Multi-Institutional Patterns of Use of Tumor-Treating Fields for Patients with Malignant Pleural Mesothelioma
Abstract
1. Introduction
2. Materials and Methods
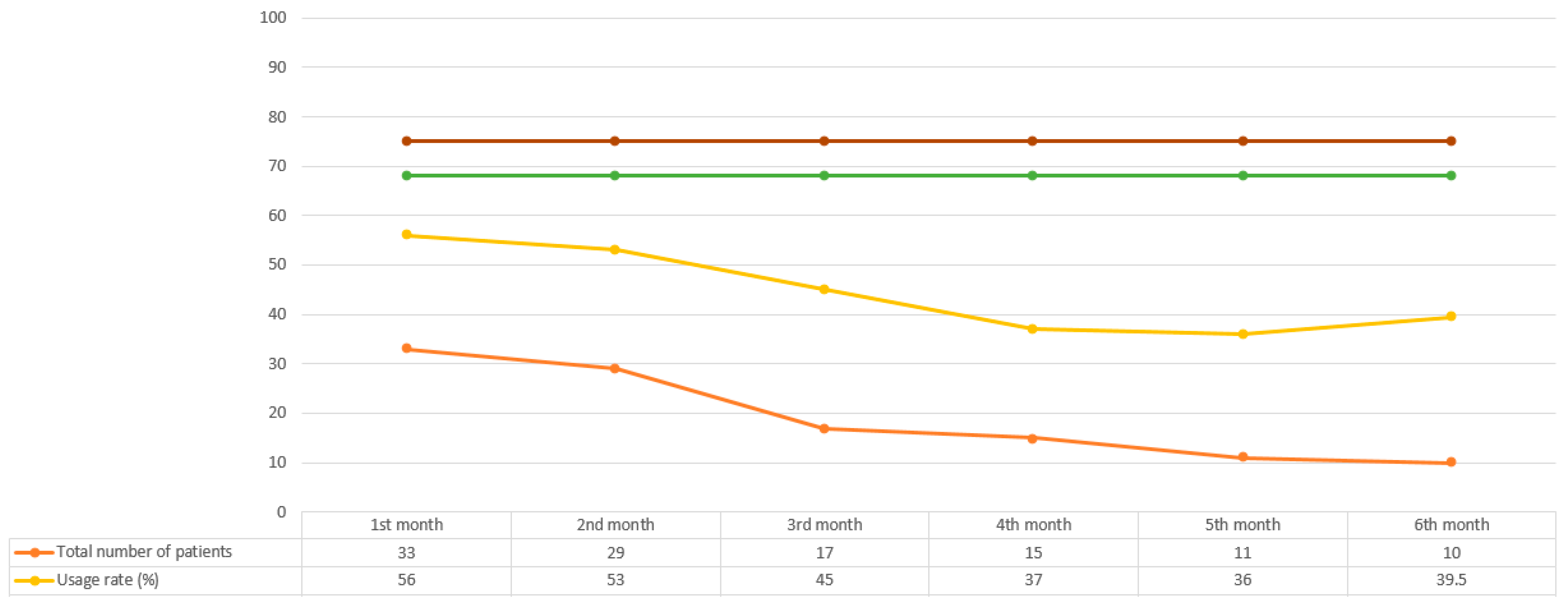
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Toms, S.A.; Kim, C.Y.; Nicholas, G.; Ram, Z. Increased compliance with tumor treating fields therapy is prognostic for improved survival in the treatment of glioblastoma: A subgroup analysis of the EF-14 phase III trial. J. Neurooncol. 2019, 141, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Taillibert, S.; Kanner, A.; Read, W.; Steinberg, D.; Lhermitte, B.; Toms, S.; Idbaih, A.; Ahluwalia, M.S.; Fink, K.; et al. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs Maintenance Temozolomide Alone on Survival in Patients with Glioblastoma: A Randomized Clinical Trial. JAMA 2017, 318, 2306–2316. [Google Scholar] [CrossRef] [PubMed]
- Rivera, F.; Benavides, M.; Gallego, J.; Guillen-Ponce, C.; Lopez-Martin, J.; Kung, M. Tumor treating fields in combination with gemcitabine or gemcitabine plus nab-paclitaxel in pancreatic cancer: Results of the PANOVA phase 2 study. Pancreatology 2019, 19, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Vergote, I.; von Moos, R.; Manso, L.; Van Nieuwenhuysen, E.; Concin, N.; Sessa, C. Tumor Treating Fields in combination with paclitaxel in recurrent ovarian carcinoma: Results of the INNOVATE pilot study. Gynecol. Oncol. 2018, 150, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Pless, M.; Droege, C.; von Moos, R.; Salzberg, M.; Betticher, D. A phase I/II trial of Tumor Treating Fields (TTFields) therapy in combination with pemetrexed for advanced non-small cell lung cancer. Lung Cancer 2013, 81, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Kirson, E.D.; Gurvich, Z.; Schneiderman, R.; Dekel, E.; Itzhaki, A.; Wasserman, Y.; Schatzberger, R.; Palti, Y. Disruption of cancer cell replication by alternating electric fields. Cancer Res. 2004, 64, 3288–3295. [Google Scholar] [CrossRef] [PubMed]
- Giladi, M.; Weinberg, U.; Schneiderman, R.S.; Porat, Y.; Munster, M.; Voloshin, T.; Blatt, R.; Cahal, S.; Itzhaki, A.; Onn, A.; et al. Alternating electric fields (tumor-treating fields therapy) can improve chemotherapy treatment efficacy in non-small cell lung cancer both in vitro and in vivo. Semin. Oncol. 2014, 41 (Suppl. S6), S35–S41. [Google Scholar] [CrossRef] [PubMed]
- Mumblat, H.; Martinez-Conde, A.; Braten, O.; Munster, M.; Dor-On, E.; Schneiderman, R.S.; Porat, Y.; Voloshin, T.; Davidi, S.; Blatt, R.; et al. Tumor Treating Fields (TTFields) downregulate the Fanconi Anemia-BRCA pathway and increase the efficacy of chemotherapy in malignant pleural mesothelioma preclinical models. Lung Cancer 2021, 160, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Ceresoli, G.L.; Aerts, J.G.; Dziadziuszko, R.; Ramlau, R.; Cedres, S.; van Meerbeeck, J.P.; Mencoboni, M.; Planchard, D.; Chella, A.; Crino, L.; et al. Tumour Treating Fields in combination with pemetrexed and cisplatin or carboplatin as first-line treatment for unresectable malignant pleural mesothelioma (STELLAR): A multicentre, single-arm phase 2 trial. Lancet Oncol. 2019, 20, 1702–1709. [Google Scholar] [CrossRef] [PubMed]
- Kutuk, T.; Appel, H.; Avendano, M.C.; Albrecht, F.; Kaywin, P.; Ramos, S.; Suarez-Murias, M.E.; Mehta, M.P.; Kotecha, R. Feasibility of Tumor Treating Fields with Pemetrexed and Platinum-Based Chemotherapy for Unresectable Malignant Pleural Mesothelioma: Single-Center, Real-World Data. Cancers 2022, 14, 2020. [Google Scholar] [CrossRef] [PubMed]
- Byrne, M.J.; Nowak, A.K. Modified RECIST criteria for assessment of response in malignant pleural mesothelioma. Ann. Oncol. 2004, 15, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Mrugala, M.M.; Engelhard, H.H.; Dinh Tran, D.; Kew, Y.; Cavaliere, R.; Villano, J.L.; Annenelie Bota, D.; Rudnick, J.; Love Sumrall, A.; Zhu, J.J.; et al. Clinical practice experience with NovoTTF-100A system for glioblastoma: The Patient Registry Dataset (PRiDe). Semin. Oncol. 2014, 41 (Suppl. S6), S4–S13. [Google Scholar] [CrossRef] [PubMed]
- Kanner, A.A.; Wong, E.T.; Villano, J.L.; Ram, Z.; Investigators, E.F. Post Hoc analyses of intention-to-treat population in phase III comparison of NovoTTF-100A system versus best physician’s choice chemotherapy. Semin. Oncol. 2014, 41 (Suppl. S6), S25–S34. [Google Scholar] [CrossRef] [PubMed]
- Lacouture, M.E.; Anadkat, M.J.; Ballo, M.T.; Iwamoto, F.; Jeyapalan, S.A.; La Rocca, R.V.; Schwartz, M.; Serventi, J.N.; Glas, M. Prevention and Management of Dermatologic Adverse Events Associated with Tumor Treating Fields in Patients with Glioblastoma. Front. Oncol. 2020, 10, 1045. [Google Scholar] [CrossRef] [PubMed]
- Anadkat, M.J.; Lacouture, M.; Friedman, A.; Horne, Z.D.; Jung, J.; Kaffenberger, B.; Kalmadi, S.; Ovington, L.; Kotecha, R.; Abdullah, H.I.; et al. Expert guidance on prophylaxis and treatment of dermatologic adverse events with Tumor Treating Fields (TTFields) therapy in the thoracic region. Front. Oncol. 2022, 12, 975473. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kutuk, T.; Walker, J.M.; Ballo, M.T.; Cameron, R.B.; Alvarez, J.B.; Chawla, S.; Luk, E.; Behl, D.; Dal Pra, A.; Morganstein, N.; et al. Multi-Institutional Patterns of Use of Tumor-Treating Fields for Patients with Malignant Pleural Mesothelioma. Curr. Oncol. 2023, 30, 5195-5200. https://doi.org/10.3390/curroncol30060394
Kutuk T, Walker JM, Ballo MT, Cameron RB, Alvarez JB, Chawla S, Luk E, Behl D, Dal Pra A, Morganstein N, et al. Multi-Institutional Patterns of Use of Tumor-Treating Fields for Patients with Malignant Pleural Mesothelioma. Current Oncology. 2023; 30(6):5195-5200. https://doi.org/10.3390/curroncol30060394
Chicago/Turabian StyleKutuk, Tugce, Joshua M. Walker, Matthew T. Ballo, Robert B. Cameron, Jean Bustamante Alvarez, Sheema Chawla, Eric Luk, Deepti Behl, Alan Dal Pra, Neil Morganstein, and et al. 2023. "Multi-Institutional Patterns of Use of Tumor-Treating Fields for Patients with Malignant Pleural Mesothelioma" Current Oncology 30, no. 6: 5195-5200. https://doi.org/10.3390/curroncol30060394
APA StyleKutuk, T., Walker, J. M., Ballo, M. T., Cameron, R. B., Alvarez, J. B., Chawla, S., Luk, E., Behl, D., Dal Pra, A., Morganstein, N., Refaat, T., Sheybani, A., Squillante, C., Zhang, J., & Kotecha, R. (2023). Multi-Institutional Patterns of Use of Tumor-Treating Fields for Patients with Malignant Pleural Mesothelioma. Current Oncology, 30(6), 5195-5200. https://doi.org/10.3390/curroncol30060394




