Anaesthetic Techniques and Strategies: Do They Influence Oncological Outcomes?
Abstract
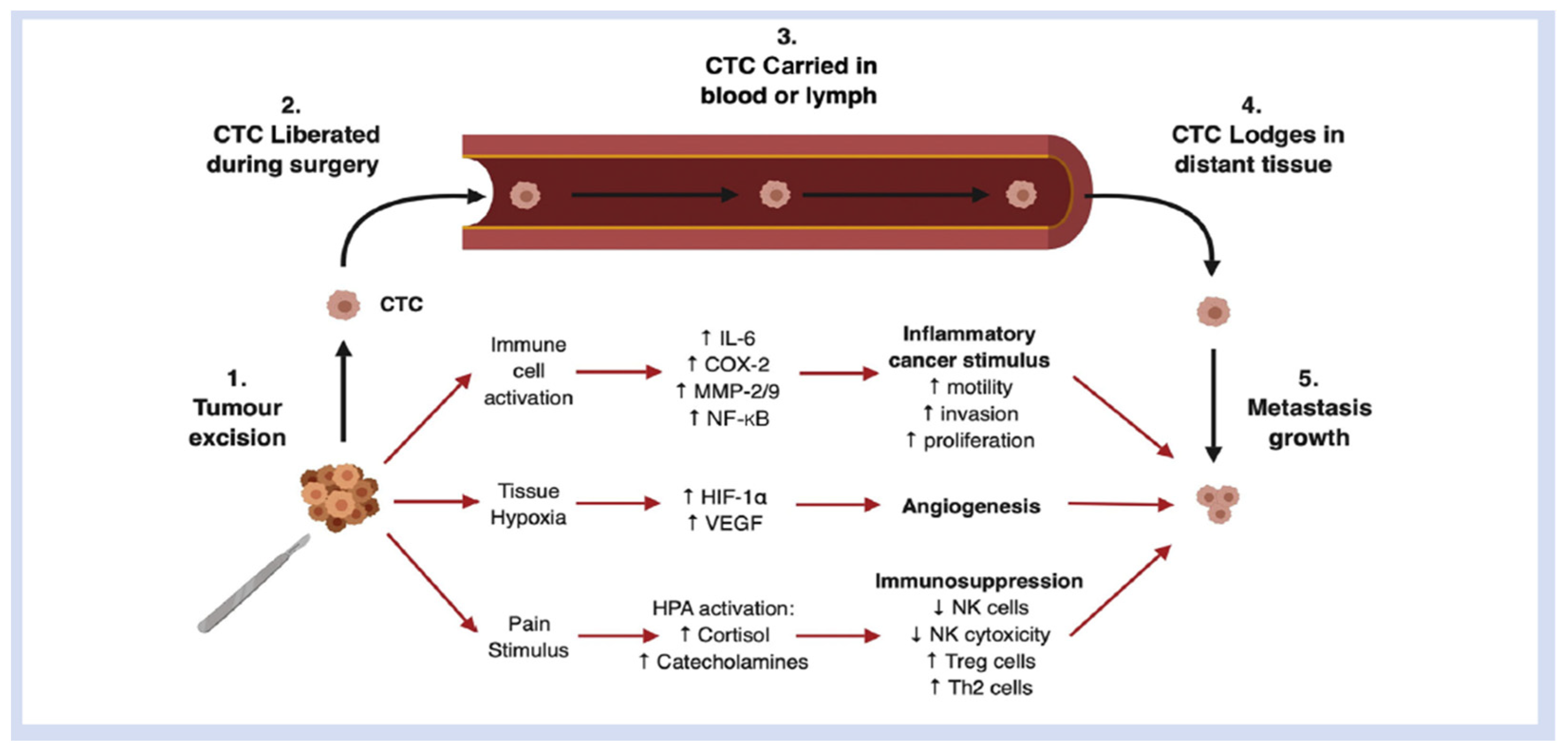
1. Introduction
2. Opioids
3. Regional Anaesthesia Techniques
4. Propofol Total Intravenous Anaesthesia (TIVA) and Volatile Anaesthesia
5. Dexamethasone
6. Dexmedetomidine
7. NSAIDs/COX 2 Inhibitors and Beta Blockers
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Global Burden of Disease 2019 Cancer Collaboration; Kocarnik, J.M.; Compton, K.; Dean, F.E.; Fu, W.; Gaw, B.L.; Harvey, J.D.; Henrikson, H.J.; Lu, D.; Pennini, A.; et al. Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups from 2010 to 2019. JAMA Oncol. 2021, 8, 420–444. [Google Scholar] [CrossRef]
- Foreman, K.J.; Marquez, N.; Dolgert, A.; Fukutaki, K.; Fullman, N.; McGaughey, M.; Pletcher, M.A.; Smith, A.E.; Tang, K.; Yuan, C.-W.; et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: Reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet 2018, 392, 2052–2090. Available online: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31694-5/fulltext (accessed on 5 January 2023). [CrossRef]
- Moorthy, A.; Eochagáin, A.N.; Buggy, D.J. Can Acute Postoperative Pain Management After Tumour Resection Surgery Modulate Risk of Later Recurrence or Metastasis? Front. Oncol. 2021, 11, 802592. [Google Scholar] [CrossRef] [PubMed]
- Murphy, O.; Forget, P.; Ma, D.; Buggy, D.J. Anesthetic technique and cancer surgery outcomes. Br. J. Anaesth. 2023, in press. [Google Scholar]
- Wall, T.; Sherwin, A.; Ma, D.; Buggy, D. Influence of perioperative anaesthetic and analgesic interventions on oncological outcomes: A narrative review. Br. J. Anaesth. 2019, 123, 135–150. [Google Scholar] [CrossRef] [PubMed]
- Efrimescu, C.I.; Buggy, P.M.; Buggy, D.J. Neutrophil Extracellular Trapping Role in Cancer, Metastases, and Cancer-Related Thrombosis: A Narrative Review of the Current Evidence Base. Curr. Oncol. Rep. 2021, 23, 118. [Google Scholar] [CrossRef] [PubMed]
- Buggy, D.; Freeman, J.; Johnson, M.; Leslie, K.; Riedel, B.; Sessler, D.; Kurz, A.; Gottumukkala, V.; Short, T.; Pace, N.; et al. Systematic review and consensus definitions for standardised endpoints in perioperative medicine: Postoperative cancer outcomes. Br. J. Anaesth. 2018, 121, 38–44. [Google Scholar] [CrossRef]
- Boland, J.W.; Pockley, A. Influence of opioids on immune function in patients with cancer pain: From bench to bedside. Br. J. Pharmacol. 2017, 175, 2726–2736. [Google Scholar] [CrossRef]
- Li, H.; Ma, Z.; Lei, Y. The expression of kappa-opioid receptor promotes the migration of breast cancer cells in vitro. BMC Anesthesiol. 2021, 21, 210. Available online: https://pubmed.ncbi.nlm.nih.gov/34461834/ (accessed on 5 January 2023). [CrossRef]
- Zylla, D.; Gourley, B.L.; Vang, D.; Jackson, S.; Boatman, S.; Lindgren, B.; Kuskowski, M.A.; Le, C.; Gupta, K.; Gupta, P. Opioid requirement, opioid receptor expression, and clinical outcomes in patients with advanced prostate cancer. Cancer 2013, 119, 4103–4110. [Google Scholar] [CrossRef]
- Mincer, J.S.; Buggy, D.J. Anaesthesia, analgesia, and cancer outcomes: Time to think like oncologists? Br. J. Anaesth. 2023. [Google Scholar] [CrossRef] [PubMed]
- Belltall, A.; Zúñiga-Trejos, S.; Garrido-Cano, I.; Eroles, P.; Argente-Navarro, M.P.; Buggy, D.J.; Díaz-Cambronero, O.; Mazzinari, G. Solid Tumor Opioid Receptor Expression and Oncologic Outcomes: Analysis of the Cancer Genome Atlas and Genotype Tissue Expression Project. Front. Oncol. 2022, 12, 801411. [Google Scholar] [CrossRef] [PubMed]
- Belltall, A.; Mazzinari, G.; Garrido-Cano, I.; Giner, F.; Marí, A.M.; Eroles, P.; Argente-Navarro, M.P.; Cata, J.P.; Diaz-Cambronero, O. Opioid Receptor Expression in Colorectal Cancer: A Nested Matched Case-Control Study. Front. Oncol. 2022, 12, 801714. [Google Scholar] [CrossRef] [PubMed]
- Rangel, F.P.; Auler Jr, J.O.; Carmona, M.J.; Cordeiro, M.D.; Nahas, W.C.; Coelho, R.F.; Simões, C.M. Opioids and premature biochemical recurrence of prostate cancer: A randomised prospective clinical trial. Br. J. Anaesth. 2021, 126, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Yuval, J.B.; Lee, J.; Wu, F.; Thompson, H.M.; Verheij, F.S.; Gupta, H.V.; Irie, T.; Scarpa, J.R.; McCormick, P.J.; Smith, J.J.; et al. Intraoperative opioids are associated with decreased recurrence rates in colon adenocarcinoma: A retrospective observational cohort study. Br. J. Anaesth. 2022, 129, 172–181. [Google Scholar] [CrossRef]
- Montagna, G.; Gupta, H.V.; Hannum, M.; Tan, K.S.; Lee, J.; Scarpa, J.R.; Plitas, G.; Irie, T.; McCormick, P.J.; Fischer, G.W.; et al. Intraoperative opioids are associated with improved recurrence-free survival in triple-negative breast cancer. Br. J. Anaesth. 2021, 126, 367–376. [Google Scholar] [CrossRef]
- Wu, H.-L.; Tai, Y.-H.; Chang, K.-Y.; Lin, S.-P. Dose-dependent association between morphine requirement and mortality risk after resection for hepatocellular carcinoma. Eur. J. Anaesthesiol. 2021, 38, 548–550. [Google Scholar] [CrossRef]
- Connolly, J.G.; Tan, K.S.; Mastrogiacomo, B.; Dycoco, J.; Caso, R.; Jones, G.D.; McCormick, P.J.; Sanchez-Vega, F.; Irie, T.; Scarpa, J.R.; et al. Intraoperative opioid exposure, tumour genomic alterations, and survival differences in people with lung adenocarcinoma. Br. J. Anaesth. 2021, 127, 75–84. [Google Scholar] [CrossRef]
- Li, T.; Meng, X.; Di Wang, D.; Wang, Q.; Ma, J.; Dai, Z. Regional anesthesia did not improve postoperative long-term survival of tumor patients: A systematic review and meta-analysis of randomized controlled trials. World J. Surg. Oncol. 2023, 21, 68. [Google Scholar] [CrossRef]
- Dockrell, L.; Buggy, D.J. The role of regional anaesthesia in the emerging subspecialty of onco-anaesthesia: A state-of-the-art review. Anaesthesia 2021, 76 (Suppl. 1), 148–159. [Google Scholar] [CrossRef]
- Hasselager, R.P.; Hallas, J.; Gögenur, I. Epidural Analgesia and Recurrence after Colorectal Cancer Surgery: A Danish Retrospective Registry-based Cohort Study. Anesthesiology 2022, 136, 459–471. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.-J.; Hsu, F.-K.; Shyr, Y.-M.; Ni, Y.-W.; Tsou, M.-Y.; Chang, K.-Y. Effect of epidural analgesia on long-term outcomes after curative surgery for pancreatic cancer. J. Chin. Med. Assoc. 2021. Publish Ahead of Print. [Google Scholar] [CrossRef] [PubMed]
- Sessler, D.I.; Pei, L.; Huang, Y.; Fleischmann, E.; Marhofer, P.; Kurz, A.; Mayers, D.B.; Meyer-Treschan, T.A.; Grady, M.; Tan, E.Y.; et al. Recurrence of breast cancer after regional or general anaesthesia: A randomised controlled trial. Lancet 2019, 394, 1807–1815. [Google Scholar] [CrossRef]
- Falk, W.; Magnuson, A.; Eintrei, C.; Henningsson, R.; Myrelid, P.; Matthiessen, P.; Gupta, A. Comparison between epidural and intravenous analgesia effects on disease-free survival after colorectal cancer surgery: A randomised multicentre controlled trial. Br. J. Anaesth. 2021, 127, 65–74. Available online: https://pubmed.ncbi.nlm.nih.gov/33966891/ (accessed on 5 January 2023). [CrossRef] [PubMed]
- Hayden, J.M.; Oras, J.; Block, L.; Thörn, S.-E.; Palmqvist, C.; Salehi, S.; Nordstrom, J.L.; Gupta, A. Intraperitoneal ropivacaine reduces time interval to initiation of chemotherapy after surgery for advanced ovarian cancer: Randomised controlled double-blind pilot study. Br. J. Anaesth. 2020, 124, 562–570. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.T.; Li, Y.W.; Zhao, B.J.; Guo, X.Y.; Feng, Y.; Zuo, M.Z.; Fu, C.; Zhou, W.-J.; Li, H.-J.; Liu, Y.-F.; et al. Long-term Survival after Combined Epidural–General Anesthesia or General Anesthesia Alone: Follow-up of a Randomized Trial. Anesthesiology 2021, 135, 233–245. [Google Scholar] [CrossRef]
- Xu, Z.-Z.; Li, H.-J.; Li, M.-H.; Huang, S.-M.; Li, X.; Liu, Q.-H.; Li, J.; Wang, D.-X.; Sessler, D.I. Epidural Anesthesia–Analgesia and Recurrence-free Survival after Lung Cancer Surgery: A Randomized Trial. Anesthesiology 2021, 135, 419–432. [Google Scholar] [CrossRef]
- Melamed, R.; Bar-Yosef, S.; Shakhar, G.; Shakhar, K.; Ben-Eliyahu, S. Suppression of Natural Killer Cell Activity and Promotion of Tumor Metastasis by Ketamine, Thiopental, and Halothane, but Not by Propofol: Mediating Mechanisms and Prophylactic Measures. Obstet. Anesth. Dig. 2003, 97, 1331–1339. [Google Scholar] [CrossRef]
- Wigmore, T.J.; Mohammed, K.; Jhanji, S. Long-term Survival for Patients Undergoing Volatile versus IV Anesthesia for Cancer Surgery. Anesthesiology 2016, 124, 69–79. Available online: https://anesthesiology.pubs.asahq.org/article.aspx?articleid=2470470 (accessed on 5 January 2023). [CrossRef]
- Buggy, D.J.; Riedel, B.; Sessler, D.I. Can anaesthetic technique influence cancer outcome? The next steps…. Br. J. Anaesth. 2021, 127, 5–7. [Google Scholar] [CrossRef]
- Hovaguimian, F.; Braun, J.; Z’graggen, B.R.; Schläpfer, M.; Dumrese, C.; Ewald, C.; Dedes, K.J.; Fink, D.; Rölli, U.; Seeberger, M.; et al. Anesthesia and Circulating Tumor Cells in Primary Breast Cancer Patients. Anesthesiology 2020, 133, 548–558. Available online: https://pubs.asahq.org/anesthesiology/article/133/3/548/108244/Anesthesia-and-Circulating-Tumor-Cells-in-Primary (accessed on 5 January 2023). [CrossRef] [PubMed]
- Oh, C.-S.; Park, H.-J.; Piao, L.; Sohn, K.-M.; Koh, S.-E.; Hwang, D.-Y.; Kim, S.-H. Expression Profiles of Immune Cells after Propofol or Sevoflurane Anesthesia for Colorectal Cancer Surgery: A Prospective Double-blind Randomized Trial. Anesthesiology 2022, 136, 448–458. [Google Scholar] [CrossRef] [PubMed]
- Aghamelu, O.; Buggy, P.; Smith, G.; Inzitari, R.; Wall, T.; Buggy, D.J. Serum NETosis expression and recurrence risk after regional or volatile anaesthesia during breast cancer surgery: A pilot, prospective, randomised single-blind clinical trial. Acta Anaesthesiol. Scand. 2020, 65, 313–319. [Google Scholar] [CrossRef]
- Enlund, M. Is It Definitely Clear That Long-Term Survival after Breast Cancer Surgery Is Not Affected by Anaesthetics? Cancers 2021, 13, 3390. [Google Scholar] [CrossRef] [PubMed]
- Cook, A.M.; McDonnell, A.M.; Lake, R.A.; Nowak, A.K. Dexamethasone co-medication in cancer patients undergoing chemotherapy causes substantial immunomodulatory effects with implications for chemo-immunotherapy strategies. OncoImmunology 2015, 5, e1066062. [Google Scholar] [CrossRef]
- Pang, J.M.; Huang, Y.-C.; Sun, S.-P.; Pan, Y.-R.; Shen, C.-Y.; Kao, M.-C.; Wang, R.-H.; Wang, L.-H.; Lin, K.-T. Effects of synthetic glucocorticoids on breast cancer progression. Steroids 2020, 164, 108738. Available online: https://pubmed.ncbi.nlm.nih.gov/33065150/ (accessed on 5 January 2023). [CrossRef]
- Kim, M.H.; Kim, D.W.; Park, S.; Kim, J.H.; Lee, K.Y.; Hwang, J.; Yoo, Y.C. Single dose of dexamethasone is not associated with postoperative recurrence and mortality in breast cancer patients: A propensity-matched cohort study. BMC Cancer 2019, 19, 251. [Google Scholar] [CrossRef]
- Newhook, T.E.; Soliz, J.M.; Prakash, L.R.; Hancher-Hodges, S.; Do, B.B.S.; Wilks, J.A.; Ikoma, N.; Kim, M.P.; Lee, J.E.; Katz, M.H.G.; et al. Impact of Intraoperative Dexamethasone on Surgical and Oncologic Outcomes for Patients with Resected Pancreatic Ductal Adenocarcinoma. Ann. Surg. Oncol. 2020, 28, 1563–1569. [Google Scholar] [CrossRef]
- Mao, S.; Wu, Y.; Wang, R.; Guo, Y.; Yuan, J.; Zhang, W.; Zhang, J.; Yan, Y.; Yao, X. Association between perioperative glucocorticoids and cancer metastasis and survival in patients undergoing radical cystectomy for urothelial carcinoma of the bladder: A single-center retrospective study. Investig. Clin. Urol. 2020, 61, 382–389. [Google Scholar] [CrossRef]
- Blank, M.C.; Katsiampoura, A.M.; Wachtendorf, L.J.C.; Linhardt, F.C.C.; Tartler, T.M.C.; Raub, D.; Azimaraghi, O.; Chen, G.; Houle, T.T.; Ferrone, C.; et al. Association Between Intraoperative Dexamethasone and Postoperative Mortality in Patients Undergoing Oncologic Surgery. Ann. Surg. 2022. Publish Ahead of Print. [Google Scholar] [CrossRef]
- Poon, W.H.; Ling, R.R.; Yang, I.X.; Luo, H.; Kofidis, T.; MacLaren, G.; Tham, C.; Teoh, K.L.K.; Ramanathan, K. Dexmedetomidine for adult cardiac surgery: A systematic review, meta-analysis and trial sequential analysis. Anaesthesia 2023, 78, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.; Kim, K.J.; Hwang, H.J.; Noh, S.; Oh, J.E.; Yoo, Y.-C. Immunomodulatory Effects of Perioperative Dexmedetomidine in Ovarian Cancer: An In Vitro and Xenograft Mouse Model Study. Front. Oncol. 2021, 11, 722743. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.S.; Seon, K.; Kim, M.-Y.; Kim, S.W.; Yoo, Y.C. Effects of Perioperative Dexmedetomidine on Immunomodulation in Uterine Cancer Surgery: A Randomized, Controlled Trial. Front. Oncol. 2021, 11, 749003. [Google Scholar] [CrossRef] [PubMed]
- Xing, M.-W.; Li, C.-J.; Guo, C.; Wang, B.-J.; Mu, D.-L.; Wang, D.-X. Effect of intraoperative dexmedetomidine on long-term survival in older patients after major noncardiac surgery: 3-year follow-up of a randomized trial. J. Clin. Anesth. 2023, 86, 111068. [Google Scholar] [CrossRef]
- Bosch, D.J.; Nieuwenhuijs-Moeke, G.J.; van Meurs, M.; Abdulahad, W.H.; Struys, M.M.R.F. Immune Modulatory Effects of Nonsteroidal Anti-inflammatory Drugs in the Perioperative Period and Their Consequence on Postoperative Outcome. Anesthesiology 2022, 136, 843–860. [Google Scholar] [CrossRef]
- Hashemi Goradel, N.; Najafi, M.; Salehi, E.; Farhood, B.; Mortezaee, K. Cyclooxygenase-2 in cancer: A review. J. Cell. Physiol. 2018, 234, 5683–5699. [Google Scholar] [CrossRef]
- Meyerhardt, J.A.; Shi, Q.; Fuchs, C.S.; Meyer, J.; Niedzwiecki, D.; Zemla, T.; Kumthekar, P.; Guthrie, K.A.; Couture, F.; Kuebler, P.; et al. Effect of Celecoxib vs Placebo Added to Standard Adjuvant Therapy on Disease-Free Survival Among Patients With Stage III Colon Cancer. JAMA 2021, 325, 1277–1286. [Google Scholar] [CrossRef]
- Coombes, R.C.; Tovey, H.; Kilburn, L.; Mansi, J.; Palmieri, C.; Bartlett, J.; Hicks, J.; Makris, A.; Evans, A.; Loibl, S.; et al. Effect of Celecoxib vs Placebo as Adjuvant Therapy on Disease-Free Survival Among Patients With Breast Cancer. JAMA Oncol. 2021, 7, 1291–1301. [Google Scholar] [CrossRef]
- Haldar, R.; Ricon-Becker, I.; Radin, A.; Gutman, M.; Cole, S.W.; Zmora, O.; Ben-Eliyahu, S. Perioperative COX2 and β-adrenergic blockade improves biomarkers of tumor metastasis, immunity, and inflammation in colorectal cancer: A randomized controlled trial. Cancer 2020, 126, 3991–4001. [Google Scholar] [CrossRef]
- Wang, R.; Zhu, J.; Zhu, Y.; Ge, Y.; Xu, G.; Jia, W. Perioperative analgesia with parecoxib sodium improves postoperative pain and immune function in patients undergoing hepatectomy for hepatocellular carcinoma. J. Eval. Clin. Pract. 2019, 26, 992–1000. [Google Scholar] [CrossRef]
- Badwe, R.A.; Parmar, V.; Nair, N.; Joshi, S.; Hawaldar, R.; Pawar, S.; Kadayaprath, G.; Borthakur, B.B.; Thammineedi, S.R.; Pandya, S.; et al. Effect of Peritumoral Infiltration of Local Anesthetic Before Surgery on Survival in Early Breast Cancer. J. Clin. Oncol. 2023. [Google Scholar] [CrossRef] [PubMed]
| Trial Number (Acronym) | Area of Focus | Type of Surgery | Number of Patients | Primary End-Point | Secondary End-Points | Est Year of Completion |
|---|---|---|---|---|---|---|
| NCT01975064 (CAN study) [32] | Propofol vs. Sevoflurane anaesthesia | Breast, Colon, Rectal Cancer surgery | 1700 | Overall Survival (OS) | OS 1 year | 2023 |
| NCT04316013 Volatile anaesthesia and perioperative outcomes related to cancer: The VAPOR-C Trial | 2 × 2 factorial design volatile vs. propofol TIVA; With and without IV lidocaine | Colorectal, non-small cell lung | 3500 | DFS | OS DAH-30 Postop complications | 2028 |
| NCT04449289 | Influence of intravenous lidocaine and peridural ropivacaine | Pancreatic surgery | 100 | 1- and 3-years recurrence rate after surgery | 1- and 3-years survival after surgery, Complication rate after surgery | December 2024 |
| NCT03034096 (GA-CARES) | Propofol vs. volatile anaesthesia | Cancer surgery | 1804 | All-cause mortality | Recurrence free survival, All-cause mortality as a binary outcome | December 2024 |
| NCT04800393 (TeMP) | Inhalation vs. Total Intravenous | Breast Cancer | 130 | NLR (1 h and 24 h) | Levels of multiple immune cells | April 2028 |
| NCT02840227 | Combined General/Regional vs. GA | Lung Cancer | 2000 | Cancer-free survival | Pain intensity, Opioid use | December 2023 |
| NCT04259398 | Propofol vs. Sevoflurane | Colon cancer | 792 | 5-year survival | Five-year RFS, One-year RFS | February 2026 |
| NCT03134430 | Regional Nerve Block on Cancer Recurrence | Gastric, colon, rectal, liver, lung | 400 | RFS | OS | May 2023 |
| NCT04601961 | Propofol vs. Sevoflurane | Colorectal cancer | 220 | HIF-1 gene expression | Number of recurrences, Gene expression (HIF-1, IL-6, TNF-alpha) | March 2024 |
| NCT04493905 (ENCORE) | Effects of anaesthetic techniques | Colorectal cancer | 10,000 | Time to Return to Intended Oncologic Therapy (RIOT) | Postoperative mortality for 0–30 days, Cancer recurrence 90 days, 1, 3- and 5-years | November 2023 |
| NCT04532606 | Remimazolam | Bladder Cancer | 1128 | Incidence of emergence delirium, recurrence free survival | Incidence of postoperative delirium, overall survival | October 2023 |
| NCT05742438 | Dexmedetomidine Infusion, Lidocaine Infusion, and Intrathecal Morphine Injection | Colorectal cancer | 114 | Plasma Matrix metalloproteinase-9 levels | Various immune cell levels | March 2024 |
| NCT05141877 | Propofol vs. sevoflurane | Primary brain tumour | 706 | Overall survival | Presence of disease progression | November 2025 |
| NCT04513808 | Propofol vs. sevoflurane | Oesophageal cancer | 950 | Recurrence free survival | The treatment effect of propofol-based anaesthesia versus volatile anaesthesia | December 2024 |
| NCT05250791 (FLICOR) | Lidocaine | Large bowel cancer | 50 | Feasibility of recruitment | Disease free survival | March 2024 |
| NCT04503148 | Propofol vs. inhalational anaesthesia | Renal Cell | 562 | 1-year metastasis-free survival | 3-year metastasis-free survival, 1-year survival | July 2025 |
| NCT04475705 | Propofol vs. sevoflurane | Paediatric tumour surgery | 100 | Difference in Hypoxia Inducible Factor-1 gene expression | Difference in levels of Interleukin-6/TNF alpha/CRP | July 2028 |
| NCT05484687 | Lidocaine | Colorectal cancer | 100 | Concentration of tumour micro metastasis markers | Concentration of stress hormones/inflammatory factors | December 2023 |
| NCT05663242 | Propofol vs. Sevoflurane | Primary lung cancer | 300 | Overall survival, presence of disease progression | Postoperative complications, hospital length of stay | November 2026 |
| NCT05331911 | Propofol vs. Sevoflurane | Primary Liver cancer | 500 | Overall survival, presence of disease progression | Postoperative complications, hospital length of stay | March 2027 |
| NCT05450055 | Postoperative Intraperitoneal Lidocaine | Ovarian cancer | 60 | Postoperative analgesic use | Survival time, Disease-free survival time | July 2029 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murphy, L.; Shaker, J.; Buggy, D.J. Anaesthetic Techniques and Strategies: Do They Influence Oncological Outcomes? Curr. Oncol. 2023, 30, 5309-5321. https://doi.org/10.3390/curroncol30060403
Murphy L, Shaker J, Buggy DJ. Anaesthetic Techniques and Strategies: Do They Influence Oncological Outcomes? Current Oncology. 2023; 30(6):5309-5321. https://doi.org/10.3390/curroncol30060403
Chicago/Turabian StyleMurphy, Liam, John Shaker, and Donal J. Buggy. 2023. "Anaesthetic Techniques and Strategies: Do They Influence Oncological Outcomes?" Current Oncology 30, no. 6: 5309-5321. https://doi.org/10.3390/curroncol30060403
APA StyleMurphy, L., Shaker, J., & Buggy, D. J. (2023). Anaesthetic Techniques and Strategies: Do They Influence Oncological Outcomes? Current Oncology, 30(6), 5309-5321. https://doi.org/10.3390/curroncol30060403





