Abstract
Introduction: The digitalized PREVED (PREgnancy, PreVention, Endocrine Disruptor) questionnaire was used in the clinical practices of health professionals (HP) who adhered to the MEDPREVED strategy. The objectives were to assess the strategy and to determine if it could improve access to endocrine disruptor (ED) exposure prevention. Methods: After having filled in the digital questionnaire in HP waiting rooms, patients were invited to talk about ED exposure during the consultation. HPs were previously trained in ED and had received a prevention kit for their patients. After the seven-month implementation phase, the evaluation phase consisted of five mixed assessments: interviews with: (i) patients who were young children’s parents; (ii) patients in the general population; (iii) paediatricians; (iv) midwives; and a quantitative study on GPs. Assessment concerned feasibility, accessibility, and usefulness of the strategy; we then used the Levesque model to evaluate how it could improve access to ED exposure prevention. Results: The study included 69 participants. The strategy appeared feasible for the filling-out step due to digital and environment access. However, it depended on patient and HP profiles. The strategy seemed useful insofar as it facilitated reflexive investment, an intention to healthy behaviour and, rather rarely, talk about ED exposure. The beginning of this discussion depended on time, prioritizing of the topic and HP profile. The strategy has confirmed the Levesque model’s limiting factors and levers to access ED prevention. Conclusions: The MEDPREVED strategy is feasible, accessible, and useful in clinical prevention practice. Further study is needed to measure the impact on knowledge, risk perception and behavior of beneficiaries of the MEDPREVED strategy in the medium and long term.
1. Introduction
Endocrine disruptors (ED) are defined as “exogenous substances or mixtures that alter function (s) of the endocrine system and consequently causes adverse health effects in an intact organism, or its progeny, or (sub)populations”. They are widely distributed, and even at very low doses, EDs are likely to have endocrine-disrupting effects [1]. People are exposed to many Eds, such as bisphenol A (BPA) through plastics [2], or parabens (PB) through cosmetics and personal care products [3]. Exposure to ED during pregnancy is likely to have negative health consequences as described by the Developmental Origins Hypothesis of Health and Diseases (DOHAD). They affect fetal development (nervous system disturbance, prematurity) and the fetus’ future life (behavioral disturbances, early puberty) [1].
Early interventions to reduce ED exposure significantly reduce this risk [4]; preventing exposure to ED must be a priority for health professionals (HP) [5]. A few studies have examined how to limit ED exposure through restrictive diet [6,7,8] or perinatal health education program. One of the perinatal education programs, is called “PREVED” (PRegnancy prEVention Endocrine Disruptors) [9,10,11]. PREVED uses an ED exposure assessment tool which consists of 33 questions exploring self-esteem, perceived health, health care renunciation and risk aversion, risk perception, knowledge about ED (routes and sources of exposure, ability to name some ED molecules or families of molecules, and definition of an ED), ED risk perception (perceived severity and vulnerability), expectations of a healthy baby, trusted person, level of concern about risks related to pregnancy, relation to risk visibility and perceived ability to reduce one’s exposure to ED with a visual analogic scale. Height questions explore the knowledge, attitude, and practice (KAP) dimensions, which identify knowledge level, attitudes linked to behavior change, preventive practices. Indeed, as it is often difficult to link knowledge to healthy behaviour, it is important to take into account the three psychological components of patient behavior (cognitive, emotional and conative) [12].
Among actors who could educate pregnant women, health professionals (HP) have had greater medical endorsement than non-medical professionals [11] and clinical prevention practices are integrated into medical practice [13]. In these prevention practices, HPs can use educational tools (e.g., pamphlets, interviews, speaking groups, and workshops), methods highlighting active listening [11] and questionnaires on different topics [14,15,16,17,18].
Some of these questionnaires use digital technology, or mhealth, such as Internet websites [19,20] accessible on smartphone. Computer software and digital questionnaires help to identify health risk behaviours, such as misuse of alcohol, smoking, lack of physical activity, after which, the doctor comments to the patient about the results, gives necessary information about the risks and tries to change the patient’s behaviour [21]. However, these tools adopt a prevention approach to risk reduction that does not always empower the patient, so other tools, filled in by the patient, are used in an asset-based approach. Indeed, paediatricians, midwives and GPs intentionally use their waiting rooms to disseminate a broad range of health-related information, sometimes with mhealth. However, some authors have shown that often there are no clearly defined prevention strategies in this workplace [22].
To our knowledge, there exists no study assessing digital tool on ED exposure prevention. Following the hypothesis that patient should be conscious of their life habits and their health impacts of them, and that new knowledge conveyed by HPs could modify attitudes and behaviour, we have developed a strategy for ED exposure prevention based on a simplified digital tool from the PREVED questionnaire, available in waiting room and integrated into clinical preventive practices. We have implemented the strategy named “MEDPREVED” and evaluated it from the standpoints of accessibility, feasibility, and usefulness, after which we have tried to determine whether the new strategy could improve access to ED exposure prevention.
Methods
The strategy was based on the patient empowerment and motivational approach with self-assessment of life habits, especially regarding ED and a brief intervention supported by HP training on ED and HP equipment with a prevention kit. Empowerment is a process that enables people to make decisions and exercise control over their lives by developing a positive representation of themselves [23]. Brief intervention is similar to a reduced version of motivational maintenance, and can naturally find its place in general or paediatric medicine, where long-term monitoring and prevention are at the heart of their practices. It consists, often over several consultations, of a risk assessment of the subject, an exchange on the motivations for change and active participation, through open, non-judgmental questions. The patient plays a central role in his/her own decision to change. It is a responsible rather than a paternalistic approach.
For the development phase we carried out a pilot study on GPs, which allowed us to adapt the strategy because there were problems recruiting patients and the questionnaire was perceived as too complex to be filled out by patients. As a result, the PREVED questionnaire was simplified in order to respect the health literacy concept in accordance with the “Facile À Lire et à Comprendre” criteria [24]. It included only eight brief questions on: (i) the participant’s ED knowledge about routes and sources of exposure, ED definition, and family names; (ii) perception of risk, especially perceived severity; (iii) patient practices (behaviours) through ED eviction and ways of achieving it. Finally, to induce patient recruitment, the questionnaire was digitalized with a QR code on posters in the waiting rooms of the different HPs.
For the implementation phase, HP recruitment was carried out through HP councils, the infant and maternal protection units of departmental council of five French departments, and the University Masters local associations of the of Nouvelle-Aquitaine region. The HP regional college (“Union Régionale des Professionnels de Santé” or URPS) in Nouvelle-Aquitaine and a pesticide control association of GPs have also agreed to spread the message of the study to GPs with major paediatric activity, as well as private and hospital paediatricians. Approximately 100 HPs were contacted by the researchers by email, telephone or directly at the place of practice. Moreover, midwives were contacted through midwives of the Nouvelle Aquitaine professional order.
Those who were interested in participating in the study were invited to send an email expressing their interest. A reply email was sent to them containing the entire MEDPREVED strategy (kits and display) along with the protocol. Recruitment of HPs began on 13 April 2021 and ended on 12 November 2021. The implementation phase began on 13 April 2021and ended on 31 December 2021.
After having filled in the digital questionnaire on their smartphone in waiting rooms, patients were invited to talk about ED exposure during their consultation with their HP. While we did not collect the patients’ answers to the PREVED questionnaire, we made their responses available to the HP during the consultation if the patient so wished, in order to initiate a discussion on ED exposure prevention. HP were previously trained on ED with a training kit and had received a prevention kit with brochures for their patients. The self-training kit included: a « 2 min all inclusive» video made by the eSET (Health Environment for All) of Bourgogne Franche-Comté [25], a link to the INSERM information package on ED [26], an article by the International Federation of Gynecology and Obstetrics (FIGO) [5], and a user’s guide for private physicians, produced by the URPS of Provence-Alpes-Côte d’Azur (PACA) [27]. The prevention kit given to the patient consisted of: the PACA URPS Guide, the same video, a guide by the Agence Régionale de Santé (ARS) Nouvelle-Aquitaine [28], a flyer from ARS Nouvelle Aquitaine [29], an application “Ma Maison Santé” created by the French Mutualité Pays de la Loire [30] and a link to the WECF (Women Engage for a Common Future) France website [31].
After the seven month implementation phase, the evaluation phase was composed of five assessments: four using a qualitative approach with interviews of: (i) patients who were young children’s parents; (ii) patients in the general population; (iii) paediatricians; (iv) midwives; and one with a quantitative approach of GPs. The patients were recruited on a voluntary basis by asking them to fill in their email at the end of the questionnaire: if they accepted, they were contacted again by two medical students (LD, MP) for a short telephone interview. The data were then anonymized. The analysis and coding of the qualitative data were done by triangulating content analysis. For the quantitative part, self-assessment was hetero-administered via Limesurvey©. (Version 4.3. Hambourg, Germany)Statistical analysis of the data was carried out without software. Qualitative variables were described in terms of numbers and percentages and quantitative variables in terms of means, standard deviation, minimum and maximum.
Using the Levesque model, we then tried to determine whether the MEDPREVED strategy could improve access to ED exposure prevention. This model presents the determinants related to the patient and the determinants related to the health system, which are of interest throughout the patient’s care pathway and may or may not result in access to health services. It is determined not only by the patient’s ability to perceive their health needs, to seek, reach, pay for and engage in health activities, but also by the characteristics of the health system: ease of access, acceptability and the availability of the service, affordability and relevance [32].
2. Results
2.1. Study Population
The study population included 69 participants. Among the hundreds of HPs contacted, eight paediatricians or GPs with a paediatric activity (Pe1 to Pe12), 26 GPs and 12 midwifes (M1 to M12) agreed to participate in the evaluation phase while of the 23 patients filled in the questionnaire, 11 included general population group patients (P1 to P11) and 12 young children’s parents (Pa1 to Pa12) agreed to participate to the evaluation phase. Characteristics of the 43 participants (23 patients, 12 midwifes and eight paediatricians or GPs with a paediatric activity) are described in Table 1. Characteristics of the 26 GPs are described in Table 2. The mean age of GP was 45 ± 13 (from 30 to 71) years. The mean number of medical practices’ duration was 16 ± 14 (from 1 to 48) years. Their responses in terms of feasibility, accessibility and utility of MEDPREVED strategy are presented in Table 3.

Table 1.
Characteristics of qualitative study population (M: midwife; Pe: Paediatrician or GP with a prenatal activity; P: patient from general population; Pa: patient with young children or pregnant woman).

Table 2.
Characteristics of the 26 GPs included in the quantitative study.

Table 3.
Feasibility, accessibility and utility of MEDPREVED strategy from General Practitioners’ point of view (n = 26).
2.2. Feasibility and Accessibility of MEDPREVED Strategy
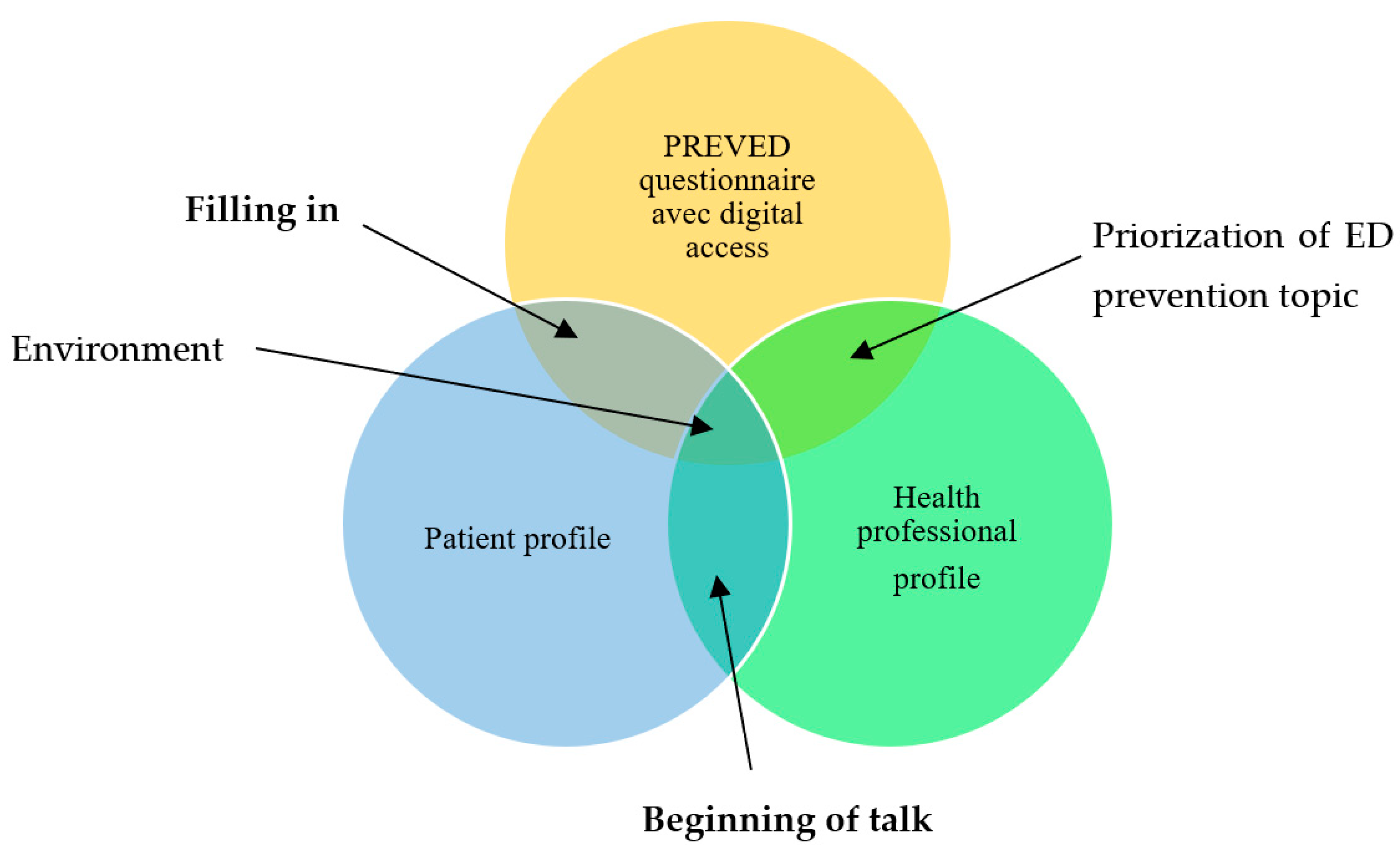
We have summarized the modalities of MEDPREVED feasibility and accessibility in Figure 1. The interface between the digital tool and the patient profile refers to the filling-in of the questionnaire. The interface between the digital tool and the HP’s profile refers to the professional’s prioritizing of ED prevention topics in his/her practice. The interface between patient and HP profiles refers to the beginning of the discussion. Results of each modality are presented below.
Figure 1.
Modalities of MEDPREVED feasibility and accessibility.
In the MEDPREVED strategy, we judged feasible the filling in of the questionnaire, but not the beginning of the talk about ED exposure prevention, notably because of non-prioritizing of ED prevention among HPs.
- 1.
- Feasibility of the filling in was permitted by digital accessibility, PREVED questionnaire accessibility, patient and physician profiles and the environment.
- (a)
- Digital accessibility, through digital technology with a QR code, facilitated complete of the questionnaire, at times in different time-steps, via smartphone use universality, COVID-19 context facilitator and digital ease of use.
- Smartphone use universality: “I think they all have a smartphone” (Pe3); “They all have the phone that goes with it to be able to do the right thing” (M3)
- Covid19 facilitator: “Given the context in which we endlessly scan QR codes: very accessible” (Pa7).
- Digital literacy and ease of use: “I found that with the QR code system it’s really not bad” (P3); “I found it simple, fast” (Pa8)
- Digital preference: “I would have put the paper in my bag, I would not have done it right away in the waiting room, I don’t think I would have done it” (P6); “I thought the QR code was pretty good and it avoided having to fill out a piece of paper it was easier to do because there was just to scan and then there was the questionnaire to display and then click on send and it was good.” (M8)
However, some participants noted the side effects of technology: unequal access due to age, culture, lack of internet access and paper preference:
- Age: “If my mother had to fill it out, she wouldn’t have a suitable phone. 'Fine, that’s fine... it’s more complicated for some people” (Pa1)
- Culture: “People don’t yet have QR code education with us” (Pe3).
- Non-internet access: “I don’t always have internet” (P7); “As soon as it is digital I find that it is... a bit excluding because there are always people who don’t have internet on their phone” (Pa6)
- Paper preference: “I find that understanding on a piece of paper is much easier and makes me want to do it a lot more than picking up the phone” (P10); “It’s not my area of choice the QR code” (M12)
- (b)
- Feasibility was helped by the accessibility of the PREVED questionnaire with it associated its form and content. Mainly, feasibility seemed to depend on patient and physician profiles.
The form characteristics of the questionnaire were its simpleness, quickness and flow:
- Simple: “It’s super simple even.” (M2); “I know I have patients who told me it was simple to do, yes and not long” (M8)
- Quick: “A questionnaire that is quick, easy to do” (Pa11)
- Flowing: “Frankly it was fluid” (Pa5); “I liked it was a bit playful euh the fact of... sliding to put in order there, for the rooms of the house...” (Pa10)
The contents of the questionnaire addressed health literacy with concrete but maybe too general questions, lacking in precision:
- Questionnaire Literacy: “I found it simple to understand and uh... no it was fine” (Pa6);
- Only one patient found it difficult: “too medical lexicon” (P10)
- Concrete questions: “I recognize myself with some plastic utensils, uh... with uh... here with product choices so it’s... oh yes we... right away we recognize our daily life» (P7).
- Lack of precision: “I found it rather generalist, I mean not ultra-precise” (Pa2); “I find it unfortunate that at the beginning of the questionnaire it is not... I mean that the definition is not given to us before asking us questions about what we think about it” (P10).
Mainly, feasibility seemed to depend on patient and physician profiles.
Patient profiles were described in terms of being informed, having previous hormonal disease, profession, parenthood, rurality, psychosocial characteristics (fatalism, risk perception, fear of judgment), interest and curiosity, ED exposure prevention behaviour:
- Informed by social media: “I think everyone has heard about it in the press at least” (Pe7); “it is true that we are hearing more and more about endocrine disruptors” (P4)
- Previous hormonal disease: “I am particularly aware of this because I had hormone-dependent breast cancer” (P1); “maybe also because I have my daughter that I see she has early signs of puberty” (P5); “My father has myelodysplasia so I am even more aware today” (Pa5); “there are patients who are already informed, which is a limit that tells you more than you already know about the subject” (M3)
- Profession: “My year as a child care worker involved a lot of prevention in this area” (P2); “I was very sensitized by my pharmacist colleague who works on bisphenol A” (Pa12)
- Rurality: “I think that here in the countryside we still have a population that is, uh… interested in it anyway” (P1)
- Pregnancy-parenthood: “my midwife told me about it and then I was told about it in the hospital, I think” (Pa2)
- Fatalism: “at the same time a feeling of helplessness…there are still many things you can’t get your hands on” (Pa4)
- Risk perception: “It can still be dangerous” (Pa1); “It’s hard, very hard to quantify... uh... that’s something that’s hard to actually touch, to palpate” (P5)
- Fear of judgment: “When you left stuff with which you can write, I didn’t have much to say because I was afraid of saying something stupid” (Pa5).
- Interest and curiosity: “I could talk for hours about this I think so much that I’m interested” (P2); “Those who told me about it were already fairly aware” (Pe6); “they still have a some curiosity” (M11)
- ED exposure prevention behavior: “I had already changed a lot in terms of cosmetics since the beginning of my pregnancy” (Pa4); “It’s true that I have a tendency to... so I buy a little more organic than before” (Pa5); “I avoid everything aluminum, cellophane, things like that” (P2).
Physician profiles were described in terms of clinical case experience, personal norms and stereotypes:
- Clinical case experience: “When we see in consultation boys with micro penises, […] or other pathologies where we can possibly suggest endocrine disrupters” (Pe7); “The parents I spoke to were either from a wealthy background or health professionals” (Pe6).
- Personal norms: “I’m not too bobo bio bike quinoa. It is not my culture” (Pe3); “I would say that it could be useful but not to all audiences, we are the audiences who do not master the reading” (M11)
- Stereotypes: “The parents here are, from an often very precarious environment and I think they don’t care” (Pe2); “It’s more of a middle-of-the-road thing a little bit, a little intellectual, those who ask themselves a lot of ecological questions” (Pe5); “We still have a diverse population, endocrine disruptors, it’s something of an elite problem” (M6)
- (c)
- The environment of the MEDPREVED strategy was important: filling in at home or in the waiting room, what mattered was a quiet environment and the time needed.
- Calm places: “it was pretty quiet so I could concentrate on answering these questions” (P2); “it’s better [to do it in the waiting room] because once I went home I wouldn’t have had time to do it” (Pa12); “In the waiting room you have to manage the child, not sure you can complete a questionnaire at the same time” (Pe6)
- To have time: “it was a way to wait, it was very good” (Pa5); “it keeps them busy in the meantime, it’s not stupid because they are all on their mobile phones in the waiting room” (M2); “I try not to be late so in the waiting room there is not too much waiting either” (Pe7); “It must also depend on the waiting rooms, at home they wait quite little, it is exceptional that they wait even 20minutes, I am not too late” (M10).
The waiting room is an adapted place for prevention because posters are attractive, but not for all because of infobesity
- Attractive: “That’s exactly what attracted me, when I saw the QR code, in the waiting room I thought, Well, I’ll look where it leads” (Pa12).
- Infobesity: “There are too many signs in waiting rooms, it won’t get enough attention for me” (Pe2); “Not sure people are taking the time to read the posters” (Pe6)
- Covid19: “Heu…. It’s true that right now it’s not the best place because of COVID” (M9)
- Alternatives: “I pasted the QR code on my desk” (Pe7)
- 2.
- The beginning of talk about ED exposure prevention seemed not feasible, mainly because of lack of time and opportunity to prioritize the subject:
- Lack of time: “we don’t have much time with the doctor so we won’t take twenty minutes here to discuss” (P5); “not the time and not the money and a consultation of two hours paid 25 euros, it doesn’t interest me anymore” (Pe1); “Don’t want to talk about endocrine disrupters when I already know I’m going to be late” (Pe5)
- Lack of prioritizing: “It doesn’t seem to me to be the priority of priorities (…) in 20 minutes I really deal with priorities of priorities”(Pe5); “Smoking, screens, food… I have lots of hobbies” (Pe1); “there are other things to talk about when you first see people” (M11); “I’m talking about endocrine disrupters like I’m talking about toxoplasmosis, lifestyle, sports and really it’s part of the three-quarter-hour consultation, that’s really it” (M1).
Moreover, the profiles of physician such as his/her openness, lack of training or science scepticism influence feasibility:
- Physician openness: “I am quite aware as an individual, it is a subject that touches me a lot” (Pe4)
- Lack of training and legitimacy: “the problem is also that we are not sufficiently trained” (Pe2); “I don’t feel like giving prevention speeches on a subject I don’t master” (Pe2); “Even during the studies we had one or two courses, I don’t even know by whom, nor in what subject” (M8)
- Skepticism: “the lack of reliable studies and (…) is a bit like pediatrics and eating? with the impression that every two years there is a new trick that comes out, that contradicts itself a bit” (Pe1); “We are still in a kind of blur I find” (Pe4)
- Relationship: “she played a somewhat more reassuring role” (P3).
2.3. Usefulness
The principal uses of the MEDPREVED strategy are reflexive investment, the intention to maintain or adopt healthy behaviour and, the beginning of talk about ED exposure prevention.
- Personal reflexive investment: “it made me think a lot at night” (P1); “there I really realize that I have no control over...” (P11); “I think that the questionnaire should arouse people’s curiosity and that’s good” (Pe2); “The idea of the questionnaire as it is a great idea, it can help to start the discussion” (Pe2); “I had forgotten but it allowed me to... get it in my head” (Pa10); “they found it interesting for the most part, many of them told me what! […] but it was for them, something they discovered” (M9).
- Healthy behavior to maintain or to adopt: “Maybe in the future, maybe pay more attention to what you buy” (P8); “It revives good habits” (Pa12); “...it made me do something I’ve been thinking about for a long time, which is buying a filter for drinking water” (Pa4).
- Talk with his/her entourage: “I realize when I talk about it, now I realize that everyone is in the same level of knowledge as me” (P3).
- Beginning of talk about ED exposure with HP: “it makes us go to the doctor because I think that if the doctor himself has to go to each person it can take him time so …” (P8); “it could be a very good “hook” for a talk” (Pe1).
- Talk could help to change: “The doctor asked me what I was washing her backside with […] I bought a... a supermarket thing you know the supermarket pchit-pchit there. She said, “Well, that’s not great”. There you go. So, it’s true that after I got home she said, “water’s better,” so I replaced that little thing with water (laughs)” (Pa5).
- But it is rarely done: “I didn’t think to talk to the doctor after” (P5); “Behind it you have to have answers to offer them what (…) If you don’t have solutions to propose behind…” (Pe4); I have no concrete feedback because I don’t necessarily talk about it (M3).
- Collective reflexive Investment: “We’re not super informed about uh...about all that” (P6).
The questionnaire’s form and contents were criticized, and its anxiety-provoking aspect was highlighted:
- Form: “Is it useful to answer a questionnaire when we won’t have the answers and information... yeah I don’t know?” (Pa1); “it is true that in the end I expected to have a little doc’ to just uh... we will say recall essential points and even if we can discuss it after...” (Pa9); “But then you don’t have the answer” (M7).
- Content: “because there were no answers, it leads to more questions than answers” (P9); “I feel like I’m still misinformed, actually” (Pa4).
- Anxiety-provoking or guilt feeling or powerlessness: “it’s hard to spend time eating well, eating healthy, eating organic… There is this time constraint” (P3); “Rather guilty, almost distressing, when you have to question everything you eat, buy” (Pe6); “One thing that keeps me from talking to parents is the anxiety side” (Pe4).
Some solutions are highlighted: (i) the central role of all HPs, who must be trained about environmental health and health education methods, during dedicated consultations using the PREVED questionnaire for priority populations; (ii) the prevention kit, which has been particularly appreciated by patients; (iii) the prevention campaign.
- HP role priority: “It would indeed reassure me to have very precise information coming from a medical authority” (Pa4); “if it is already something given by health professionals, we can really have confidence” (Pa11).
- HP training on ED topic and on health education methods: “I also think we need to adapt it…to the audience we have, because we can scare everyone after the person who is starving if we tell them that in addition to buying their canned goods, they are poisoning themselves … that’s not a good message either” (Pa12).
- Dedicated consultations: “We should really talk about it during the follow-up consultation of the “x” months or gender at the annual consultation” (Pe2); “Ah, it must not be at the same time as anything else, I think. It has to be dedicated to that” (Pa6); “Since I can’t organize that at every consultation, basically the dedicated consultation would be a good idea” (M9).
- Or not: “I think that [a fully dedicated consultation] could really stress me out.” (Pa10); “Birth preparation classes are about feeding the baby so there could be...a course on the baby’s environment because we’re talking in the classes about life after birth” (Pa6); “It’s complicated to do the whole thing on top” (M1).
- By all HP: “The pediatrician has a role to play” (Pe6) -“it should be done as soon as patients know they are pregnant (…) should intervene early” (Pe1); “Other professionals also have a say: in antenatal consultations midwives and gynecologists must brief parents well upstream, before we do” (Pe6); “pediatricians or doctors can play their role, especially in the patient-caregiver relationship” (Pa7).
- Questionnaire systematically for one and all: “give a brochure systematically with the QR code written on it” (Pe2); “adults are also affected by endocrine disrupters” (Pa1); “Maybe there should be flyers with QR code given in addition to consultation” (M1).
- On the contrary, target a specific population: “People who are really interested in it don’t need the doctor to tell them about it” (Pe5); “You need to talk about it more,... some people have heard the word but don’t necessarily know” (Pa6).
- Consulting group: “After no kind of Tupperware meeting and nobody will ever go” (Pa5).
- Prevention kit: “There is one that has images, which is much simpler, has much less text and is much more telling” (P10); “Platelets with just simple things that they can do, that’s really what I want to go on” (Pe4); “I think it’s good, they take it because I have more” (M10).
- Prevention campaign for the general population: “There are not enough prevention campaigns, I think.” (Pe6); “There are a lot of things, prevention, when it’s taught in school and it goes down the road and it works. But it means that it has to go through the State” (Pa6).
Among HP, only five paediatricians had a patient who talked about ED exposure after having filled in the questionnaire versus 13 in GP.
Among training kit resources, GPs preferred the video (13/26), the URPS guide (8/26) and the Inserm website (2/26). Among prevention kit resources, GP preferred the ARS flyer (11/26), the video (10/26), the Mpedia guide (9/26) and the ARS guide (6/26). The regional website was preferred to the National one.
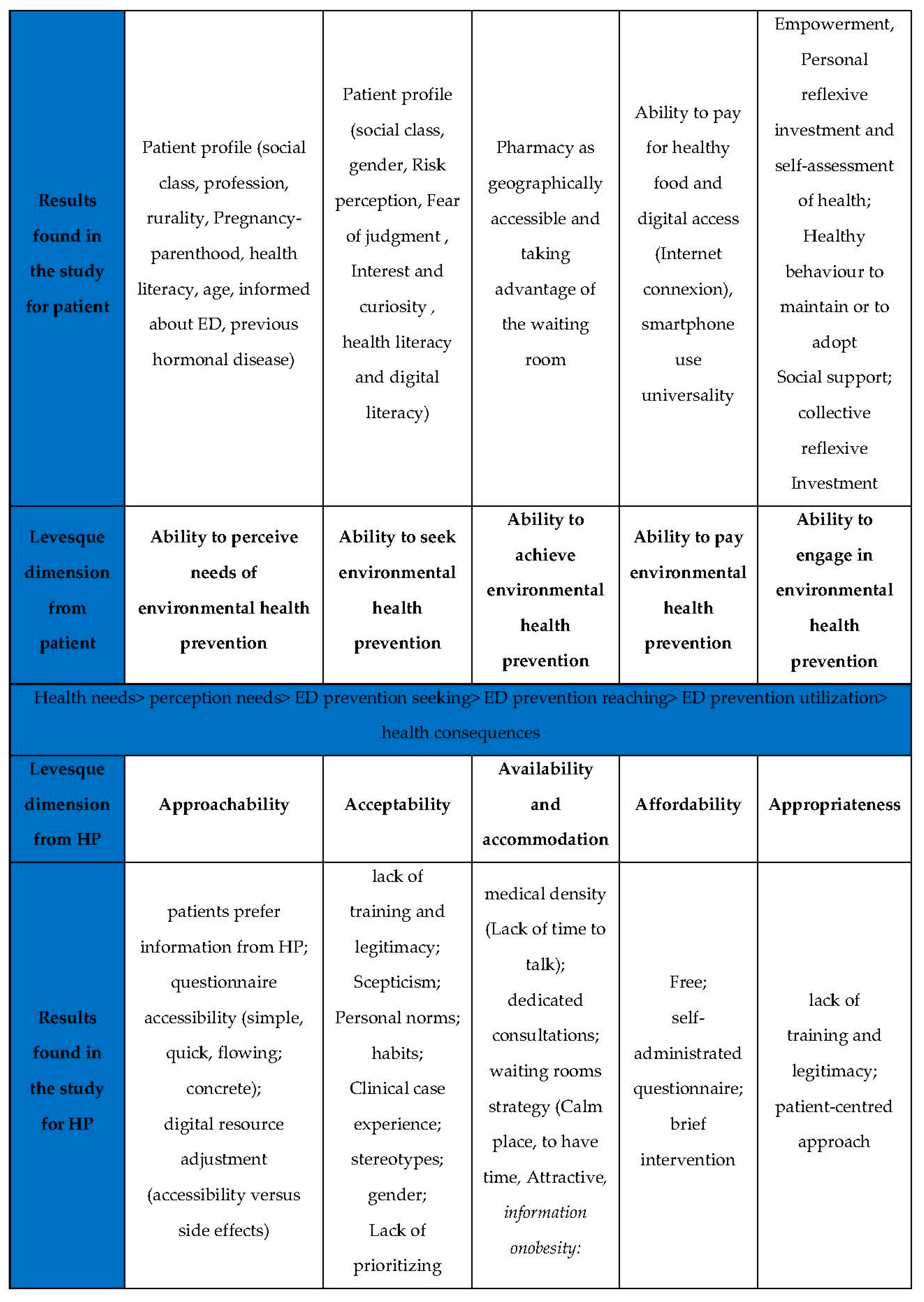
From these results, we tried to use the Levesque model to highlight the determinants related to the patient and the determinants related to the health system in accessing the ED prevention (Figure 2). In the center of the figure, Levesque described health steps: health needs, perception of needs, ED prevention seeking, ED prevention reaching, ED prevention utilization and health consequences. For each step, he described dimensions from patient (upper part of figure) and dimension from HP (lower part of figure). We added the results found in the study for the patient (first line) and HP (last line) in front of these dimensions.
Figure 2.
Results implemented in Levesque model.
3. Discussion
In our study, we utilized Levesque’s patient dimensions (from 1 to 5) and professional dimensions (from 6 to 10) in examination of an environmental health prevention tool.
3.1. Ability to Perceive Needs of Environmental Health Prevention
From points of view expressed in this study, we found this to be a major determinant of MEDPREVED strategy use. Ability to perceive needs appeared associated with socio-professional level; the patient with lower status had less perception. Indeed, socio-professional level is known to be related to health literacy [33]: persons with low health literacy level are more vulnerable and exposed to environmental pollutants and less compliant to healthy lifestyles. Indeed, they are less inclined to use prevention or screening programs [34,35].
Moreover, younger persons seemed less inclined to perceive health environmental prevention needs then older persons. Younger persons, such as pregnant women or the parents of young children, are seen by health professionals as the target population to educate.
Finally, participants in our study were already well-informed about ED. Information and sensitization to health topics improves with social category, probably by better information dissemination in the upper social classes. Information is a determinant of risk perception on which behaviour change depends [36]. This result confirms that knowledge, beliefs, attitudes and practices of patients concerning this topic are a major determinant of ED prevention access.
3.2. Ability to Seek Environmental Health Prevention
From points of view expressed in this study, we found that the second Levesque patient dimension, the ability to seek ED prevention, is present and associated with patient profile such as social class, gender, health literacy and digital literacy.
In our study, patient participants were predominantly women, which is concordant with literature data showing that mothers are known to be more concerned than fathers about health [37].
In our study, while many patient participants predominantly found the PREVED questionnaire easy to understand, but some of them judged it overly complex, with too much medical jargon. This lack of health literacy could certainly affect the ability to seek environmental health prevention.
Moreover, our study used a digital tool to implement the PREVED questionnaire. This could have affected persons with low digital literacy. Indeed, persons with low literacy level have less access to digital tools and are less likely to use or perceive health information technology tools as easy or useful [38]. Illectronism, which increased with the COVID-19 crisis, is a key element of this Leveque dimension, as it defines the digital divide, which increases health inequalities. In France, in 2022, 30% of persons more than 65 years of age do not have Internet [39]. It is essential to locate these situations so as to avoid care renouncement.
3.3. Ability to Achieve Environmental Health Prevention
From the points of view expressed in this study, we found that this third Levesque’s patient dimension, the ability to seek ED prevention, is present insofar as geographic location of the practice as a site for education is not a problem because it is near people’s homes. Indeed, patients visit health professionals for different health reasons and take advantage of the waiting room. Moreover, our study was carried out in both rural and urban areas with the same result.
Patient transport is not a problem because PREVED can be filled in everywhere through the QR code. It permits universal access and personal usefulness.
3.4. Ability to Pay for Environmental Health Prevention
From the points of view expressed in this study, we found that the ability to pay for environmental health prevention was rarely mentioned. As income is associated with the ability to pay for healthy food [40], and some health professionals highlighted the difficulty of educating low-income patients. Moreover, while filling in the PREVED questionnaire is free of charge, it requires digital access (Internet connection and smartphone).
3.5. Ability to Engage in ED Prevention
From the points of view expressed in this study, we found an ability to engage in environmental heath prevention through the empowerment concept. Our study has shown that the PREVED questionnaire develops self-reflection and self-assessment of health. By this reflexive approach, many participants have become actors in their prevention by changing some of their practices, while others have become aware of a real lack of knowledge and have deepened their knowledge of the subject using computer resources.
One condition of this empowerment appears to be social support. Indeed, educating the whole family instead of one person is more efficient. Social support allows the patient to identify peers who can help them in a practical way in their behaviour change [41]. According to the health determinants model [42], social relationships and patient networks are among the most important factors with positive or negative influences on health.
3.6. Approachability
Approachability refers to transparency outreach, information, screening. From the points of view expressed in this study, we identified a lever of approachability: patients preferred information from HPs or the government than other sources because they appeared more reliable than industrial sources [43,44].
Moreover, we identified a limitation factor regarding approachability: according to one person, the questionnaire was judged to be overly complex, with too much medical jargon. The PREVED questionnaire should perhaps be improved according to health literacy levels [33].
Approachability depends on digital resource adjustment (QR code).
Patient are facing digital information through the Internet, which is a key source of accessible health information [45]. The Internet appeared in this study to have several advantages: it is convenient, democratized, universal, remotely accessible, usable, and fast to use, allowing users to pause when and where they want. This could be explained by a young survey population, corresponding to a generation accustomed to the digital [46]. Nowadays, digital applications are common in clinical prevention practices, for example for gestational age calculation [47], physical exercise measurement [48], cardiovascular risk factor measurement [49], weight loss measurement [50], skin cancer prevention [51] with an application where a person could be shown on a screen with the consequences of unprotected sun exposure on his or her face [52]. The smartphone can be useful in health promotion by encouraging a healthier lifestyle [53]. Patients who are satisfied with the digital form would be more likely to report health information about themselves on a regular basis, which could help in better monitoring and adaptation of advice from HP [54]. Moreover, in the pandemic context, the digital format appeared in the waiting room to be more hygienic compared to the paper format, which could be a vector of potentially pathogenic microorganisms [55].
However, several side effects have been demonstrated. Tools are not adapted for every age. For example, digital aids to discuss sexual health with HPs are acceptable and feasible to implement in younger populations but need testing with older patients so as to overcome uncomfortable feelings [56]. Tools are not adapted to low-income populations [57], and may even exacerbate health inequalities [58,59]. Moreover, they are sometimes anxiety-provoking [52]. While different supports, such as video-based digital health interventions (video clips), interactive tailored messages, graphics, are now possible, digital health education should follow the health education guidelines [60], with positive messages and video intervention in clinical settings [61]. For example, parents are five times less attentive to their child’s request for attention when using a telephone [62] and its use in a waiting room is a counter-productive message of reasoned smartphone utilization.
3.7. Acceptability
Acceptability refers to professionals’ values, norms, culture, and gender. From the points of view expressed in this study, we identified that HPs may have little belief in their effectiveness in prevention, even though prevention requires belief in its effectiveness [63], unfortunately, training in health education and in environmental health are limited during curricula. Indeed, several studies of American paediatricians showed that while they were interested to include environmental health in their practices, they were limited by a lack of training [64]. In France in 2017, a study indicated that out of 962 perinatal HPs, 74% recognize a lack of knowledge to address environmental health with their patients [65]. In fact, in a survey of 752 French GPs, only one out of four doctors reported having had training in environmental health (5% as part of their initial training and 21% as part of continuing education) [66].
We observed that HPs’ habits influence their MEDPREVED strategy adoption and prevention practice [67].
We observed that female HPs were more likely to respond to our survey.
We observed that the beginning of discussions was not encouraged by HPs faced with low-income patients. Some HPs did not integrate environmental health in their preventive practices because this topic was poorly comprehended. Indeed, HPs could consider that health subjects are the prerogative of affluent populations [37,68,69,70,71], a phenomenon which is described in the literature on stereotypes and discrimination [72].
We observed that the topic was not prioritized by HPs as they think scientific data are not robust enough and they prefer their prevention comfort zones, such as the elimination of tobacco consumption [73]. Lack of time and fear of provoking anxiety, notably from paediatricians who see pregnant women as vulnerable, are other dissuasive factors. The education of pregnant women about ED requires a positive discourse, as we have argued elsewhere [11].
3.8. Availability and Accommodation
Availability and accommodation refer to geographic location, accommodation, hours of opening, appointment mechanisms.
Geographical location positively influenced it accessibility, given the fact that equal shares of the population in the waiting rooms surveyed were living in rural and urban areas. A limitation factors could have been the medical density in our region. It may decrease further for a few years, making access to, and availability for, consultations more difficult. The share of prevention in general practices is currently estimated to exceed more than 30% of the general practitioner’s working time [74], which remains low and could be impacted by the decrease in general practitioners in some areas.
Accommodation (waiting room) is an essential point of this study whereas, in the pandemic period patient waiting time decreased [75], which may have impacted the MEDPREVED poster visibility and the time taken to complete the PREVED questionnaire.
MEDPREVED strategy allowed patients to take care of themselves before their consultation facilitating patient patience. We found that a lack of time and fees-for-service are not conducive to clinical prevention practices, specifically health education as described in the literature [76] and not all HPs grasp the waiting room as a prevention site [77], whereas it is an appropriate place to deliver prevention messages and promote health from both the physicians’ and patients’ perspectives [22,78,79]. Indeed, several studies have underlined the efficacy of this prevention tool: Besera et al. [64] showed in the USA that a low-resource video intervention for waiting rooms can provide sufficient exposure to positively influence sexually transmitted disease-related attitudes/behaviours; Eubele et al. [80] showed in Belgium that exposure to an audio-visual message about anti-tetanus vaccination was associated with an increase in the number of tetanus vaccine prescriptions. Several authors showed that video-formatted oral hygiene health education dental waiting rooms was effective in educating patients and instigating both immediate and sustained self-reported behaviour change (reduction in sweets consumption, reducing cavity rates) [52,81,82]. Single-session, video-based interventions can be highly cost-effective when implemented at scale [83].
If waiting rooms are salutogenic-designed, with plants reducing stress [84] or visual art [85,86], prevention information can increase patient awareness of certain health topics. Without salutogenic-design, posters alone are not necessarily effective in behaviour change [87,88]. However, as is shown in a French study on 60 HPs, none of them have a clearly defined strategy, mostly because they do not know how to act after risk factor screening [22,89]. In our study, HPs had the freedom to choose the document from the prevention kit that could be made accessible also in waiting rooms, as recommended by some authors [90].
3.9. Affordability
Affordability refers to direct, indirect and opportunity costs. MEDPREVED strategy is fee-free. It hypothesizes that as HPs do not have enough time during consultation, waiting time should be used with a self-administrated questionnaire. These tools (paper or online questionnaires, software) in primary care can be of help for the HP in overall patient management and follow-up, with early identification and a more rapid assessment of risk behaviours. Their utilisation has recently increased in Canada [91].
However, some respondents of our study proposed a hetero-administrated questionnaire containing the remarks and attitudes of the patients. Even if France belongs to the group of countries with the longest primary care consultation time, with an average of 16 min (compared to an average of 7 min for Germany and Spain) [92], there is clearly a lack of HP availability to address ED. In the French context of fee-for-prevention clinical practices, if adopted, the hetero-administrated questionnaire would be very quick. For example, HPs could ask two questions to each patient who, such as “Do you smoke?” and “Do you want to quit smoking?”; such questions have significantly increased the smoking cessation success rates [93,94]. This brief intervention in likewise effective with regard to physical exercise [95], fruit and vegetable consumption [96] or alcohol consumption in different populations [97,98,99]. HPs can use the 5A tool (Assess, Advise, Agree, Assist, Arrange) to support behaviour respecting the patient’s priorities and autonomy [100,101]. The structure of the PREVED questionnaire, both in its layout and in its length or simplicity of understanding, has made it accessible to many patients and could be utilized again in a brief intervention.
3.10. Appropriateness
Appropriateness refers to technical and interpersonal quality, adequacy, coordination, and continuity.
Whereas the interviewed HPs seemed to practice a global, biopsychosocial medicine, focusing on the patient-centred approach, excluding the traditional attitude of full control with a passive patient, encouraging the patient to be empowered [102], our main result was that the initiation of a discussion after the filling-in of the PREVED questionnaire was rare. The principal reason seems to be the lack of medical training in environmental health [103,104] and the wish to adapt an adaptive discourse [65,105,106,107,108,109] before using practical tools.
The MEDPREVED strategy is not inseparable from medical training. It could be improved by adding prevention kits to the QR code and delivering a paper with the QR code or internet site link at home for the whole family [110].
4. Strengths and Limits
The mixed method, with the guarantee of a collection of anonymised data, was appropriate, favouring the free expression of feelings, highlighting opinions on the device and objectifying practices. In qualitative studies, data saturation was obtained by the number of interviews carried out [111] and triangulation of the data during the analysis made it possible to limit interpretation errors. Interviews with participants were sometimes conducted at a distance from the completion of the questionnaire. As a result, loss of information was sometimes possible. In order to mitigate this limitation, some interviews were conducted just after the PREVED questionnaire was completed. There was also a selection and recruitment bias. Indeed, the participants may not be representative of the general population or of French health professionals. They may have been interested in the subject beforehand, whether they are professionals or patients.
5. Conclusions
The simplified MEDPREVED strategy is mostly feasible, accessible, and useful in clinical prevention practices. Compared to Levesque dimensions, at patient and HP levels, the MEDPREVED strategy has confirmed the same limiting factors and levers to access to ED prevention: need perception, ability to seek, reach and use ED exposure prevention. Analysis of this strategy could improve access to endocrine disruptor exposure prevention. The teachable moment could occur in every care setting. Further study is needed to measure the impact on knowledge, risk perception and behavior of beneficiaries of the MEDPREVED strategy in the medium and long term.
Author Contributions
Conceptualization, M.A.; methodology, M.A. software, J.P. validation, M.A. and A.D.; formal analysis, M.P., L.D., Z.B., M.N. and A.L.; investigation, D.R., M.P., L.D., Z.B., M.N. and A.L. data curation, A.-S.G., M.P., L.D., Z.B., M.N. and A.L. writing—original draft preparation, M.A.; writing—review and editing, V.M. and A.D.; supervision, M.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding but the original questionnaire PREVED whose development and validation has been funded the “Fondation de France” gantt n°2015 00060744.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Poitiers University (Declaration RGPD).
Informed Consent Statement
Every participant has been informed and give their consent to participate.
Data Availability Statement
All verbatims are available from Marion Albouy.
Acknowledgments
The authors thank all the participants. The authors would also like to thank the Cognition and Learning Research Center for its contribution to the digitalization of the psychosocial questionnaire. We likewise wish to thank Jeffrey Arsham, American English native speaker and English teacher at the University of Poitiers, for his help in preparation of the English version of this publication. We likewise wish to thank the “Fondation de France” who brought its financial support for the PREVED study by grant no. 2015 00060744.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Barouki, R.; Gluckman, P.D.; Grandjean, P.; Hanson, M.; Heindel, J.J. Developmental Origins of Non-Communicable Disease: Implications for Research and Public Health. Environ. Health 2012, 11, 42. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, Z.-H.; Zhang, J.; Huang, R.-P.; Yin, H.; Dang, Z. Human Exposure of Bisphenol A and Its Analogues: Understandings from Human Urinary Excretion Data and Wastewater-Based Epidemiology. Environ. Sci. Pollut. Res. Int. 2020, 27, 3247–3256. [Google Scholar] [CrossRef]
- Biesterbos, J.W.H.; Dudzina, T.; Delmaar, C.J.E.; Bakker, M.I.; Russel, F.G.M.; von Goetz, N.; Scheepers, P.T.J.; Roeleveld, N. Usage Patterns of Personal Care Products: Important Factors for Exposure Assessment. Food Chem. Toxicol. 2013, 55, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Hanson, M.; Gluckman, P. Developmental Origins of Noncommunicable Disease: Population and Public Health Implications. Am. J. Clin. Nutr. 2011, 94, 1754S–1758S. [Google Scholar] [CrossRef]
- Di Renzo, G.C.; Conry, J.A.; Blake, J.; DeFrancesco, M.S.; DeNicola, N.; Martin, J.N.; McCue, K.A.; Richmond, D.; Shah, A.; Sutton, P.; et al. International Federation of Gynecology and Obstetrics Opinion on Reproductive Health Impacts of Exposure to Toxic Environmental Chemicals. Int. J. Gynaecol. Obstet. 2015, 131, 219–225. [Google Scholar] [CrossRef]
- Carwile, J.L. Canned Soup Consumption and Urinary Bisphenol A: A Randomized Crossover Trial. JAMA 2011, 306, 2218. [Google Scholar] [CrossRef]
- Rudel, R.A.; Gray, J.M.; Engel, C.L.; Rawsthorne, T.W.; Dodson, R.E.; Ackerman, J.M.; Rizzo, J.; Nudelman, J.L.; Brody, J.G. Food Packaging and Bisphenol A and Bis(2-Ethyhexyl) Phthalate Exposure: Findings from a Dietary Intervention. Environ. Health Perspect. 2011, 119, 914–920. [Google Scholar] [CrossRef]
- Sathyanarayana, S.; Alcedo, G.; Saelens, B.E.; Zhou, C.; Dills, R.L.; Yu, J.; Lanphear, B. Unexpected Results in a Randomized Dietary Trial to Reduce Phthalate and Bisphenol A Exposures. J. Expo. Sci. Environ. Epidemiol. 2013, 23, 378–384. [Google Scholar] [CrossRef]
- El Ouazzani, H.; Fortin, S.; Venisse, N.; Dupuis, A.; Rouillon, S.; Cambien, G.; Gourgues, A.-S.; Pierre-Eugène, P.; Rabouan, S.; Migeot, V.; et al. Perinatal Environmental Health Education Intervention to Reduce Exposure to Endocrine Disruptors: The PREVED Project. Int. J. Environ. Res. Public Health 2021, 19, 70. [Google Scholar] [CrossRef]
- Ouazzani, H.E.; Rouillon, S.; Venisse, N.; Sifer-Rivière, L.; Dupuis, A.; Cambien, G.; Ayraud-Thevenot, S.; Gourgues, A.-S.; Pierre-Eugène, P.; Pierre, F.; et al. Impact of Perinatal Environmental Health Education Intervention on Exposure to Endocrine Disruptors during Pregnancy-PREVED Study: Study Protocol for a Randomized Controlled Trial. Trials 2021, 22, 876. [Google Scholar] [CrossRef]
- Rouillon, S.; El Ouazzani, H.; Hardouin, J.-B.; Enjalbert, L.; Rabouan, S.; Migeot, V.; Albouy-Llaty, M. How to Educate Pregnant Women about Endocrine Disruptors? Int. J. Environ. Res. Public Health 2020, 17, 2156. [Google Scholar] [CrossRef] [PubMed]
- Essi, M.J. The KAP Survey. Health Sci. Dis. 2013, 14, 1–3. [Google Scholar]
- Soto, J.C.; Chauvet, M.L.; Groulx, S.; Provost, S. The Practice and Acceptance of Physician Preventive Medicine Services in a Montreal University Hospital and the Obstacles That Deter Their Implementation. Can. J. Public Health 2010, 101, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Castéra, P.; Maurat, F.; Fleury, B.; Démeaux, J. Peut-on Repérer «en Routine» Les Mésusages d’alcool? Médecine 2007, 3, 330–334. [Google Scholar]
- Gil-Llario, M.D.; Ruiz-Palomino, E.; Morell-Mengual, V.; Giménez-García, C.; Ballester-Arnal, R. Validation of the AIDS Prevention Questionnaire: A Brief Self-Report Instrument to Assess Risk of HIV Infection and Guide Behavioral Change. AIDS Behav. 2019, 23, 272–282. [Google Scholar] [CrossRef]
- Langevin, V.; François, M.; Boini, S.; Riou, A. Les questionnaires dans la démarche de prévention du stress au travail—Article de revue—INRS. Doc. Méd. Trav. 2011, 125, 23–35. [Google Scholar]
- Moula, H.; Mercier-Nicoux, F.; Velin, J. Un Questionnaire-Amorce de Dialogue Peut-Il Optimiser La Consultation d’un Adolescent En Médecine Générale? Evaluation d’un Questionnaire de Prévention Auprès de 347 Adolescents Examinés Par 41 Médecins Généralistes. Rev. Prat. Méd. Gén. 2001, 533, 741–746. [Google Scholar]
- Ricci, G.; Castelpietra, E.; Romano, F.; Di Lorenzo, G.; Zito, G.; Ronfani, L.; Biffi, S.; Monasta, L. Case-Control Study to Develop and Validate a Questionnaire for the Secondary Prevention of Endometriosis. PLoS ONE 2020, 15, e0230828. [Google Scholar] [CrossRef]
- MSSS Canada Guide Des Bonnes Pratiques En Prévention Clinique. Available online: https://www.msss.gouv.qc.ca/aide-decision-app/etape.php?situation=pc-adulte (accessed on 6 June 2022).
- Ryu, S. Book Review: MHealth: New Horizons for Health through Mobile Technologies: Based on the Findings of the Second Global Survey on EHealth (Global Observatory for EHealth Series, Volume 3). Health Inform. Res. 2012, 18, 231–233. [Google Scholar] [CrossRef]
- Chevallier, P.; Colombet, I.; Chatellier, G.; Wajs, C.; Leneveut, L. Une Consultation de Prévention Dédiée et Structurée à l’aide d’un Outil Informatique. Étude C-PRED-EsPeR: Nouveau Concept Pour La Vraie Vie? Exerc. Rev. Fr. Méd. Gén. 2008, 81, 36–41. [Google Scholar]
- Gignon, M.; Idris, H.; Manaouil, C.; Ganry, O. The Waiting Room: Vector for Health Education? The General Practitioner’s Point of View. BMC Res. Notes 2012, 5, 511. [Google Scholar] [CrossRef] [PubMed]
- Aujoulat, I.; d’Hoore, W.; Deccache, A. Patient Empowerment in Theory and Practice: Polysemy or Cacophony? Patient Educ. Couns. 2007, 66, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Information for All: European Standards for Making Information Easy to Read and Understand. 2021. Available online: https://www.inclusion-europe.eu/easy-to-read-standards-guidelines/ (accessed on 6 June 2022).
- Video Extract “2 Minutes Tout Compris”: Le Bruit et les Jeunes. eSET-Bourgogne-Franche-Comté. Available online: https://www.bing.com/videos/search?q=2+minutes+tout+compris%e2%80%9d+%3a+Le+bruit+et+les+jeunes.+eSET-Bourgogne-Franche-Comt%c3%a9.&qpvt=2+minutes+tout+compris%e2%80%9d+%3a+Le+bruit+et+les+jeunes.+eSET-Bourgogne-Franche-Comt%c3%a9.&view=detail&mid=9EEB2E7536C0F578AD399EEB2E7536C0F578AD39&&FORM=VRDGAR&ru=%2Fvideos%2Fsearch%3Fq%3D2%2Bminutes%2Btout%2Bcompris%25e2%2580%259d%2B%253a%2BLe%2Bbruit%2Bet%2Bles%2Bjeunes.%2BeSET-Bourgogne-Franche-Comt%25c3%25a9.%26qpvt%3D2%2Bminutes%2Btout%2Bcompris%25e2%2580%259d%2B%253a%2BLe%2Bbruit%2Bet%2Bles%2Bjeunes.%2BeSET-Bourgogne-Franche-Comt%25c3%25a9.%26FORM%3DVDRE (accessed on 6 June 2022).
- Perturbateurs Endocriniens—Inserm, La Science Pour la Santé. Available online: https://www.inserm.fr/dossier/perturbateurs-endocriniens/ (accessed on 6 June 2022).
- Contamination Chimique et Perturbateurs Endocriniens—URPS Médecins Libéraux PACA. Available online: https://www.urps-ml-paca.org/portfolio-item/guide-sur-les-perturbateurs-endocriniens-et-la-contamination-chimique/ (accessed on 6 June 2022).
- Guide Sante Environnement: Des Solutions Pour un Quotidien Plus Sain. Available online: https://www.nouvelle-aquitaine.ars.sante.fr/guide-sante-environnement-des-solutions-pour-un-quotidien-plus-sain (accessed on 6 June 2022).
- Accueillir Bébé dans un Environnement Sain/Particuliers. Available online: https://www.nouvelle-aquitaine.ars.sante.fr/accueillir-bebe-dans-un-environnement-sain-particuliers (accessed on 6 June 2022).
- Ma Maison Santé > Accueil. Available online: https://www.ma-maison-sante.fr/ (accessed on 6 June 2022).
- Guides et Fiches. Available online: https://wecf-france.org/ressources/guides-et-fiches/ (accessed on 6 June 2022).
- Levesque, J.-F.; Harris, M.F.; Russell, G. Patient-Centred Access to Health Care: Conceptualising Access at the Interface of Health Systems and Populations. Int. J. Equity Health 2013, 12, 18. [Google Scholar] [CrossRef] [PubMed]
- Dodson, S.; Good, S.; Osborne, R. Health Literacy Toolkit for Low- and Middle-Income Countries: A Series of Information Sheets to Empower Communities and Strengthen Health Systems; World Health Organization. Regional Office for South-East Asia: New Delhi, India, 2015.
- Panahi, R.; Namdar, P.; Siboni, F.S.; Fallah, S.; Anbari, M.; Dehghankar, L.; Yekefallah, L.; Shafaei, M. Association between Health Literacy and Adopting Preventive Behaviors of Breast Cancer in Iran. J. Educ. Health Promot. 2020, 9, 241. [Google Scholar] [CrossRef]
- Oldach, B.R.; Katz, M.L. Health Literacy and Cancer Screening: A Systematic Review. Patient Educ. Couns. 2014, 94, 149–157. [Google Scholar] [CrossRef]
- Ferrer, R.; Klein, W.M. Risk Perceptions and Health Behavior. Curr. Opin. Psychol. 2015, 5, 85–89. [Google Scholar] [CrossRef]
- Marie, C.; Lémery, D.; Vendittelli, F.; Sauvant-Rochat, M.-P. Perception of Environmental Risks and Health Promotion Attitudes of French Perinatal Health Professionals. IJERPH 2016, 13, 1255. [Google Scholar] [CrossRef]
- Mackert, M.; Mabry-Flynn, A.; Champlin, S.; Donovan, E.E.; Pounders, K. Health Literacy and Health Information Technology Adoption: The Potential for a New Digital Divide. J. Med. Internet Res. 2016, 18, e264. [Google Scholar] [CrossRef]
- Etudes et Résultats—Difficultés d’Accès aux Droits et Discriminations Liées à l’Âge Avancé. Available online: https://www.defenseurdesdroits.fr/fr/etudes-et-recherches/2021/10/etudes-et-resultats-difficultes-dacces-aux-droits-et-discriminations (accessed on 22 February 2022).
- Yoder, R.A. Are People Willing and Able to Pay for Health Services? Soc. Sci. Med. 1989, 29, 35–42. [Google Scholar] [CrossRef]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Whitehead, M.; Dahlgren, G. What Can Be Done about Inequalities in Health? Lancet 1991, 338, 1059–1063. [Google Scholar] [CrossRef]
- Ashley, J.M.; Hodgson, A.; Sharma, S.; Nisker, J. Pregnant Women’s Navigation of Information on Everyday Household Chemicals: Phthalates as a Case Study. BMC Pregnancy Childbirth 2015, 15, 312. [Google Scholar] [CrossRef] [PubMed]
- Farnood, A.; Johnston, B.; Mair, F.S. A Mixed Methods Systematic Review of the Effects of Patient Online Self-Diagnosing in the “smart-Phone Society” on the Healthcare Professional-Patient Relationship and Medical Authority. BMC Med. Inform. Decis. Mak. 2020, 20, 253. [Google Scholar] [CrossRef] [PubMed]
- Bujnowska-Fedak, M.M.; Waligóra, J.; Mastalerz-Migas, A. The Internet as a Source of Health Information and Services. In Advancements and Innovations in Health Sciences; Springer: Berlin/Heidelberg, Germany, 2019; Volume 1211, pp. 1–16. [Google Scholar] [CrossRef]
- Prensky, M. Digital Natives, Digital Immigrants. Gifted 2005, 29–31. [Google Scholar]
- Farzandipour, M.; Nabovati, E.; Anvari, S.; Vahedpoor, Z.; Sharif, R. Phone-Based Interventions to Control Gestational Weight Gain: A Systematic Review on Features and Effects. Inform. Health Soc. Care 2020, 45, 15–30. [Google Scholar] [CrossRef]
- Feter, N.; Dos Santos, T.S.; Caputo, E.L.; da Silva, M.C. What Is the Role of Smartphones on Physical Activity Promotion? A Systematic Review and Meta-Analysis. Int. J. Public Health 2019, 64, 679–690. [Google Scholar] [CrossRef] [PubMed]
- Widmer, R.J.; Collins, N.M.; Collins, C.S.; West, C.P.; Lerman, L.O.; Lerman, A. Digital Health Interventions for the Prevention of Cardiovascular Disease: A Systematic Review and Meta-Analysis. Mayo Clin. Proc. 2015, 90, 469–480. [Google Scholar] [CrossRef]
- Stephens, J.; Allen, J. Mobile Phone Interventions to Increase Physical Activity and Reduce Weight: A Systematic Review. J. Cardiovasc. Nurs. 2013, 28, 320–329. [Google Scholar] [CrossRef]
- Heydari, E.; Dehdari, T.; Solhi, M. Can Adopting Skin Cancer Preventive Behaviors among Seafarers Be Increased via a Theory-Based Mobile Phone-Based Text Message Intervention? A Randomized Clinical Trial. BMC Public Health 2021, 21, 134. [Google Scholar] [CrossRef]
- Brinker, T.J.; Klode, J.; Esser, S.; Schadendorf, D. Facial-Aging App Availability in Waiting Rooms as a Potential Opportunity for Skin Cancer Prevention. JAMA Dermatol. 2018, 154, 1085–1086. [Google Scholar] [CrossRef]
- Bert, F.; Giacometti, M.; Gualano, M.R.; Siliquini, R. Smartphones and Health Promotion: A Review of the Evidence. J. Med. Syst. 2014, 38, 9995. [Google Scholar] [CrossRef] [PubMed]
- Reychav, I.; Arora, A.; Sabherwal, R.; Polyak, K.; Sun, J.; Azuri, J. Reporting Health Data in Waiting Rooms with Mobile Technology: Patient Expectation and Confirmation. Int. J. Med. Inform. 2021, 148, 104376. [Google Scholar] [CrossRef] [PubMed]
- Adé, M.; Burger, S.; Cuntzmann, A.; Exinger, J.; Meunier, O. Magazines in Waiting Areas of Hospital: A Forgotten Microbial Reservoir? Ann. Biol. Clin. 2017, 75, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Malta, S.; Temple-Smith, M.; Hunter, J.; McGavin, D.; Lyne, J.; Bickerstaffe, A.; Hocking, J. Could an Online or Digital Aid Facilitate Discussions about Sexual Health with Older Australians in General Practice? Aust. J. Gen. Pract. 2018, 47, 870–875. [Google Scholar] [CrossRef]
- Cambon, L. Health Smart Devices and Applications...towards a New Model of Prevention? Eur. J. Public Health 2017, 27, 390–391. [Google Scholar] [CrossRef]
- Rattermann, M.J.; Angelov, A.; Reddicks, T.; Monk, J. Advancing Health Equity by Addressing Social Determinants of Health: Using Health Data to Improve Educational Outcomes. PLoS ONE 2021, 16, e0247909. [Google Scholar] [CrossRef]
- Arcaya, M.C.; Arcaya, A.L.; Subramanian, S.V. Inequalities in Health: Definitions, Concepts, and Theories. Glob. Health Action 2015, 8, 27106. [Google Scholar] [CrossRef]
- Bonell, C.; Michie, S.; Reicher, S.; West, R.; Bear, L.; Yardley, L.; Curtis, V.; Amlôt, R.; Rubin, G.J. Harnessing Behavioural Science in Public Health Campaigns to Maintain “social Distancing” in Response to the COVID-19 Pandemic: Key Principles. J. Epidemiol. Community Health 2020, 74, 617–619. [Google Scholar] [CrossRef]
- Harshbarger, C.; Burrus, O.; Rangarajan, S.; Bollenbacher, J.; Zulkiewicz, B.; Verma, R.; Galindo, C.A.; Lewis, M.A. Challenges of and Solutions for Developing Tailored Video Interventions That Integrate Multiple Digital Assets to Promote Engagement and Improve Health Outcomes: Tutorial. JMIR Mhealth Uhealth 2021, 9, e21128. [Google Scholar] [CrossRef]
- Vanden Abeele, M.M.P.; Abels, M.; Hendrickson, A.T. Are Parents Less Responsive to Young Children When They Are on Their Phones? A Systematic Naturalistic Observation Study. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 363–370. [Google Scholar] [CrossRef]
- Aulagnier, M.; Videau, Y.; Combes, J.B.; Sebbah, R.; Paraponaris, A.; Verger, P. Pratiques Des Médecins Généralistes En Matière de Prévention: Les Enseignements d’un Panel de Médecins Généralistes En Provence-Alpes-Côtes d’Azur. Pratiques Organisation Soins 2007, 4, 259–268. [Google Scholar]
- Besera, G.T.; Cox, S.; Malotte, C.K.; Rietmeijer, C.A.; Klausner, J.D.; O’Donnell, L.; Margolis, A.D.; Warner, L. Assessing Patient Exposure to a Video-Based Intervention in STD Clinic Waiting Rooms: Findings From the Safe in the City Trial. Health Promot. Pract. 2016, 17, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Sunyach, C.; Antonelli, B.; Tardieu, S.; Marcot, M.; Perrin, J.; Bretelle, F. Environmental Health in Perinatal and Early Childhood: Awareness, Representation, Knowledge and Practice of Southern France Perinatal Health Professionals. Ijerph 2018, 15, 2259. [Google Scholar] [CrossRef] [PubMed]
- Ménard, C.; Léon, C.; Benmarhnia, T. Médecins généralistes et santé environnement. Evolutions 2012, 26, 1–6. [Google Scholar]
- Underner, M.; Ingrand, P.; Allouch, A.; Laforgue, A.V.; Migeot, V.; Defossez, G.; Meurice, J.C. Influence du tabagisme des médecins généralistes sur leur pratique du conseil minimal d’aide à l’arrêt du tabac. Rev. Mal. Respir. 2006, 23, 426–429. [Google Scholar] [CrossRef]
- Belfrage, A.S.V.; Grotmol, K.S.; Tyssen, R.; Moum, T.; Finset, A.; Isaksson Rø, K.; Lien, L. Factors Influencing Doctors’ Counselling on Patients’ Lifestyle Habits: A Cohort Study. BJGP Open 2018, 2, bjgpopen18X101607. [Google Scholar] [CrossRef]
- Ibanez, G.; Zabar, J.; Cadwallader, J.-S.; Rondet, C.; Lochard, M.; Magnier, A.M. Views of General Practitioners on Indoor Environmental Health Risks in the Perinatal Period. Front. Med. 2015, 2, 32. [Google Scholar] [CrossRef]
- Saposnik, G.; Redelmeier, D.; Ruff, C.C.; Tobler, P.N. Cognitive Biases Associated with Medical Decisions: A Systematic Review. BMC Med. Inform. Decis. Mak. 2016, 16, 138. [Google Scholar] [CrossRef]
- van Ryn, M.; Burke, J. The Effect of Patient Race and Socio-Economic Status on Physicians’ Perceptions of Patients. Soc. Sci. Med. 2000, 50, 813–828. [Google Scholar] [CrossRef]
- Chapman, E.N.; Kaatz, A.; Carnes, M. Physicians and Implicit Bias: How Doctors May Unwittingly Perpetuate Health Care Disparities. J. Gen. Intern. Med. 2013, 28, 1504–1510. [Google Scholar] [CrossRef]
- Buka, I.; Rogers, W.T.; Osornio-Vargas, A.R.; Hoffman, H.; Pearce, M.; Li, Y.Y. An Urban Survey of Paediatric Environmental Health Concerns: Perceptions of Parents, Guardians and Health Care Professionals. Paediatr. Child Health 2006, 11, 235–238. [Google Scholar] [PubMed]
- Gallois, P.; Vallée, J.; Noc, Y.L. Prévention En Médecine Générale. Deuxième Partie: Regards Croisés Patients-Médecins. Médecine 2008, 4, 406–410. [Google Scholar]
- Ministère des Solidarités et de la Santé Fiche Professionnels de Santé de Ville. Organisation des Cabinets de Ville Dans un Contexte de Poursuite de L’épidémie COVID-19 et en Phase de Déconfinement 2020. Available online: https://www.nouvelle-aquitaine.ars.sante.fr/system/files/2020-05/COVID_19_PS_Fiche_Organisation_Cabinet_Ville_Deconfinement.pdf (accessed on 6 June 2022).
- Franc, C.; Lesur, R. Systèmes de rémunération des médecins et incitations à la prévention. Rev. Économique 2004, 55, 901–922. [Google Scholar] [CrossRef]
- Dodgson, J.E.; Watkins, A.L.; Bond, A.B.; Kintaro-Tagaloa, C.; Arellano, A.; Allred, P.A. Compliance with the International Code of Marketing of Breast-Milk Substitutes: An Observational Study of Pediatricians’ Waiting Rooms. Breastfeed Med. 2014, 9, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Amstutz, C.; Arnold, M.; Bersier, M.; Blanc, M.; Cambridge, É.; Chevey, J.-M.; Dizerens, P.; Gruaz, A.-J.; Michel, C.; Muerner, R.; et al. La salle d’attente idéale existe-t-elle ? Rev. Med. Suisse 2016, 12, 2084–2086. [Google Scholar]
- Marquant Thibaut, M.-L. La Prévention par Exposition d’Affiches dans les Salles d’Attente des Médecins Généralistes: Une Etude Qualitative sur le Ressenti des Patients; Thèse d’exercice en Médecine, Université de Rouen Faculté de Médecine et Pharmacie: Rouen, France, 2018. [Google Scholar]
- Eubelen, C.; Brendel, F.; Belche, J.-L.; Freyens, A.; Vanbelle, S.; Giet, D. Effect of an Audiovisual Message for Tetanus Booster Vaccination Broadcast in the Waiting Room. BMC Fam. Pract. 2011, 12, 104. [Google Scholar] [CrossRef]
- Habermehl, N.; Diekroger, E.; Lazebnik, R.; Kim, G. Injury Prevention Education in the Waiting Room of an Underserved Pediatric Primary Care Clinic. Clin. Pediatr. 2019, 58, 73–78. [Google Scholar] [CrossRef]
- O’CONNOR, P.J.; INNES, J.M. Audio-Visual Information on Child Illness Prevention in Hospital Waiting Rooms: An Experimental Evaluation. Health Promot. Int. 1990, 5, 3–8. [Google Scholar] [CrossRef]
- Williams, A.M.; Gift, T.L.; O’Donnell, L.N.; Rietmeijer, C.A.; Malotte, C.K.; Margolis, A.D.; Warner, L. Assessment of the Cost-Effectiveness of a Brief Video Intervention for Sexually Transmitted Disease Prevention. Sex. Transm. Dis. 2020, 47, 130–135. [Google Scholar] [CrossRef]
- Baldwin, A.L. How Do Plants in Hospital Waiting Rooms Reduce Patient Stress? J. Altern. Complement. Med. 2012, 18, 309–310. [Google Scholar] [CrossRef]
- Beukeboom, C.J.; Langeveld, D.; Tanja-Dijkstra, K. Stress-Reducing Effects of Real and Artificial Nature in a Hospital Waiting Room. J. Altern. Complement. Med. 2012, 18, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Nanda, U.; Chanaud, C.; Nelson, M.; Zhu, X.; Bajema, R.; Jansen, B.H. Impact of Visual Art on Patient Behavior in the Emergency Department Waiting Room. J. Emerg. Med. 2012, 43, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Ashe, D.; Patrick, P.A.; Stempel, M.M.; Shi, Q.; Brand, D.A. Educational Posters to Reduce Antibiotic Use. J. Pediatr. Health Care 2006, 20, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Ward, K.; Hawthorne, K. Do Patients Read Health Promotion Posters in the Waiting Room? A Study in One General Practice. Br. J. Gen. Pract. 1994, 44, 583–585. [Google Scholar] [PubMed]
- Assathiany, R.; Kemeny, J.; Sznajder, M.; Hummel, M.; Egroo, L.D.; Chevallier, B. La Salle d’attente Du Pédiatre: Lieu d’éducation Pour La Santé? Arch. Pédiatrie 2005, 12, 10–15. [Google Scholar] [CrossRef]
- Humphris, G.M.; Field, E.A. The Immediate Effect on Knowledge, Attitudes and Intentions in Primary Care Attenders of a Patient Information Leaflet: A Randomized Control Trial Replication and Extension. Br. Dent. J. 2003, 194, 683–688; discussion 675. [Google Scholar] [CrossRef]
- Sauvageau, C.; Groulx, S.; Pelletier, A.; Ouakki, M.; Dubé, E. Les Médecins Discutent-Ils Des Habitudes de Vie Avec Leurs Patients? Can. J. Public Health 2008, 99, 31–35. [Google Scholar] [CrossRef]
- Irving, G.; Neves, A.L.; Dambha-Miller, H.; Oishi, A.; Tagashira, H.; Verho, A.; Holden, J. International Variations in Primary Care Physician Consultation Time: A Systematic Review of 67 Countries. BMJ Open 2017, 7, e017902. [Google Scholar] [CrossRef]
- Slama, K.; Karsenty, S.; Hirsch, A. Effectiveness of Minimal Intervention by General Practitioners with Their Smoking Patients: A Randomised, Controlled Trial in France. Tob. Control 1995, 4, 162–169. [Google Scholar] [CrossRef][Green Version]
- Stead, L.F.; Buitrago, D.; Preciado, N.; Sanchez, G.; Hartmann-Boyce, J.; Lancaster, T. Physician Advice for Smoking Cessation. Cochrane Database Syst. Rev. 2013, 5, CD000165. [Google Scholar] [CrossRef]
- Vallée, É.; Vastel, É.; Piquet, M.-A.; Savey, V. Efficacité d’un conseil minimal abordant l’activité physique et délivré par les médecins généralistes lors d’une consultation pour renouvellement d’ordonnance. Nutr. Clin. Métabolisme 2017, 31, 194–206. [Google Scholar] [CrossRef]
- Kearney, M.; Bradbury, C.; Ellahi, B.; Hodgson, M.; Thurston, M. Mainstreaming Prevention: Prescribing Fruit and Vegetables as a Brief Intervention in Primary Care. Public Health 2005, 119, 981–986. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fleming, M.; Manwell, L.B. Brief Intervention in Primary Care Settings. A Primary Treatment Method for at-Risk, Problem, and Dependent Drinkers. Alcohol Res. Health 1999, 23, 128–137. [Google Scholar] [PubMed]
- Holloway, A.S.; Watson, H.E.; Arthur, A.J.; Starr, G.; McFadyen, A.K.; McIntosh, J. The Effect of Brief Interventions on Alcohol Consumption among Heavy Drinkers in a General Hospital Setting. Addiction 2007, 102, 1762–1770. [Google Scholar] [CrossRef] [PubMed]
- Kaner, E.F.; Beyer, F.R.; Muirhead, C.; Campbell, F.; Pienaar, E.D.; Bertholet, N.; Daeppen, J.B.; Saunders, J.B.; Burnand, B. Effectiveness of Brief Alcohol Interventions in Primary Care Populations. Cochrane Database Syst. Rev. 2018, 2018, CD004148. [Google Scholar] [CrossRef]
- Puschel, K.; Thompson, B.; Coronado, G.; Huang, Y.; Gonzalez, L.; Rivera, S. Effectiveness of a Brief Intervention Based on the “5A” Model for Smoking Cessation at the Primary Care Level in Santiago, Chile. Health Promot. Int. 2008, 23, 240–250. [Google Scholar] [CrossRef]
- Nakhle, R.; Gache, P.; Humair, J. Le Généraliste Face Aux Quatre Principaux Facteurs de Risque Comportementaux. Rev. Med. Suisse 2006, 80, 2163. [Google Scholar]
- Wonca la Définition Européenne de la Médecine Générale—Médecine de Famille. Available online: https://www.woncaeurope.org/file/afaa93f5-dc46-4b0e-8546-71ebf368f41c/WONCA%20definition%20French%20version.pdf (accessed on 6 June 2022).
- Roberts, J.R.; Balk, S.J.; Forman, J.; Shannon, M. Teaching about Pediatric Environmental Health. Acad. Pediatr. 2009, 9, 129–130. [Google Scholar] [CrossRef]
- Trasande, L.; Schapiro, M.L.; Falk, R.; Haynes, K.A.; Behrmann, A.; Vohmann, M.; Stremski, E.S.; Eisenberg, C.; Evenstad, C.; Anderson, H.A.; et al. Pediatrician Attitudes, Clinical Activities, and Knowledge of Environmental Health in Wisconsin. WMJ 2006, 105, 45–49. [Google Scholar]
- Albouy-Llaty, M.; Rouillon, S.; El Ouazzani, H.; DisProSE, G.; Rabouan, S.; Migeot, V. Environmental Health Knowledge, Attitudes, and Practices of French Prenatal Professionals Working with a Socially Underprivileged Population: A Qualitative Study. Int. J. Environ. Res. Public Health 2019, 16, 2544. [Google Scholar] [CrossRef]
- Gehle, K.S.; Crawford, J.L.; Hatcher, M.T. Integrating Environmental Health into Medical Education. Am. J. Prev. Med. 2011, 41, S296–S301. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, W.J.; Ryder, D.J.; Cooper, H.P.; Williams, D.M.; Weinberg, A.D. Environmental Health: A Survey of Texas Primary Care Physicians. Tex. Med. 2005, 101, 62–70. [Google Scholar] [PubMed]
- Kligler, B.; Pinto Zipp, G.; Rocchetti, C.; Secic, M.; Ihde, E.S. The Impact of Integrating Environmental Health into Medical School Curricula: A Survey-Based Study. BMC Med. Educ. 2021, 21, 40. [Google Scholar] [CrossRef] [PubMed]
- Sanborn, M.; Grierson, L.; Upshur, R.; Marshall, L.; Vakil, C.; Griffith, L.; Scott, F.; Benusic, M.; Cole, D. Family Medicine Residents’ Knowledge of, Attitudes toward, and Clinical Practices Related to Environmental Health: Multi-Program Survey. Can. Fam. Physician 2019, 65, e269–e277. [Google Scholar]
- Morisky, D.E.; DeMuth, N.M.; Field-Fass, M.; Green, L.W.; Levine, D.M. Evaluation of Family Health Education to Build Social Support for Long-Term Control of High Blood Pressure. Health Educ. Q. 1985, 12, 35–50. [Google Scholar] [CrossRef]
- Boddy, C. Sample Size for Qualitative Research. Qual. Mark. Res. 2016, 19, 426–432. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).