Effects and Adaptation of Visual-Motor Illusion Using Different Visual Stimuli on Improving Ankle Joint Paralysis of Stroke Survivors—A Randomized Crossover Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
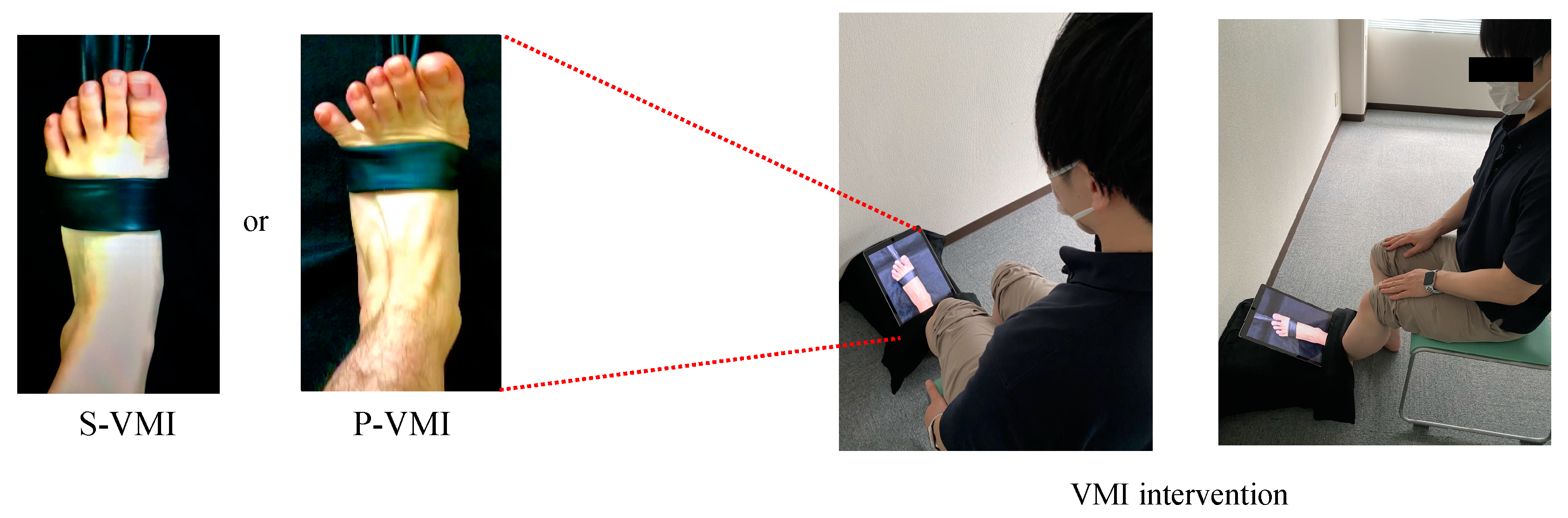
2.3. VMI Intervention
2.4. Outcome Measures
2.4.1. Assessment of Ankle Joint Dorsiflexion Movement
2.4.2. Measuring SoA and Sense of SoO
2.4.3. TMT-B
2.4.4. FMA Lower Extremity Items
2.4.5. SIAS Sensory Items
2.4.6. Measurement of Ankle Plantar Flexor Muscle Tone
2.5. Statistical Analysis
Sample Size
3. Results
3.1. Participants
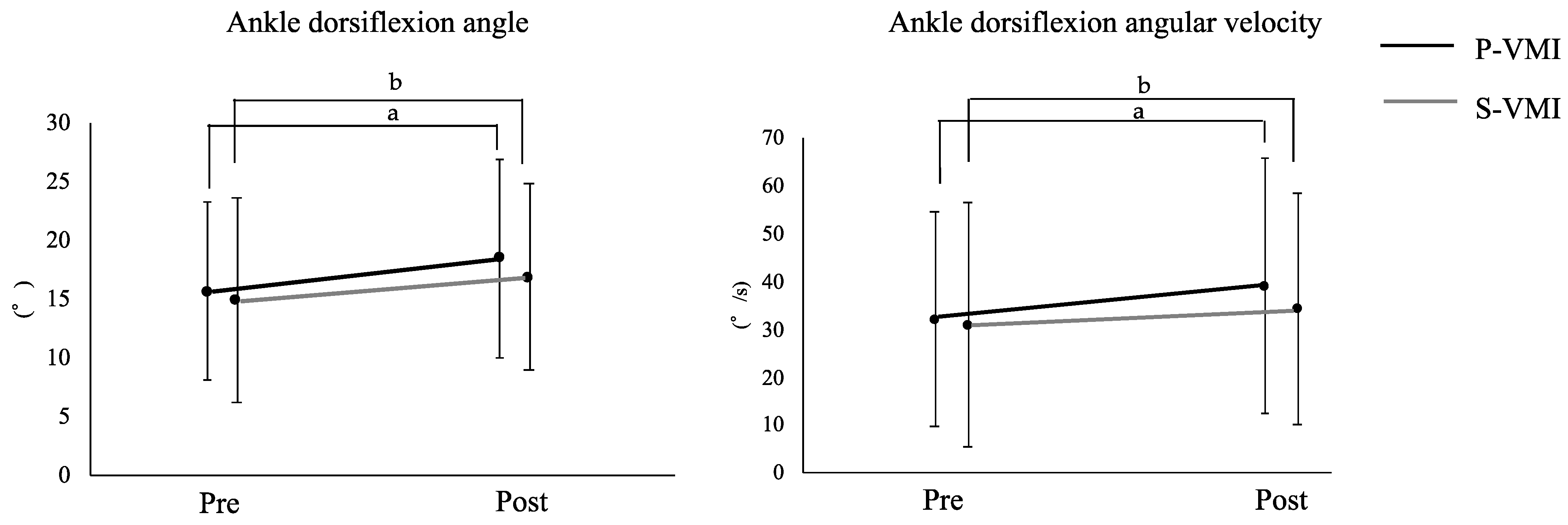
3.2. Comparison of Ankle Dorsiflexion Function between P-VMI and S-VMI
3.3. MCID
3.4. Relationship between the Degree of Improvement of Ankle Joint Function by P-VMI and S-VMI and the Sense of Embodiment (SoA and SoO)
3.5. Relationship between Cognitive Flexibility and Degree of Improvement in Ankle Joint Function by P-VMI and S-VMI
3.6. Relationship between Degree of Improvement in Ankle Function and Physical Function by P-VMI and S-VMI
3.7. Comparison of P-VMI and S-VMI for Sense of Embodiment
4. Discussion
4.1. Comparison of the Effects of P-VMI and S-VMI on Paralyzed Lateral Ankle Dorsiflexion Function
4.2. Relationship between the Degree of Improvement of VMI on the Paralyzed Side of the Ankle Joint Function and the SoA
4.3. Relationship between Cognitive Flexibility and Degree of Improvement in Ankle Joint Function by P-VMI and S-VMI
4.4. Relationship between the Degree of Improvement in Ankle Joint Function and Physical Function with the Use of P-VMI and S-VMI
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Winter, D.A. Human balance and posture control during standing and walking. Gait Posture 1995, 3, 193–214. [Google Scholar] [CrossRef]
- Liston, R.A.; Brouwer, B.J. Reliability and validity of measures obtained from stroke patients using the Balance Master. Arch. Phys. Med. Rehabil. 1996, 77, 425–430. [Google Scholar] [CrossRef]
- Mirjam, D.H.; Geurts, A.C.; Huidekoper, S.C.; Fasotti, L.; Jacques, V.L. Recovery of standing balance in postacute stroke patients: A rehabilitation cohort study. Arch. Phys. Med. Rehabil. 2004, 85, 886–895. [Google Scholar] [CrossRef]
- Lin, P.Y.; Yang, Y.R.; Cheng, S.J.; Wang, R.Y. The relation between ankle impairments and gait velocity and symmetry in people with stroke. Arch. Phys. Med. Rehabil. 2006, 87, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Hyndman, D.; Ashburn, A.; Stack, E. Fall events among people with stroke living in the community: Circumstances of falls and characteristics of fallers. Arch. Phys. Med. Rehabil. 2002, 83, 165–170. [Google Scholar] [CrossRef]
- Karakaya, M.G.; RutbIl, H.; Akpinar, E.; Yildirim, A.; Karakaya, I.Ç. Effect of ankle proprioceptive training on static body balance. J. Phys. Ther. Sci. 2015, 27, 3299–3302. [Google Scholar] [CrossRef]
- Morasso, P.G.; Vittorio, S. Ankle muscle stiffness alone cannot stabilize balance during quiet standing. J. Neurophysiol. 2002, 88, 2157–2162. [Google Scholar] [CrossRef]
- Kaneko, F.; Inada, T.; Matsuda, N.; Shibata, E.; Koyama, S. Acute effect of visually induced kinesthetic illusion in patients with stroke: A preliminary report. Int. J. Neurorehabilit. 2016, 3, 212. [Google Scholar] [CrossRef]
- Kaneko, F.; Shindo, K.; Yoneta, M.; Okawada, M.; Akaboshi, K.; Liu, M.A. A case series clinical trial of a novel approach using augmented reality that inspires self-body cognition in patients with stroke: Effects on motor function and resting-state brain functional connectivity. Front. Syst. Neurosci. 2019, 13, 76. [Google Scholar] [CrossRef]
- Takahashi, R.; Koiwa, M.; Ide, W.; Okawada, M.; Akaboshi, K.; Kaneko, F. Visually induced kinaesthetic illusion combined with therapeutic exercise for patients with chronic stroke: A pilot study. J. Rehabil. Med. 2022, 54, jrm00276. [Google Scholar] [CrossRef]
- Okawada, M.; Inada, T.; Matsuda, N.; Motozawa, S.; Yoneta, M.; Sasaki, S.; Shibata, E.; Kaneko, F. Effects of kinesthetic illusion induced by visual stimulation (KINVIS) therapy on patients with stroke in the subacute phase: A visual analysis based on paralysis severity. Neurocase 2022, 28, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Miyawaki, Y.; Yoneta, M.; Okawada, M.; Kawakami, M.; Liu, M.; Kaneko, F. Model-based analyses for the causal relationship between post-stroke impairments and functional brain connectivity regarding the effects of kinesthetic illusion therapy combined with conventional exercise. Front. Syst. Neurosci. 2022, 15, 804263. [Google Scholar] [CrossRef] [PubMed]
- Sakai, K.; Ikeda, Y.; Amimoto, K. Effect of kinesthetic illusion induced by visual stimulation on ankle dorsiflexion dysfunction in a stroke patient: ABAB single-case design. Neurocase 2018, 24, 245–249. [Google Scholar] [CrossRef]
- Tanabe, J.; Amimoto, K.; Sakai, K.; Osaki, S.; Yoshihiro, N. Effects of kinesthetic illusion induced by visual stimulation on the ankle joint for sit-to-stand in a hemiparesis stroke patient: ABA’ single-case design. J. Phys. Ther. Sci. 2022, 34, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, F.; Yasojima, T.; Kizuka, T. Kinesthetic illusory feeling induced by a finger movement movie effects on corticomotor excitability. Neuroscience 2007, 149, 976–984. [Google Scholar] [CrossRef]
- Aoyama, T.; Kaneko, F.; Hayami, T.; Shibata, E. The effects of kinesthetic illusory sensation induced by a visual stimulus on the corticomotor excitability of the leg muscles. Neurosci. Lett. 2012, 514, 106–109. [Google Scholar] [CrossRef]
- Kaneko, F.; Blanchard, C.; Lebar, N.; Nazarian, B.; Kavounoudias, A.; Romaiguère, P. Brain regions associated to a kinesthetic illusion evoked by watching a video of one’s own moving hand. PLoS ONE 2015, 10, e0131970. [Google Scholar] [CrossRef]
- Okawada, M.; Kaneko, F.; Shindo, K.; Yoneta, M.; Sakai, K.; Okuyama, K.; Akaboshi, K.; Liu, M. Kinesthetic illusion induced by visual stimulation influences sensorimotor event-related desynchronization in stroke patients with severe upper-limb paralysis: A pilot study. Restor. Neurol. Neurosci. 2020, 38, 455–465. [Google Scholar] [CrossRef]
- Sakai, K.; Goto, K.; Tanabe, J.; Amimoto, K.; Kumai, K.; Kamio, H.; Ikeda, Y. Effects of visual-motor illusion on functional connectivity during motor imagery. Exp. Brain. Res. 2021, 239, 2261–2271. [Google Scholar] [CrossRef]
- Shibata, E.; Kaneko, F. Event-related desynchronization possibly discriminates the kinesthetic illusion induced by visual stimulation from movement observation. Exp. Brain. Res. 2019, 237, 3233–3240. [Google Scholar] [CrossRef]
- Sakai, K.; Goto, K.; Watanabe, R.; Tanabe, J.; Amimoto, K.; Kumai, K.; Shibata, K.; Morikawa, K.; Ikeda, Y. Immediate effects of visual-motor illusion on resting-state functional connectivity. Brain. Cogn. 2020, 146, 105632. [Google Scholar] [CrossRef] [PubMed]
- Wakata, S.; Morioka, S. Brain activity and the perception of self-agency while viewing a video of tool manipulation: A functional near-infrared spectroscopy study. NeuroReport 2014, 25, 422–426. [Google Scholar] [CrossRef] [PubMed]
- Peng, T.H.; Zhu, J.D.; Chen, C.C.; Tai, R.Y.; Lee, C.Y.; Hsieh, Y.W. Action observation therapy for improving arm function, walking ability, and daily activity performance after stroke: A systematic review and meta-analysis. Clin. Rehabil. 2019, 33, 1277–1285. [Google Scholar] [CrossRef] [PubMed]
- Sakai, K.; Tanabe, J.; Goto, K.; Kumai, K.; Ikeda, Y. Comparison of functional connectivity during visual-motor illusion, observation, and motor execution. J. Mot. Behav. 2022, 54, 354–362. [Google Scholar] [CrossRef]
- Mizuguchi, N.; Umehara, I.; Nakata, H.; Kanosue, K. Modulation of corticospinal excitability dependent upon imagined force level. Exp. Brain Res. 2013, 230, 243–249. [Google Scholar] [CrossRef]
- Weiss, C.; Tsakiris, M.; Haggard, P.; Schütz-Bosbach, S. Agency in the sensorimotor system and its relation to explicit action awareness. Neuropsychologia 2014, 52, 82–92. [Google Scholar] [CrossRef]
- Minohara, R.; Wen, W.; Hamasaki, S.; Maeda, T.; Kato, M.; Yamakawa, H.; Yamashita, A.; Asama, H. Strength of intentional effort enhances the sense of agency. Front. Psychol. 2016, 7, 1165. [Google Scholar] [CrossRef]
- Kawagoe, T.; Sekiyama, K. Visually encoded working memory is closely associated with mobility in older adults. Exp. Brain Res. 2014, 232, 2035–2043. [Google Scholar] [CrossRef]
- Kawasaki, T.; Aramaki, H.; Tozawa, R.; Kato, M. Immediate beneficial effects of action-observation, and its effects underlying working memory. Phys. Ther. Jpn. 2015, 42, 569–574. [Google Scholar] [CrossRef]
- Sakai, K.; Hosoi, Y. Relationship between the vividness of motor imagery and physical function in patients with subacute hemiplegic stroke: A cross-sectional preliminary study. Brain Inj. 2022, 36, 121–126. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomized trials. BMJ 2010, 152, 726–732. [Google Scholar] [CrossRef]
- Miyara, K.; Matsumoto, S.; Uema, T.; Noma, T.; Ikeda, K.; Ohwatashi, A.; Kiyama, R.; Shimodozono, M. Effect of whole body vibration on spasticity in hemiplegic legs of patients with stroke. Top. Stroke Rehabil. 2018, 25, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Kanai, A.; Kiyama, S.; Goto, H.; Tomita, H.; Tanaka, A.; Kunimi, M.; Okada, T.; Nakai, T. Use of the sit-to-stand task to evaluate motor function of older adults using telemetry. BMC Geriatr. 2016, 16, 121. [Google Scholar] [CrossRef] [PubMed]
- Ota, S.; Goto, H.; Fujita, R.; Haruta, M.; Noda, Y.; Tamakoshi, K. Application of pole walking to day service centers for use by community-dwelling frail elderly people. Int. J. Gerontol. 2014, 8, 6–11. [Google Scholar] [CrossRef]
- Dehail, P.; Bestaven, E.; Muller, F.; Mallet, A.; Robert, B.; Bourdel-Marchasson, I.; Petit, J. Kinematic and electromyographic analysis of rising from a chair during a “Sit-to-Walk” task in elderly subjects: Role of strength. Clin. Biomech. 2007, 22, 1096–1103. [Google Scholar] [CrossRef]
- Lee, T.H.; Choi, J.D.; Lee, N.G. Activation timing patterns of the abdominal and leg muscles during the sit-to-stand movement in individuals with chronic hemiparetic stroke. J. Phys. Ther. Sci. 2015, 27, 3593–3595. [Google Scholar] [CrossRef]
- Sidarus, N.; Vuorre, M.; Metcalfe, J.; Haggard, P. Investigating the prospective sense of agency: Effects of processing fluency, stimulus ambiguity, and response conflict. Front. Psychol. 2017, 8, 545. [Google Scholar] [CrossRef]
- Arbuthnott, K.; Frank, J. Trail making test, part B as a measure of executive control: Validation using a set-switching paradigm. J. Clin. Exp. Neuropsychol. 2000, 22, 518–528. [Google Scholar] [CrossRef]
- Fugl-Meyer, A.R.; Jääskö, L.; Leyman, I.; Olsson, S.; Steglind, S. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand. J. Rehabil. Med. 1975, 7, 13–31. [Google Scholar]
- Chino, N.; Sonoda, S.; Domen, K.; Saitoh, E.; Kimura, A. Stroke Impairment Assessment Set (SIAS). A new evaluation instrument for stroke patients. Jpn. J. Rehabil. Med. 1994, 31, 119–125. [Google Scholar] [CrossRef]
- Poon, D.M.; Hui-Chan, C.W. Hyperactive stretch reflexes, co-contraction, and muscle weakness in children with cerebral palsy. Dev. Med. Child Neurol. 2009, 51, 128–135. [Google Scholar] [CrossRef]
- Cheon, S.; Lee, J.H.; Jun, H.P.; An, Y.W.; Chang, E. Acute effects of open kinetic chain exercise versus those of closed kinetic chain exercise on quadriceps muscle thickness in healthy adults. Int. J. Environ. Res. Public Health 2020, 17, 4669. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 2013. [Google Scholar]
- Lin, K.C.; Hsieh, Y.W.; Wu, C.Y.; Chen, C.L.; Jang, Y.; Liu, J.S. Minimal detectable change and clinically important difference of the Wolf Motor Function Test in stroke patients. Neurorehabilit. Neural Repair 2009, 23, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Norman, G.R.; Sloan, J.A.; Wyrwich, K.W. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Med. Care 2003, 41, 582–592. [Google Scholar] [CrossRef] [PubMed]
- Paravlic, A.H.; Maffulli, N.; Kovač, S.; Pisot, R. Home-based motor imagery intervention improves functional performance following total knee arthroplasty in the short term: A randomized controlled trial. J. Orthop. Surg. Res. 2020, 15, 451. [Google Scholar] [CrossRef] [PubMed]
- Tanabe, J.; Morishita, M. Effects of action observation therapy with limited visual attention on walking ability in stroke patients. J. Mot. Behav. 2022, 54, 27–36. [Google Scholar] [CrossRef]
- Seghezzi, S.; Giannini, G.; Zapparoli, L. Neurofunctional correlates of body-ownership and sense of agency: A meta-analytical account of self-consciousness. Cortex 2019, 121, 169–178. [Google Scholar] [CrossRef]
- Matsumiya, K. Awareness of voluntary action, rather than body ownership, improves motor control. Sci. Rep. 2021, 11, 418. [Google Scholar] [CrossRef]
- Wolpert, D.M.; Goodbody, S.J.; Husain, M. Maintaining internal representations: The role of the human superior parietal lobe. Nat. Neurosci. 1998, 1, 529–533. [Google Scholar] [CrossRef]
- Miyawaki, Y.; Otani, T.; Morioka, S. Dynamic relationship between sense of agency and post-stroke sensorimotor deficits: A longitudinal case study. Brain Sci. 2020, 10, 294. [Google Scholar] [CrossRef]
- Gabbard, C.; Lee, J.; Caçola, P. Role of working memory in transformation of visual and motor representations for use in mental simulation. Cogn. Neurosci. 2013, 4, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Vinti, M.; Couillandre, A.; Hausselle, J.; Bayle, N.; Primerano, A.; Merlo, A.; Hutin, E.; Gracies, J.M. Influence of effort intensity and gastrocnemius stretch on co-contraction and torque production in the healthy and paretic ankle. Clin. Neurophysiol. 2013, 124, 528–535. [Google Scholar] [CrossRef] [PubMed]
- Flansbjer, U.B.; Miller, M.; Downham, D.; Lexell, J. Progressive resistance training after stroke: Effects on muscle strength, muscle tone, gait performance and perceived participation. J. Rehabil. Med. 2008, 40, 42–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Outcomes | Power (1-β) | Effect Size |
|---|---|---|
| P-VMI | ||
| Ankle dorsiflexion angle | 0.99 | 0.96 |
| Ankle dorsiflexion angular velocity | 0.97 | 0.86 |
| S-VMI | ||
| Ankle dorsiflexion angle | 0.84 | 0.67 |
| Ankle dorsiflexion angular velocity | 0.53 | 0.46 |
| Variable | Group A (n = 11) | Group B (n = 11) | p Value |
|---|---|---|---|
| Age (years) | 60.3 (16.5) | 64.5 (8.1) | 0.459 a |
| Gender (male/female) | 8/3 | 5/6 | 0.193 c |
| Time since stroke (days) | 97.1 (28.5) | 90.4 (29.9) | 0.596 a |
| Paralyzed side (right/left) | 6/5 | 4/7 | 0.392 c |
| Lower FMA (points) | 20.3 (3.1) | 21.2 (3.6) | 0.533 a |
| MAS | 2.6 (0.7) | 2.0 (1.1) | 0.217 b |
| MMSE (points) | 27.6 (2.7) | 28.6 (2.2) | 0.353 a |
| P-VMI | S-VMI | |||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| Ankle dorsiflexion angle | 15.7 (7.6) | 18.5 (8.7) * | 14.9 (8.5) | 16.9 (7.9) * |
| Ankle dorsiflexion angular velocity | 32.1 (22.6) | 39.1 (26.7) *† | 30.9 (22.5) | 34.2 (24.1) * |
| Degree of Improvement in Ankle Dorsiflexion Function | Various Variables | Correlation Coefficient | p-Value |
|---|---|---|---|
| P-VMI | |||
| Dorsiflexion angle | Sense of ownership | 0.248 | 0.266 |
| Sense of agency | 0.518 | 0.014 | |
| TMT-B | −0.570 | 0.006 | |
| FMA | 0.124 | 0.266 | |
| SIAS-LE touch | 0.071 | 0.754 | |
| SIAS-LE position | 0.049 | 0.828 | |
| CSS | −0.179 | 0.426 | |
| Dorsiflexion angular velocity | Sense of ownership | 0.019 | 0.857 |
| Sense of agency | 0.449 | 0.036 | |
| TMT-B | −0.449 | 0.036 | |
| FMA | 0.094 | 0.678 | |
| SIAS-LE touch | 0.029 | 0.898 | |
| SIAS-LE position | 0.009 | 0.970 | |
| CSS | −0.430 | 0.047 | |
| S-VMI | |||
| Dorsiflexion angle | Sense of ownership | 0.360 | 0.100 |
| Sense of agency | 0.493 | 0.020 | |
| TMT-B | −0.257 | 0.248 | |
| FMA | 0.066 | 0.950 | |
| SIAS-LE touch | 0.178 | 0.428 | |
| SIAS-LE position | 0.186 | 0.406 | |
| CSS | 0.290 | 0.177 | |
| Dorsiflexion angular velocity | Sense of ownership | 0.387 | 0.076 |
| Sense of agency | 0.366 | 0.093 | |
| TMT-B | −0.351 | 0.109 | |
| FMA | −0.114 | 0.613 | |
| SIAS-LE touch | 0.071 | 0.754 | |
| SIAS-LE position | 0.081 | 0.720 | |
| CSS | 0.119 | 0.590 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanabe, J.; Amimoto, K.; Sakai, K.; Osaki, S.; Yoshihiro, N.; Kataoka, T. Effects and Adaptation of Visual-Motor Illusion Using Different Visual Stimuli on Improving Ankle Joint Paralysis of Stroke Survivors—A Randomized Crossover Controlled Trial. Brain Sci. 2022, 12, 1249. https://doi.org/10.3390/brainsci12091249
Tanabe J, Amimoto K, Sakai K, Osaki S, Yoshihiro N, Kataoka T. Effects and Adaptation of Visual-Motor Illusion Using Different Visual Stimuli on Improving Ankle Joint Paralysis of Stroke Survivors—A Randomized Crossover Controlled Trial. Brain Sciences. 2022; 12(9):1249. https://doi.org/10.3390/brainsci12091249
Chicago/Turabian StyleTanabe, Junpei, Kazu Amimoto, Katsuya Sakai, Shinpei Osaki, Nao Yoshihiro, and Tokuei Kataoka. 2022. "Effects and Adaptation of Visual-Motor Illusion Using Different Visual Stimuli on Improving Ankle Joint Paralysis of Stroke Survivors—A Randomized Crossover Controlled Trial" Brain Sciences 12, no. 9: 1249. https://doi.org/10.3390/brainsci12091249
APA StyleTanabe, J., Amimoto, K., Sakai, K., Osaki, S., Yoshihiro, N., & Kataoka, T. (2022). Effects and Adaptation of Visual-Motor Illusion Using Different Visual Stimuli on Improving Ankle Joint Paralysis of Stroke Survivors—A Randomized Crossover Controlled Trial. Brain Sciences, 12(9), 1249. https://doi.org/10.3390/brainsci12091249






