The Impact of Medicaid Expansion on Patients with Cancer in the United States: A Review
Abstract
1. Introduction
2. Medicaid Expansion: A Brief History
3. Key Features of the ACA That Enabled Medicaid Expansion
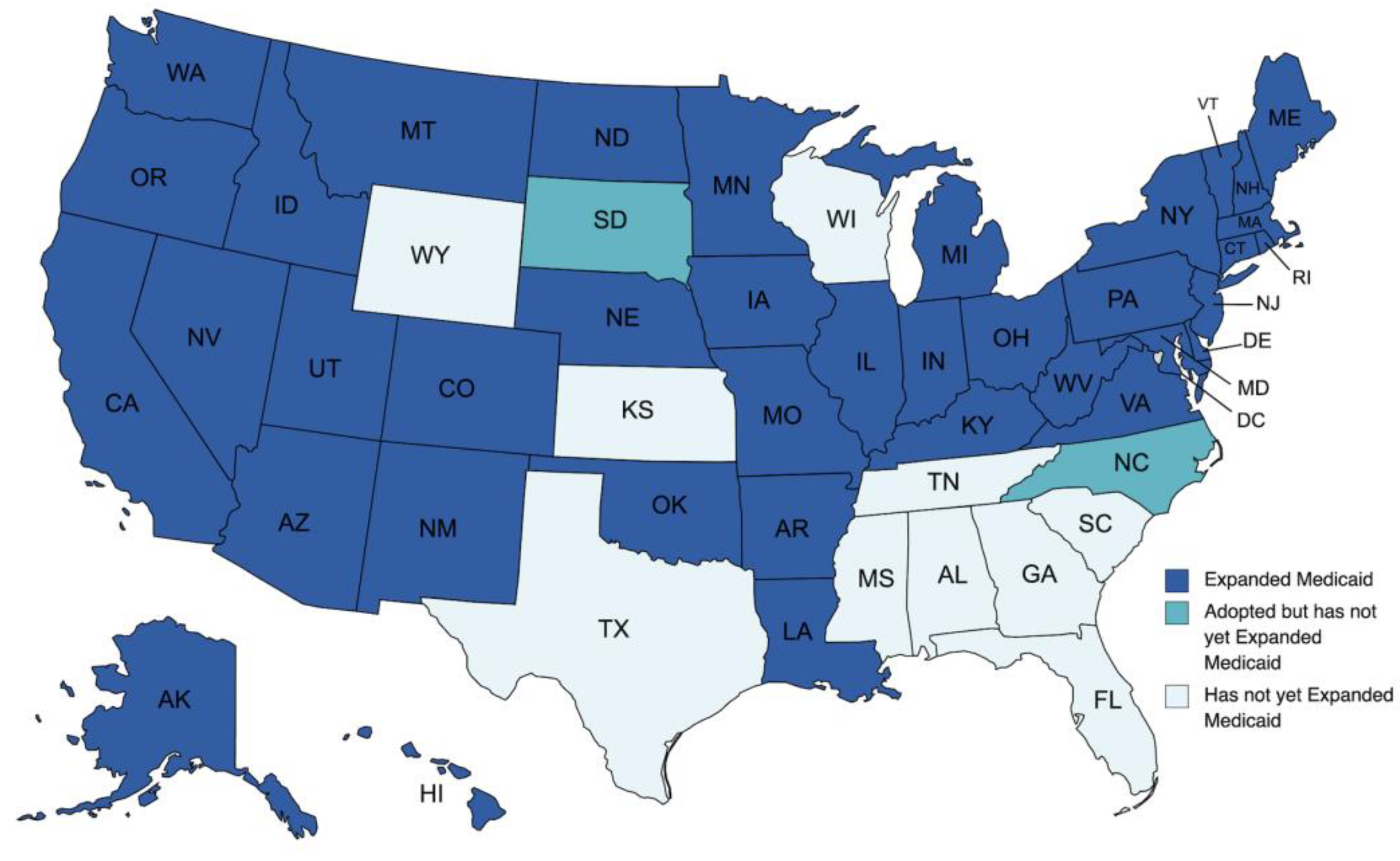
4. Current Status of Medicaid Expansion
5. Impact of Medicaid Expansion on Health and Hospitals
6. Impact of Medicaid Expansion on Patients with Cancer
6.1. Improved Access to Care
6.2. Enhanced Quality of Care
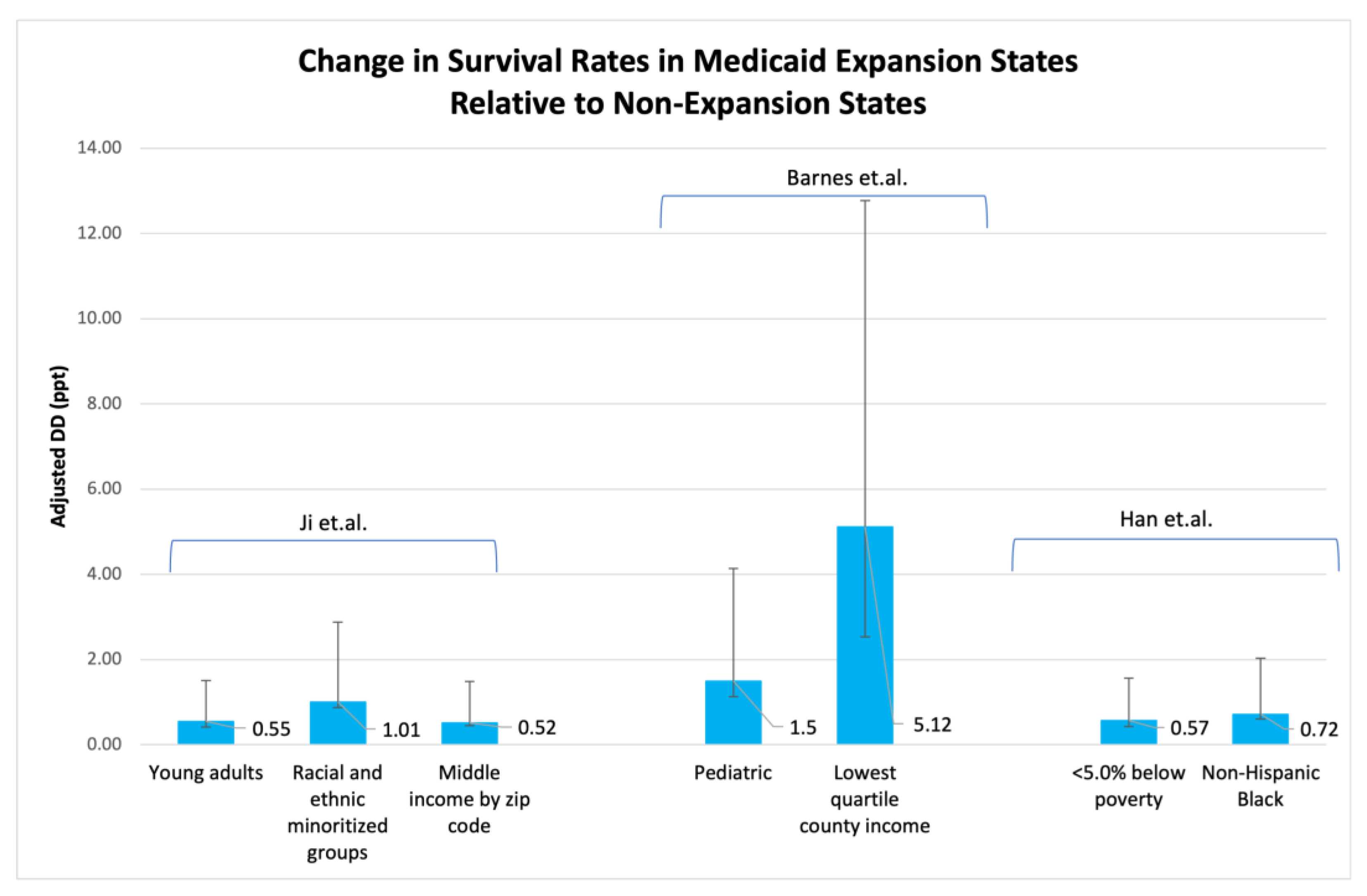
6.3. Positive Health Outcomes
7. Limitations, Gaps, and Future Directions
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoffman, E.D.J.; Klees, B.S.; Curtis, C.A. Overview of the Medicare and Medicaid Programs. Health Care Financ. Rev. 2000, 22, 175–193. [Google Scholar] [PubMed]
- Health Insurance Coverage: 2000. Available online: https://www2.census.gov/library/publications/2001/demographics/p60-215.pdf (accessed on 4 May 2023).
- Health Insurance Coverage: Early Release of Estimates From the National Health Interview Survey. 2009. Available online: https://www.cdc.gov/nchs/data/nhis/earlyrelease/insur201006.pdf (accessed on 4 May 2023).
- Affordable Care Act. Available online: https://www.healthaffairs.org/topic/4#:~:text=ThepurposeoftheACA,curbrisinghealthcarecosts (accessed on 4 May 2023).
- Lyon, S.M.; Douglas, I.S.; Cooke, C.R. Medicaid Expansion under the Affordable Care Act. Implications for Insurance-related Disparities in Pulmonary, Critical Care, and Sleep. Ann. Am. Thorac. Soc. 2014, 11, 661–667. [Google Scholar] [CrossRef] [PubMed]
- Sindhu, K.K.; Alker, J.C.; Adashi, E.Y. The Children’s Health Insurance Program at 25: The Road Ahead. JAMA 2022, 327, 2185–2186. [Google Scholar] [CrossRef]
- Crowley, R.A.; Golden, W. Health Policy Basics: Medicaid Expansion. Ann. Intern. Med. 2014, 160, 423–425. [Google Scholar] [CrossRef] [PubMed]
- Carman, K.G.; Eibner, C.; Paddock, S.M. Trends In Health Insurance Enrollment, 2013–2015. Health Aff. 2015, 34, 1044–1048. [Google Scholar] [CrossRef] [PubMed]
- State and Federal Spending under the ACA. Available online: https://www.macpac.gov/subtopic/state-and-federal-spending-under-the-aca/ (accessed on 4 May 2023).
- Program History. Available online: https://www.medicaid.gov/about-us/program-history/index.html (accessed on 4 May 2023).
- Status of State Medicaid Expansion Decisions: Interactive Map. Available online: https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/ (accessed on 4 May 2023).
- H.R.1319—117th Congress (2021–2022). Available online: https://www.congress.gov/bill/117th-congress/house-bill/1319 (accessed on 4 May 2023).
- New Incentive for States to Adopt the ACA Medicaid Expansion: Implications for State Spending. Available online: https://www.kff.org/medicaid/issue-brief/new-incentive-for-states-to-adopt-the-aca-medicaid-expansion-implications-for-state-spending/ (accessed on 4 May 2023).
- 100% FMAP for LTSS—Educate Your State. Available online: https://www.cms.gov/outreach-and-education/american-indian-alaska-native/aian/ltss-ta-center/info/100-percent-fmap-educate-your-state#:~:text=CMSreimburseseachstatefor,typicallyhaveahigherFMAP (accessed on 4 May 2023).
- Mazurenko, O.; Balio, C.P.; Agarwal, R.; Carroll, A.E.; Menachemi, N. The Effects Of Medicaid Expansion Under The ACA: A Systematic Review. Health Aff. 2018, 37, 944–950. [Google Scholar] [CrossRef]
- Sommers, B.D.; Blendon, R.J.; Orav, E.J.; Epstein, A.M. Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance. JAMA Intern. Med. 2016, 176, 1501–1509. [Google Scholar] [CrossRef]
- Taubman, S.L.; Allen, H.L.; Wright, B.J.; Baicker, K.; Finkelstein, A.N. Medicaid Increases Emergency-Department Use: Evidence from Oregon′s Health Insurance Experiment. Science 2014, 343, 263–268. [Google Scholar] [CrossRef]
- Cole, M.B.; Galarraga, O.; Wilson, I.B.; Wright, B.; Trivedi, A.N. At Federally Funded Health Centers, Medicaid Expansion Was Associated with Improved Quality of Care. Health Aff. 2017, 36, 40–48. [Google Scholar] [CrossRef]
- Sammon, J.D.; Serrell, E.C.; Karabon, P.; Leow, J.; Abdollah, F.; Weissman, J.S.; Han, P.K.; Hansen, M.; Menon, M.; Trinh, Q.-D. Prostate Cancer Screening in Early Medicaid Expansion States. J. Urol. 2018, 199, 81–88. [Google Scholar] [CrossRef]
- Charles, E.J.; Johnston, L.E.; Herbert, M.A.; Mehaffey, J.H.; Yount, K.W.; Likosky, D.S.; Theurer, P.F.; Fonner, C.E.; Rich, J.B.; Speir, A.M.; et al. Impact of Medicaid Expansion on Cardiac Surgery Volume and Outcomes. Ann. Thorac. Surg. 2017, 104, 1251–1258. [Google Scholar] [CrossRef] [PubMed]
- McMorrow, S.; Gates, J.A.; Long, S.K.; Kenney, G.M. Medicaid Expansion Increased Coverage, Improved Affordability, And Reduced Psychological Distress For Low-Income Parents. Health Aff. 2017, 36, 808–818. [Google Scholar] [CrossRef] [PubMed]
- Simon, K.; Soni, A.; Cawley, J. The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions. J. Policy Anal. Manag. 2017, 36, 390–417. [Google Scholar] [CrossRef] [PubMed]
- Blavin, F. Association Between the 2014 Medicaid Expansion and US Hospital Finances. JAMA 2016, 316, 1475–1483. [Google Scholar] [CrossRef] [PubMed]
- Bazzoli, G.J. Effects of Expanded California Health Coverage on Hospitals: Implications for ACA Medicaid Expansions. Health Serv. Res. 2016, 51, 1368–1387. [Google Scholar] [CrossRef]
- Sommers, B.D.; Gruber, J. Federal Funding Insulated State Budgets From Increased Spending Related To Medicaid Expansion. Health Aff. 2017, 36, 938–944. [Google Scholar] [CrossRef]
- Chen, J.; Vargas-Bustamante, A.; Mortensen, K.; Ortega, A.N. Racial and Ethnic Disparities in Health Care Access and Utilization Under the Affordable Care Act. Med. Care 2016, 54, 140–146. [Google Scholar] [CrossRef]
- Han, X.; Yabroff, K.R.; Ward, E.; Brawley, O.W.; Jemal, A. Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act. JAMA Oncol. 2018, 4, 1713–1720. [Google Scholar] [CrossRef]
- Kehl, K.L.; Fullmer, C.P.; Fu, S.; George, G.C.; Hess, K.R.; Janku, F.; Karp, D.D.; Kato, S.; Kizer, C.K.; Kurzrock, R.; et al. Insurance Clearance for Early-Phase Oncology Clinical Trials Following the Affordable Care Act. Clin. Cancer Res. 2017, 23, 4155–4162. [Google Scholar] [CrossRef]
- Mackay, C.B.; Antonelli, K.R.; Bruinooge, S.S.; Onge, J.M.S.; Ellis, S.D. Insurance denials for cancer clinical trial participation after the Affordable Care Act mandate. Cancer 2017, 123, 2893–2900. [Google Scholar] [CrossRef]
- Takvorian, S.U.; Oganisian, A.; Mamtani, R.; Mitra, N.; Shulman, L.N.; Bekelman, J.E.; Werner, R.M. Association of Medicaid Expansion Under the Affordable Care Act With Insurance Status, Cancer Stage, and Timely Treatment Among Patients With Breast, Colon, and Lung Cancer. JAMA Netw. Open 2020, 3, e1921653. [Google Scholar] [CrossRef]
- Patel, K.B.; Shabani, S.; Padhya, T.; Cao, B.; Wang, X.; Turner, K.; Nichols, A.C.; Kang, S.Y.; Rocco, J.W.; Old, M. The Impact of the Affordable Care Act on Insurance Coverage and Stage Among Head and Neck Squamous Cell Carcinoma Patients. J. Health Care Poor Underserved 2022, 33, 1322–1336. [Google Scholar] [CrossRef]
- Albright, B.B.; Nasioudis, D.; Craig, S.; Moss, H.A.; Latif, N.A.; Ko, E.M.; Haggerty, A.F. Impact of Medicaid expansion on women with gynecologic cancer: A difference-in-difference analysis. Am. J. Obstet. Gynecol. 2020, 224, 195.e1–195.e17. [Google Scholar] [CrossRef] [PubMed]
- Lima, H.A.; Moazzam, Z.; Endo, Y.; Alaimo, L.; Diaz, A.; Woldesenbet, S.; Shaikh, C.; Munir, M.M.; Azap, L.E.; Yang, J.; et al. Impact of the Affordable Care Act on Presentation, Treatment, and Outcomes of Intrahepatic Cholangiocarcinoma. J. Gastrointest. Surg. 2023, 27, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Elshami, M.; Hoehn, R.; Hue, J.J.; Rothermel, L.; Chavin, K.D.; Ammori, J.B.; Hardacre, J.M.; Winter, J.M.; Ocuin, L.M. Medicaid expansion is associated with a higher likelihood of early diagnosis, resection, transplantation, and overall survival in patients with hepatocellular carcinoma. HPB 2022, 24, 1482–1491. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Sandilos, G.; Henry, O.; Sensenig, R.; Gaughan, J.; Spitz, F.; Atabek, U.; Hong, Y. Medicaid expansion is associated with earlier diagnosis of gastric cancer. Am. J. Surg. 2022, 224, 539–545. [Google Scholar] [CrossRef]
- Michel, K.F.; Spaulding, A.; Jemal, A.; Yabroff, K.R.; Lee, D.J.; Han, X. Associations of Medicaid Expansion With Insurance Coverage, Stage at Diagnosis, and Treatment Among Patients With Genitourinary Malignant Neoplasms. JAMA Netw. Open 2021, 4, e217051. [Google Scholar] [CrossRef]
- Hoehn, R.S.; Rieser, C.J.; Phelos, H.; Sabik, L.M.; Nassour, I.; Khan, S.; Kaltenmeier, C.; Paniccia, A.; Zureikat, A.H.; Tohme, S.T. Medicaid expansion and the management of pancreatic cancer. J. Surg. Oncol. 2021, 124, 324–333. [Google Scholar] [CrossRef]
- Straker, R.J., III.; Song, Y.; Shannon, A.B.; Chu, E.Y.; Miura, J.T.; Ming, M.E.; Karakousis, G.C. Association of the Affordable Care Act′s Medicaid expansion with the diagnosis and treatment of clinically localized melanoma: A National Cancer Database study. J. Am. Acad. Dermatol. 2021, 84, 1628–1635. [Google Scholar] [CrossRef]
- Chavez-MacGregor, M.; Lei, X.; Malinowski, C.; Zhao, H.; Shih, Y.-C.; Giordano, S.H. Medicaid expansion, chemotherapy delays, and racial disparities among women with early-stage breast cancer. J. Natl. Cancer Inst. 2023, 115, 644–651. [Google Scholar] [CrossRef]
- Sineshaw, H.M.; Ellis, M.A.; Yabroff, K.R.; Han, X.; Jemal, A.; Day, T.A.; Graboyes, E.M. Association of Medicaid Expansion Under the Affordable Care Act With Stage at Diagnosis and Time to Treatment Initiation for Patients With Head and Neck Squamous Cell Carcinoma. JAMA Otolaryngol.-Head Neck Surg. 2020, 146, 247–255. [Google Scholar] [CrossRef]
- Adamson, B.J.; Cohen, A.B.; Gross, C.P.; Estévez, M.; Magee, F.-B.K.; Williams, B.E.; Meropol, N.J.; Davidoff, A.J. ACA Medicaid expansion association with racial disparity reductions in timely cancer treatment. Am. J. Manag. Care 2021, 27, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Sharon, C.E.; Song, Y.; Straker, R.J.; Kelly, N.; Shannon, A.B.; Kelz, R.R.; Mahmoud, N.N.; Saur, N.M.; Miura, J.T.; Karakousis, G.C. Impact of the affordable care act′s medicaid expansion on presentation stage and perioperative outcomes of colorectal cancer. J. Surg. Oncol. 2022, 126, 1471–1480. [Google Scholar] [CrossRef] [PubMed]
- Khan, H.; Cherla, D.; Mehari, K.; Tripathi, M.; Butler, T.W.; Crook, E.D.; Heslin, M.J.; Johnston, F.M.; Fonseca, A.L. Palliative Therapies in Metastatic Pancreatic Cancer: Does Medicaid Expansion Make a Difference? Ann. Surg. Oncol. 2023, 30, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Moyers, J.T.; Patel, A.; Shih, W.; Nagaraj, G. Association of Sociodemographic Factors With Immunotherapy Receipt for Metastatic Melanoma in the US. JAMA Netw. Open 2020, 3, e2015656. [Google Scholar] [CrossRef]
- Le Blanc, J.; Golshan, M.; Lannin, D.; Greenup, R.; Berger, E.R.; Saridakis, A.; Horowitz, N.; Zanieski, G.; Avraham, T.; Mastrioanni, M.; et al. Association of Medicaid Expansion with Post-mastectomy Reconstruction Rates. Ann. Surg. Oncol. 2022, 29, 2181–2189. [Google Scholar] [CrossRef]
- Bailey, S.R.; Voss, R.; Angier, H.; Huguet, N.; Marino, M.; Valenzuela, S.H.; Chung-Bridges, K.; DeVoe, J.E. Affordable Care Act Medicaid expansion and access to primary-care based smoking cessation assistance among cancer survivors: An observational cohort study. BMC Health Serv. Res. 2022, 22, 488. [Google Scholar] [CrossRef]
- Fillon, M. Medicaid expansion increases survival for patients with cancer. CA A Cancer J. Clin. 2022, 72, 407–408. [Google Scholar] [CrossRef]
- Han, X.; Zhao, J.; Yabroff, K.R.; Johnson, C.J.; Jemal, A. Association Between Medicaid Expansion Under the Affordable Care Act and Survival Among Newly Diagnosed Cancer Patients. J. Natl. Cancer Inst. 2022, 114, 1176–1185. [Google Scholar] [CrossRef]
- Huepenbecker, S.P.; Fu, S.; Sun, C.C.; Zhao, H.; Primm, K.M.; Giordano, S.H.; Meyer, L.A. Medicaid Expansion and Postoperative Mortality in Women with Gynecologic Cancer: A Difference-in-Difference Analysis. Ann. Surg. Oncol. 2023, 30, 1508–1519. [Google Scholar] [CrossRef]
- Malinowski, C.; Lei, X.; Zhao, H.; Giordano, S.H.; Chavez-MacGregor, M. Association of Medicaid Expansion With Mortality Disparity by Race and Ethnicity Among Patients With De Novo Stage IV Breast Cancer. JAMA Oncol. 2022, 8, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.J.M.B.; Applebaum, J.; Fader, A.N. Association of the Affordable Care Act's Medicaid Expansion With 1-Year Survival Among Patients With Ovarian Cancer. Obstet. Gynecol. 2022, 139, 1123–1129. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.; O’guinn, M.D.; Zipprer, E.D.; Hsieh, J.C.M.; Dardon, A.T.; Raman, S.; Foglia, C.M.M.; Chao, S.Y.M. Impact of Medicaid Expansion on the Diagnosis, Treatment, and Outcomes of Stage II and III Rectal Cancer Patients. J. Am. Coll. Surg. 2022, 234, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, A.L.; Cherla, D.; Kothari, A.N.; Tzeng, C.-W.D.; Heslin, M.J.; Mehari, K.R.; Johnston, F.M.; Tran-Cao, H.S. Association of Medicaid Expansion with Pancreatic Cancer Treatment and Outcomes: Evidence from the National Cancer Database. Ann. Surg. Oncol. 2022, 29, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Barnes, J.M.; Johnson, K.J.; Boakye, E.A.; Schapira, L.; Akinyemiju, T.; Park, E.M.; Graboyes, E.M.; Osazuwa-Peters, N. Early Medicaid Expansion and Cancer Mortality. J. Natl. Cancer Inst. 2021, 113, 1714–1722. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Vazquez, L.; Howard, J.M.; Kenigsberg, A.P.; Singla, N.; Margulis, V.; Bagrodia, A.; Lotan, Y.; Xi, Y.; Woldu, S.L. The early impact of medicaid expansion on urologic malignancies in the United States. Urol. Oncol. Semin. Orig. Investig. 2022, 40, 103.e1–103.e8. [Google Scholar] [CrossRef]
- Barnes, J.M.; Neff, C.; Han, X.; Kruchko, C.; Barnholtz-Sloan, J.S.; Ostrom, Q.T.; Johnson, K.J. The association of Medicaid expansion and pediatric cancer overall survival. J. Natl. Cancer Inst. 2023, 115, 749–752. [Google Scholar] [CrossRef]
- Ji, X.; Shi, K.S.; Mertens, A.C.; Zhao, J.; Yabroff, K.R.; Castellino, S.M.; Han, X. Survival in Young Adults With Cancer Is Associated With Medicaid Expansion Through the Affordable Care Act. J. Clin. Oncol. 2023, 41, 1909–1920. [Google Scholar] [CrossRef]
- Laughlin, A.I.M.; Li, T.M.; Yu, Q.; Wu, X.-C.M.; Yi, Y.; Hsieh, M.-C.P.; Havron, W.M.; Shoup, M.M.; Chu, Q.D.M. Impact of Medicaid Expansion on Breast Cancer Diagnosis and Treatment in Southern States. J. Am. Coll. Surg. 2023, 236, 838–845. [Google Scholar] [CrossRef]
- Barnes, J.M.; Johnson, K.J.; Osazuwa-Peters, N.; Yabroff, K.R.; Chino, F. Changes in cancer mortality after Medicaid expansion and the role of stage at diagnosis. JNCI J. Natl. Cancer Inst. 2023, djad094. [Google Scholar] [CrossRef]
- Manisundaram, N.; Snyder, R.A.; Hu, C.-Y.; DiBrito, S.R.; Chang, G.J. Racial disparities in cancer mortality in patients with gastrointestinal malignancies following Medicaid expansion. J. Clin. Oncol. 2023, 41 (Suppl. 16), 6546. [Google Scholar] [CrossRef]
- Things to Know About Medicaid Managed Care. Available online: https://www.kff.org/medicaid/issue-brief/10-things-to-know-about-medicaid-managed-care/ (accessed on 28 May 2023).
| Cancer Type/Patient Population | Key Findings | Implications of Medicaid Expansion |
|---|---|---|
| Breast cancer [30,39,45,50,58] | ↑ Early-stage diagnoses ↑ 5-year survival ↑ Time to initiation of treatment for Black and Hispanic patients ↓ 2-year mortality gap for stage IV patients ↑ Comprehensive treatment in Southern states ↑ Rates of post-mastectomy breast reconstruction | Earlier detection, improved diagnosis and survival, faster treatment initiation, expanded treatment options |
| HNSCC Non-oropharyngeal HNSCC [31,40] | ↑ Early-stage diagnoses ↑ Time to initiation of treatment for non-oropharyngeal HNSCC | Earlier detection, faster treatment initiation |
| Colorectal cancer [42] | ↑ Early-stage diagnoses ↑ Perioperative outcomes | Earlier detection, improved surgical outcomes |
| Hepatocellular carcinoma [34] | ↑ Early-stage diagnoses | Earlier detection |
| Gastric cancer [35] | ↑ Early-stage diagnoses | Earlier detection |
| Kidney cancer [36] | ↑ Early-stage diagnoses | Earlier detection |
| Pancreatic cancer [37,53,54] | ↑ Early-stage diagnoses ↑ survival benefit | Earlier detection, improved survival rates |
| Intrahepatic cholangiocarcinoma [33] | ↑ Surgical treatment | Increased treatment accessibility |
| Rectal cancer [52] | ↓ 90-day mortality | Improved short-term survival |
| Gynecologic cancer (ovarian and endometrial) [32,49,51] | ↑ Time to initiation of treatment ↑ Post-operative survival and 1-year survival due to earlier diagnoses for ovarian cancer | Faster treatment initiation, improved post-operative outcomes, improved early detection and survival |
| Genitourinary cancers [55] | No impact on diagnosis stage or survival rates | No significant impact |
| Melanoma [38,44] | ↑ Early-stage diagnoses ↑ Receipt of therapies such as immunotherapy | Earlier detection, expanded treatment options |
| All cancer sites [47,48,59] | ↑ In prognosis for specific cancer types ↓ Rates of distant stage cancer diagnoses and cancer death | Improved prognosis, improved diagnosis, and reduced mortality |
| Gastrointestinal cancers (Black individuals) [60] | ↓ In 2-year mortality rates | Improved survival rates |
| Advanced/Metastatic cancers [41,43] | ↓ Black–White racial disparities in treatment ↑ Receipt of timely systemic treatment | Decreased racial disparities, expanded treatment options |
| Cancer survivors [46] | ↑ Access to smoking cessation assistance | Improved preventive care access |
| Pediatric and young adults [56,57] | Survival benefits | Improved survival rates |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hotca, A.; Bloom, J.R.; Runnels, J.; Salgado, L.R.; Cherry, D.R.; Hsieh, K.; Sindhu, K.K. The Impact of Medicaid Expansion on Patients with Cancer in the United States: A Review. Curr. Oncol. 2023, 30, 6362-6373. https://doi.org/10.3390/curroncol30070469
Hotca A, Bloom JR, Runnels J, Salgado LR, Cherry DR, Hsieh K, Sindhu KK. The Impact of Medicaid Expansion on Patients with Cancer in the United States: A Review. Current Oncology. 2023; 30(7):6362-6373. https://doi.org/10.3390/curroncol30070469
Chicago/Turabian StyleHotca, Alexandra, Julie R. Bloom, Juliana Runnels, Lucas Resende Salgado, Daniel R. Cherry, Kristin Hsieh, and Kunal K. Sindhu. 2023. "The Impact of Medicaid Expansion on Patients with Cancer in the United States: A Review" Current Oncology 30, no. 7: 6362-6373. https://doi.org/10.3390/curroncol30070469
APA StyleHotca, A., Bloom, J. R., Runnels, J., Salgado, L. R., Cherry, D. R., Hsieh, K., & Sindhu, K. K. (2023). The Impact of Medicaid Expansion on Patients with Cancer in the United States: A Review. Current Oncology, 30(7), 6362-6373. https://doi.org/10.3390/curroncol30070469





