Comparative Efficacy of Photodynamic Therapy and Cold Knife Conization for Cervical High-Grade Squamous Intraepithelial Lesions
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Considerations
2.2. Treatment Procedure
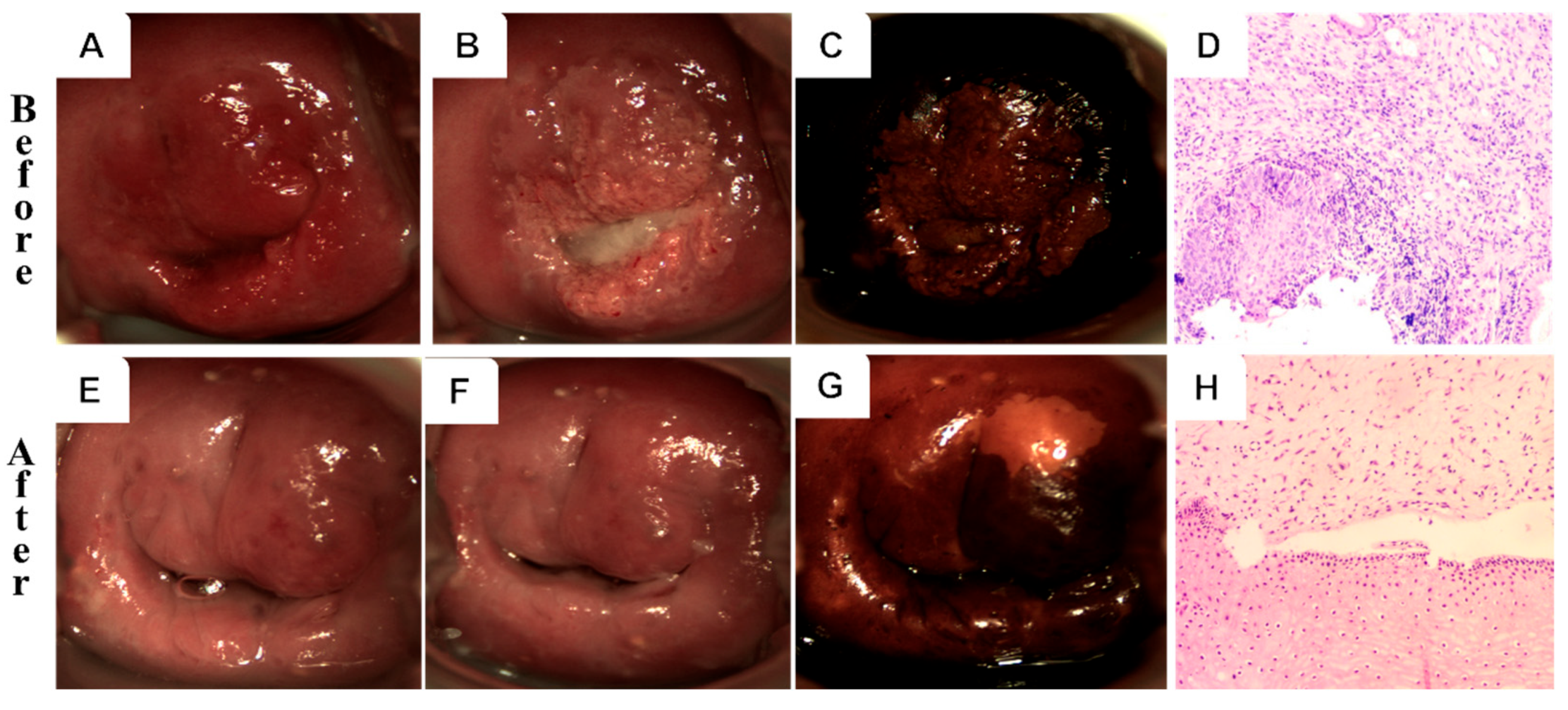
2.2.1. 5-ALA PDT
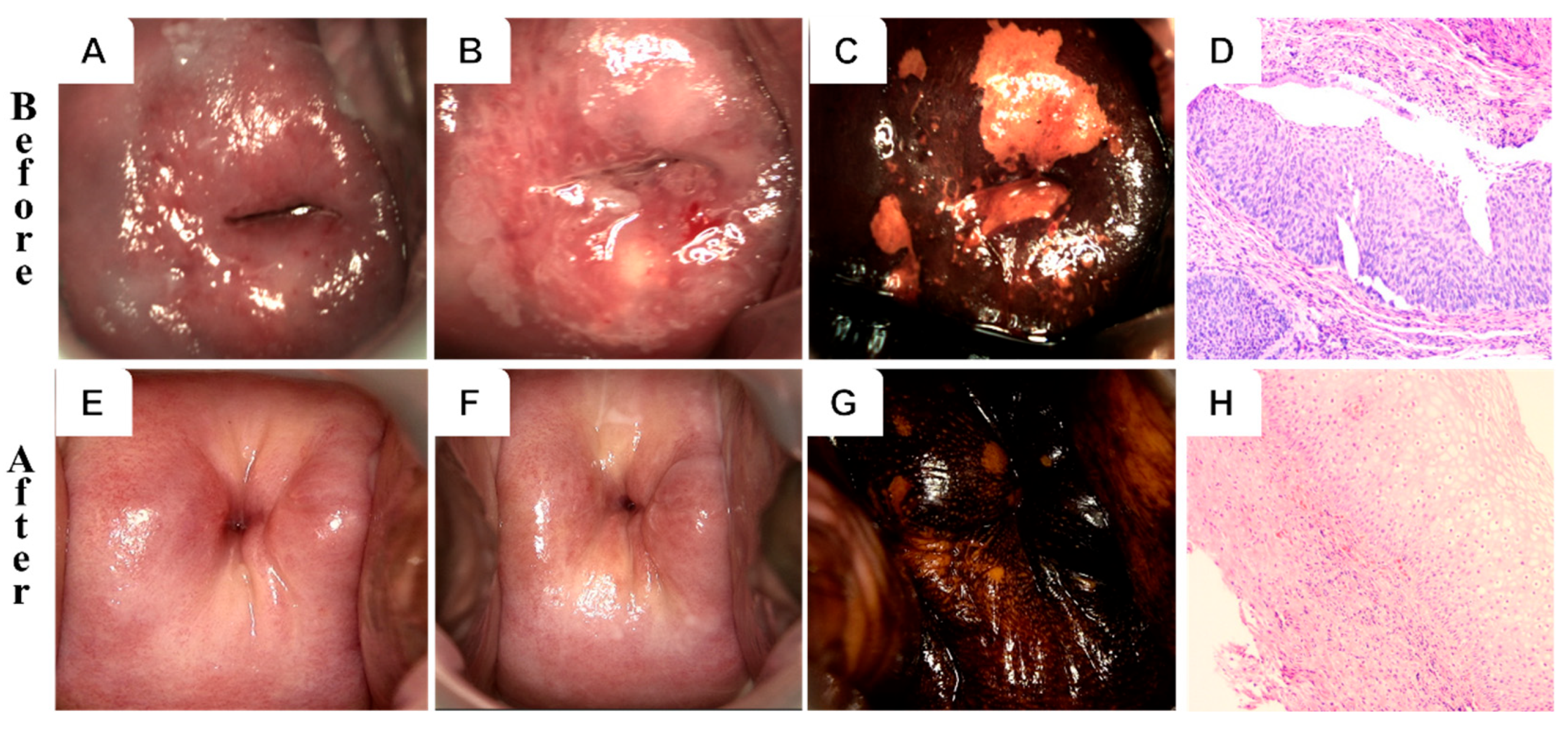
2.2.2. CKC
2.3. Follow-Up and Outcome Assessment
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Comparison of HPV-Negative Rates
3.3. Comparison of the Lesion Effective Rates
3.4. Logistic Regression Analysis of Factors for Lesion Remission and HPV Clearance
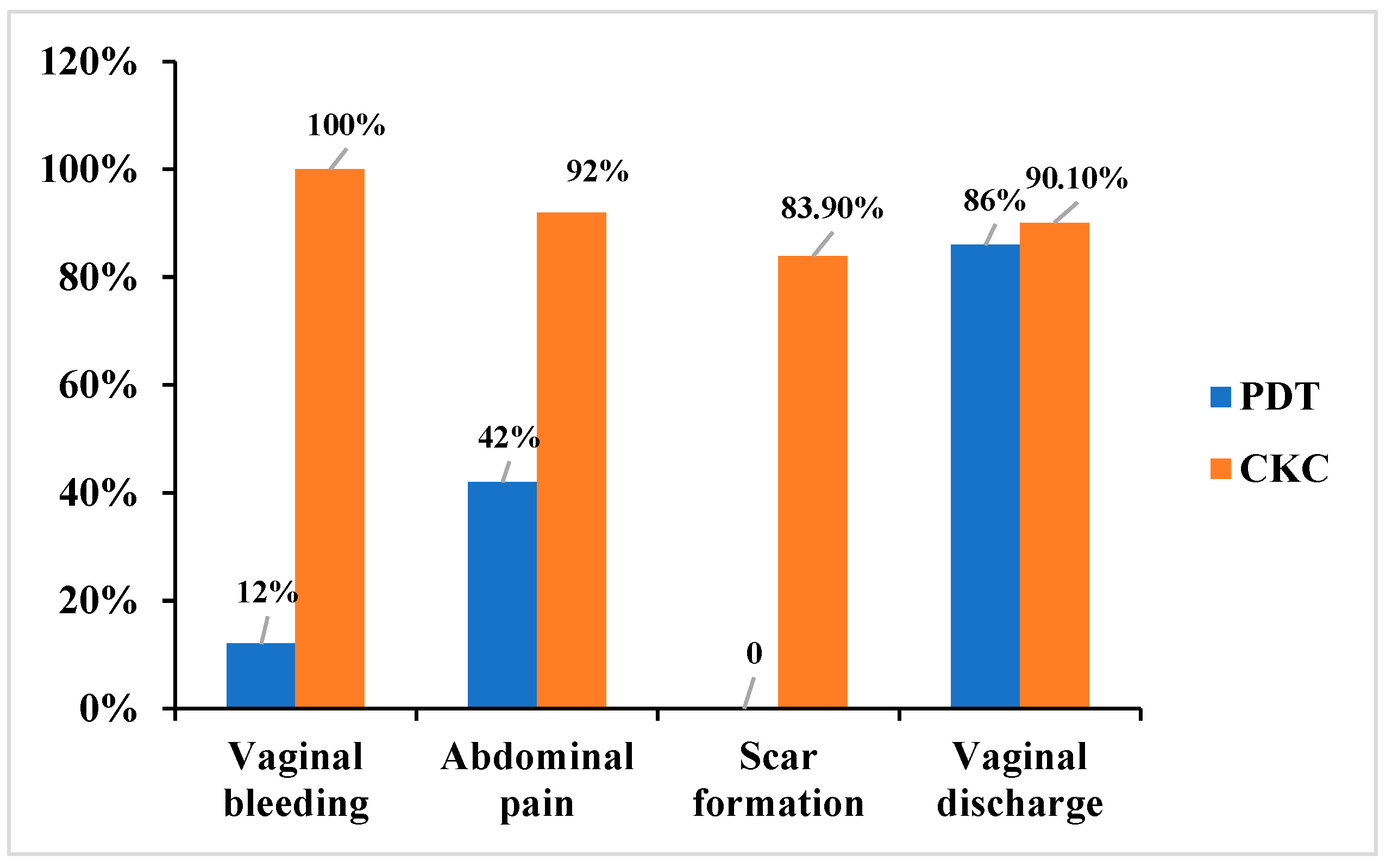
3.5. Comparison of Side Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HPV | human papillomavirus |
| CIN | cervical intraepithelial neoplasia |
| PDT | photodynamic therapy |
| CKC | cervical conization |
| CI | confidence interval |
| OR | odds ratio |
| HSIL | cervical high-grade squamous intraepithelial lesions |
References
- World Health Organization. WHO Guidelines Approved by the Guidelines Review Committee. WHO Guidelines for Treatment of Cervical Intraepithelial Neo-Plasia 2–3 and Adenocarcinoma In Situ: Cryotherapy, Large Loop Excision of the Transformation Zone, and Cold Knife Conization; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Ferrari, F.; Bonetti, E.; Oliveri, G.; Giannini, A.; Gozzini, E.; Conforti, J.; Ferrari, F.A.; Salinaro, F.; Tisi, G.; Ciravolo, G.; et al. Cold Knife Versus Carbon Dioxide for the Treatment of Preinvasive Cervical Lesion. Medicina 2024, 60, 1056. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Zhang, R.; Song, S.; Wang, Y.; Mu, X. Analysis of the clinical characteristics and surgical methods of high-grade squamous intraepithelial lesions of the cervix in postmenopausal women: A retrospective case study. Medicine 2024, 103, e38657. [Google Scholar] [CrossRef]
- Cui, N.; Li, X.; Wen, X.; Xu, J.; Chen, L. Pathological Changes and Pregnancy Outcomes in Cervical Intraepithelial Neoplasia Patients After Cold Knife Conization. Int. J. Gen. Med. 2024, 17, 3641–3648. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Gu, L.; Zhang, Y.; Yang, Q.; Chen, F.; Hong, Z.; Di, W.; Qiu, L. Efficacy of ALA-PDT in treating cervical low-grade squamous intraepithelial lesions with high-risk HPV patients: A multicentre randomized controlled trial. Int. J. Cancer 2025, 157, 908–915. [Google Scholar] [CrossRef]
- de Castro, C.A.; da Silva, C.F.; Silva, F.L.; Marchetti, L.O.; Lombardi, W.; Bagnato, V.S.; Inada, N.M. Evaluating photodynamic therapy protocols for high-grade cervical neoplasia: A comparative study. Photodiagn. Photodyn. Ther. 2025, 53, 104603. [Google Scholar] [CrossRef]
- Bodner, K.; Bodner-Adler, B.; Wierrani, F.; Kubin, A.; Szölts-Szölts, J.; Spängler, B.; Grünberger, W. Cold-knife conization versus photodynamic therapy with topical 5-aminolevulinic acid (5-ALA) in cervical intraepithelial neoplasia (CIN) II with associated human papillomavirus infection: A comparison of preliminary results. Anticancer Res. 2003, 23, 1785–1788. [Google Scholar] [PubMed]
- Kapp, P.; Schmucker, C.; Siemens, W.; Brugger, T.; Gorenflo, L.; Röbl-Mathieu, M.; Grummich, K.; Thörel, E.; Askar, M.; Brotons, M.; et al. Human papillomavirus (HPV) vaccination in women with conisation. Cochrane Database Syst. Rev. 2025, 9, Cd016121. [Google Scholar] [CrossRef]
- Fu, K.; Yangzom, K.; Li, L.; Wu, L.; Zhang, Y. Optimizing the Follow-Up Interval After Successful Cold Knife Conization of CIN3: A 10-Year Retrospective Cohort Study. Cancer Med. 2025, 14, e70825. [Google Scholar] [CrossRef]
- McCluggage, W.G.; Singh, N.; Gilks, C.B. Key changes to the World Health Organization (WHO) classification of female genital tumours introduced in the 5th edition (2020). Histopathology 2022, 80, 762–778. [Google Scholar] [CrossRef]
- Wang, X.; Qiu, H.; Zhan, H.; Huang, Z. Photodynamic therapy of vaginal intraepithelial neoplasia-How to do it? Photodiagn. Photodyn. Ther. 2024, 45, 103997. [Google Scholar] [CrossRef]
- Cai, H.; Che, Y.; Chen, Y.; Sun, H.; Ma, T.; Wang, Y. Long-term follow-up of photodynamic therapy of cervical intraepithelial neoplasia grade 2 (CIN2). Photodiagn. Photodyn. Ther. 2024, 47, 104219. [Google Scholar] [CrossRef]
- López-Cárdenas, M.T.; Jiménez, A.; Espinosa-Montesinos, A.; Maldonado-Alvarado, E.; Osorio-Peralta, M.O.; Martinez-Escobar, A.; Moreno-Vázquez, A.; Aguilera-Arreola, M.G.; Ramón-Gallegos, E. Elimination of Human Papillomavirus and Cervical Pathological Microbiota with Photodynamic Therapy in Women from Mexico City with Cervical Intraepithelial Neoplasia I. Photochem. Photobiol. 2023, 99, 1468–1475. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; You, L.; Zhang, W.; Ma, Y.; Tang, Y.; Xu, W. Evaluation of 5-aminolevulinic acid-mediated photodynamic therapy on cervical low-grade squamous intraepithelial lesions with high-risk HPV infection. Photodiagn. Photodyn. Ther. 2022, 38, 102807. [Google Scholar] [CrossRef]
- Qiu, L.; Li, J.; Chen, F.; Wang, Y.; Wang, Y.; Wang, X.; Lv, Q.; Li, C.; Li, M.; Yang, Q.; et al. Chinese expert consensus on the clinical applications of aminolevulinic acid-based photodynamic therapy in female lower genital tract diseases (2022). Photodiagn. Photodyn. Ther. 2022, 39, 102993. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Xu, X.; Ma, Y.; Tang, Y.; Huang, Z. Comparative Study of 5-Aminolevulinic Acid-Mediated Photodynamic Therapy and the Loop Electrosurgical Excision Procedure for the Treatment of Cervical High-Grade Squamous Intraepithelial Lesions. Pharmaceutics 2024, 16, 686. [Google Scholar] [CrossRef]
- Tang, Y.; Su, Y.; Xu, Y.; Zhang, Y.; Shen, Y.; Qin, L.; Zhang, L.; Cao, L.; Zhou, Y.; Zhang, T.; et al. Therapeutic effects of topical photodynamic therapy with 5-aminolevulinic acid on cervical high-grade squamous intraepithelial lesions. Photodiagn. Photodyn. Ther. 2022, 39, 102884. [Google Scholar] [CrossRef]
- Ma, L.; Gao, X.; Geng, L.; You, K.; Wu, Z.; Li, Y.; Han, Q.; Wang, Y.; Guo, H. Efficacy and safety of photodynamic therapy mediated by 5-aminolevulinic acid for the treatment of cervical intraepithelial neoplasia 2: A single-center, prospective, cohort study. Photodiagn. Photodyn. Ther. 2021, 36, 102472. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Liu, X.; Zhang, J.; Song, M.; Liu, H.; Xu, Y.; Meng, L.; Zhang, Y.; Jia, L. Comparison of 5-ALA-PDT and LEEP of cervical squamous intraepithelial neoplasia (CIN2) with high-risk human papillomavirus infection in childbearing age women: A non-randomized controlled polit study. Photodiagn. Photodyn. Ther. 2024, 46, 104044. [Google Scholar] [CrossRef]
- Zhang, T.; Zhang, Y.; Tang, Y.; Qin, L.; Shen, Y.; Wang, B.; Zhang, L.; Cao, L.; Zhou, Y.; Su, Y.; et al. The effect of high-risk HPV E6/E7 mRNA on the efficacy of topical photodynamic therapy with 5-aminolevulinic acid for cervical high-grade squamous intraepithelial lesions. Photodiagn. Photodyn. Ther. 2022, 39, 102974. [Google Scholar] [CrossRef]
- Ferrari, F.A.; Magni, F.; Bosco, M.; Biancotto, G.; Zorzato, P.C.; Laganà, A.S.; Chiantera, V.; Raffaelli, R.; Franchi, M.; Uccella, S.; et al. The Role of Micronutrients in Human Papillomavirus Infection, Cervical Dysplasia, and Neoplasm. Healthcare 2023, 11, 1652. [Google Scholar] [CrossRef]
- Cai, L.; Huang, Y.; Lin, C.; Liu, G.; Mao, X.; Dong, B.; Lu, T.; Sun, P. A comparison study of post-operative infection analysis of cold-knife conization and loop electrosurgical excision procedure for cervical high-grade squamous intraepithelial lesion. Transl. Cancer Res. 2020, 9, 949–957. [Google Scholar] [CrossRef] [PubMed]
- Bittencourt, D.D.; Zanine, R.M.; Sebastião, A.P.M.; Ribas, C.M. Risk Factors for Persistence or Recurrence of High-Grade Cervical Squamous Intraepithelial Lesions. Rev. Col. Bras. Cir. 2023, 50, e20233537. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Yuan, S.; Su, Y.; Zhang, C.; Zhou, M.; Zhang, M.; Dai, K.; Wang, Y.; Cao, L.; Zhang, T.; et al. Comparative study of topical 5-aminolevulinic acid photodynamic therapy and surgery for recurrent cervical high-grade squamous intraepithelial lesions following surgery. Photodiagn. Photodyn. Ther. 2024, 46, 103974. [Google Scholar] [CrossRef] [PubMed]

| Clinical Characteristics | PDT (N = 50) | CKC (N = 87) | p Value |
|---|---|---|---|
| Age | 0.08 | ||
| <40 | 41 | 58 | |
| 20–29 | 24 | 20 | |
| 30–39 | 17 | 38 | |
| ≥40 | 9 | 29 | |
| Median (range) | 30.9 (25–48) | 36.0 (24–65) | |
| HPV genotype | 0.45 | ||
| 16/18 | 30 | 45 | |
| Non-16/18 | 20 | 42 | |
| Single | 25 | 43 | 1 |
| Multiple | 25 | 44 | |
| TCT | 0.34 | ||
| NILM | 16 | 20 | |
| ASC-US | 15 | 28 | |
| LSIL | 15 | 20 | |
| HSIL | 4 | 19 | |
| Transformation Zone | 0.81 | ||
| TZ I | 30 | 49 | |
| TZ II | 18 | 30 | |
| TZ III | 2 | 8 | |
| Lesion characteristics | 0.10 | ||
| CIN II | 44 | 65 | |
| CIN III | 6 | 22 |
| HPV | The 6th Month (95%CI) | ||
|---|---|---|---|
| PDT | CKC | p Value | |
| Negative rates | 80.0% (66.3–90.0%) | 82.7% (73.2–90.0%) | 0.86 |
| HPV genotype | |||
| HPV16/18 | 80.0% (61.4–92.3%) | 82.2% (67.9–92.0%) | 1 |
| non-HPV16/18 | 80.0% (56.3–94.3%) | 83.3% (68.6–93.0%) | 1 |
| Lesion severity | |||
| CIN II | 84.1% (69.9–93.4%) | 84.6% (73.5–92.3%) | 1 |
| CIN III | 50.0% (11.8–88.2%) | 77.3% (54.6–92.2%) | 0.42 |
| Positive | |||
| Partial-negative | 12.0% (4.5–24.3%) | 9.2% (4.1–17.3%) | 0.82 |
| Persistence | 8.0% (2.2–19.2%) | 8.1% (3.2–15.9%) | 1 |
| Lesion | The 6th Month | (95%CI) | |
|---|---|---|---|
| PDT | CKC | p Value | |
| Effective rates | 88.0% (75.7–95.5%) | 89.6% (81.3–95.2%) | 0.99 |
| Cure | 84.0% (70.9–92.8%) | 85.1% (75.8–91.8%) | 1 |
| Remission | 6.0% (1.3–16.5%) | 4.6% (1.3–11.4%) | 1 |
| HPV genotype | |||
| HPV16/18 | 90.0% (73.5–97.9%) | 91.1% (78.8–97.5%) | 1 |
| non-HPV16/18 | 85.0% (62.1–96.8%) | 88.1% (74.4–96.0%) | 1 |
| Lesion severity | |||
| CIN II | 86.4% (72.6–94.8%) | 89.2% (79.1–95.6%) | 0.88 |
| CINIII | 100.0% (54.1–100%) | 90.9% (70.8–98.9%) | 1 |
| Ineffective | |||
| Persistence | 12.0% (4.5–24.3%) | 10.3% (4.8–18.7%) | 0.99 |
| Progression | 0 (0.0%) | 0 (0.0%) |
| The 6th Month | ||||||||
|---|---|---|---|---|---|---|---|---|
| Clinical Characteristics | PDT | CKC | ||||||
| Lesion Remission | HPV Clearance | Lesion Remission | HPV Clearance | |||||
| OR (95%CI) | p | OR (95%CI) | p | OR (95%CI) | p | OR (95%CI) | p | |
| Age | 0.89 (0.66–1.12) | 0.38 | 0.95 (0.75–1.18) | 0.65 | 0.98 (0.85–1.14) | 0.81 | 0.95 (0.86–1.00) | 0.43 |
| non-HPV16/18 | 0.69 (0.06–6.42) | 1.31 (0.23–7.26) | 0.74 | 1.21 (0.21–7.65) | 0.83 | 1.05 (0.27–4.24) | 0.94 | |
| Multiple HPV | 0.08 (0.04–0.72) | 0.045 * | 0.12 (0.02–0.67) | 0.026 * | 0.42 (0.08–1.83) | 0.27 | 0.30 (0.08–1.01) | 0.06 |
| Abnormal cytology | 4.77 — | 0.99 | 0.19 (0.02–1.26) | 0.14 | 0.53 (0.06–2.86) | 0.50 | 0.79 (0.17–3.02) | 0.73 |
| Transformation Zone | 9.05 — | 0.35 | 7.89 (0.42–9.36) | 0.16 | 0.47 (0.40–4.8) | 0.53 | 1.45 (0.24–8.55) | 0.68 |
| Lesion characteristics (CINIII) | — | 0.99 | 0.09 (0.01–0.99) | 0.07 | 0.34 (0.41–3.74) | 0.36 | 0.26 (0.04–1.49) | 0.14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, X.; Chen, Y.; Huang, J.; He, Q.; Zhou, J. Comparative Efficacy of Photodynamic Therapy and Cold Knife Conization for Cervical High-Grade Squamous Intraepithelial Lesions. Curr. Oncol. 2025, 32, 590. https://doi.org/10.3390/curroncol32110590
Wang X, Chen Y, Huang J, He Q, Zhou J. Comparative Efficacy of Photodynamic Therapy and Cold Knife Conization for Cervical High-Grade Squamous Intraepithelial Lesions. Current Oncology. 2025; 32(11):590. https://doi.org/10.3390/curroncol32110590
Chicago/Turabian StyleWang, Xiaoyun, Yiquan Chen, Jianxia Huang, Qiong He, and Jianwei Zhou. 2025. "Comparative Efficacy of Photodynamic Therapy and Cold Knife Conization for Cervical High-Grade Squamous Intraepithelial Lesions" Current Oncology 32, no. 11: 590. https://doi.org/10.3390/curroncol32110590
APA StyleWang, X., Chen, Y., Huang, J., He, Q., & Zhou, J. (2025). Comparative Efficacy of Photodynamic Therapy and Cold Knife Conization for Cervical High-Grade Squamous Intraepithelial Lesions. Current Oncology, 32(11), 590. https://doi.org/10.3390/curroncol32110590





