Regional and Temporal Variation in Receipt of Gabapentinoid and SSRI/SNRI Therapy Among Older Cancer Survivors in the United States
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Cohort
2.3. Outcome Variables
2.4. Covariates
2.5. Statistical Analysis
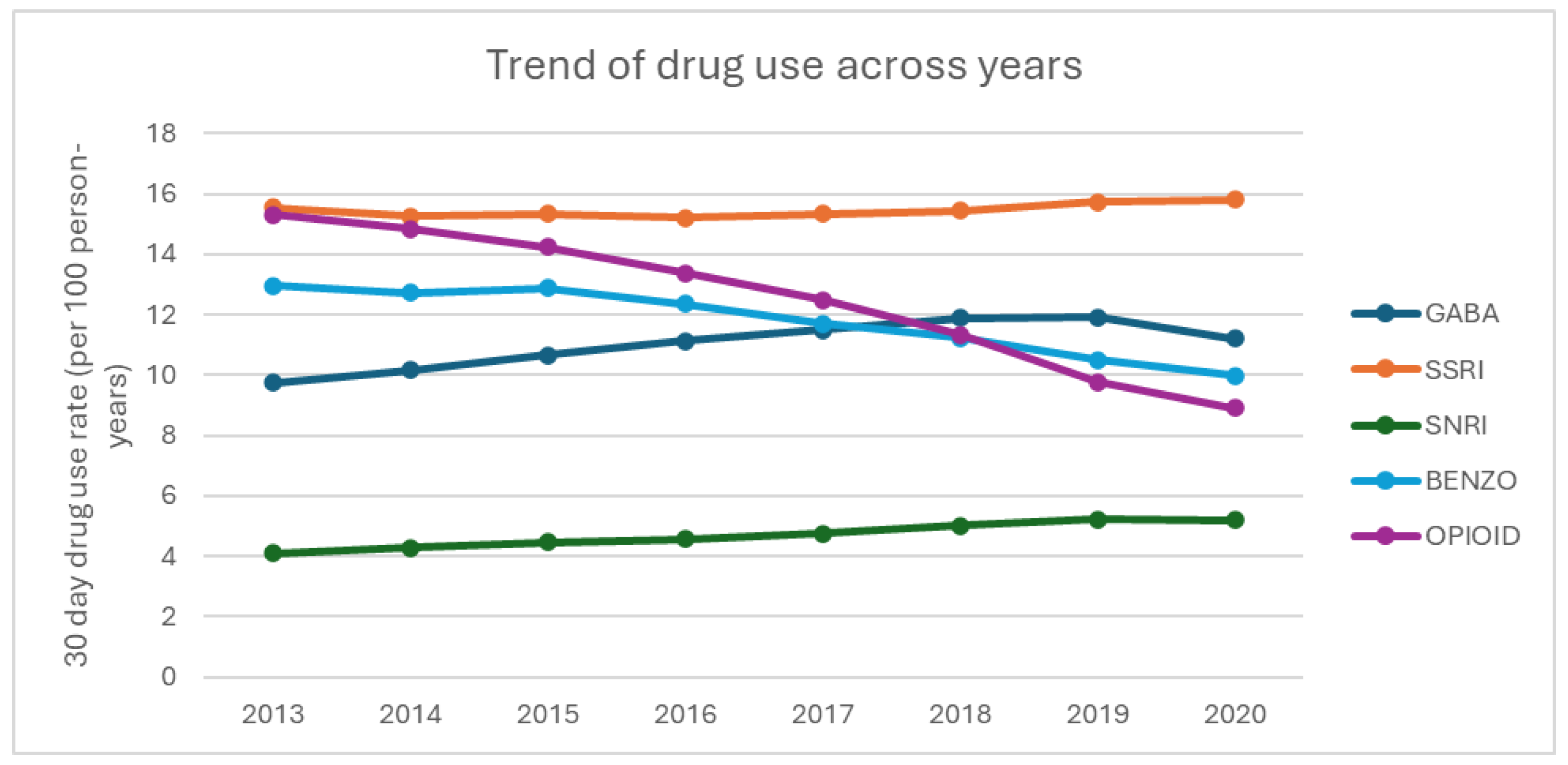
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| aOR | Adjusted odds ratio |
| AR1 | Autoregressive |
| BZD | Benzodiazepine |
| CI | Confidence Interval |
| CDC | Centers for Disease Control and Prevention |
| CMS | Centers for Medicare and Medicaid Services |
| CNS | Central nervous system |
| GABA | Gabapentinoids |
| GEE | Generalized estimating equations |
| HMO | Health Maintenance Organization |
| ICD | International Classification of Disease |
| NHB | Non-Hispanic Black |
| NHW | Non-Hispanic White |
| NSAID | Non-steroidal anti-inflammatory drugs |
| RECORD | Reporting of studies Conducted using Observational Routinely collected Data |
| SD | standard deviation |
| SEER | Surveillance, Epidemiology, and End Results |
| SNRI | Serotonin-Norepinephrine Reuptake Inhibitor |
| SSRI | Selective Serotonin Reuptake Inhibitor |
References
- Miller, K.D.; Nogueira, L.; Devasia, T.; Mariotto, A.B.; Yabroff, K.R.; Jemal, A.; Kramer, J.; Siegel, R.L. Cancer Treatment and Survivorship Statistics, 2022. CA Cancer J. Clin. 2022, 72, 409–436. [Google Scholar] [CrossRef]
- Jiang, Y.; Li, J.; Lin, H.; Huang, Q.; Wang, T.; Zhang, S.; Zhang, Q.; Rong, Z.; Xiong, J. The Efficacy of Gabapentin in Reducing Pain Intensity and Morphine Consumption after Breast Cancer Surgery: A Meta-Analysis. Medicine 2018, 97, e11581. [Google Scholar] [CrossRef]
- Andersen, B.L.; Lacchetti, C.; Ashing, K.; Berek, J.S.; Berman, B.S.; Bolte, S.; Dizon, D.S.; Given, B.; Nekhlyudov, L.; Pirl, W.; et al. Management of Anxiety and Depression in Adult Survivors of Cancer: ASCO Guideline Update. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2023, 41, 3426–3453. [Google Scholar] [CrossRef]
- Shah, R.; Chou, L.-N.; Kuo, Y.-F.; Raji, M.A. Long-Term Opioid Therapy in Older Cancer Survivors: A Retrospective Cohort Study. J. Am. Geriatr. Soc. 2019, 67, 945–952. [Google Scholar] [CrossRef]
- van den Beuken-van Everdingen, M.H.J.; Hochstenbach, L.M.J.; Joosten, E.A.J.; Tjan-Heijnen, V.C.G.; Janssen, D.J.A. Update on Prevalence of Pain in Patients with Cancer: Systematic Review and Meta-Analysis. J. Pain Symptom Manag. 2016, 51, 1070–1090.e9. [Google Scholar] [CrossRef]
- Glare, P.A.; Davies, P.S.; Finlay, E.; Gulati, A.; Lemanne, D.; Moryl, N.; Oeffinger, K.C.; Paice, J.A.; Stubblefield, M.D.; Syrjala, K.L. Pain in Cancer Survivors. J. Clin. Oncol. 2014, 32, 1739–1747. [Google Scholar] [CrossRef]
- Bell, R.J.; Robinson, P.J.; Nazeem, F.; Panjari, M.; Fradkin, P.; Schwarz, M.; Davis, S.R. Persistent Breast Pain 5 Years after Treatment of Invasive Breast Cancer Is Largely Unexplained by Factors Associated with Treatment. J. Cancer Surviv. Res. Pract. 2014, 8, 1–8. [Google Scholar] [CrossRef]
- Rief, W.; Bardwell, W.A.; Dimsdale, J.E.; Natarajan, L.; Flatt, S.W.; Pierce, J.P. Long-Term Course of Pain in Breast Cancer Survivors: A 4-Year Longitudinal Study. Breast Cancer Res. Treat. 2011, 130, 579–586. [Google Scholar] [CrossRef] [PubMed]
- Joshy, G.; Khalatbari-Soltani, S.; Soga, K.; Butow, P.; Laidsaar-Powell, R.; Koczwara, B.; Rankin, N.M.; Brown, S.; Weber, M.; Mazariego, C.; et al. Pain and Its Interference with Daily Living in Relation to Cancer: A Comparative Population-Based Study of 16,053 Cancer Survivors and 106,345 People without Cancer. BMC Cancer 2023, 23, 774. [Google Scholar] [CrossRef] [PubMed]
- Deimling, G.T.; Sterns, S.; Bowman, K.F.; Kahana, B. The Health of Older-Adult, Long-Term Cancer Survivors. Cancer Nurs. 2005, 28, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Lowery, A.E.; Starr, T.; Dhingra, L.K.; Rogak, L.; Hamrick-Price, J.R.; Farberov, M.; Kirsh, K.L.; Saltz, L.B.; Breitbart, W.S.; Passik, S.D. Frequency, Characteristics, and Correlates of Pain in a Pilot Study of Colorectal Cancer Survivors 1–10 Years Post-Treatment. Pain Med. 2013, 14, 1673–1680. [Google Scholar] [CrossRef] [PubMed]
- El-Shami, K.; Oeffinger, K.C.; Erb, N.L.; Willis, A.; Bretsch, J.K.; Pratt-Chapman, M.L.; Cannady, R.S.; Wong, S.L.; Rose, J.; Barbour, A.L.; et al. American Cancer Society Colorectal Cancer Survivorship Care Guidelines. CA. Cancer J. Clin. 2015, 65, 427–455. [Google Scholar] [CrossRef] [PubMed]
- Sutradhar, R.; Lokku, A.; Barbera, L. Cancer Survivorship and Opioid Prescribing Rates: A Population-Based Matched Cohort Study among Individuals with and without a History of Cancer. Cancer 2017, 123, 4286–4293. [Google Scholar] [CrossRef]
- Guerard, E.J.; Cleary, J.F. Managing Cancer Pain in Older Adults. Cancer J. Sudbury Mass 2017, 23, 242–245. [Google Scholar] [CrossRef]
- Winn, A.N.; Check, D.K.; Farkas, A.; Fergestrom, N.M.; Neuner, J.M.; Roberts, A.W. Association of Current Opioid Use with Serious Adverse Events Among Older Adult Survivors of Breast Cancer. JAMA Netw. Open 2020, 3, e2016858. [Google Scholar] [CrossRef]
- Paice, J.A.; Portenoy, R.; Lacchetti, C.; Campbell, T.; Cheville, A.; Citron, M.; Constine, L.S.; Cooper, A.; Glare, P.; Keefe, F.; et al. Management of Chronic Pain in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J. Clin. Oncol. 2016, 34, 3325–3345. [Google Scholar] [CrossRef]
- Gibson, D.C.; Raji, M.A.; Baillargeon, J.G.; Kuo, Y.-F. Regional and Temporal Variation in Receipt of Long-Term Opioid Therapy among Older Breast, Colorectal, Lung, and Prostate Cancer Survivors in the United States. Cancer Med. 2021, 10, 1550–1561. [Google Scholar] [CrossRef]
- Pauly, N.J.; Delcher, C.; Slavova, S.; Lindahl, E.; Talbert, J.; Freeman, P.R. Trends in Gabapentin Prescribing in a Commercially Insured U.S. Adult Population, 2009–2016. J. Manag. Care Spec. Pharm. 2020, 26, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Leung, M.T.Y.; Turner, J.P.; Marquina, C.; Ilomäki, J.; Tran, T.; Bykov, K.; Bell, J.S. Gabapentinoids and Risk of Hip Fracture. JAMA Netw. Open 2024, 7, e2444488. [Google Scholar] [CrossRef]
- Sobieraj, D.M.; Martinez, B.K.; Hernandez, A.V.; Coleman, C.I.; Ross, J.S.; Berg, K.M.; Steffens, D.C.; Baker, W.L. Adverse Effects of Pharmacologic Treatments of Major Depression in Older Adults. J. Am. Geriatr. Soc. 2019, 67, 1571–1581. [Google Scholar] [CrossRef]
- Esechie, A.; Kuo, Y.-F.; Goodwin, J.S.; Westra, J.; Raji, M.A. Trends in Prescribing Pattern of Opioid and Benzodiazepine Substitutes among Medicare Part D Beneficiaries from 2013 to 2018: A Retrospective Study. BMJ Open 2021, 11, e053487. [Google Scholar] [CrossRef]
- King, M.; Essick, C. The Geography of Antidepressant, Antipsychotic, and Stimulant Utilization in the United States. Health Place 2013, 20, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Fitch, M.I.; Nicoll, I.; Newton, L.; Strohschein, F.J. Challenges of Survivorship for Older Adults Diagnosed with Cancer. Curr. Oncol. Rep. 2022, 24, 763–773. [Google Scholar] [CrossRef] [PubMed]
- About the SEER Program. Available online: https://seer.cancer.gov/about/overview.html (accessed on 19 September 2024).
- Benchimol, E.I.; Smeeth, L.; Guttmann, A.; Harron, K.; Moher, D.; Petersen, I.; Sørensen, H.T.; von Elm, E.; Langan, S.M. RECORD Working Committee the REporting of Studies Conducted Using Observational Routinely-Collected Health Data (RECORD) Statement. PLoS Med. 2015, 12, e1001885. [Google Scholar] [CrossRef] [PubMed]
- Surbone, A.; Tralongo, P. Categorization of Cancer Survivors: Why We Need It. J. Clin. Oncol. 2016, 34, 3372–3374. [Google Scholar] [CrossRef]
- Pratt, L.A.; Brody, D.J.; Gu, Q. Antidepressant use in persons aged 12 and over: United States, 2005–2008. NCHS Data Brief 2011, 1–8. Available online: https://www.cdc.gov/nchs/data/databriefs/db76.pdf (accessed on 9 October 2024).
- Milani, S.A.; Raji, M.A.; Chen, L.; Kuo, Y.-F. Trends in the Use of Benzodiazepines, Z-Hypnotics, and Serotonergic Drugs Among US Women and Men Before and During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2131012. [Google Scholar] [CrossRef]
- Jeffery, M.M.; Hooten, W.M.; Jena, A.B.; Ross, J.S.; Shah, N.D.; Karaca-Mandic, P. Rates of Physician Coprescribing of Opioids and Benzodiazepines After the Release of the Centers for Disease Control and Prevention Guidelines in 2016. JAMA Netw. Open 2019, 2, e198325. [Google Scholar] [CrossRef]
- Grauer, J.S.; Cramer, J.D. Association of State-Imposed Restrictions on Gabapentin with Changes in Prescribing in Medicare. J. Gen. Intern. Med. 2022, 37, 3630–3637. [Google Scholar] [CrossRef]
- Lyu, X.; Guy, G.P.; Baldwin, G.T.; Losby, J.L.; Bohnert, A.S.B.; Goldstick, J.E. State-to-State Variation in Opioid Dispensing Changes Following the Release of the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain. JAMA Netw. Open 2023, 6, e2332507. [Google Scholar] [CrossRef]
- Dowell, D.; Haegerich, T.M.; Chou, R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA 2016, 315, 1624–1645. [Google Scholar] [CrossRef]
- Sayed, D.; Deer, T.R.; Hagedorn, J.M.; Sayed, A.; D’Souza, R.S.; Lam, C.M.; Khatri, N.; Hussaini, Z.; Pritzlaff, S.G.; Abdullah, N.M.; et al. A Systematic Guideline by the ASPN Workgroup on the Evidence, Education, and Treatment Algorithm for Painful Diabetic Neuropathy: SWEET. J. Pain Res. 2024, 17, 1461–1501. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 12. Retinopathy, Neuropathy, and Foot Care: Standards of Care in Diabetes—2024. Diabetes Care 2023, 47, S231–S243. [Google Scholar] [CrossRef]
- American Society of Anesthesiologists Task Force on Chronic Pain Management; American Society of Regional Anesthesia and Pain Medicine. Practice Guidelines for Chronic Pain Management: An Updated Report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine *. Anesthesiology 2010, 112, 810–833. [Google Scholar] [CrossRef]
- Runowicz, C.D.; Leach, C.R.; Henry, N.L.; Henry, K.S.; Mackey, H.T.; Cowens-Alvarado, R.L.; Cannady, R.S.; Pratt-Chapman, M.L.; Edge, S.B.; Jacobs, L.A.; et al. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. J. Clin. Oncol. 2016, 34, 611–635. [Google Scholar] [CrossRef]
- Smith, E.M.L.; Pang, H.; Cirrincione, C.; Fleishman, S.; Paskett, E.D.; Ahles, T.; Bressler, L.R.; Fadul, C.E.; Knox, C.; Le-Lindqwister, N.; et al. Effect of Duloxetine on Pain, Function, and Quality of Life among Patients with Chemotherapy-Induced Painful Peripheral Neuropathy: A Randomized Clinical Trial. JAMA 2013, 309, 1359–1367. [Google Scholar] [CrossRef] [PubMed]
- Lavu, A.; Janzen, D.; Aboulatta, L.; Peymani, P.; Haidar, L.; Desrochers, B.; Alessi-Severini, S.; Eltonsy, S. Prescription Trends of Antiseizure Medications before and during the COVID-19 Pandemic. Front. Neurol. 2023, 14, 1135962. [Google Scholar] [CrossRef]
- Johansen, M.E.; Maust, D.T. Update to Gabapentinoid Use in the United States, 2002–2021. Ann. Fam. Med. 2024, 22, 45–49. [Google Scholar] [CrossRef]
- Gorfinkel, L.R.; Hasin, D.; Saxon, A.J.; Wall, M.; Martins, S.S.; Cerdá, M.; Keyes, K.; Fink, D.S.; Keyhani, S.; Maynard, C.C.; et al. Trends in Prescriptions for Non-Opioid Pain Medications Among U.S. Adults with Moderate or Severe Pain, 2014–2018. J. Pain 2022, 23, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- Yunusa, I.; Gagne, J.J.; Yoshida, K.; Bykov, K. Risk of Opioid Overdose Associated with Concomitant Use of Oxycodone and Selective Serotonin Reuptake Inhibitors. JAMA Netw. Open 2022, 5, e220194. [Google Scholar] [CrossRef]
- DailyMed-ROXICODONE-Oxycodone Hydrochloride Tablet. Available online: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=5a8157d3-ba20-4abf-b0d4-6ad141b31d63 (accessed on 19 September 2024).
- DailyMed-OXYCONTIN-Oxycodone Hydrochloride Tablet, Film Coated, Extended Release. Available online: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=bfdfe235-d717-4855-a3c8-a13d26dadede (accessed on 19 September 2024).
- Sutherland, K.; Levesque, J.-F. Unwarranted Clinical Variation in Health Care: Definitions and Proposal of an Analytic Framework. J. Eval. Clin. Pract. 2020, 26, 687–696. [Google Scholar] [CrossRef] [PubMed]
- 2023 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2023 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J. Am. Geriatr. Soc. 2023, 71, 2052–2081. [Google Scholar] [CrossRef]
- Noyes, K.; Liu, H.; Lyness, J.M.; Friedman, B. Medicare Beneficiaries with Depression: Comparing Diagnoses in Claims Data with the Results of Screening. Psychiatr. Serv. Wash. DC 2011, 62, 1159–1166. [Google Scholar] [CrossRef]
- Hwang, S.; Jayadevappa, R.; Zee, J.; Zivin, K.; Bogner, H.R.; Raue, P.J.; Bruce, M.L.; Reynolds, C.F.; Gallo, J.J. Concordance between Clinical Diagnosis and Medicare Claims of Depression among Older Primary Care Patients. Am. J. Geriatr. Psychiatry 2015, 23, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Fung, V.; Price, M.; McDowell, A.; Nierenberg, A.A.; Hsu, J.; Newhouse, J.P.; Lê Cook, B. Coverage Parity And Racial and Ethnic Disparities in Mental Health and Substance Use Care Among Medicare Beneficiaries. Health Aff. Proj. Hope 2023, 42, 83–93. [Google Scholar] [CrossRef] [PubMed]





| Variables | 2013 (n = 281,168) | 2016 (n = 397,369) | 2018 (n = 381,601) | 2020 (n = 359,097) |
|---|---|---|---|---|
| Age | ||||
| mean (std) | 77.6 (7.3) | 77.6 (7.3) | 77.8 (7.3) | 78.2 (7.4) |
| median (IQR) | 77.0 (72.0, 83.0) | 77.0 (72.0, 83.0) | 77.0 (72.0, 83.0) | 77.0 (72.0, 83.0) |
| Age, categorical | ||||
| 66–74 | 111,333 (39.6) | 157,955 (39.8) | 145,367 (38.1) | 131,360 (36.6) |
| 75–84 | 116,008 (41.3) | 163,628 (41.2) | 162,445 (42.6) | 154,057 (42.9) |
| 85+ | 53,827 (19.1) | 75,786 (19.1) | 73,789 (19.3) | 73,680 (20.5) |
| Years post-cancer diagnosis | ||||
| Mean (std) | 7.6 (3.4) | 9.0 (4.1) | 10.3 (4.4) | 12.0 (4.5) |
| Median (IQR) | 7.0 (5.0, 10.0) | 9.0 (6.0, 12.0) | 10.0 (7.0, 14.0) | 12.0 (8.0, 16.0) |
| Gender | ||||
| Male | 149,342 (53.1) | 215,658 (54.3) | 204,782 (53.7) | 189,403 (52.7) |
| Female | 131,826 (46.9) | 181,711 (45.7) | 176,819 (46.3) | 169,694 (47.3) |
| Race and Ethnicity | ||||
| Hispanic | 21,894 (7.8) | 25,314 (6.4) | 24,720 (6.5) | 22,755 (6.3) |
| NHB | 20,059 (7.1) | 28,178 (7.1) | 25,320 (6.6) | 22,054 (6.1) |
| NHW | 225,164 (80.1) | 324,992 (81.8) | 311,409 (81.6) | 294,233 (81.9) |
| NH Others | 14,051 (5.0) | 18,885 (4.8) | 20,152 (5.3) | 20,055 (5.6) |
| Cancer diagnosis | ||||
| Breast | 89,279 (31.8) | 129,550 (32.6) | 129,879 (34.0) | 128,550 (35.8) |
| Colorectal | 49,513 (17.6) | 62,416 (15.7) | 57,635 (15.1) | 51,989 (14.5) |
| Lung | 18,881 (6.7) | 24,674 (6.2) | 21,860 (5.7) | 18,406 (5.1) |
| Prostate | 123,495 (43.9) | 180,729 (45.5) | 172,227 (45.1) | 160,152 (44.6) |
| Diagnosis cohort | ||||
| 2000–2003 | 91,889 (32.7) | 99,202 (25.0) | 84,464 (22.1) | 74,091 (20.6) |
| 2004–2007 | 101,418 (36.1) | 112,943 (28.4) | 98,691 (25.9) | 88,955 (24.8) |
| 2008–2011 | 83,641 (29.8) | 118,612 (29.9) | 108,257 (28.4) | 101,296 (28.2) |
| 2012–2015 | 4220 (1.5) | 66,612 (16.8) | 90,189 (23.6) | 94,755 (26.4) |
| Census region * | ||||
| Midwest | 22,132 (7.9) | 31,161 (7.8) | 28,289 (7.4) | 25,737 (7.2) |
| Northeast | 94,608 (33.6) | 140,235 (35.3) | 132,379 (34.7) | 123,681 (34.4) |
| South | 85,964 (30.6) | 117,379 (29.5) | 110,746 (29.0) | 103,225 (28.7) |
| West | 78,365 (27.9) | 108,443 (27.3) | 110,062 (28.8) | 106,245 (29.6) |
| Urban-rural status | ||||
| Metro | 239,065 (85.0) | 342,713 (86.3) | 331,230 (86.8) | 313,068 (87.2) |
| Non-Metro | 42,041 (15.0) | 54,572 (13.7) | 50,298 (13.2) | 45,969 (12.8) |
| Unknown | 62 (0.0) | 84 (0.0) | 73 (0.0) | 60 (0.0) |
| Original reason for enrollment | ||||
| Disability | 27,061 (9.6) | 36,041 (9.1) | 34,504 (9.0) | 31,900 (8.9) |
| Not disability related | 254,107 (90.4) | 361,328 (90.9) | 347,097 (91.0) | 327,197 (91.1) |
| Dual eligibility | ||||
| Yes | 64,312 (22.9) | 63,790 (16.1) | 59,736 (15.7) | 52,866 (14.7) |
| No | 216,856 (77.1) | 333,579 (83.9) | 321,865 (84.4) | 306,231 (85.3) |
| Charlson comorbidity => 1 | 192,886 (68.6) | 269,970 (67.9) | 258,751 (67.8) | 245,176 (68.3) |
| Depressive disorder | 32,962 (12.4) | 53,326 (12.2) | 53,500 (14.0) | 55,797 (15.5) |
| Anxiety disorder | 27,752 (9.9) | 49,190 (12.4) | 54,607 (14.3) | 57,067 (15.9) |
| Alcohol use disorder | 3944 (1.4) | 7664 (1.9) | 5829 (1.5) | 5887 (1.6) |
| Drug use disorder | 2333 (0.8) | 5652 (1.4) | 7372 (1.9) | 8358 (2.3) |
| Opioid naïve ** | 189,083 (67.3) | 277,532 (69.8) | 278,559 (73.0) | 277,098 (77.2) |
| GABA aOR (95% CI) | BENZO aOR (95% CI) | SSRI aOR (95% CI) | SNRI aOR (95% CI) | OPIOID aOR (95% CI) | ||
|---|---|---|---|---|---|---|
| Years post-cancer diagnosis | 0.99 (0.99, 1.00) | 1.01 (1.00, 1.01) | 1.02 (1.01, 1.02) | 1.01 (0.99, 1.01) | 1.01 (1.00, 1.01) | |
| calendar year | 2014 | 1.09 (1.08, 1.11) | 0.98 (0.97, 0.99) | 0.99 (0.98, 1.00) | 1.05 (1.03, 1.07) | 0.98 (0.96, 0.99) |
| 2015 | 1.15 (1.13, 1.17) | 0.98 (0.97, 1.00) | 0.98 (0.97, 1.00) | 1.06 (1.03, 1.09) | 0.90 (0.88, 0.92) | |
| 2016 | 1.23 (1.21, 1.26) | 0.93 (0.91, 0.94) | 0.97 (0.95, 0.99) | 1.09 (1.05, 1.12) | 0.84 (0.83, 0.86) | |
| 2017 | 1.31 (1.28, 1.35) | 0.87 (0.84, 0.89) | 0.98 (0.96, 1.00) | 1.14 (1.09, 1.19) | 0.80 (0.78, 0.82) | |
| 2018 | 1.37 (1.33, 1.42) | 0.81 (0.79, 0.84) | 0.98 (0.95, 1.01) | 1.19 (1.14, 1.25) | 0.72 (0.70, 0.74) | |
| 2019 | 1.40 (1.35, 1.45) | 0.75 (0.72, 0.78) | 0.99 (0.96, 1.02) | 1.25 (1.18, 1.32) | 0.62 (0.60, 0.64) | |
| 2020 | 1.34 (1.28, 1.40) | 0.71 (0.68, 0.74) | 0.99 (0.95, 1.02) | 1.25 (1.17, 1.34) | 0.59 (0.57, 0.62) | |
| age | 75–84 | 1.08 (1.07, 1.09) | 1.01 (0.99, 1.01) | 1.02 (1.01, 1.03) | 0.86 (0.84, 0.87) | 1.06 (1.05, 1.08) |
| 85+ | 0.99 (0.97, 1.01) | 0.97 (0.95, 0.98) | 1.12 (1.11, 1.14) | 0.69 (0.67, 0.71) | 1.14 (1.13, 1.16) | |
| Gender | Female | 1.18 (1.15, 1.21) | 1.59 (1.55, 1.64) | 1.73 (1.68, 1.77) | 1.86 (1.77, 1.95) | 1.25 (1.22, 1.28) |
| Race and Ethnicity | Hispanics | 1.01 (0.98, 1.03) | 0.75 (0.73, 0.77) | 0.71 (0.69, 0.72) | 0.62 (0.59, 0.65) | 0.84 (0.82, 0.86) |
| NH Unknowns/Others | 0.85 (0.83, 0.88) | 0.50 (0.48, 0.52) | 0.41 (0.40, 0.43) | 0.42 (0.39, 0.45) | 0.54 (0.52, 0.56) | |
| NHB | 1.03 (1.00, 1.05) | 0.44 (0.43, 0.46) | 0.40 (0.39, 0.41) | 0.45 (0.43, 0.47) | 1.02 (1.00, 1.04) | |
| Cancer diagnosis | Breast | 0.84 (0.82, 0.86) | 0.73 (0.71, 0,75) | 0.87 (0.85, 0.89) | 1.11 (1.07, 1.15) | 0.76 (0.74, 0.78) |
| Colorectal | 0.81 (0.78, 0.83) | 0.66 (0.64, 0.68) | 0.78 (0.76, 0.80) | 0.79 (0.76, 0.83) | 0.77 (0.75, 0.79) | |
| Prostate | 0.71 (0.69, 0.73) | 0.68 (0.66, 0.71) | 0.81 (0.78, 0.83) | 0.89 (0.85, 0.94) | 0.70 (0.69, 0.72) | |
| Diagnosis cohort | 2004–2007 | 1.01 (0.98, 1.04) | 1.02 (0.99, 1.05) | 1.02 (1.00, 1.05) | 0.98 (0.94, 1.03) | 0.99 (0.97, 1.02) |
| 2008–2011 | 1.01 (0.95, 1.05) | 1.03 (0.98, 1.09) | 1.03 (0.99, 1.08) | 0.99 (0.92, 1.06) | 0.99 (0.95, 1.04) | |
| 2012–2015 | 0.99 (0.92, 1.06) | 1.05 (0.98, 1.13) | 1.06 (0.99, 1.13) | 1.02 (0.92, 1.14) | 0.96 (0.90, 1.03) | |
| Census region | NorthEast | 0.83 (0.81, 0.86) | 1.04 (1.01, 1.06) | 0.95 (0.93, 0.97) | 0.86 (0.83, 0.90) | 0.65 (0.64, 0.67) |
| South | 1.24 (1.21, 1.27) | 1.15 (1.12, 1.17) | 1.11 (1.09, 1.14) | 1.22 (1.18, 1.27) | 0.98 (0.96, 1.00) | |
| West | 1.07 (1.05, 1.10) | 0.98 (0.96, 1.01) | 0.92 (0.90, 0.94) | 1.03 (0.99, 1.08) | 0.94 (0.91, 0.96) | |
| Urban-rural status | Non-Metro | 1.09 (1.07, 1.11) | 0.91 (0.89, 0.93) | 1.08 (1.06, 1.10) | 0.91 (0.88, 0.94) | 1.17 (1.15, 1.19) |
| Unknown | 0.92 (0.59, 1.44) | 1.28 (0.84, 1.96) | 0.86 (0.56, 1.32) | 1.39 (0.79, 2.46) | 1.29 (0.85, 1.94) | |
| Original reason for entitlement | Disability | 1.72 (1.69, 1.75) | 1.71 (1.68, 1.75) | 1.44 (1.42, 1.47) | 1.76 (1.71, 1.81) | 1.95 (1.92, 1.99) |
| Dual eligibility | Yes | 1.53 (1.51, 1.55) | 1.31 (1.29, 1.33) | 1.48 (1.46, 1.50) | 1.22 (1.19, 1.24) | 1.70 (1.68, 1.73) |
| Charlson comorbidity ≥ 1 | 1.33 (1.32, 1.34) | 1.09 (1.08, 1.10) | 1.12 (1.11, 1.13) | 1.11 (1.10, 1.13) | 1.38 (1.36, 1.40) | |
| Depressive disorder | 1.19 (1.18, 1.20) | 1.24 (1.22, 1.25) | 1.51 (1.50, 1.53) | 1.59 (1.56, 1.61) | 1.27 (1.26, 1.29) | |
| Anxiety disorder | 1.10 (1.09, 1.11) | 1.56 (1.54, 1.57) | 1.22 (1.21, 1.23) | 1.18 (1.16, 1.20) | 1.26 (1.25, 1.28) | |
| Alcohol use disorder | 1.06 (1.03, 1.09) | 0.98 (0.95, 1.00) | 1.04 (1.02, 1.06) | 1.05 (1.01, 1.09) | 0.95 (0.92, 0.98) | |
| Drug use disorder | 1.26 (1.23, 1.29) | 1.13 (1.10, 1.15) | 1.01 (0.99, 1.03) | 1.17 (1.13, 1.21) | 2.79 (2.73, 2.86) | |
| Opioid naive | 0.70 (0.69, 0.70) | 0.85 (0.84, 0.85) | 0.94 (0.94, 0.95) | 0.80 (0.79, 0.81) | 0.14 (0.14, 0.14) |
| GABA aOR (95% CI) | BENZO aOR (95% CI) | SSRI aOR (95% CI) | SNRI aOR (95% CI) | OPIOID aOR (95% CI) | ||
|---|---|---|---|---|---|---|
| Opioid Naive | ||||||
| Calendar Year | 2014 | 1.12 (1.10, 1.14) | 0.99 (0.98, 1.01) | 0.99 (0.98, 1.01) | 1.03 (1.01, 1.06) | 0.97 (0.94, 1.01) |
| 2015 | 1.27 (1.24, 1.30) | 1.02 (1.01, 1.04) | 1.01 (0.98, 1.02) | 1.07 (1.04, 1.11) | 0.95 (0.92, 0.98) | |
| 2016 | 1.38 (1.34, 1.42) | 0.97 (0.94, 0.99) | 0.99 (0.97, 1.01) | 1.09 (1.05, 1.14) | 0.84 (0.81, 0.87) | |
| 2017 | 1.48 (1.43, 1.53) | 0.91 (0.88, 0.94) | 1.01 (0.98, 1.03) | 1.16 (1.10, 1.23) | 0.77 (0.74, 0.80) | |
| 2018 | 1.56 (1.50, 1.63) | 0.86 (0.83, 0.90) | 1.01 (0.98, 1.04) | 1.22 (1.15, 1.30) | 0.65 (0.62, 0.68) | |
| 2019 | 1.62 (1.54, 1.69) | 0.80 (0.77, 0.84) | 1.02 (0.99, 1.06) | 1.29 (1.20, 1.38) | 0.51 (0.48, 0.53) | |
| 2020 | 1.55 (1.47, 1.63) | 0.76 (0.72, 0.80) | 1.02 (0.97, 1.06) | 1.27 (1.17, 1.38) | 0.47 (0.45, 0.50) | |
| Non-Opioid Naïve * | ||||||
| Calendar Year | 2014 | 1.06 (1.04, 1.09) | 0.94 (0.92, 0.96) | 0.94 (0.92, 0.96) | 1.05 (1.02, 1.09) | 1.02 (1.00, 1.03) |
| 2015 | 1.08 (1.05, 1.11) | 0.91 (0.89, 0.94) | 0.91 (0.88, 0.93) | 1.06 (1.02, 1.10) | 0.98 (0.96, 1.01) | |
| 2016 | 1.14 (1.11, 1.18) | 0.85 (0.83, 0.88) | 0.88 (0.86, 0.91) | 1.10 (1.05, 1.16) | 0.95 (0.93, 0.98) | |
| 2017 | 1.23 (1.18, 1.27) | 0.79 (0.76, 0.82) | 0.88 (0.85, 0.91) | 1.16 (1.09, 1.23) | 0.92 (0.89, 0.95) | |
| 2018 | 1.30 (1.24, 1.35) | 0.74 (0.70, 0.77) | 0.87 (0.83, 0.90) | 1.23 (1.15, 1.31) | 0.85 (0.82, 0.88) | |
| 2019 | 1.32 (1.25, 1.38) | 0.66 (0.63, 0.70) | 0.85 (0.82, 0.90) | 1.28 (1.19, 1.38) | 0.76 (0.73, 0.79) | |
| 2020 | 1.21 (1.14, 1.28) | 0.61 (0.57, 0.65) | 0.84 (0.80, 0.89) | 1.30 (1.19, 1.41) | 0.72 (0.69, 0.76) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, A.; Kuo, Y.-F.; Gao, D.; Raji, M. Regional and Temporal Variation in Receipt of Gabapentinoid and SSRI/SNRI Therapy Among Older Cancer Survivors in the United States. Curr. Oncol. 2025, 32, 576. https://doi.org/10.3390/curroncol32100576
Nguyen A, Kuo Y-F, Gao D, Raji M. Regional and Temporal Variation in Receipt of Gabapentinoid and SSRI/SNRI Therapy Among Older Cancer Survivors in the United States. Current Oncology. 2025; 32(10):576. https://doi.org/10.3390/curroncol32100576
Chicago/Turabian StyleNguyen, Amber, Yong-Fang Kuo, Daoqi Gao, and Mukaila Raji. 2025. "Regional and Temporal Variation in Receipt of Gabapentinoid and SSRI/SNRI Therapy Among Older Cancer Survivors in the United States" Current Oncology 32, no. 10: 576. https://doi.org/10.3390/curroncol32100576
APA StyleNguyen, A., Kuo, Y.-F., Gao, D., & Raji, M. (2025). Regional and Temporal Variation in Receipt of Gabapentinoid and SSRI/SNRI Therapy Among Older Cancer Survivors in the United States. Current Oncology, 32(10), 576. https://doi.org/10.3390/curroncol32100576





