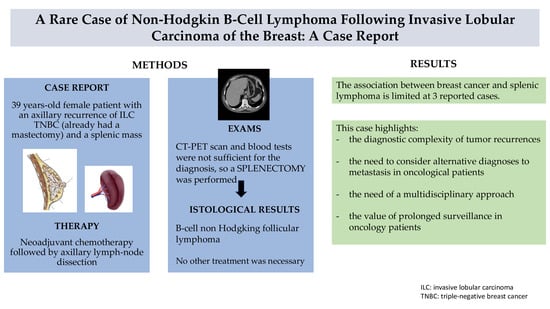
A Rare Case of Non-Hodgkin B-Cell Lymphoma Following Invasive Lobular Carcinoma of the Breast: A Case Report
Abstract
1. Introduction
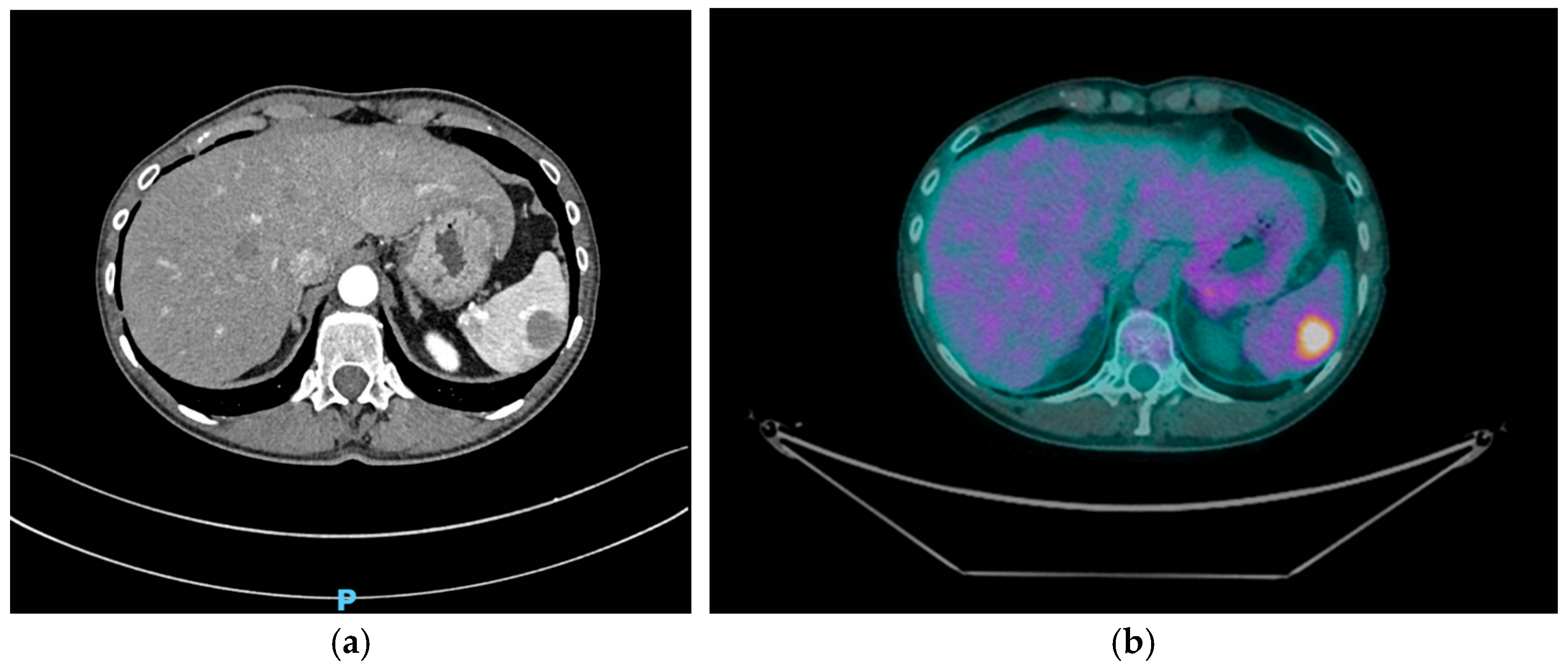
2. Case Presentation
3. Discussion
4. Conclusions
- A clinical follow-up (every 3–6 months for the first 2 years, then annually): comprehensive physical examination and blood tests, including complete blood count (CBC), lactate dehydrogenase (LDH) as a marker of lymphoma activity, tumor markers (CEA, CA 15-3), and liver and renal function tests.
- Imaging surveillance:
- –
- Breast ultrasound and chest and abdominal contrast-enhanced CT scan every 6 months for the first 2 years, then annually.
- –
- PET-CT scan after 6 months after the last one, then every 12 months (particularly if new symptoms or imaging changes arise).
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tari, D.U. Breast Cancer: A Multi-Disciplinary Approach from Imaging to Therapy. Curr. Oncol. 2024, 31, 598–602. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-D.; Chen, S.-C.; Chan, C.H.; Lu, C.-H.; Chen, C.-C.; Lin, J.-T.; Chen, M.-F.; Huang, S.-H.; Yeh, C.-M.; Chen, M.-C. Increased Risk for Second Primary Malignancies in Women with Breast Cancer Diagnosed at Young Age: A Population-Based Study in Taiwan. Cancer Epidemiol. Biomark. Prev. 2008, 17, 2647–2655. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Parhizgar, P.; Bahadori Monfared, A.; Mohseny, M.; Keramatinia, A.; Hashemi Nazari, S.S.; Rahman, S.A.; Al Marzouqi, A.; Al-Yateem, N.; Mosavi Jarrahi, A. Risk of Second Primary Cancer among Breast Cancer Patients: A Systematic Review and Meta-Analysis. Front. Oncol. 2022, 12, 1094136. [Google Scholar] [CrossRef] [PubMed]
- Allen, I.; Hassan, H.; Joko-Fru, W.Y.; Huntley, C.; Loong, L.; Rahman, T.; Torr, B.; Bacon, A.; Knott, C.; Jose, S.; et al. Risks of Second Primary Cancers among 584,965 Female and Male Breast Cancer Survivors in England: A 25-Year Retrospective Cohort Study. Lancet Reg. Health-Eur. 2024, 40, 100903. [Google Scholar] [CrossRef]
- Bazire, L.; De Rycke, Y.; Asselain, B.; Fourquet, A.; Kirova, Y.M. Risks of Second Malignancies after Breast Cancer Treatment: Long-Term Results. Cancer Radiother. 2017, 21, 10–15. [Google Scholar] [CrossRef]
- Supramaniam, R. New Malignancies among Cancer Survivors: SEER Cancer Registries, 1973–2000. J. Epidemiol. Community Health 2008, 62, 375–376. [Google Scholar] [CrossRef]
- Bernstein, J.L.; Lapinski, R.H.; Thakore, S.S.; Doucette, J.T.; Thompson, W.D. The Descriptive Epidemiology of Second Primary Breast Cancer. Epidemiology 2003, 14, 552–558. [Google Scholar] [CrossRef]
- Corso, G.; Veronesi, P.; Santomauro, G.I.; Maisonneuve, P.; Morigi, C.; Peruzzotti, G.; Intra, M.; Sacchini, V.; Galimberti, V. Multiple Primary Non-Breast Tumors in Breast Cancer Survivors. J. Cancer Res. Clin. Oncol. 2018, 144, 979–986. [Google Scholar] [CrossRef]
- Kirova, Y.M.; De Rycke, Y.; Gambotti, L.; Pierga, J.-Y.; Asselain, B.; Fourquet, A. Second Malignancies after Breast Cancer: The Impact of Different Treatment Modalities. Br. J. Cancer 2008, 98, 870–874. [Google Scholar] [CrossRef]
- Mellemkjær, L.; Friis, S.; Olsen, J.H.; Scélo, G.; Hemminki, K.; Tracey, E.; Andersen, A.; Brewster, D.H.; Pukkala, E.; McBride, M.L.; et al. Risk of Second Cancer among Women with Breast Cancer. Intl. J. Cancer 2006, 118, 2285–2292. [Google Scholar] [CrossRef]
- Tamaoki, M.; Nio, Y.; Tsuboi, K.; Nio, M.; Tamaoki, M.; Maruyama, R. A Rare Case of Non-Invasive Ductal Carcinoma of the Breast Coexisting with Follicular Lymphoma: A Case Report with a Review of the Literature. Oncol. Lett. 2014, 7, 1001–1006. [Google Scholar] [CrossRef] [PubMed]
- Salemis, N.S. Synchronous Occurrence of Breast Cancer and Refractory Diffuse Large B-Cell Abdominal Lymphoma: Management and Review of the Literature. Intractable Rare Dis. Res. 2021, 10, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Syamsu, S.A.; Setiady, R.; Smaradania, N.; Prihantono; Irsandy, F.; Faruk, M. Synchronous Breast Cancer and Non-Hodgkin Lymphoma: A Case Report. Int. J. Surg. Case Rep. 2022, 97, 107398. [Google Scholar] [CrossRef] [PubMed]
- Engin, H.; Baltali, E.; Oyan, B.; Göksel, H.; Demirel, B. Breast Cancer and Splenic Non-Hodgkin’s Lymphoma, a Rare Occurrence. Breast J. 2002, 8, 400–401. [Google Scholar] [CrossRef]
- Weide, R.; Görg, C.; Pflüger, K.H.; Ramaswamy, A.; Steinmetz, A.; Falk, S.; Schwerk, W.B. Concomitant Primary Low Grade Non-Hodgkin’s Lymphoma of the Spleen and Breast Carcinoma. Leuk. Lymphoma 1992, 7, 337–339. [Google Scholar] [CrossRef]
- Ueda, Y.; Makino, Y.; Tochigi, T.; Ota, Y.; Hidaka, H.; Nakamura, T.; Beppu, K.; Ohuchida, J.; Odate, S.; Terasaka, S.; et al. A Rare Case of Synchronous Multiple Primary Malignancies of Breast Cancer and Diffuse Large B-Cell Lymphoma That Responded to Multidisciplinary Treatment: A Case Report. Surg. Case Rep. 2022, 8, 99. [Google Scholar] [CrossRef]
- Mirkheshti, N.; Mohebtash, M. A Rare Case of Bilateral Breast Lobular Carcinoma Coexisting with Primary Breast Follicular Lymphoma. J. Community Hosp. Intern. Med. Perspect. 2019, 9, 155–158. [Google Scholar] [CrossRef]
- Khanna, L.; Prasad, S.R.; Yedururi, S.; Parameswaran, A.M.; Marcal, L.P.; Sandrasegaran, K.; Tirumani, S.H.; Menias, C.O.; Katabathina, V.S. Second Malignancies after Radiation Therapy: Update on Pathogenesis and Cross-sectional Imaging Findings. Radiographics 2021, 41, 876–894. [Google Scholar] [CrossRef]
- Hughes, K.S.; Schnaper, L.A.; Bellon, J.R.; Cirrincione, C.T.; Berry, D.A.; McCormick, B.; Muss, H.B.; Smith, B.L.; Hudis, C.A.; Winer, E.P.; et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: Long-term follow-up of CALGB 9343. J. Clin. Oncol. 2013, 31, 2382–2387. [Google Scholar] [CrossRef]
- Kang, D.; Yoon, S.E.; Shin, D.; Lee, J.; Hong, Y.S.; Lee, S.K.; Lee, J.E.; Park, Y.H.; Ahn, J.S.; Guallar, E.; et al. Risk of Non-Hodgkin Lymphoma in Breast Cancer Survivors: A Nationwide Cohort Study. Blood Cancer J. 2021, 11, 200. [Google Scholar] [CrossRef]
- Meattini, I.; De Santis, M.C.; Visani, L.; Scorsetti, M.; Fozza, A.; Meduri, B.; De Rose, F.; Bonzano, E.; Prisco, A.; Masiello, V.; et al. Single-modality endocrine therapy versus radiotherapy after breast-conserving surgery in women aged 70 years and older with luminal A-like early breast cancer (EUROPA): A preplanned interim analysis of a phase 3, non-inferiority, randomised trial. Lancet Oncol. 2025, 26, 37–50. [Google Scholar] [CrossRef]
| Sources | Age | Gender | Histology of BC | Stage | Main Findings | Surgical Treatments | Histology of NHL | Clinical Treatments |
|---|---|---|---|---|---|---|---|---|
| Weide, R., 1992 [15] | 71 | Female | Invasive ductal carcinoma | I | Hypoechogenicspleen lesions | Mastectomy, splenectomy | Low-grade NHL, centroblastic–centrocytic | NR |
| Ueda, Y., 2022 [16] | 71 | Female | Invasive carcinoma ER—PR—HER2 + | NR | Splenic mass and multiple enlarged lymph nodes | Mastectomy, axillary lymph node dissection | Diffuse large B-cell lymphoma (DLBCL) | R-CHOP therapy, radiation therapy, and trastuzumab for NHL. The patient refused chemo and radiation therapy treatment post-mastectomy. |
| Engin, H., 2022 [14] | 66 | Female | Invasive ductal carcinoma | IIA | Splenomegaly after 5 years of remission | Mastectomy, splenectomy | Marginal zone lymphoma | Chemo and radiotherapy for BC. The patient refused other treatments for NHL. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertulla, E.; Diaz, R.; Mascherini, M.; Casaccia, M.; Depaoli, F.; Cuniolo, L.; Cornacchia, C.; Margarino, C.; Murelli, F.; Franchelli, S.; et al. A Rare Case of Non-Hodgkin B-Cell Lymphoma Following Invasive Lobular Carcinoma of the Breast: A Case Report. Curr. Oncol. 2025, 32, 218. https://doi.org/10.3390/curroncol32040218
Bertulla E, Diaz R, Mascherini M, Casaccia M, Depaoli F, Cuniolo L, Cornacchia C, Margarino C, Murelli F, Franchelli S, et al. A Rare Case of Non-Hodgkin B-Cell Lymphoma Following Invasive Lobular Carcinoma of the Breast: A Case Report. Current Oncology. 2025; 32(4):218. https://doi.org/10.3390/curroncol32040218
Chicago/Turabian StyleBertulla, Elisa, Raquel Diaz, Matteo Mascherini, Marco Casaccia, Francesca Depaoli, Letizia Cuniolo, Chiara Cornacchia, Cecilia Margarino, Federica Murelli, Simonetta Franchelli, and et al. 2025. "A Rare Case of Non-Hodgkin B-Cell Lymphoma Following Invasive Lobular Carcinoma of the Breast: A Case Report" Current Oncology 32, no. 4: 218. https://doi.org/10.3390/curroncol32040218
APA StyleBertulla, E., Diaz, R., Mascherini, M., Casaccia, M., Depaoli, F., Cuniolo, L., Cornacchia, C., Margarino, C., Murelli, F., Franchelli, S., Pesce, M., Boccardo, C., Gipponi, M., De Cian, F., & Fregatti, P. (2025). A Rare Case of Non-Hodgkin B-Cell Lymphoma Following Invasive Lobular Carcinoma of the Breast: A Case Report. Current Oncology, 32(4), 218. https://doi.org/10.3390/curroncol32040218