Stereotactic Body Radiation Therapy for Symptomatic Pancreatic Insulinoma: Two-Case Report and Literature Review
Abstract
1. Introduction
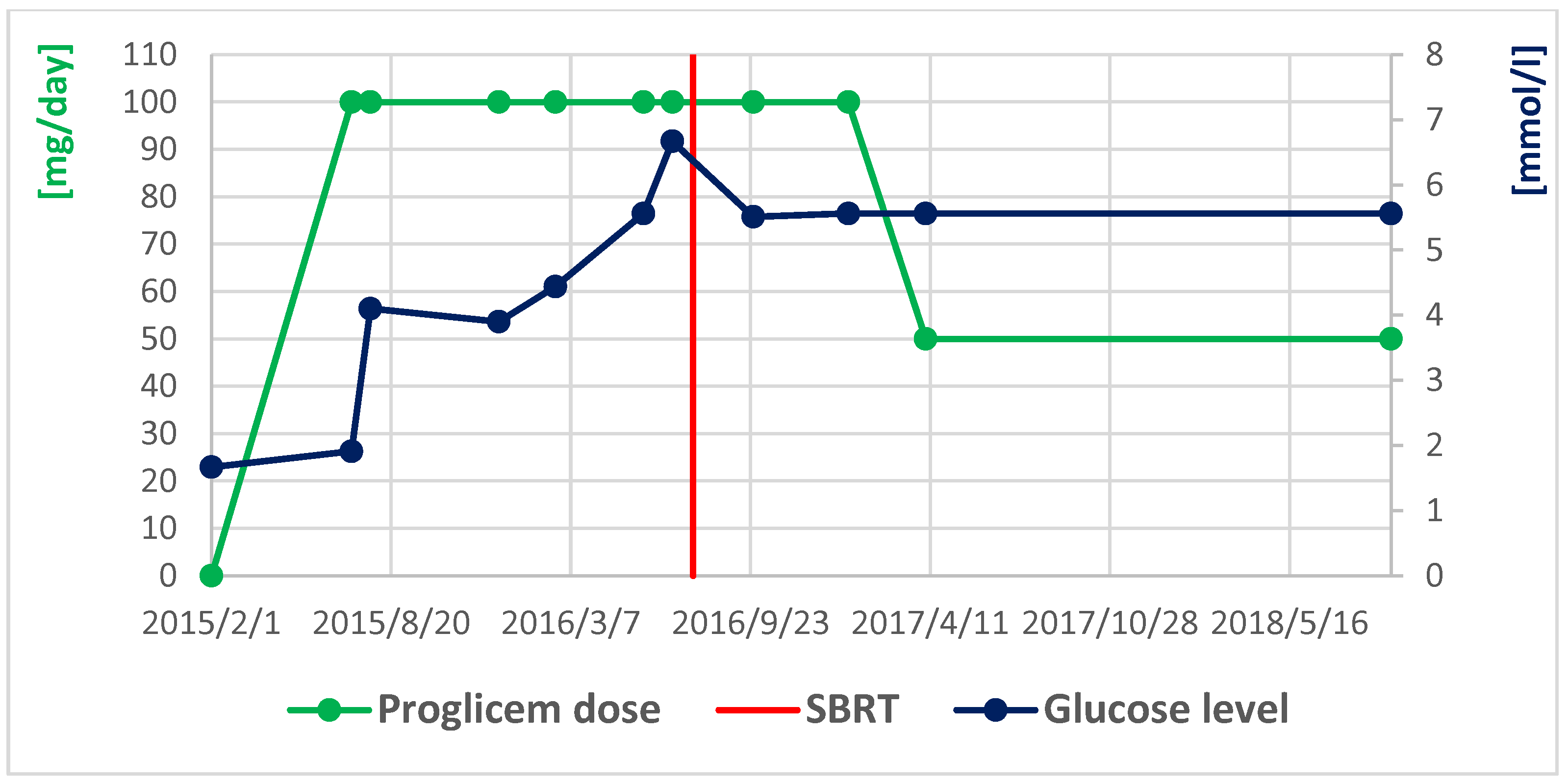
2. First Case
3. Second Case
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Okabayashi, T.; Shima, Y.; Sumiyoshi, T.; Kozuki, A.; Ito, S.; Ogawa, Y.; Kobayashi, M.; Hanazaki, K. Diagnosis and management of insulinoma. World J. Gastroenterol. 2013, 19, 829–837. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- De Herder, W.W.; Niederle, B.; Scoazec, J.Y.; Pauwels, S.; Klöppel, G.; Falconi, M.; Kwekkeboom, D.J.; Öberg, K.; Eriksson, B.; Wiedenmann, B.; et al. Diego FeroneFrascati Consensus Conference; European Neuroendocrine Tumor Society: Well-differentiated pancreatic tumor/carcinoma: Insulinoma. Neuroendocrinology 2006, 84, 183–188. [Google Scholar] [CrossRef]
- Tucker, O.N.; Crotty, P.L.; Conlon, K.C. The management of insulinoma. Br. J. Surg. 2006, 93, 264–275. [Google Scholar] [CrossRef] [PubMed]
- McAuley, G.; Delaney, H.; Colville, J.; Lyburn, I.; Worsley, D.; Govender, P.; Torreggiani, W.C. Multimodality preoperative imaging of pancreatic insulinomas. Clin. Radiol. 2005, 60, 1039–1050. [Google Scholar] [CrossRef] [PubMed]
- Kos-Kudła, B.; Rosiek, V.; Borowska, M.; Bednarczuk, T.; Bolanowski, M.; Chmielik, E.; Ćwikła, J.B.; Foltyn, W.; Gisterek, I.; Handkiewicz-Junak, D.; et al. Pancreatic neuroendocrine neoplasms—Update of the diagnostic and therapeutic guidelines (recommended by the Polish Network of Neuroendocrine Tumours) [Nowotwory neuroendokrynne trzustki—Uaktualnione zasady diagnostyki i leczenia (rekomendowane przez Polską Sieć Guzów Neuroendokrynych)]. Endokrynol. Pol. 2022, 73, 491–548. [Google Scholar] [CrossRef] [PubMed]
- De Carbonnières, A.; Challine, A.; Cottereau, A.S.; Coriat, R.; Soyer, P.; Abou Ali, E.; Prat, F.; Terris, B.; Bertherat, J.; Dousset, B.; et al. Surgical management of insulinoma over three decades. HPB 2021, 23, 1799–1806. [Google Scholar] [CrossRef] [PubMed]
- Swanson, R.S.; Pezzi, C.M.; Mallin, K.; Loomis, A.M.; Winchester, D.P. The 90-day mortality after pancreatectomy for cancer is double the 30- day mortality: More than 20,000 resections from the national cancer data base. Ann. Surg. Oncol. 2014, 21, 4059–4067. [Google Scholar] [CrossRef] [PubMed]
- El Amrani, M.; Clément, G.; Lenne, X.; Laueriere, C.; Turpin, A.; Theis, D.; Pruvot, F.R.; Truant, S. Should all pancreatic surgery be centralized regardless of patients’ comorbidity? HPB 2020, 22, 1057–1066. [Google Scholar] [CrossRef] [PubMed]
- El Amrani, M.; Lenne, X.; Clement, G.; Delpero, J.R.; Theis, D.; Pruvot, F.R.; Bruandet, A.; Truant, S. Specificity of procedure volume and its association with post operative mortality in digestive cancer surgery: A nationwide study of 225,752 patients. Ann. Surg. 2019, 270, 775–782. [Google Scholar] [CrossRef]
- Hofland, J.; Falconi, M.; Christ, E.; Castaño, J.P.; Faggiano, A.; Lamarca, A.; Perren, A.; Petrucci, S.; Prasad, V.; Ruszniewski, P.; et al. European Neuroendocrine Tumor Society 2023 guidance paper for functioning pancreatic neuroendocrine tumour syndromes. J. Neuroendocrinol. 2023, 35, e13318. [Google Scholar] [CrossRef] [PubMed]
- Habibollahi, P.; Bai, H.X.; Sanampudi, S.; Soulen, M.C.; Dagli, M. Effectiveness of Liver-Directed Therapy for the Management of Intractable Hypoglycemia in Metastatic Insulinoma. Pancreas 2020, 49, 763–767. [Google Scholar] [CrossRef] [PubMed]
- Huscher, C.G.S.; Mingoli, A.; Sgarzini, G.; Mereu, A.; Gasperi, M. Image-guided robotic radiosurgery (Cyber Knife) for pancreatic insulinoma: Is laparoscopy becoming old? Surg. Innov. 2012, 19, NP14–NP17. [Google Scholar] [CrossRef]
- Giannis, D.; Moris, D.; Karachaliou, G.S.; Tsilimigras, D.I.; Karaolanis, G.; Papalampros, A.; Felekouras, E. Insulinomas: From diagnosis to treatment. A review of the literature. J. BUON 2020, 25, 1302–1314. [Google Scholar] [PubMed]
- Ehehalt, F.; Saeger, H.D.; Schmidt, C.M.; Grützmann, R. Neuroendocrine tumors of the pancreas. Oncologist 2009, 14, 456–467. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Liu, X.; Wu, J.; Xu, W.; Gao, W.; Jiang, K.; Zhang, Z.; Miao, Y. Diagnosis and surgical management of insulinomas in 33 consecutive patients at a single institution. Langenbecks Arch. Surg. 2016, 401, 1019–1025. [Google Scholar] [CrossRef] [PubMed]
- Atiq, M.; Bhutani, M.S.; Bektas, M.; Lee, J.E.; Gong, Y.; Tamm, E.P.; Shah, C.P.; Ross, W.A.; Yao, J.; Raju, G.S.; et al. EUS-FNA for pancreatic neuroendocrine tumors: A tertiary cancer center experience. Dig. Dis. Sci. 2012, 57, 791–800. [Google Scholar] [CrossRef] [PubMed]
- Zografos, G.N.; Stathopoulou, A.; Mitropapas, G.; Karoubalis, J.; Kontogeorgos, G.; Kaltsas, G.; Piaditis, G.; Papastratis, G.I. Preoperative imaging and localization of small sized insulinoma with EUS-guided fine needle tattoing: A case report. Hormones 2005, 4, 111–116. [Google Scholar] [PubMed]
- Calabrò, D.; Argalia, G.; Ambrosini, V. Role of PET/CT and Therapy Management of Pancreatic Neuroendocrine Tumors. Diagnostics 2020, 10, 1059. [Google Scholar] [CrossRef] [PubMed]
- Antwi, K.; Fani, M.; Heye, T.; Nicolas, G.; Rottenburger, C.; Kaul, F.; Merkle, E.; Zech, C.J.; Boll, D.; Vogt, D.R.; et al. Comparison of glucagon-like peptide-1 receptor (GLP-1R) PET/CT, SPECT/CT and 3T MRI for the localisation of occult insulinomas: Evaluation of diagnostic accuracy in a prospective crossover imaging study. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 2318–2327. [Google Scholar] [CrossRef] [PubMed]
- Gill, G.V.; Rauf, O.; McFarlane, I.A. Diazoxide treatment for insulinoma: A national UK survey. Postgrad. Med. J. 1997, 73, 640–641. [Google Scholar] [CrossRef]
- Niitsu, Y.; Minami, I.; Izumiyama, H.; Hashimoto, K.; Yoshimoto, T.; Satou, F.; Tsujino, M.; Ota, K.; Kudo, A.; Tanabe, M.; et al. Clinical outcomes of 20 Japanese patients with insulinoma treated with diazoxide. Endocr. J. 2019, 66, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Jensen, R.T. Perspectives on the current pharmacotherapeutic strategies for management of functional neuroendocrine tumor syndromes. Expert Opin. Pharmacother. 2021, 22, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Rimbaş, M.; Rizzatti, G.; Tosoni, A.; Impagnatiello, M.; Panzuto, F.; Larghi, A. Small nonfunctional pancreatic neuroendocrine neoplasms: Time for a step-up treatment approach? Endosc. Ultrasound. 2022, 12, 1–17. [Google Scholar] [CrossRef]
- Falconi, M.; Eriksson, B.; Kaltsas, G.; Bartsch, D.K.; Capdevila, J.; Caplin, M.; Kos-Kudla, B.; Kwekkeboom, D.; Rindi, G.; Klöppel, G.; et al. Vienna Consensus Conference participants. ENETS Consensus Guidelines Update for the Management of Patients with Functional Pancreatic Neuroendocrine Tumors and Non-Functional Pancreatic Neuroendocrine Tumors. Neuroendocrinology 2016, 103, 153–171. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Armellini, E.; Facciorusso, A.; Crinò, S.F. Efficacy and Safety of Endoscopic Ultrasound-Guided Radiofrequency Ablation for Pancreatic Neuroendocrine Tumors: A Systematic Review and Metanalysis. Medicina 2023, 59, 359. [Google Scholar] [CrossRef] [PubMed]
- Mehrabi, A.; Fischer, L.; Hafezi, M.; Dirlewanger, A.; Grenacher, L.; Diener, M.K.; Fonouni, H.; Golriz, M.; Garoussi, C.; Fard, N.; et al. A systematic review of localization, surgical treatment options, and outcome of insulinoma. Pancreas 2014, 43, 675–686. [Google Scholar] [CrossRef] [PubMed]
- Timmerman, R. A Story of Hypofractionation and the Table on the Wall. Int. J. Radiat. Oncol. Biol. Phys. 2022, 112, 4–21. [Google Scholar] [CrossRef] [PubMed]
- Alsuhaibani, A.A.; Alsuhaibani, A.A.; Hassan, T.S. Curative treatment of pancreatic functioning insulinoma with stereotactic ablative radiation therapy: Case report. Int. Surg. J. 2022, 9, 181–184. [Google Scholar] [CrossRef]
- Schellenberg, D.; Goodman, K.A.; Lee, F.; Chang, S.; Kuo, T.; Ford, J.M.; Fisher, G.A.; Quon, A.; Desser, T.S.; Norton, J.; et al. Gemcitabine chemotherapy and single-fraction stereotactic body radiotherapy for locally advanced pancreatic cancer. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 678–686. [Google Scholar] [CrossRef]
- Pollom, E.L.; Alagappan, M.; von Eyben, R.; Kunz, P.L.; Fisher, G.A.; Ford, J.A.; Poultsides, G.A.; Visser, B.C.; Norton, J.A.; Kamaya, A.; et al. Single- versus multifraction stereotactic body radiation therapy for pancreatic adenocarcinoma: Outcomes and toxicity. Int. J. Radiat. Oncol. Biol. Phys. 2014, 90, 918–925. [Google Scholar] [CrossRef] [PubMed]
- Song, C.W.; Park, I.; Cho, L.C.; Yuan, J.; Dusenbery, K.E.; Griffin, R.J.; Levitt, S.H. Is indirect cell death involved in response of tumors to stereotactic radiosurgery and stereotactic body radiation therapy? Int. J. Radiat. Oncol. Biol. Phys. 2014, 89, 924–925. [Google Scholar] [CrossRef] [PubMed]
- Keisari, Y. Tumor abolition and antitumor immunostimulation by physico-chemical tumor ablation. Front. Biosci. 2017, 22, 310–347. [Google Scholar] [CrossRef] [PubMed]
- Jan Van Limbergen, E.; Lieverse, R.I.Y.; Houben, R.; Overhof, C.; Postma, A.; Zindler, J.; Verhelst, F.; Dubois, L.J.; De Ruyssche, D.; Lambin, P. Toxicity of L19-Interleukin 2 Combined with Stereotactic Body Radiation Therapy: A Phase 1 Study. Int. J. Radiat. Oncol. Biol. Phys. 2021, 109, 1421–1430. [Google Scholar] [CrossRef] [PubMed]









Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Namysl-Kaletka, A.; Wydmanski, J.; Debosz-Suwinska, I.; Kaszuba, M.; Gabrys, D.; Roch-Zniszczol, A.; Handkiewicz-Junak, D. Stereotactic Body Radiation Therapy for Symptomatic Pancreatic Insulinoma: Two-Case Report and Literature Review. Curr. Oncol. 2024, 31, 4123-4132. https://doi.org/10.3390/curroncol31070307
Namysl-Kaletka A, Wydmanski J, Debosz-Suwinska I, Kaszuba M, Gabrys D, Roch-Zniszczol A, Handkiewicz-Junak D. Stereotactic Body Radiation Therapy for Symptomatic Pancreatic Insulinoma: Two-Case Report and Literature Review. Current Oncology. 2024; 31(7):4123-4132. https://doi.org/10.3390/curroncol31070307
Chicago/Turabian StyleNamysl-Kaletka, Agnieszka, Jerzy Wydmanski, Iwona Debosz-Suwinska, Malgorzata Kaszuba, Dorota Gabrys, Agata Roch-Zniszczol, and Daria Handkiewicz-Junak. 2024. "Stereotactic Body Radiation Therapy for Symptomatic Pancreatic Insulinoma: Two-Case Report and Literature Review" Current Oncology 31, no. 7: 4123-4132. https://doi.org/10.3390/curroncol31070307
APA StyleNamysl-Kaletka, A., Wydmanski, J., Debosz-Suwinska, I., Kaszuba, M., Gabrys, D., Roch-Zniszczol, A., & Handkiewicz-Junak, D. (2024). Stereotactic Body Radiation Therapy for Symptomatic Pancreatic Insulinoma: Two-Case Report and Literature Review. Current Oncology, 31(7), 4123-4132. https://doi.org/10.3390/curroncol31070307





