A Narrative Review of the Roles of Nursing in Addressing Sexual Dysfunction in Oncology Patients
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
- Non-English publications;
- Conference abstracts and commentaries;
- Studies not directly addressing the core topic;
- Duplicate articles.
3. Results
3.1. Prevalence and Impact of Sexual Dysfunction in Cancer Patients
| References | Cancer | Gender | Reported Prevalence | Common Manifestations/Concerns |
|---|---|---|---|---|
| [26,54,55,56] | Breast | F | 16–100% (majority 50–75%) | Sexual difficulty, sexual pain, altered sexual self-image, reduced desire, vaginal dryness, dyspareunia |
| [27,28,56,57] | Gynecologic | F | 30–100% | Vaginal dryness, dyspareunia, loss of sensation, decreased libido, hot flashes, difficulty achieving orgasm, and painful intercourse |
| [56,58] | Rectal (surgery) | F, M | 19–62% (most ~60%) | Sexual dysfunction, body image concerns (stomas), and relationship issues. |
| [41,42,56] | Prostate | M | 40–100% | Erectile dysfunction, loss of desire, problems reaching orgasm |
| [59] | Childhood cancer | F, M | ~1/3 overall, ~½ with 1+ problem, 30% with 2+ problems | Difficulties relaxing/enjoying sex/becoming sexually aroused/achieving orgasm, erection difficulties (men), altered body image, fertility concerns |
| [60,61] | Hematologic (e.g., lymphoma) | F, M | 54% decreased activity, 41% decreased interest | Decreased sexual activity, decreased sexual interest |
| [56] | Lung | F, M | ~50% loss of libido (overall), ~40% decrease in sexual activity in F) | Loss of libido, decrease in sexual activity |
| [56] | Head and neck | F, M | 24–100% negative impact | Negative impact on sexuality |
3.2. Psychological and Social Impact of Sexual Dysfunction
3.2.1. Impact on Partners
3.2.2. Psychological Consequences
3.2.3. Relational Strains
3.2.4. Coping Mechanisms
3.3. Barriers to Addressing Sexual Dysfunction in Cancer Care
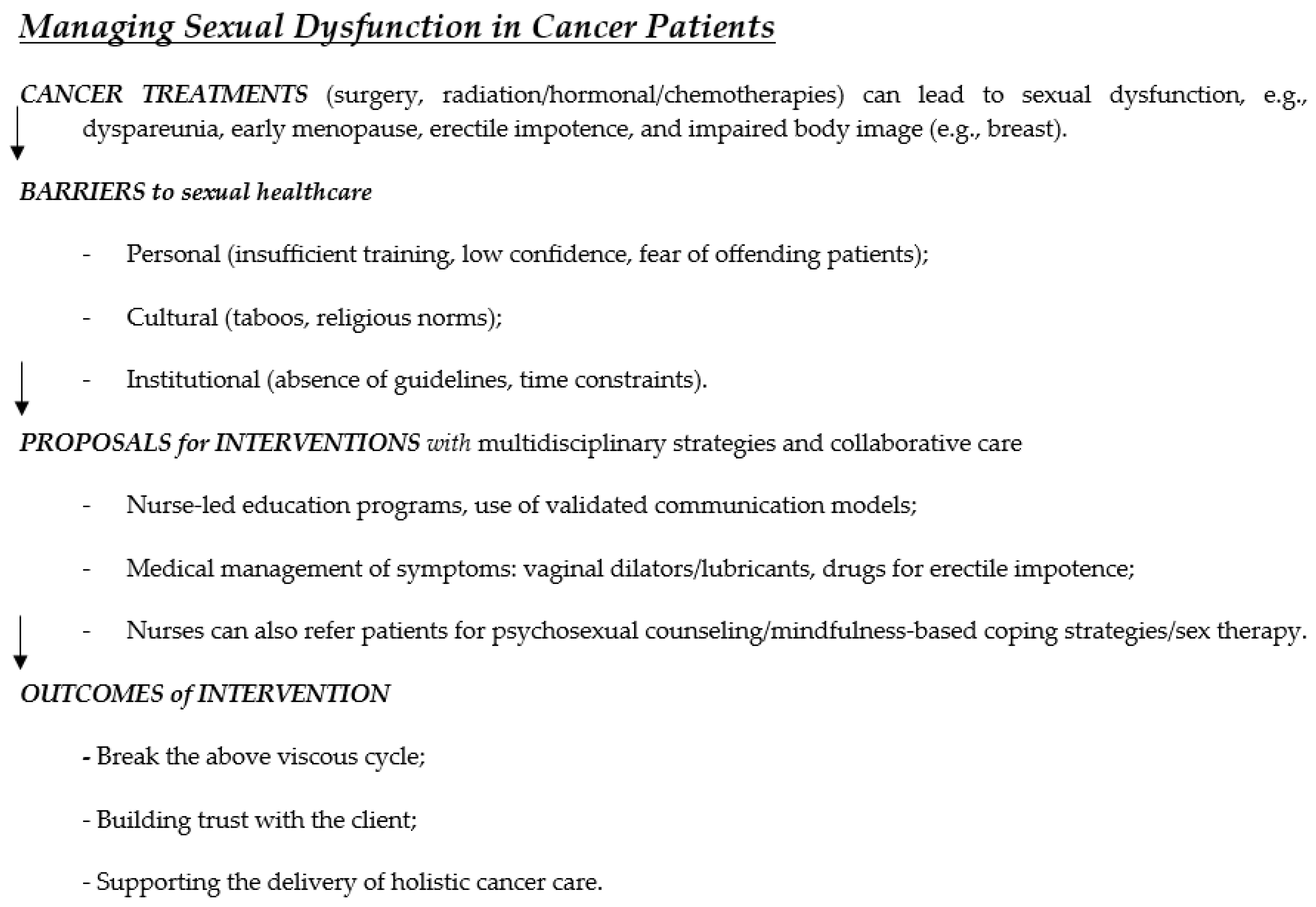
3.4. Interventions for Managing Sexual Dysfunction in Cancer Patients—Training Programs to Build the Trust of Patients and Achieve Holistic Cancer Care
3.5. How to Deal with Attitudes and Beliefs of Nurses About Sexual Health
3.5.1. Personal Beliefs and Knowledge Gaps
3.5.2. Culture and Religious Influences
3.5.3. Experience, Gender, and Communication Challenges
3.5.4. Institutional Roles and Professional Development
3.5.5. Global Effort in Oncology Sexual Health Education in Recent Years
4. Discussion
4.1. Comparisons with the Literature
4.2. Implications for Practice, Policy, and Education
4.3. Strengths and Limitations of the Review
4.4. Recommendations and Future Directions for Research
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| 5 A’s | Ask, Assess, Advise, Assist, Arrange |
| BETTER | B: bringing up the topic. E: Explain that you are concerned with all aspects of patients’ lives. T: Tells patients that sexual dysfunction is common. T: Timing might not be right now, but you are open to future discussion. E: Educate patients about sexual side effects. R: Record the conversation in the medical records |
| CINAHL | Cumulative Index to Nursing and Allied Health Literature |
| ENRICH | Educating Nurses about Reproductive Issues in Cancer Healthcare |
| IMRAD | Introduction, Methods, Results, and Discussion |
| LGBTQ | Lesbian, Gay, Bisexual, Transgender, Queer or Questioning |
| NCCN | National Comprehensive Cancer Network |
| PLISSIT | P: Permission. LI: Limited Information. SS: Specific Suggestions. IT: Intensive Therapy. |
References
- Alqaisi, O.; Maha, S.; Joseph, K.; Yu, E.; Tai, P. Oncology Nurses’ Attitudes, Knowledge, and Practices in Providing Sexuality Care to Cancer Patients: A Scoping Review. Curr. Oncol. 2025, 32, 337. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Evans, D.T. Promoting sexual health and wellbeing: The role of the nurse. Nurs. Stand. 2013, 28, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Cherven, B.O.; Demedis, J.; Frederick, N.N. Sexual health in adolescents and young adults with cancer. J. Clin. Oncol. 2024, 42, 717–724. [Google Scholar] [CrossRef]
- Ussher, J.M.; Perz, J.; Gilbert, E. Australian Cancer and Sexuality Study Team. Perceived causes and consequences of sexual changes after cancer for women and men: A mixed method study. BMC Cancer 2015, 15, 268. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Krouwel, E.M.; Nicolai, M.P.; van Steijn-van Tol, A.Q.; Putter, H.; Osanto, S.; Pelger, R.C.; Elzevier, H. Addressing changed sexual functioning in cancer patients: A cross-sectional survey among Dutch oncology nurses. Eur. J. Oncol. Nurs. 2015, 19, 707–715. [Google Scholar] [CrossRef] [PubMed]
- Alappattu, M.; Harrington, S.E.; Hill, A.; Roscow, A.; Jeffrey, A. Oncology Section EDGE Task Force on Cancer: A systematic review of patient-reported measures for sexual dysfunction. Rehabil. Oncol. 2017, 35, 137–143. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bakker, R.M.; Mens, J.W.; de Groot, H.E.; Tuijnman-Raasveld, C.C.; Braat, C.; Hompus, W.C.; Poelman, J.G.; Laman, M.S.; Velema, L.A.; de Kroon, C.D.; et al. A nurse-led sexual rehabilitation intervention after radiotherapy for gynecological cancer. Support. Care Cancer 2017, 25, 729–737. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barbera, L.; Zwaal, C.; Elterman, D.; McPherson, K.; Wolfman, W.; Katz, A.; Matthew, A.; Interventions to Address Sexual Problems in People with Cancer Guideline Development Group. Interventions to address sexual problems in people with cancer. Curr. Oncol. 2017, 24, 192–200. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Esmat Hosseini, S.; Ilkhani, M.; Rohani, C.; Nikbakht Nasrabadi, A.; Ghanei Gheshlagh, R.; Moini, A. Prevalence of sexual dysfunction in women with cancer: A systematic review and meta-analysis. Int. J. Reprod. Biomed. 2022, 20, 1–12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jing, L.; Zhang, C.; Li, W.; Jin, F.; Wang, A. Incidence and severity of sexual dysfunction among women with breast cancer: A meta-analysis based on female sexual function index. Support. Care Cancer 2019, 27, 1171–1180. [Google Scholar] [CrossRef] [PubMed]
- Proctor, C.J.; Reiman, A.J.; Brunelle, C.; Best, L.A. Intimacy and sexual functioning after cancer: The intersection with psychological flexibility. PLoS Ment. Health 2024, 1, e0000001. [Google Scholar] [CrossRef]
- Cancer Fact Sheets. World Health Organization, 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 30 July 2025).
- World Health Organization (WHO). What Constitutes Sexual Health. Progress in Reproductive Health Research; World Health Organization (WHO): Geneva, Switzerland, 2004; Volume 67, pp. 2–3.
- Cairo Notari, S.; Favez, N.; Notari, L.; Panes-Ruedin, B.; Antonini, T.; Delaloye, J.F. Women’s experiences of sexual functioning in the early weeks of breast cancer treatment. Eur. J. Cancer Care 2018, 27, e12607. [Google Scholar] [CrossRef] [PubMed]
- Fouladi, N.; Pourfarzi, F.; Dolattorkpour, N.; Alimohammadi, S.; Mehrara, E. Sexual life after mastectomy in breast cancer survivors: A qualitative study. Psychooncology 2018, 27, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Gorman, J.R.; Smith, E.; Drizin, J.H.; Lyons, K.S.; Harvey, S.M. Navigating sexual health in cancer survivorship: A dyadic perspective. Support. Care Cancer 2020, 28, 5429–5439. [Google Scholar] [CrossRef] [PubMed]
- Gong, N.; Zhang, Y.; Suo, R.; Dong, W.; Zou, W.; Zhang, M. The role of space in obstructing clinical sexual health education: A qualitative study on breast cancer patients’ perspectives on barriers to expressing sexual concerns. Eur. J. Cancer Care 2021, 30, e13422. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.C.; Hu, W.Y.; Chang, Y.M.; Chiu, S.C. Changes in sexual life experienced by women in Taiwan after receiving treatment for breast cancer. Int. J. Qual. Stud. Health Well-being 2019, 14, 1654343. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Reese, J.B.; Sorice, K.A.; Pollard, W.; Zimmaro, L.A.; Beach, M.C.; Handorf, E.; Lepore, S.J. Understanding sexual help-seeking for women with breast cancer: What distinguishes women who seek help from those who do not? J. Sex. Med. 2020, 17, 1729–1739. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dyer, K.; das Nair, R. Why don’t healthcare professionals talk about sex? A systematic review of recent qualitative studies conducted in the United kingdom. J. Sex. Med. 2013, 10, 2658–2670. [Google Scholar] [CrossRef] [PubMed]
- Canzona, M.R.; Ledford, C.J.W.; Fisher, C.L.; Garcia, D.; Raleigh, M.; Kalish, V.B. Clinician barriers to initiating sexual health conversations with breast cancer survivors: The influence of assumptions and situational constraints. Fam. Syst. Health 2018, 36, 20–28. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, S.R.; Connaghan, J.; Maguire, R.; Kotronoulas, G.; Flannagan, C.; Jain, S.; Brady, N.; McCaughan, E. Healthcare professional perceived barriers and facilitators to discussing sexual wellbeing with patients after diagnosis of chronic illness: A mixed-methods evidence synthesis. Patient Educ. Couns. 2019, 102, 850–863. [Google Scholar] [CrossRef] [PubMed]
- Green, B.N.; Johnson, C.D.; Adams, A. Writing narrative literature reviews for peer-reviewed journals: Secrets of the trade. J. Chiropr. Med. 2006, 5, 101–117. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pimsen, A.; Lin, W.H.; Lin, C.Y.; Kuo, Y.L.; Shu, B.C. Healthcare providers’ experiences in providing sexual health care to breast cancer survivors: A mixed-methods systematic review. J. Clin. Nurs. 2024, 33, 797–816. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, C.; Sime, C.; Rooney, K.; Kotronoulas, G. Sexual health care provision in cancer nursing care: A systematic review on the state of evidence and deriving international competencies chart for cancer nurses. Int. J. Nurs. Stud. 2019, 100, 103405. [Google Scholar] [CrossRef] [PubMed]
- Qi, A.; Li, Y.; Sun, H.; Jiao, H.; Liu, Y.; Chen, Y. Incidence and risk factors of sexual dysfunction in young breast cancer survivors. Ann. Palliat. Med. 2021, 10, 4428–4434. [Google Scholar] [CrossRef] [PubMed]
- Tramacere, F.; Lancellotta, V.; Casà, C.; Fionda, B.; Cornacchione, P.; Mazzarella, C.; de Vincenzo, R.P.; Macchia, G.; Ferioli, M.; Rovirosa, A.; et al. Assessment of sexual dysfunction in cervical cancer patients after different treatment modality: A systematic review. Medicina 2022, 58, 1223. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tee, B.C.; Ahmad Rasidi, M.S.; Mohd Rushdan, M.N.; Ismail, A.; Sidi, H. The prevalence and risk factors of sexual dysfunction in gynecological cancer patients. Med. Health Univ. Kebangs. Malays. 2014, 9, 53–61. [Google Scholar]
- Oldertrøen Solli, K.; de Boer, M.; Nyheim Solbrække, K.; Thoresen, L. Male partners’ experiences of caregiving for women with cervical cancer—A qualitative study. J. Clin. Nurs. 2019, 28, 987–996. [Google Scholar] [CrossRef]
- Paulsen, A.; Vistad, I.; Fegran, L. Nurse-patient sexual health communication in gynecological cancer follow-up: A qualitative study from nurses’ perspectives. J. Adv. Nurs. 2023, 79, 4648–4659. [Google Scholar] [CrossRef] [PubMed]
- Schover, L.R.; van der Kaaij, M.; van Dorst, E.; Creutzberg, C.; Huyghe, E.; Kiserud, C.E. Sexual dysfunction and infertility as late effects of cancer treatment. Eur. J. Cancer Suppl. 2014, 12, 41–53. [Google Scholar] [CrossRef]
- Cagle, J.G.; Bolte, S. Sexuality and life-threatening illness: Implications for social work and palliative care. Health Soc. Work. 2009, 34, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Redelman, M.J. Is there a place for sexuality in the holistic care of patients in the palliative care phase of life? Am. J. Hosp. Palliat. Care. 2008, 25, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Wazqar, D.Y. Sexual health care in cancer patients: A survey of healthcare providers’ knowledge, attitudes and barriers. J. Clin. Nurs. 2020, 29, 4239–4247. [Google Scholar] [CrossRef] [PubMed]
- Kedde, H.; van de Wiel, H.B.; Weijmar Schultz, W.C.; Wijsen, C. Sexual dysfunction in young women with breast cancer. Support. Care Cancer 2013, 21, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Serçekuş Ak, P.; Partlak Günüşen, N.; Göral Türkcü, S.; Özkan, S. Sexuality in Muslim Women with Gynecological Cancer. Cancer Nurs. 2020, 43, E47–E53. [Google Scholar] [CrossRef] [PubMed]
- Mansour, S.E.; Mohamed, H.E. Handling sexuality concerns in women with gynecological cancer: Egyptian nurse’s knowledge and attitudes. J. Educ. Pract. 2015, 6, 146–159. [Google Scholar]
- Åling, M.; Lindgren, A.; Löfall, H.; Okenwa-Emegwa, L. A Scoping Review to Identify Barriers and Enabling Factors for Nurse-Patient Discussions on Sexuality and Sexual Health. Nurs. Rep. 2021, 11, 253–266. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Neenan, C.; Chatzi, A.V. Quality of Nursing Care: Addressing Sexuality as Part of Prostate Cancer Management, an Umbrella Review. J. Adv. Nurs. 2025, 81, 4485–4499. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Forbat, L.; White, I.; Marshall-Lucette, S.; Kelly, D. Discussing the sexual consequences of treatment in radiotherapy and urology consultations with couples affected by prostate cancer. BJU Int. 2012, 109, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Twitchell, D.K.; Wittmann, D.A.; Hotaling, J.M.; Pastuszak, A.W. Psychological Impacts of Male Sexual Dysfunction in Pelvic Cancer Survivorship. Sex. Med. Rev. 2019, 7, 614–626. [Google Scholar] [CrossRef]
- Duran, E.; Tanriseven, M.; Ersoz, N.; Oztas, M.; Ozerhan, I.H.; Kilbas, Z.; Demirbas, S. Urinary and sexual dysfunction rates and risk factors following rectal cancer surgery. Int. J. Color. Dis. 2015, 30, 1547–1555. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.; Lacchetti, C.; Andersen, B.L.; Barton, D.L.; Bolte, S.; Damast, S.; Diefenbach, M.A.; DuHamel, K.; Florendo, J.; Ganz, P.A.; et al. Interventions to Address Sexual Problems in People With Cancer: American Society of Clinical Oncology Clinical Practice Guideline Adaptation of Cancer Care Ontario Guideline. J. Clin. Oncol. 2018, 36, 492–511. [Google Scholar] [CrossRef] [PubMed]
- Jonsdottir, J.I.; Zoëga, S.; Saevarsdottir, T.; Sverrisdottir, A.; Thorsdottir, T.; Einarsson, G.V.; Gunnarsdottir, S.; Fridriksdottir, N. Changes in attitudes, practices and barriers among oncology health care professionals regarding sexual health care: Outcomes from a 2-year educational intervention at a University Hospital. Eur. J. Oncol. Nurs. 2016, 21, 24–30. [Google Scholar] [CrossRef]
- Paterson, C.L.; Lengacher, C.A.; Donovan, K.A.; Kip, K.E.; Tofthagen, C.S. Body image in younger breast cancer survivors: A systematic review. Cancer Nurs. 2016, 39, E39–E58. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Available online: https://www.who.int/news/item/01-02-2024-global-cancer-burden-growing--amidst-mounting-need-for-services (accessed on 30 July 2025).
- Sexual and Reproductive Health: Defining Sexual Health. 2014. Available online: https://www.who.int/teams/sexual-and-reproductive-health-and-research/key-areas-of-work/sexual-health/defining-sexual-health (accessed on 30 July 2025).
- What Constitutes Sexual Health? Progress in Reproductive Health Research 2009. Available online: https://www.who.int/teams/sexual-and-reproductive-health-and-research-(srh)/overview (accessed on 30 July 2025).
- Dai, Y.; Cook, O.Y.; Yeganeh, L.; Huang, C.; Ding, J.; Johnson, C.E. Patient-Reported Barriers and Facilitators to Seeking and Accessing Support in Gynecologic and Breast Cancer Survivors with Sexual Problems: A Systematic Review of Qualitative and Quantitative Studies. J. Sex. Med. 2020, 17, 1326–1358. [Google Scholar] [CrossRef] [PubMed]
- Vizza, R.; Capomolla, E.M.; Tosetto, L.; Corrado, G.; Bruno, V.; Chiofalo, B.; Di Lisa, F.S.; Filomeno, L.; Pizzuti, L.; Krasniqi, E.; et al. Sexual dysfunctions in breast cancer patients: Evidence in context. Sex. Med. Rev. 2023, 11, 179–195. [Google Scholar] [CrossRef] [PubMed]
- Maree, J.; Fitch, M.I. Holding conversations with cancer patients about sexuality: Perspectives from Canadian and African healthcare professionals. Can. Oncol. Nurs. J. 2019, 29, 64. [Google Scholar]
- Kim, J.H.; Yang, Y.; Hwang, E.S. The effectiveness of psychoeducational interventions focused on sexuality in cancer. Cancer Nurs. 2015, 38, E32–E42. [Google Scholar] [CrossRef]
- Chang, C.P.; Wilson, C.M.; Rowe, K.; Snyder, J.; Dodson, M.; Deshmukh, V.; Newman, M.; Fraser, A.; Smith, K.; Date, A.; et al. Sexual dysfunction among gynecologic cancer survivors in a population-based cohort study. Support. Care Cancer 2022, 31, 51. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Valpey, R.; Kucherer, S.; Nguyen, J. Sexual dysfunction in female cancer survivors: A narrative review. Gen. Hosp. Psychiatry 2019, 60, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.C.; Chang, S.R.; Chiu, S.C. Sexual Problems of Patients with Breast Cancer After Treatment: A Systematic Review. Cancer Nurs. 2019, 42, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Candy, B.; Chi, Y.; Graham-Wisener, L.; Jones, L.; King, M.; Lanceley, A.; Vickerstaff, V.; Tookman, A. Interventions for sexual dysfunction following treatments for cancer in women. Cochrane Database Syst. Rev. 2016, 2022, CD005540. [Google Scholar] [CrossRef] [PubMed]
- Del Pup, L.; Nappi, R.E.; Biglia, N. Sexual dysfunction in gynecologic cancer patients. World Cancer Res. J. 2017, 4, e835. [Google Scholar]
- Cihan, E.; Vural, F. Effect of a telephone-based perioperative nurse-led counselling program on unmet needs, quality of life and sexual function in colorectal cancer patients: A non-randomized study. Eur. J. Oncol. Nurs. 2024, 68, 102504. [Google Scholar] [CrossRef]
- Available online: www.cancertherapyadvisor.com (accessed on 6 August 2025).
- Karacan, Y.; Yildiz, H.; Demircioglu, B.; Ali, R. Evaluation of sexual dysfunction in patients with hematological malignancies. Asia-Pac. J. Oncol. Nurs. 2021, 8, 51–57. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Olsson, C.; Sandin-Bojö, A.K.; Bjuresäter, K.; Larsson, M. Changes in sexuality, body image and health related quality of life in patients treated for hematologic malignancies: A longitudinal study. Sex. Disabil. 2016, 34, 367–388. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Quinn, C.; Platania-Phung, C.; Bale, C.; Happell, B.; Hughes, E. Understanding the current sexual health service provision for mental health consumers by nurses in mental health settings: Findings from a survey in Australia and England. Int. J. Ment. Health Nurs. 2018, 27, 1522–1534. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.G. Sexuality and menopause: Unique issues in gynecologic cancer. Semin. Oncol. Nurs. 2019, 35, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Al-Ghabeesh, S.H.; Al-Kalaldah, M.; Rayan, A.; Al-Rifai, A.; Al-Halaiqa, F. Psychological distress and quality of life among Jordanian women diagnosed with breast cancer: The role of trait mindfulness. Eur. J. Cancer Care 2019, 28, e13082. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.C.; Liu, X.; Loke, A.Y. Addressing sexuality issues of women with gynecological cancer: Chinese nurses’ attitudes and practice. J. Adv. Nurs. 2012, 68, 280–292. [Google Scholar] [CrossRef] [PubMed]
- Reese, J.B.; Beach, M.C.; Smith, K.C.; Bantug, E.T.; Casale, K.E.; Porter, L.S.; Bober, S.L.; Tulsky, J.A.; Daly, M.B.; Lepore, S.J. Effective patient-provider communication about sexual concerns in breast cancer: A qualitative study. Support. Care Cancer 2017, 25, 3199–3207. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al-Ghabeesh, S.H.; Bashayreh, I.H.; Saifan, A.R.; Rayan, A.; Alshraifeen, A.A. Barriers to effective pain management in cancer patients from the perspective of patients and family caregivers: A qualitative study. Pain Manag. Nurs. 2020, 21, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Roushar, A. 9th Conference of the Scientific Network of Female Sexual Health and Cancer. Cancersexnetwork.org. 2024. Available online: https://www.cancersexnetwork.org/events/annual-meeting/past-meetings/2024 (accessed on 13 August 2025).
- Eid, K.; Christensen, S.; Hoff, J.; Yadav, K.; Burtson, P.; Kuriakose, M.; Patton, H.; Nyamathi, A. Sexual health education: Knowledge level of oncology nurses and barriers to discussing concerns with patients. Clin. J. Oncol. Nurs. 2020, 24, E50–E56. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.C.; Li, Q.; Wang, N.; Ching, S.S.; Loke, A.Y. Chinese nurses’ attitudes and beliefs toward sexuality care in cancer patients. Cancer Nurs. 2011, 34, E14–E20. [Google Scholar] [CrossRef] [PubMed]
- Oskay, Ü.; Can, G.; Başgöl, S. Discussing sexuality with cancer patients: Oncology nurses attitudes and views. Asian Pac. J. Cancer Prev. 2014, 15, 7321–7326. [Google Scholar] [CrossRef] [PubMed]
- Moore, A.; Higgins, A.; Sharek, D. Barriers and facilitators for oncology nurses discussing sexual issues with men diagnosed with testicular cancer. Eur. J. Oncol. Nurs. 2013, 17, 416–422. [Google Scholar] [CrossRef]
- Available online: https://www.blueberrytherapy.ca/post/breaking-the-silence-addressing-the-stigma-surrounding-women-s-sexual-health-in-healthcare-settings (accessed on 1 August 2025).
- Shahin, M.A.; Gaafar, H.A.A.; Alqersh, D.L.A. Effect of nursing counseling guided by BETTER model on sexuality, marital satisfaction and psychological status among breast cancer women. Egypt. J. Health Care 2021, 12, 75–95. [Google Scholar] [CrossRef]
- Mrad, H.; Chouinard, A.; Pichette, R.; Piché, L.; Bilodeau, K. Feasibility and impact of an online simulation focusing on nursing communication about sexual health in gynecologic oncology. J. Cancer Educ. 2024, 39, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Sousa Rodrigues Guedes, T.; Barbosa Otoni Gonçalves Guedes, M.; de Castro Santana, R.; Costa da Silva, J.F.; Almeida Gomes Dantas, A.; Ochandorena-Acha, M.; Terradas-Monllor, M.; Jerez-Roig, J.; Bezerra de Souza, D.L. Sexual dysfunction in women with cancer: A systematic review of longitudinal studies. Int. J. Environ. Res. Public Health 2022, 19, 11921. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Williams, N.F.; Hauck, Y.L.; Bosco, A.M. Nurses’ perceptions of providing psychosexual care for women experiencing gynecological cancer. Eur. J. Oncol. Nurs. 2017, 30, 35–42. [Google Scholar] [CrossRef] [PubMed]
- David, K.; Davis, M.E. Cancer in sexual and gender minorities: Role of oncology RNs in health equity. Clin. J. Oncol. Nurs. 2024, 28, 329–334. [Google Scholar] [CrossRef]
- Chow, K.M.; Chan, C.W.H.; Choi, K.C.; White, I.D.; Siu, K.Y.; Sin, W.H. A practice model of sexuality nursing care: A concept mapping approach. Support. Care Cancer 2021, 29, 1663–1673. [Google Scholar] [CrossRef] [PubMed]
- Cook, O.; McIntyre, M.; Recoche, K. Exploration of the role of specialist nurses in the care of women with gynecological canc er: A systematic review. J. Clin. Nurs. 2014, 24, 683–695. [Google Scholar] [CrossRef]
- de Vocht, H.; Hordern, A.; Notter, J.; van de Wiel, H. Stepped Skills: A team approach toward communication about sexuality and intimacy in cancer and palliative care. Australas. Med. J. 2011, 4, 610–619. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Suvaal, I.; Hummel, S.B.; Mens, J.M.; Tuijnman-Raasveld, C.C.; Tsonaka, R.; Velema, L.A.; Westerveld, H.; Cnossen, J.S.; Snyers, A.; Jürgenliemk-Schulz, I.M.; et al. Efficacy of a nurse-led sexual rehabilitation intervention for women with gynecological cancers receiving radiotherapy: Results of a randomized trial. Br. J. Cancer 2024, 131, 808–819. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Katz, A. Symptom Management Guidelines for Oncology Nursing; Springer Publishing Company: New York, NY, USA, 2024. [Google Scholar]
- Smith, A. A workshop for educating nurses to address sexual health in patients with breast cancer. Clin. J. Oncol. Nurs. 2015, 19, 248–250. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.who.int/teams/sexual-and-reproductive-health-and-research-%28srh%29/overview (accessed on 30 July 2025).
- Ahn, S.H.; Kim, J.H. Healthcare professionals’ attitudes and practice of sexual health care: Preliminary study for developing training program. Front. Public Health 2020, 8, 559851. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Frederick, N.N.; Campbell, K.; Kenney, L.B.; Moss, K.; Speckhart, A.; Bober, S.L. Barriers and facilitators to sexual and reproductive health communication between pediatric oncology clinicians and adolescent and young adult patients: The clinician perspective. Pediatr. Blood Cancer 2018, 65, e27087. [Google Scholar] [CrossRef] [PubMed]
- Dahouri, A.; Sahebihagh, M.H.; Gilani, N. Factors associated with sexual dysfunction in patients with colorectal cancer in Iran: A cross-sectional study. Sci. Rep. 2024, 14, 4915. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Whitlock, E.P.; Orleans, C.T.; Pender, N.; Allan, J. Evaluating primary care behavioral counseling interventions: An evi dence-based approach. Am. J. Prev. Med. 2002, 22, 267–284. [Google Scholar] [CrossRef] [PubMed]
- Bond, C.B.; Jensen, P.T.; Groenvold, M.; Johnsen, A.T. Prevalence and possible predictors of sexual dysfunction and self-reported needs related to the sexual life of advanced cancer patients. Acta Oncol. 2019, 58, 769–775. [Google Scholar] [CrossRef] [PubMed]
- Correia, R.A.; Bonfim, C.V.D.; Feitosa, K.M.A.; Furtado, B.M.A.S.M.; Ferreira, D.K.D.S.; Santos, S.L.D. Sexual dysfunction after cervical cancer treatment. Rev. Esc. Enferm. USP. 2020, 54, e03636. [Google Scholar] [CrossRef] [PubMed]
| Thematic Area | Summary Point | References |
|---|---|---|
| Prevalence and impact of sexual dysfunction | Sexual dysfunction is highly prevalent (affecting approximately 50–70% of survivors). It has a significant negative impact on quality of life and intimate relationships, yet it often remains underrecognized in oncology practice. Addressing this issue requires integrating sexual health into routine survivorship care. | [18,24,25,26,27,28,29] |
| Psychological and social impact | Untreated sexual dysfunction leads to psychological distress (e.g., anxiety, depression) and social problems such as relationship strain and isolation. A lack of open communication about sexual issues can exacerbate these psychological outcomes, indicating a need for holistic support for patients and partners. | [24,30,31,32,33] |
| Barriers in cancer care | Oncology nurses face multifaceted barriers–personal (insufficient training, low confidence), cultural (taboos, religious norms), and institutional (absence of guidelines, time constraints)– that hinder discussions of sexual health. These barriers contribute to a gap in care, as many patients’ sexual concerns go unaddressed. | [34,35,36,37,38,39,40] |
| Interventions for managing sexual dysfunction | A range of nursing interventions can improve sexual health outcomes: patients’ education and counseling (including models like PLISSIT and BETTER), appropriate use of medications (e.g., PDE5 inhibitors for erectile dysfunction, vaginal moisturizers or estrogen for dyspareunia), and multidisciplinary approaches (involving oncologists, psychologists, and sex therapists). Implementing these interventions—alongside nurse training programs and sexual health clinics—has been shown to increase patients’ satisfaction and sexual functioning. Clinical guidelines now recommend proactive sexual rehabilitation as part of standard cancer care. | [7,24,30,41,42,43] |
| Nurses attitudes and beliefs | Nurses’ attitudes and beliefs can significantly impact sexual healthcare. Many nurses feel uncomfortable or believe sexual matters are too private to discuss, often due to cultural/religious influences or lack of training. Such attitudes can prevent essential conversations, training, and education. Hence, its integration into nursing curricula and professional development, along with supportive institutional polices, is crucial to change perceptions and empower nurses to address sexual dysfunction confidently. | [30,34,35,36,37,44,45] |
| Barrier | Description | References |
|---|---|---|
| Provider discomfort and training deficits | Many healthcare providers lack specific sexual health training and feel anxious or unprepared to discuss intimacy topics. This leads to the avoidance of sexual health conversations to prevent offending patients. | [34,43,68] |
| Cultural and religious norms | In many cultures, sexual topics are taboo. Providers fear violating social norms and may face adverse reactions. Such taboos create strong reluctance for both providers and patients to bring up sexual issues. | [36,37,45,69,70,71] |
| Institutional constraints | Hospital often has no standardized protocol or guidelines for addressing sexual health, and nurses have limited time in busy oncology settings. Lack of institutional support (e.g., training resources, specialized experts) further hinders the integration of sexual health into routine care. | [24,30,38,39,40,66,72] |
| Patient-related factors | Patients themselves frequently feel embarrassed or uncertain about the relevance of sexual health issues and may prefer providers to initiate the topic. Many reports indicate that it is easier to discuss sexual concerns with a same gender provider, and both sides often wait for the other to speak first, resulting in unmet needs. | [24,40,62,65,72] |
| Intervention | Description | References |
|---|---|---|
| Nurse-led education and counseling | Structured sexual health education and counseling sessions (e.g., BETTER Model) help patients understand treatment-related changes and coping strategies. A nurse-led program improves patients’ knowledge about the physical and emotional aspects of sexuality after cancer. | [7,44,74] |
| Pharmacological treatment | Medication can directly address physical dysfunction, e.g., phosphodiesterase-5 inhibitors (sildenafil, tadalafil) improve post-treatment erectile function, and topical estrogen therapies with vaginal moisturizers relieve vaginal atrophy and dyspareunia. Nurses play a key role in informing patients about this treatment and managing side effects. | [41,42,53,66,75] |
| Psycho-Sexual therapy | Individual and couple counseling (psychosexual therapy) addresses the emotional and relational impact of sexual dysfunction. Clinical studies show that such counseling improves sexual satisfaction, reduces anxiety, and enhances partners’ communication. Nurse-led psychosexual support provides emotional assistance along with practical suggestions for intimacy. | [30,31,42,62] |
| Multi-disciplinary team care | Collaborative care involving oncologists, nurses, psychologists, physiotherapists, and sex therapists creates comprehensive treatment plans. Establishing dedicated sexual health clinics within oncology departments has been shown to improve patients’ outcomes and satisfaction. | [24,30,62,73] |
| Digital and Telehealth intervention | Telemedicine platforms, online education modules, and virtual support groups offer accessible sexual health resources. These can overcome geographic and stigma barriers, allowing confidential counseling and education. Studies find digital programs help patients engage with sexual healthcare despite time or cultural constraints. | [44,75,76,77] |
| Nurse training and frameworks | Targeted training programs and communication frameworks (e.g., PLISSIT or stepped-skill models) build nurses’ confidence and skills. Education and systems-based strategies (workshops, protocols) are shown to increase their competence in discussing sexual concerns and conducting more proactive and routine sexual health assessments. | [7,24,30,45,62,74,75,78,79,80] |
| High-Income Countries | Low- and Middle-Income Countries | |
|---|---|---|
| Training and education | Specialized training programs like TrueNTH (Canada) and iSHARE (USA) enhance nurses’ confidence and skills in sexual health communication. | Limited access to formal training; nurses often lack education in sexual health and oncology-specific sexual dysfunction. |
| Clinical guidelines | National guidelines (e.g., ASCO, NCCN) recommend routine screening and referrals for sexual dysfunction. | Guidelines are often absent or not enforced; sexual health is rarely integrated into oncology care plans. |
| Multidisciplinary clinics | Dedicated sexual health clinics exist within cancer centers (e.g., Alberta, Manitoba in Canada). | Few or no specialized clinics; care is fragmented and often deprioritized due to resource constraints. |
| Cultural acceptance | Increasing openness to discussing sexual health; use of structured models like PLISSIT and BETTER. | Cultural taboos and stigma inhibit open discussions; patients and providers may avoid the topic entirely. |
| Patient engagement | Patients are encouraged to voice concerns; nurses initiate conversations during survivorship planning. | Patients rarely disclose sexual concerns due to embarrassment, stigma, or belief that dysfunction is inevitable. |
| Access to resources | Availability of lubricants, dilators, sex therapy referrals, and pelvic floor physiotherapy. | Limited or no access to sexual health resources; interventions are often nonpharmacological due to cost. |
| Technology and innovation | Using online modules, telehealth, and digital tools for training and patient support. | Minimal technology use; infrastructure and internet access may be barriers. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqaisi, O.; Al-Ghabeesh, S.; Tai, P.; Wong, K.; Joseph, K.; Yu, E. A Narrative Review of the Roles of Nursing in Addressing Sexual Dysfunction in Oncology Patients. Curr. Oncol. 2025, 32, 457. https://doi.org/10.3390/curroncol32080457
Alqaisi O, Al-Ghabeesh S, Tai P, Wong K, Joseph K, Yu E. A Narrative Review of the Roles of Nursing in Addressing Sexual Dysfunction in Oncology Patients. Current Oncology. 2025; 32(8):457. https://doi.org/10.3390/curroncol32080457
Chicago/Turabian StyleAlqaisi, Omar, Suhair Al-Ghabeesh, Patricia Tai, Kelvin Wong, Kurian Joseph, and Edward Yu. 2025. "A Narrative Review of the Roles of Nursing in Addressing Sexual Dysfunction in Oncology Patients" Current Oncology 32, no. 8: 457. https://doi.org/10.3390/curroncol32080457
APA StyleAlqaisi, O., Al-Ghabeesh, S., Tai, P., Wong, K., Joseph, K., & Yu, E. (2025). A Narrative Review of the Roles of Nursing in Addressing Sexual Dysfunction in Oncology Patients. Current Oncology, 32(8), 457. https://doi.org/10.3390/curroncol32080457







