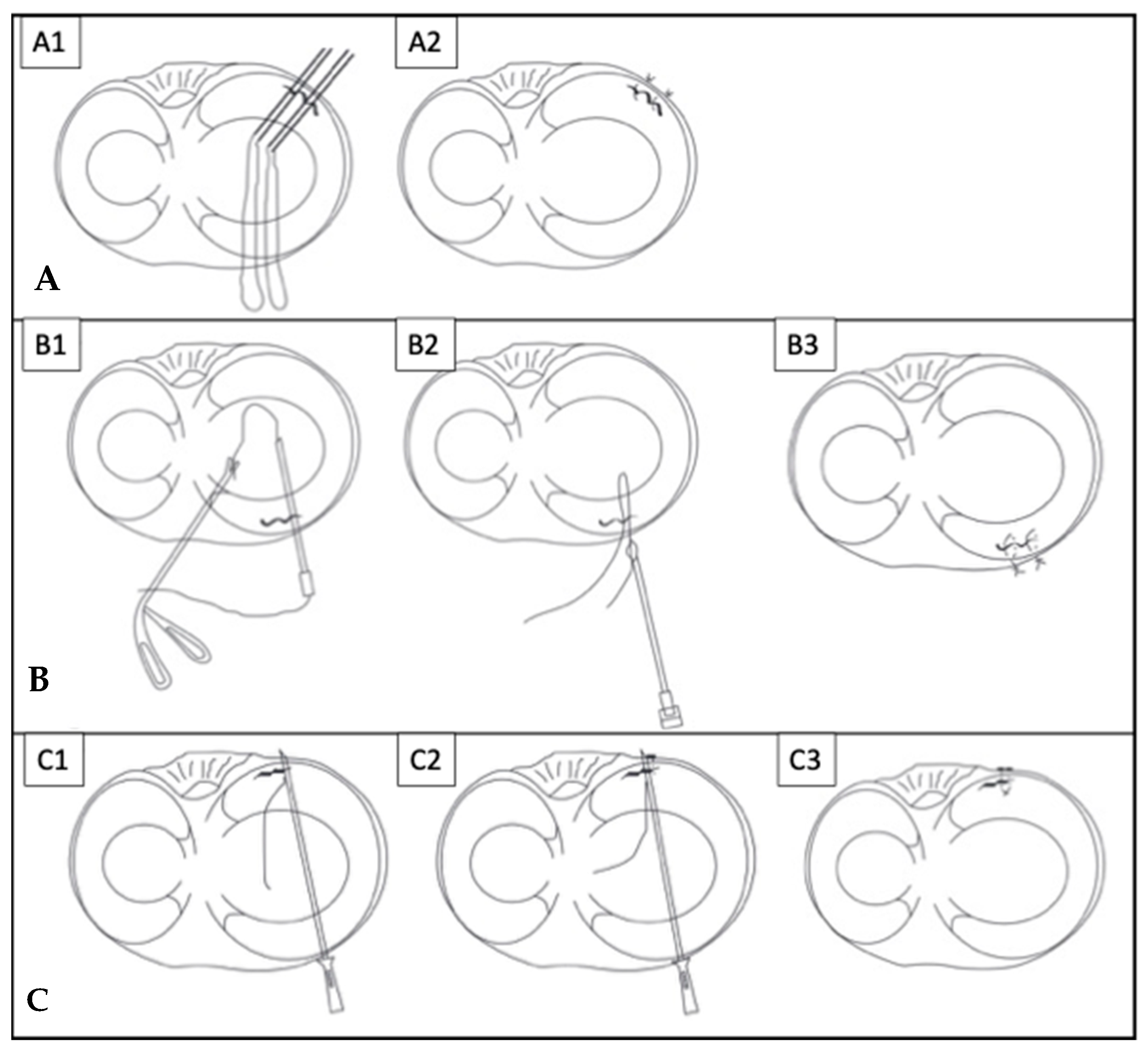
3.2. Considerations of Tear Locations
3.3. Considerations of Tear Patterns
3.4. Management of the Discoid Meniscus
3.5. Evolving Treatment for Meniscus Injuries
3.6. Outcomes after Surgical Treatment
4. Postoperative Rehabilitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Clark, C.R.; Ogden, J.A. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J. Bone Jt. Surg. Am. 1983, 65, 538–547. [Google Scholar] [CrossRef]
- Fithian, D.C.; Kelly, M.A.; Mow, V.C. Material properties and structure-function relationships in the menisci. Clin. Orthop. Relat. Res. 1990, 252, 19–31. [Google Scholar] [CrossRef]
- Fox, A.J.S.; Bedi, A.; Rodeo, S.A. The Basic Science of Human Knee Menisci: Structure, Composition, and Function. Sports Health 2012, 4, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Greis, P.E.; Bardana, D.D.; Holmstrom, M.C.; Burks, R.T. Meniscal Injury: I. Basic Science and Evaluation. J. Am. Acad. Orthop. Surg. 2002, 10, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Kumari, A.; Gupta, G.; Kumar, P.; Rani, S. Morphological study of the menisci of the knee joint in human cadaver in Jharkhand population. J. Fam. Med. Prim. Care 2022, 11, 4723–4729. [Google Scholar] [CrossRef] [PubMed]
- Bellisari, G.; Samora, W.; Klingele, K. Meniscus Tears in Children. Sports Med. Arthrosc. Rev. 2011, 19, 50–55. [Google Scholar] [CrossRef]
- Vinagre, G.; Cruz, F.; Alkhelaifi, K.; D’Hooghe, P. Isolated meniscus injuries in skeletally immature children and adolescents: State of the art. J. ISAKOS 2022, 7, 19–26. [Google Scholar] [CrossRef]
- Bryceland, J.K.; Powell, A.J.; Nunn, T. Knee Menisci. Cartilage 2017, 8, 99–104. [Google Scholar] [CrossRef]
- Gray, J.C. Neural and Vascular Anatomy of the Menisci of the Human Knee. J. Orthop. Sports Phys. Ther. 1999, 29, 23–30. [Google Scholar] [CrossRef]
- Scapinelli, R. Vascular anatomy of the human cruciate ligaments and surrounding structures. Clin. Anat. 1997, 10, 151–162. [Google Scholar] [CrossRef]
- Mine, T.; Kimura, M.; Sakka, A.; Kawai, S. Innervation of nociceptors in the menisci of the knee joint: An immunohistochemical study. Arch. Orthop. Trauma Surg. 2000, 120, 201–204. [Google Scholar] [CrossRef]
- Allen, C.R.; Wong, E.K.; Livesay, G.A.; Sakane, M.; Fu, F.H.; Woo, S.L.-Y. Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J. Orthop. Res. 2000, 18, 109–115. [Google Scholar] [CrossRef] [PubMed]
- DePhillipo, N.N.; Moatshe, G.; Chahla, J.; Aman, Z.S.; Storaci, H.W.; Morris, E.R.; Robbins, C.M.; Engebretsen, L.; LaPrade, R.F. Quantitative and Qualitative Assessment of the Posterior Medial Meniscus Anatomy: Defining Meniscal Ramp Lesions. Am. J. Sports Med. 2018, 47, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.J.; Erickson, B.J.; Cvetanovich, G.L.; Yanke, A.B.; Bach, B.R.; Cole, B.J. The Meniscus-Deficient Knee: Biomechanics, Evaluation, and Treatment Options. Orthop. J. Sports Med. 2015, 3, 2325967115611386. [Google Scholar] [CrossRef] [PubMed]
- Śmigielski, R.; Becker, R.; Zdanowicz, U.; Ciszek, B. Medial meniscus anatomy—From basic science to treatment. Knee Surg. Sports Traumatol. Arthrosc. 2014, 23, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Walker, P.S.; Erkiuan, M.J. The Role of the Menisci in Force Transmission Across the Knee. Clin. Orthop. Relat. Res. 1975, 109, 184–192. [Google Scholar] [CrossRef]
- Radin, E.L.; Rose, R.M. Role of subchondral bone in the initiation and progression of cartilage damage. Clin. Orthop. Relat. Res. 1986, 213, 34–40. [Google Scholar] [CrossRef]
- Itthipanichpong, T.; Moonwong, S. Medial Meniscus Root Tear: Current Update Review. In Arthroscopy; Suarez-Ahedo, C., Ed.; IntechOpen: London, UK, 2022. [Google Scholar] [CrossRef]
- Papageorgiou, C.D.; Gil, J.E.; Kanamori, A.; Fenwick, J.A.; Woo, S.L.-Y.; Fu, F.H. The Biomechanical Interdependence between the Anterior Cruciate Ligament Replacement Graft and the Medial Meniscus. Am. J. Sports Med. 2001, 29, 226–231. [Google Scholar] [CrossRef]
- Everhart, J.S.; Higgins, J.D.; Poland, S.G.; Abouljoud, M.M.; Flanigan, D.C. Meniscal repair in patients age 40 years and older: A systematic review of 11 studies and 148 patients. Knee 2018, 25, 1142–1150. [Google Scholar] [CrossRef]
- Liechti, D.J.; Constantinescu, D.S.; Ridley, T.J.; Chahla, J.; Mitchell, J.J.; Vap, A.R. Meniscal Repair in Pediatric Populations: A Systematic Review of Outcomes. Orthop. J. Sports Med. 2019, 7, 232596711984335. [Google Scholar] [CrossRef]
- Jackson, T.; Fabricant, P.D.; Beck, N.; Storey, E.; Patel, N.M.; Ganley, T.J. Epidemiology, Injury Patterns, and Treatment of Meniscal Tears in Pediatric Patients: A 16-Year Experience of a Single Center. Orthop. J. Sports Med. 2019, 7, 232596711989032. [Google Scholar] [CrossRef]
- Carter, C.W.; Kocher, M.S. Meniscus Repair in Children. Clin. Sports Med. 2012, 31, 135–154. [Google Scholar] [CrossRef]
- Kurzweil, P.R.; Cannon, W.D.; DeHaven, K.E. Meniscus Repair and Replacement. Sports Med. Arthrosc. Rev. 2018, 26, 160–164. [Google Scholar] [CrossRef]
- Wilson, P.L.; Wyatt, C.W.; Romero, J.; Sabatino, M.J.; Ellis, H.B. Incidence, Presentation, and Treatment of Pediatric and Adolescent Meniscal Root Injuries. Orthop. J. Sports Med. 2018, 6, 2325967118803888. [Google Scholar] [CrossRef] [PubMed]
- Srimongkolpitak, S.; Chernchujit, B. Current concepts on meniscal repairs. J. Clin. Orthop. Trauma 2022, 27, 101810. [Google Scholar] [CrossRef] [PubMed]
- Ozeki, N.; Seil, R.; Krych, A.J.; Koga, H. Surgical treatment of complex meniscus tear and disease: State of the art. J. ISAKOS 2021, 6, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Saltzman, B.M.; Cotter, E.J.; Wang, K.C.; Rice, R.; Manning, B.T.; Yanke, A.B.; Forsythe, B.; Verma, N.N.; Cole, B.J. Arthroscopically Repaired Bucket-Handle Meniscus Tears: Patient Demographics, Postoperative Outcomes, and a Comparison of Success and Failure Cases. Cartilage 2020, 11, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Andrish, J.T. Meniscal Injuries in Children and Adolescents: Diagnosis and Management. J. Am. Acad. Orthop. Surg. 1996, 4, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Bedi, A.; Kelly, N.; Baad, M.; Fox, A.J.; Ma, Y.; Warren, R.F.; Maher, S.A. Dynamic Contact Mechanics of Radial Tears of the Lateral Meniscus: Implications for Treatment. Arthrosc. J. Arthrosc. Relat. Surg. 2012, 28, 372–381. [Google Scholar] [CrossRef] [PubMed]
- Maffulli, N.; Longo, U.G.; Campi, S.; Denaro, V. Meniscal tears. Open Access J. Sports Med. 2010, 1, 45–54. [Google Scholar] [CrossRef]
- Chahla, J.; LaPrade, R.F. Meniscal Root Tears. Arthroscopy 2019, 35, 1304–1305. [Google Scholar] [CrossRef]
- Ciemniewska-Gorzela, K.; Bąkowski, P.; Naczk, J.; Jakob, R.; Piontek, T. Complex Meniscus Tears Treated with Collagen Matrix Wrapping and Bone Marrow Blood Injection: Clinical Effectiveness and Survivorship after a Minimum of 5 Years’ Follow-Up. Cartilage 2021, 13, 228S–238S. [Google Scholar] [CrossRef] [PubMed]
- Shieh, A.; Bastrom, T.; Roocroft, J.; Edmonds, E.W.; Pennock, A.T. Meniscus Tear Patterns in Relation to Skeletal Immaturity: Children Versus Adolescents. Am. J. Sports Med. 2013, 41, 2779–2783. [Google Scholar] [CrossRef]
- Jordan, M.R. Lateral Meniscal Variants: Evaluation and Treatment. J. Am. Acad. Orthop. Surg. 1996, 4, 191–200. [Google Scholar] [CrossRef]
- Watanabe, M.; Takeda, S.; Ikeuchi, H. Atlas of Arthroscopy, 3rd ed.; Springer: Berlin/Heidelberg, Germany, 1979. [Google Scholar]
- Kocher, M.S.; Logan, C.A.; Kramer, D.E. Discoid Lateral Meniscus in Children: Diagnosis, Management, and Outcomes. J. Am. Acad. Orthop. Surg. 2017, 25, 736–743. [Google Scholar] [CrossRef] [PubMed]
- Yoo, W.J.; Choi, I.H.; Chung, C.Y.; Lee, M.C.; Cho, T.-J.; Park, M.S.; Lee, D.Y. Discoid Lateral Meniscus in Children. Limited Knee Extension and Meniscal Instability in the Posterior Segment. J. Pediatr. Orthop. 2008, 28, 544–548. [Google Scholar] [CrossRef] [PubMed]
- Arner, J.W.; Ruzbarsky, J.J.; Vidal, A.F.; Frank, R.M. Meniscus Repair Part 1: Biology, Function, Tear Morphology, and Special Considerations. J. Am. Acad. Orthop. Surg. 2022, 30, e852–e858. [Google Scholar] [CrossRef] [PubMed]
- Arner, J.W.; Ruzbarsky, J.J.; Vidal, A.F.; Frank, R.M. Meniscus Repair Part 2: Technical Aspects, Biologic Augmentation, Rehabilitation, and Outcomes. J. Am. Acad. Orthop. Surg. 2022, 30, 613–619. [Google Scholar] [CrossRef]
- Barber, F.; Herbert, M.A.; Richards, D.P. Load to failure testing of new meniscal repair devices. Arthrosc. J. Arthrosc. Relat. Surg. 2004, 20, 45–50. [Google Scholar] [CrossRef]
- Fillingham, Y.A.; Riboh, J.C.; Erickson, B.J.; Bach, B.R.; Yanke, A.B. Inside-Out Versus All-Inside Repair of Isolated Meniscal Tears: An Updated Systematic Review. Am. J. Sports Med. 2016, 45, 234–242. [Google Scholar] [CrossRef]
- Malinowski, K.; Góralczyk, A.; Hermanowicz, K.; LaPrade, R.F. Tips and Pearls for All-Inside Medial Meniscus Repair. Arthrosc. Tech. 2019, 8, e131–e139. [Google Scholar] [CrossRef] [PubMed]
- Yoon, K.H.; Park, K.H. Meniscal Repair. Knee Surg. Relat. Res. 2014, 26, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Mesiha, M.; Zurakowski, D.; Soriano, J.; Nielson, J.H.; Zarins, B.; Murray, M.M. Pathologic Characteristics of the Torn Human Meniscus. Am. J. Sports Med. 2007, 35, 103–112. [Google Scholar] [CrossRef]
- Pauli, C.; Grogan, S.; Patil, S.; Otsuki, S.; Hasegawa, A.; Koziol, J.; Lotz, M.; D’lima, D. Macroscopic and histopathologic analysis of human knee menisci in aging and osteoarthritis. Osteoarthr. Cartil. 2011, 19, 1132–1141. [Google Scholar] [CrossRef] [PubMed]
- Cabral, J.; Sinikumpu, J. Clinical considerations of anatomy and magnetic resonance imaging in pediatric meniscus tear, with imaging-based treatment options. J. Child. Orthop. 2023, 17, 63–69. [Google Scholar] [CrossRef]
- Hirtler, L.; Unger, J.; Weninger, P. Acute and chronic menisco-capsular separation in the young athlete: Diagnosis, treatment and results in thirty seven consecutive patients. Int. Orthop. 2015, 39, 967–974. [Google Scholar] [CrossRef]
- Bonasia, D.E.; Pellegrino, P.; D’Amelio, A.; Cottino, U.; Rossi, R. Meniscal root tear repair: Why, when and how? Orthop. Rev. 2015, 7, 5792. [Google Scholar] [CrossRef]
- Krych, A.J.; Hevesi, M.; Leland, D.P.; Stuart, M.J. Meniscal Root Injuries. J. Am. Acad. Orthop. Surg. 2020, 28, 491–499. [Google Scholar] [CrossRef]
- De Girolamo, L.; Galliera, E.; Volpi, P.; Denti, M.; Dogliotti, G.; Quaglia, A.; Cabitza, P.; Romanelli, M.M.C.; Randelli, P. Why menisci show higher healing rate when repaired during ACL reconstruction? Growth factors release can be the explanation. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 90–96. [Google Scholar] [CrossRef]
- Meister, K.; Indelicato, P.A.; Spanier, S.; Franklin, J.; Batts, J. Histology of the Torn Meniscus: A Comparison of Histologic Differences in Meniscal Tissue between Tears in Anterior Cruciate Ligament-Intact and Anterior Cruciate Ligament-Deficient Knees. Am. J. Sports Med. 2004, 32, 1479–1483. [Google Scholar] [CrossRef]
- Rodríguez-Roiz, J.M.; Sastre-Solsona, S.; Popescu, D.; Montañana-Burillo, J.; Combalia-Aleu, A. The relationship between ACL reconstruction and meniscal repair: Quality of life, sports return, and meniscal failure rate—2- to 12-year follow-up. J. Orthop. Surg. Res. 2020, 15, 361. [Google Scholar] [CrossRef] [PubMed]
- Klingele, K.E.; Kocher, M.S.; Hresko, M.T.; Gerbino, P.; Micheli, L.J. Discoid Lateral Meniscus: Prevalence of Peripheral Rim Instability. J. Pediatr. Orthop. 2004, 24, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, L.K.; Yamaga, H.; Ida, K.; Miura, T. Arthroscopic meniscectomy for discoid lateral meniscus in children. J. Bone Jt. Surg Am. 1988, 70, 1495–1500. [Google Scholar] [CrossRef]
- Jacob, G.; Shimomura, K.; Krych, A.J.; Nakamura, N. The Meniscus Tear: A Review of Stem Cell Therapies. Cells 2019, 9, 92. [Google Scholar] [CrossRef] [PubMed]
- Middleton, S.; Asplin, L.; Stevenson, C.; Thompson, P.; Spalding, T. Meniscal allograft transplantation in the paediatric population: Early referral is justified. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1908–1913. [Google Scholar] [CrossRef]
- Brophy, R.H.; Wojahn, R.D.; Lillegraven, O.; Lamplot, J.D. Outcomes of Arthroscopic Posterior Medial Meniscus Root Repair: Association with Body Mass Index. J. Am. Acad. Orthop. Surg. 2019, 27, 104–111. [Google Scholar] [CrossRef]
- Ridley, T.J.; McCarthy, M.A.; Bollier, M.J.; Wolf, B.R.; Amendola, A. Age Differences in the Prevalence of Isolated Medial and Lateral Meniscal Tears in Surgically Treated Patients. Iowa Orthop. J. 2017, 37, 91–94. [Google Scholar]
- Yang, S.-J.; Ding, Z.-J.; Li, J.; Xue, Y.; Chen, G. Factors influencing postoperative outcomes in patients with symptomatic discoid lateral meniscus. BMC Musculoskelet. Disord. 2020, 21, 551. [Google Scholar] [CrossRef]
- Harput, G.; Guney-Deniz, H.; Nyland, J.; Kocabey, Y. Postoperative rehabilitation and outcomes following arthroscopic isolated meniscus repairs: A systematic review. Phys. Ther. Sport 2020, 45, 76–85. [Google Scholar] [CrossRef]
- VanderHave, K.L.; Perkins, C.; Le, M. Weightbearing Versus Non-weightbearing After Meniscus Repair. Sports Health 2015, 7, 399–402. [Google Scholar] [CrossRef]
- Pabian, P.; Hanney, W.J. Functional rehabilitation after medial meniscus repair in a high school football quarterback: A case report. N. Am. J. Sports Phys. Ther. 2008, 3, 161–169. [Google Scholar] [PubMed]
- Spang, R.C., III; Nasr, M.C.; Mohamadi, A.; DeAngelis, J.P.; Nazarian, A.; Ramappa, A.J. Rehabilitation following meniscal repair: A systematic review. BMJ Open Sport Exerc. Med. 2018, 4, e000212. [Google Scholar] [CrossRef] [PubMed]
- Meadows, K.D.; Peloquin, J.M.; Markhali, M.I.; Zgonis, M.H.; Schaer, T.P.; Mauck, R.L.; Elliott, D.M. Acute Repair of Meniscus Root Tear Partially Restores Joint Displacements as Measured with Magnetic Resonance Images and Loading in a Cadaveric Porcine Knee. J. Biomech. Eng. 2023, 145, 081002. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution-NonCommercial 4.0 International (CC BY NC) license (https://creativecommons.org/licenses/by-nc/4.0/).
Share and Cite
Popper, H.R.; Fliegel, B.E.; Elliott, D.M.; Su, A.W. Surgical Management of Traumatic Meniscus Injuries. Pathophysiology 2023, 30, 618-629. https://doi.org/10.3390/pathophysiology30040044
Popper HR, Fliegel BE, Elliott DM, Su AW. Surgical Management of Traumatic Meniscus Injuries. Pathophysiology. 2023; 30(4):618-629. https://doi.org/10.3390/pathophysiology30040044
Chicago/Turabian StylePopper, Hannah R., Brian E. Fliegel, Dawn M. Elliott, and Alvin W. Su. 2023. "Surgical Management of Traumatic Meniscus Injuries" Pathophysiology 30, no. 4: 618-629. https://doi.org/10.3390/pathophysiology30040044
APA StylePopper, H. R., Fliegel, B. E., Elliott, D. M., & Su, A. W. (2023). Surgical Management of Traumatic Meniscus Injuries. Pathophysiology, 30(4), 618-629. https://doi.org/10.3390/pathophysiology30040044





