Simultaneous Presbyopia and Astigmatism Correction with a Novel Trifocal Toric Intraocular Lens—A One-Year Follow-Up
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Pre- and Postoperative Examinations
2.3. The Bi-Flex Liberty 677MTY Intraocular Lens
2.4. Surgical Technique
2.5. Vector Analysis
2.6. Statistical Analysis
3. Results
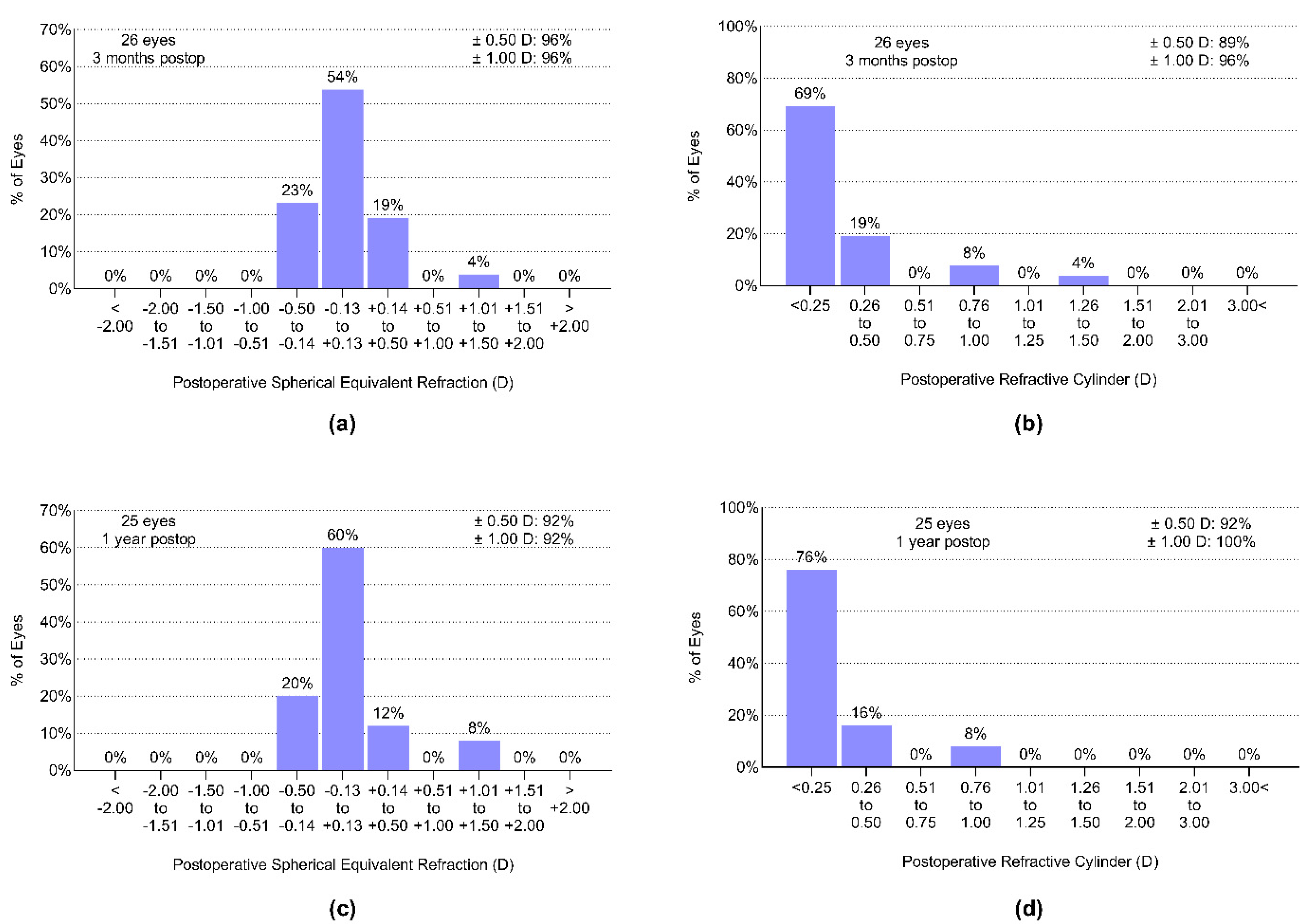
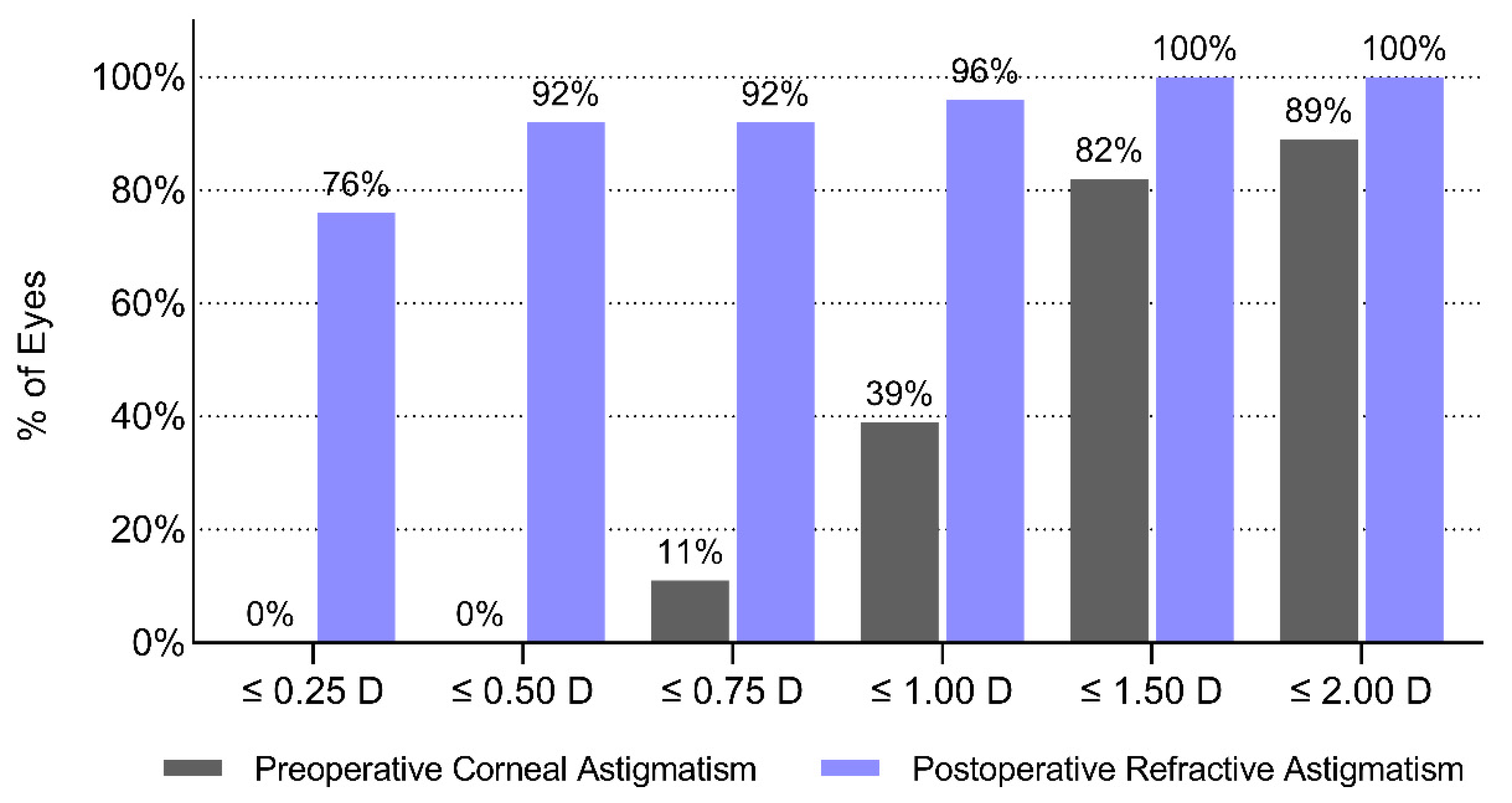
3.1. Refractive Outcomes–Astigmatism—Correction
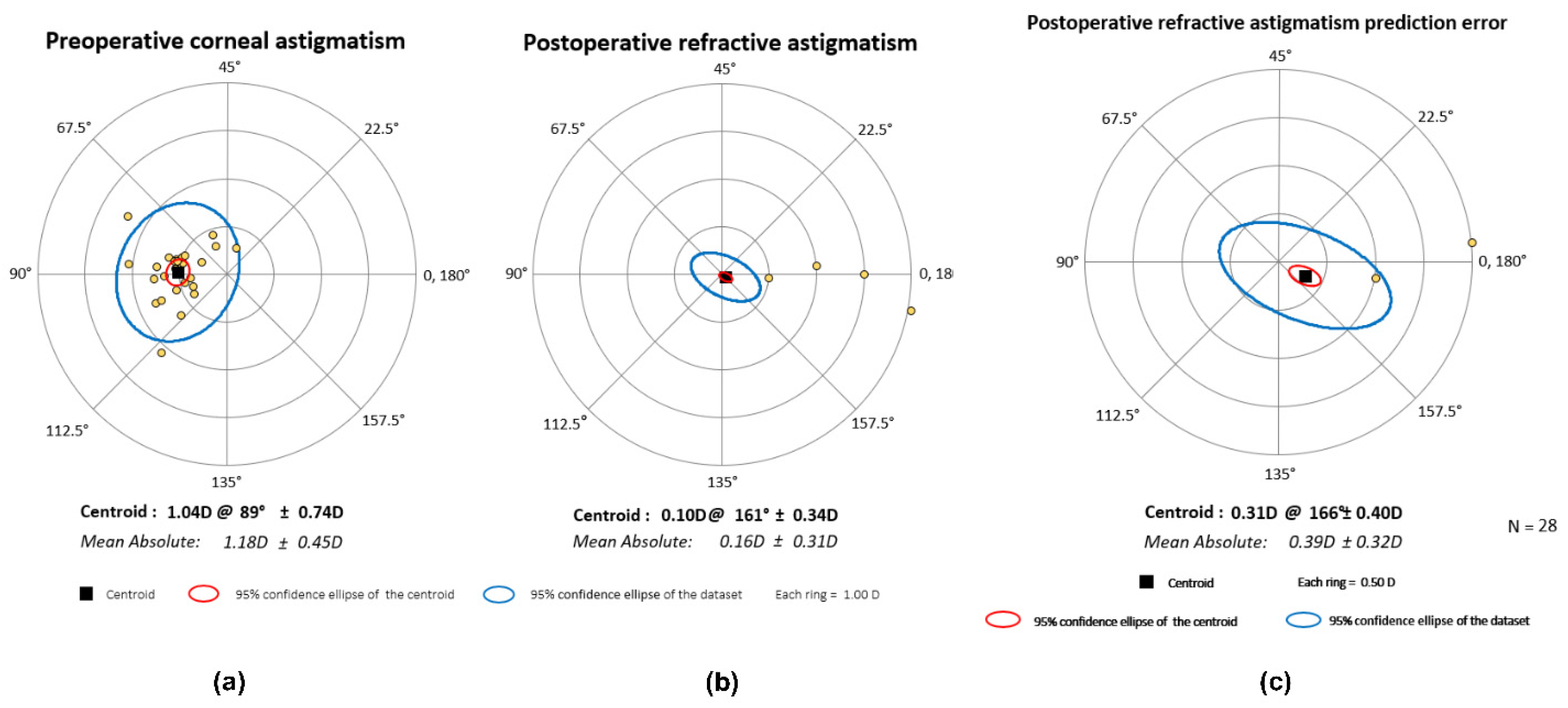
3.2. Vector Analysis
3.3. Rotational Stability of the IOL
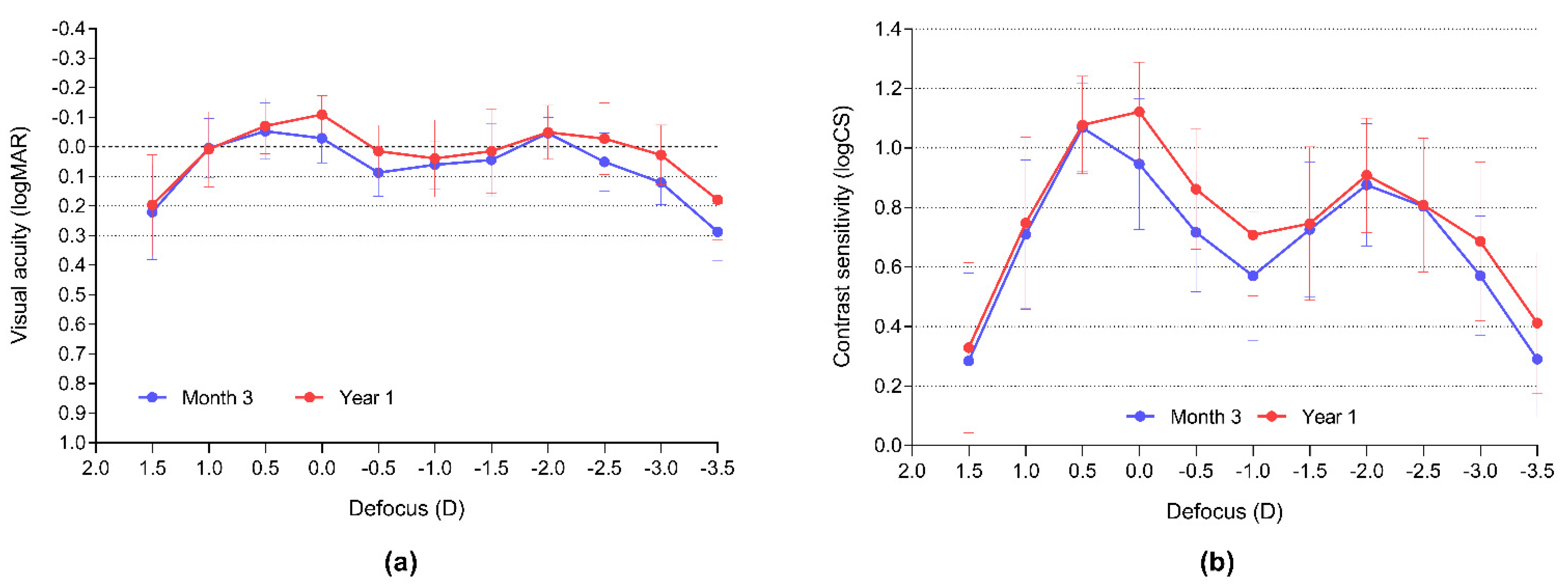
3.4. Visual Outcomes
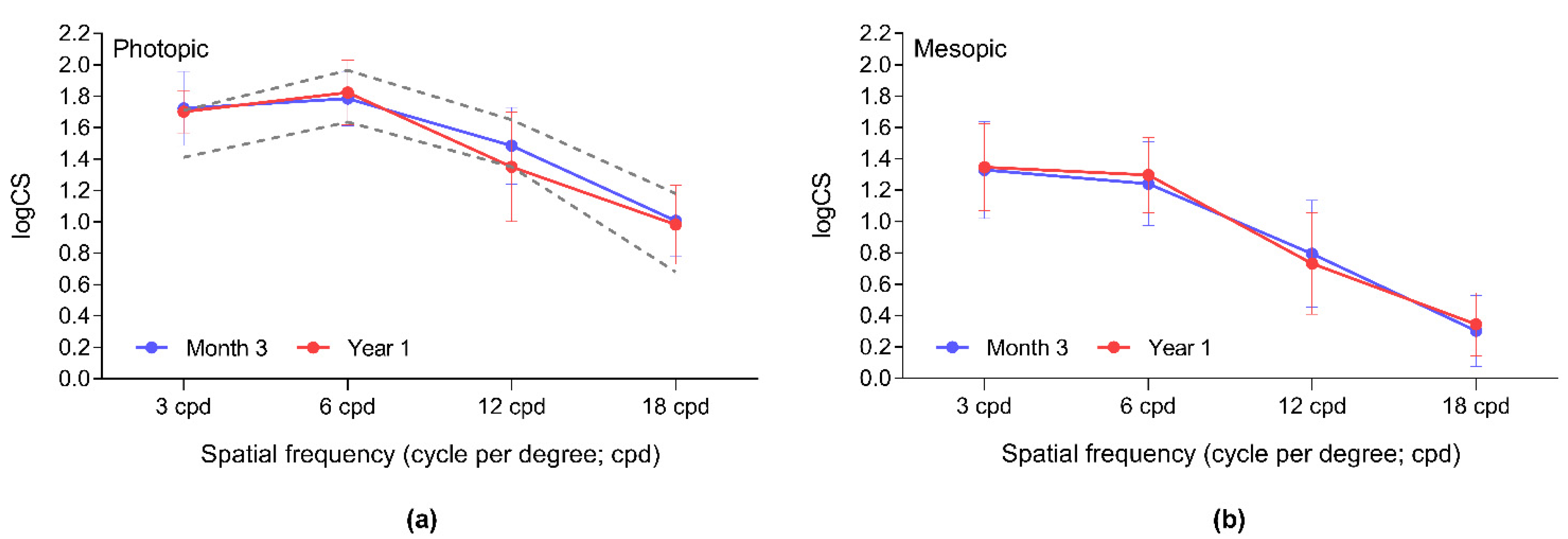
3.5. Visual Quality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Berdahl, J.; Bala, C.; Dhariwal, M.; Lemp-Hull, J.; Thakker, D.; Jawla, S. Patient and economic burden of presbyopia: A systematic literature review. Clin. Ophthalmol. 2020, 14, 3439–3450. [Google Scholar] [CrossRef]
- Carones, F. Residual astigmatism threshold and patient satisfaction with bifocal, trifocal and extended range of vision intraocular lenses (IOLs). Open J. Ophthalmol. 2017, 7, 73363. [Google Scholar] [CrossRef] [Green Version]
- Day, A.C.; Dhariwal, M.; Keith, M.S.; Ender, F.; Vives, C.P.; Miglio, C.; Zou, L.; Anderson, D.F. Distribution of preoperative and postoperative astigmatism in a large population of patients undergoing cataract surgery in the UK. Br. J. Ophthalmol. 2019, 103, 993–1000. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cervantes-Coste, G.; Tapia, A.; Corredor-Ortega, C.; Osorio, M.; Valdez, R.; Massaro, M.; Velasco-Barona, C.; Gonzalez-Salinas, R. The Influence of angle alpha, angle kappa, and optical aberrations on visual outcomes after the Implantation of a high-addition trifocal IOL. J. Clin. Med. 2022, 11, 896. [Google Scholar] [CrossRef]
- Ferrer-Blasco, T.; Montés-Micó, R.; Peixoto-De-Matos, S.C.; González-Méijome, J.M.; Cerviño, A. Prevalence of corneal astigmatism before cataract surgery. J. Cataract Refract. Surg. 2009, 35, 70–75. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- Qvision Almería. Vision C visual Acuity Measurement Application. Available online: https://www.test-eye.com/en/apps-for-eye-care-research/visionc (accessed on 6 September 2019).
- Qvision Almería. Multifocal Lens Analyzer 3.0 Visual Acuity and Contrast Sensitivity Defocus Curve Measurement Application. Available online: https://www.defocuscurve.com/en/ (accessed on 6 September 2019).
- Medicontur Medical Engineering Ltd. Medicontur IOL Optimizer. Available online: https://toriccalculator.net (accessed on 1 September 2019).
- Haigis, W. IOL Calculation According to Haigis, Last Revision: 7 December 1998. Available online: http://www.augenklinik.uniwuerzburg.de/uslab/ioltxt/haie.htm (accessed on 1 September 2019).
- Nováček, L.V.; Němcová, M.; Tyx, K.; Lahodová, K.; Rejmont, L.; Rozsíval, P.; Studený, P. Evaluation of astigmatism-correcting efficiency and rotational stability after cataract surgery with a double-loop haptic toric intraocular lens: A 1-year follow-up. Biomed. Hub. 2021, 6, 30–41. [Google Scholar] [CrossRef]
- Abulafia, A.; Koch, D.D.; Holladay, J.T.; Wang, L.; Hill, W. Pursuing perfection in intraocular lens calculations IV. Rethinking astigmatism analysis for intraocular lens-based surgery: Suggested terminology, analysis, and standards for outcome reports. J. Cataract Refract. Surg. 2017, 44, 1169–1174. [Google Scholar] [CrossRef]
- Nováček, L.V. Simultaneous presbyopia- and astigmatism-correction with a novel trifocal toric intraocular lens—A one-year follow-up. Mendeley Data 2022, 1. [Google Scholar] [CrossRef]
- Reinstein, D.Z.; Archer, T.J.; Srinivasan, S.; Mamalis, N.; Kohnen, T.; Dupps, W.J.; Randleman, J.B. Standard for reporting refractive outcomes of intraocular lens-based refractive surgery. J. Refract. Surg. 2017, 33, 218–222. [Google Scholar] [CrossRef] [Green Version]
- Fernández, J.; Rodríguez-Vallejo, M.; Tauste, A.; Albarrán, C.; Basterra, I.; Piñero, D. Fast measure of visual acuity and contrast sensitivity defocus curves with an iPad application. Open Ophthalmol. J. 2019, 13, 15–22. [Google Scholar] [CrossRef]
- Rodríguez-Vallejo, M.; Remón, L.; Monsoriu, J.A.; Furlan, W.D. Designing a new test for contrast sensitivity function measurement with iPad. J. Optom. 2015, 8, 101–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- VectorVision. Population Values for VectorVision Contrast Sensitivity. Available online: https://vectorvision.com/csv1000-norms/ (accessed on 18 February 2022).
- Bachernegg, A.; Rückl, T.; Strohmaier, C.; Jell, G.; Grabner, G.; Dexl, A.K. Vector analysis, rotational stability, and visual outcome after implantation of a new aspheric toric IOL. J. Refract. Surg. 2015, 31, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Nováček, L.; Němcová, M.; Tyx, K.; Lahodová, K.; Rejmont, L.; Rozsíval, P.; Studený, P. Comparison of clinical outcomes, visual quality and visual function of two presbyopia-correcting intraocular lenses made from the same material, but with different design and optics. J. Clin. Med. 2021, 10, 3268. [Google Scholar] [CrossRef]
- Gundersen, K.G.; Potvin, R. Comparison of visual outcomes after implantation of the diffractive trifocal toric intraocular lens and a diffractive apodized bifocal toric intraocular lens. Clin. Ophthalmol. 2016, 10, 455–461. [Google Scholar] [CrossRef] [Green Version]
- Piovella, M.; Colonval, S.; Kapp, A.; Reiter, J.; Van Cauwenberge, F.; Alfonso, J. Patient outcomes following implantation with a trifocal toric IOL: Twelve-month prospective multicentre study. Eye 2019, 33, 144–153. [Google Scholar] [CrossRef]
- Kretz, F.T.A.; Breyer, D.; Klabe, K.; Hagen, P.; Kaymak, H.; Koss, M.J.; Gerl, M.; Mueller, M.; Gerl, R.H.; Auffarth, G. Clinical outcomes after implantation of a trifocal toric intraocular lens. J. Refract. Surg. 2015, 31, 504–510. [Google Scholar] [CrossRef] [Green Version]
- Vandekerckhove, K. Rotational stability of monofocal and trifocal intraocular toric lenses with identical design and material but different surface treatment. J. Refract. Surg. 2018, 34, 84–91. [Google Scholar] [CrossRef] [Green Version]
- Ribeiro, F.J.; Ferreira, T.B. Comparison of visual and refractive outcomes of 2 trifocal intraocular lenses. J. Cataract Refract. Surg. 2020, 46, 694–699. [Google Scholar] [CrossRef]
- Ninomiya, Y.; Minami, K.; Miyata, K.; Eguchi, S.; Sato, R.; Okamoto, F.; Oshika, T. Toric intraocular lenses in eyes with with-the-rule, against-the-rule, and oblique astigmatism: One-year results. J. Cataract Refract. Surg. 2016, 42, 1431–1440. [Google Scholar] [CrossRef]
- Felipe, A.; Artigas, J.M.; Díez-Ajenjo, A.; García-Domene, C.; Alcocer, P. Residual astigmatism produced by toric intraocular lens rotation. J. Cataract Refract. Surg. 2011, 37, 1895–1901. [Google Scholar] [CrossRef] [PubMed]
- Rementería-Capelo, L.A.; Contreras, I.; García-Pérez, J.L.; Blázquez, V.; Ruiz-Alcocer, J. Visual quality and patient satisfaction with a trifocal intraocular lens and its new toric version. J. Cataract Refract. Surg. 2019, 45, 1584–1590. [Google Scholar] [CrossRef] [PubMed]
- Mojzis, P.; Majerova, K.; Plaza-Puche, A.B.; Hrckova, L.; Alio, J.L. Visual outcomes of a new toric trifocal diffractive intraocular lens. J. Cataract Refract. Surg. 2015, 41, 2695–2706. [Google Scholar] [CrossRef]
- Pomerance, G.; Evans, D. Test-retest reliability of the CSV-1000 contrast test and its relationship to glaucoma therapy. Investig. Ophthalmol. Vis. Sci. 1994, 35, 3357–3361. [Google Scholar]
- García-Bella, J.; Ventura-Abreu, N.; Morales-Fernández, L.; Talavero-González, P.; Carballo-Álvarez, J.; Sanz-Fernández, J.C.; Vázquez-Moliní, J.M.; Martínez-de-la-Casa, J.M. Visual outcomes after progressive apodized diffractive intraocular lens implantation. Eur. J. Ophthalmol. 2018, 28, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Gundersen, K.G.; Potvin, R. Comparing visual acuity, low contrast acuity and contrast sensitivity after trifocal toric and extended depth of focus toric intraocular lens implantation. Clin. Ophthalmol. 2020, 14, 1071–1078. [Google Scholar] [CrossRef] [Green Version]
- Serdiuk, V.; Ustymenko, S.; Fokina, S.; Ivantsov, I. Comparison of three different presbyopia-correcting intraocular lenses. Rom. J. Ophthalmol. 2020, 64, 364–379. [Google Scholar] [CrossRef]
- Győry, J.F.; Srinivasan, S.; Madár, E.; Balla, L. Long-term performance of a diffractive-refractive trifocal IOL with centralized diffractive rings: 5-year prospective clinical trial. J. Cataract Refract. Surg. 2021, 47, 1258–1264. [Google Scholar] [CrossRef]
- Höhn, F.; Tandogan, T.; Breyer, D.R.; Kaymak, H.; Hagen, P.; Klabe, K.; Koss, J.; Gerl, M.; Auffarth, G.U.; Kretz, F.T.A. Funktionelle Ergebnisse 1 Jahr nach Implantation einer bitorischen, trifokalen Intraokularlinse [Functional results one year after implantation of a bitoric, trifocal intraocular lens]. Klin. Mon. Augenheilkd. 2015, 232, 957–961. (In German) [Google Scholar]


| Demographic | Mean ± SD | Range |
|---|---|---|
| Age (y) | 52.4 ± 5.26 | 45–64 |
| Sex (n) | ||
| Female | 9 (60.0%) | |
| Male | 6 (40.0%) | |
| AXL (mm) | 22.66 ± 1.00 | 20.80–24.72 |
| ACD (mm) | 3.04 ± 0.29 | 2.54–3.02 |
| K1 (mm) | 7.91 ± 0.27 | 6.98–8.27 |
| K2 (mm) | 7.69 ± 0.23 | 6.89–8.05 |
| CYL (D) | −0.45 ± 0.69 | −2.75–−0.50 |
| SEQ (D) | 2.78 ± 1.67 | 0.00–6.75 |
| UDVA (logMAR) | 0.54 ± 0.30 | 1.10–0.30 |
| CDVA (logMAR) | 0.01 ± 0.07 | 0.20–−0.10 |
| UNVA (logMAR) | 0.31 ± 0.42 | 0.90–0.20 |
| CNVA (logMAR) | 0.17 ± 0.11 | 0.20–0.00 |
| IOP (mmHg) | 15.1 ± 2.86 | 11.0–20.0 |
| IOL power (D) | 24.6 ± 3.69 | 17.5–33.0 |
| IOL Cylinder (D) | 1.23 ± 0.40 | 1.00–2.50 |
| Follow-Up Visit | Signed | Absolute |
|---|---|---|
| Month 3 | −0.68 ± 2.58 | 2.04 ± 1.67 |
| Month 6 | 0.04 ± 3.03 | 2.27 ± 1.95 |
| Year 1 | −0.35 ± 3.86 | 2.96 ± 2.42 |
| Visual Acuity (logMAR) | Preop | Month 3 | Year 1 | Preop vs. Month 3 p = | Month 3 vs. Year 1 p = |
|---|---|---|---|---|---|
| Monocular | |||||
| UDVA | 0.54 ± 0.30 | 0.02 ± 0.08 | −0.01 ± 0.12 | <0.0001 | 0.0861 |
| CDVA | 0.01 ± 0.07 | −0.02 ± 0.05 | −0.05 ± 0.12 | 0.0898 | 0.4126 |
| UIVA | n.m. | 0.18 ± 0.20 | 0.19 ± 0.16 | n.a. | 0.8438 |
| CIVA | n.m. | 0.02 ± 0.09 | −0.01 ± 0.11 | n.a. | >0.9999 |
| UNVA | 0.31 ± 0.42 | 0.19 ± 0.12 | 0.21 ± 0.13 | 0.0007 | 0.7051 |
| CNVA | 0.17 ± 0.11 | 0.15 ± 0.08 | 0.17 ± 0.10 | 0.4442 | 0.6133 |
| Binocular | |||||
| CDVA | n.m. | −0.05 ± 0.11 | −0.06 ± 0.09 | n.a. | 0.3125 |
| DCIVA | n.m. | 0.05 ± 0.08 | 0.04 ± 0.13 | n.a. | 0.3613 |
| DCNVA | n.m. | 0.11 ± 0.09 | 0.03 ± 0.11 | n.a. | 0.0176 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nováček, L.V.; Němcová, M.; Sičová, K.; Tyx, K.; Rozsíval, P.; Němčanský, J.; Studený, P. Simultaneous Presbyopia and Astigmatism Correction with a Novel Trifocal Toric Intraocular Lens—A One-Year Follow-Up. J. Clin. Med. 2022, 11, 4194. https://doi.org/10.3390/jcm11144194
Nováček LV, Němcová M, Sičová K, Tyx K, Rozsíval P, Němčanský J, Studený P. Simultaneous Presbyopia and Astigmatism Correction with a Novel Trifocal Toric Intraocular Lens—A One-Year Follow-Up. Journal of Clinical Medicine. 2022; 11(14):4194. https://doi.org/10.3390/jcm11144194
Chicago/Turabian StyleNováček, Ladislav Viktor, Marie Němcová, Kristýna Sičová, Kateřina Tyx, Pavel Rozsíval, Jan Němčanský, and Pavel Studený. 2022. "Simultaneous Presbyopia and Astigmatism Correction with a Novel Trifocal Toric Intraocular Lens—A One-Year Follow-Up" Journal of Clinical Medicine 11, no. 14: 4194. https://doi.org/10.3390/jcm11144194





