Effects of Antibody Response after Booster Vaccination on SARS-CoV-2 Breakthrough Infections and Disease Outcomes in Advanced Cancer Patients: A Prospective Analysis of the Vax-on-Third Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Microbiological Assessments
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
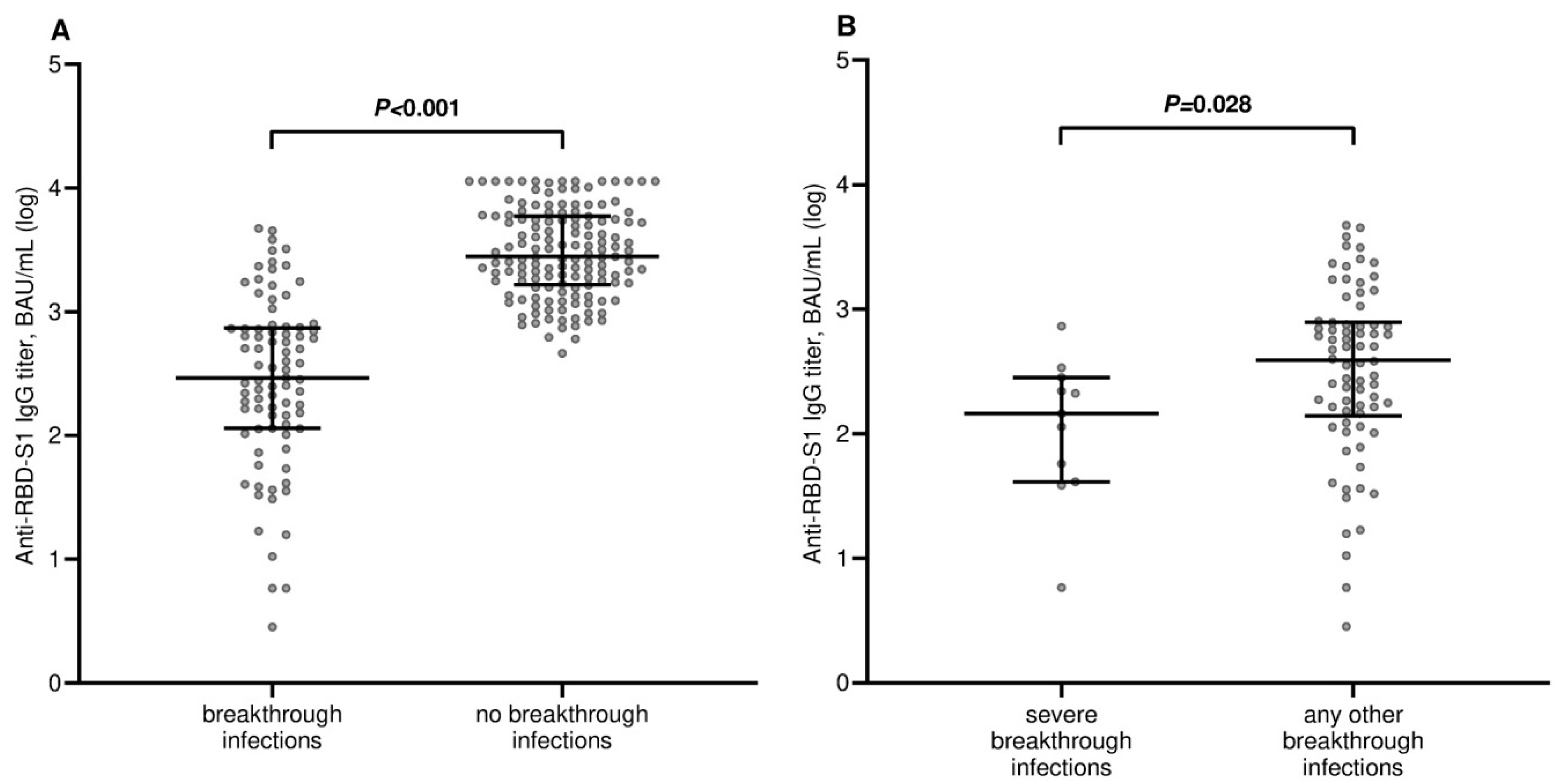
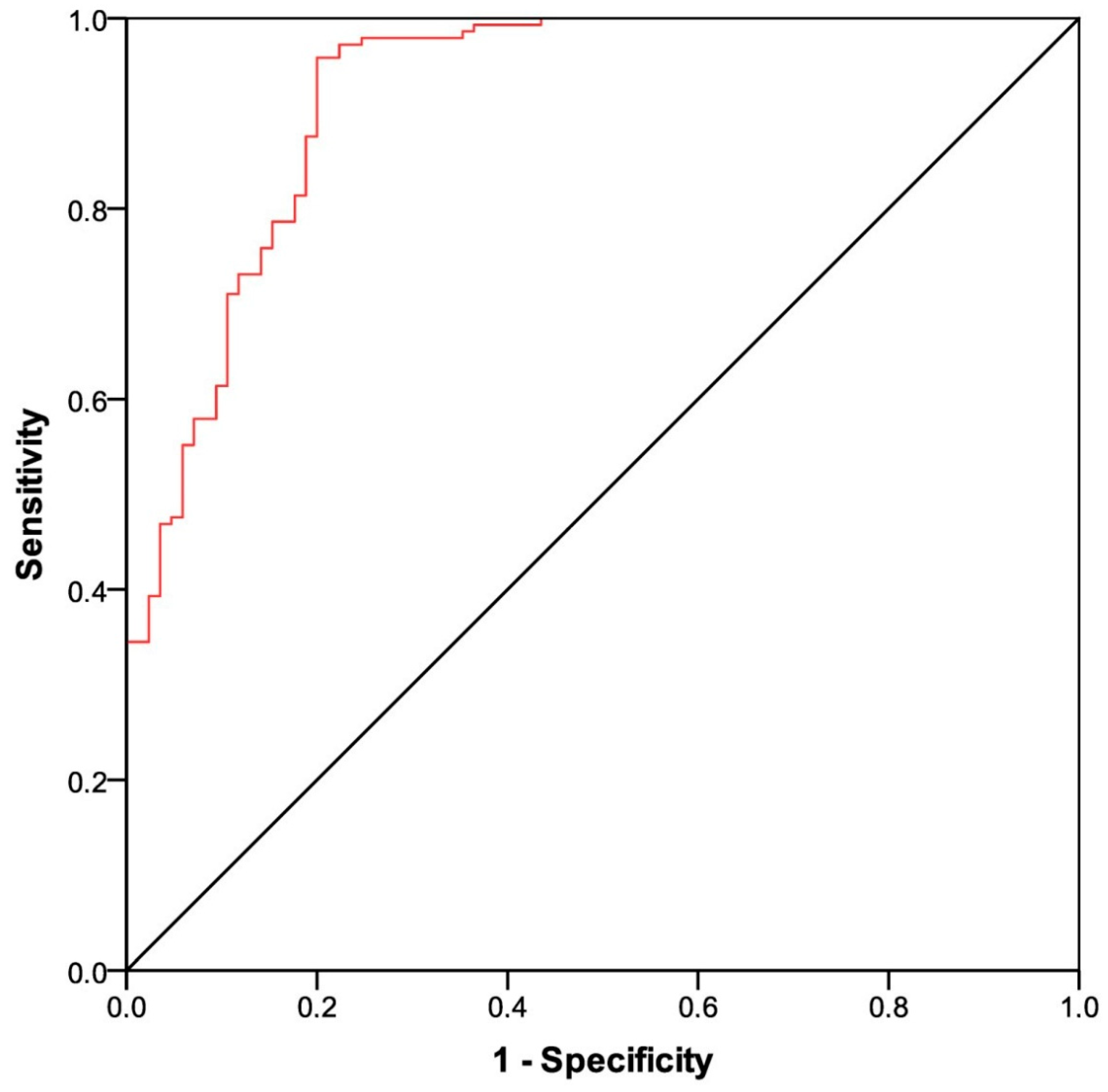
3.2. Breakthrough Infections and Antibody Responses
3.3. Time-to-Treatment Failure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, A.R.Y.B.; Wong, S.Y.; Chai, L.Y.A.; Lee, S.C.; Lee, M.X.; Muthiah, M.D.; Tay, S.H.; Teo, C.B.; Tan, B.K.J.; Chan, Y.H.; et al. Efficacy of covid-19 vaccines in immunocompromised patients: Systematic review and meta-analysis. BMJ 2022, 376, e068632. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Kaelber, D.C.; Xu, R.; Berger, N.A. Breakthrough SARS-CoV-2 infections, hospitalizations, and mortality in vaccinated patients with cancer in the US between December 2020 and November 2021. JAMA Oncol. 2022, 8, 1027–1034. [Google Scholar] [CrossRef] [PubMed]
- Song, Q.; Bates, B.; Shao, Y.R.; Hsu, F.C.; Liu, F.; Madhira, V.; Mitra, A.K.; Bergquist, T.; Kavuluru, R.; Li, X.; et al. Risk and Outcome of Breakthrough COVID-19 Infections in Vaccinated Patients with Cancer: Real-World Evidence from the National COVID Cohort Collaborative. J. Clin. Oncol. 2022, 40, 1414–1427. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.Y.W.; Starkey, T.; Ionescu, M.C.; Little, M.; Tilby, M.; Tripathy, A.R.; Mckenzie, H.S.; Al-Hajji, Y.; Barnard, M.; Benny, L.; et al. Vaccine effectiveness against COVID-19 breakthrough infections in patients with cancer (UKCCEP): A population-based test-negative case-control study. Lancet Oncol. 2022, 23, 748–757. [Google Scholar] [CrossRef] [PubMed]
- Sakuraba, A.; Luna, A.; Micic, D. Serologic response following SARS-COV2 vaccination in patients with cancer: A systematic review and meta-analysis. J. Hematol. Oncol. 2022, 15, 15. [Google Scholar] [CrossRef]
- Sette, A.; Crotty, S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell 2021, 184, 861–880. [Google Scholar] [CrossRef]
- Ligumsky, H.; Dor, H.; Etan, T.; Golomb, I.; Nikolaevski-Berlin, A.; Greenberg, I.; Halperin, T.; Angel, Y.; Henig, O.; Spitzer, A.; et al. Immunogenicity and safety of BNT162b2 mRNA vaccine booster in actively treated patients with cancer. Lancet Oncol. 2022, 23, 193–195. [Google Scholar] [CrossRef]
- Rottenberg, Y.; Grinshpun, A.; Ben-Dov, I.Z.; Oiknine Djian, E.; Wolf, D.G.; Kadouri, L. Assessment of response to a third dose of the SARS-CoV-2 BNT162b2 mRNA vaccine in patients with solid tumors undergoing active treatment. JAMA Oncol. 2022, 8, 300–301. [Google Scholar] [CrossRef]
- Debie, Y.; Vandamme, T.; Goossens, M.E.; van Dam, P.A.; Peeters, M. Antibody titres before and after a third dose of the SARS-CoV-2 BNT162b2 vaccine in patients with cancer. Eur. J. Cancer. 2022, 163, 177–179. [Google Scholar] [CrossRef]
- Fenioux, C.; Teixeira, L.; Fourati, S.; Melica, G.; Lelievre, J.D.; Gallien, S.; Zalcman, G.; Pawlotsky, J.M.; Tournigand, C. SARS-CoV-2 Antibody Response to 2 or 3 Doses of the BNT162b2 Vaccine in Patients Treated with Anticancer Agents. JAMA Oncol. 2022, 8, 612–617. [Google Scholar] [CrossRef]
- Fendler, A.; Shepherd, S.T.C.; Au, L.; Wilkinson, K.A.; Wu, M.; Schmitt, A.M.; Tippu, Z.; Farag, S.; Rogiers, A.; Harvey, R.; et al. Immune responses following third COVID-19 vaccination are reduced in patients with hematological malignancies compared to patients with solid cancer. Cancer Cell 2022, 40, 438. [Google Scholar] [CrossRef] [PubMed]
- Zeng, C.; Evans, J.P.; Chakravarthy, K.; Qu, P.; Reisinger, S.; Song, N.J.; Rubinstein, M.P.; Shields, P.G.; Li, Z.; Liu, S.L. COVID-19 mRNA booster vaccines elicit strong protection against SARS-CoV-2 Omicron variant in patients with cancer. Cancer Cell 2022, 40, 117–119. [Google Scholar] [CrossRef] [PubMed]
- Choueiri, T.K.; Labaki, C.; Bakouny, Z.; Hsu, C.Y.; Schmidt, A.L.; de Lima Lopes, G., Jr.; Hwang, C.; Singh, S.R.K.; Jani, C.; Weissmann, L.B.; et al. Breakthrough SARS-CoV-2 infections among patients with cancer following two and three doses of COVID-19 mRNA vaccines: A retrospective observational study from the COVID-19 and Cancer Consortium. Lancet Reg. Health Am. 2023, 19, 100445. [Google Scholar] [CrossRef] [PubMed]
- Gong, I.Y.; Vijenthira, A.; Powis, M.; Calzavara, A.; Patrikar, A.; Sutradhar, R.; Hicks, L.K.; Wilton, D.; Singh, S.; Krzyzanowska, M.K.; et al. Association of COVID-19 Vaccination with Breakthrough Infections and Complications in Patients with Cancer. JAMA Oncol. 2023, 9, 386–394. [Google Scholar] [CrossRef]
- Lee, L.Y.W.; Ionescu, M.C.; Starkey, T.; Little, M.; Tilby, M.; Tripathy, A.R.; Mckenzie, H.S.; Al-Hajji, Y.; Appanna, N.; Barnard, M.; et al. UK Coronavirus Cancer Programme. COVID-19: Third dose booster vaccine effectiveness against breakthrough coronavirus infection, hospitalisations and death in patients with cancer: A population-based study. Eur. J. Cancer 2022, 175, 1–10. [Google Scholar] [CrossRef]
- van Vliet, E.D.; Eijkelboom, A.H.; van Giessen, A.; Siesling, S.; de Wit, G.A. Physical and mental health outcomes of COVID-19 induced delay in oncological care: A systematic review. Front. Oncol. 2023, 13, 998940. [Google Scholar] [CrossRef]
- van der Veldt, A.A.M.; Oosting, S.F.; Fehrmann, R.S.N.; GeurtsvanKessel, C.H.; van Binnendijk, R.S.; Dingemans, A.C.; Smit, E.F.; Hiltermann, T.J.N.; Hartog, G.D.; Jalving, M.; et al. One-year data on immunogenicity and breakthrough infections in patients with solid tumors vaccinated against COVID-19 during systemic cancer treatment. ESMO Open 2023, 8, 100785. [Google Scholar] [CrossRef]
- Macrae, K.; Martinez-Cajas, J.; Bessai, K.; Abdulhamed, A.; Gong, Y. Quantitative Analysis of SARS-CoV-2 Antibody Levels in Cancer Patients Post Three Doses of Immunization and Prior to Breakthrough COVID-19 Infections. Curr. Oncol. 2022, 29, 7059–7071. [Google Scholar] [CrossRef]
- Nelli, F.; Giannarelli, D.; Fabbri, A.; Silvestri, M.A.; Berrios, J.R.G.; Virtuoso, A.; Marrucci, E.; Schirripa, M.; Mazzotta, M.; Onorato, A.; et al. Immunogenicity and early clinical outcome after two or three doses of SARS-CoV-2 mRNA-BNT162b2 vaccine in actively treated cancer patients: Results from the prospective observational Vax-On-Third study. Ann. Oncol. 2022, 33, 740–742. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- COVID-19 Integrated Surveillance Data in Italy. Available online: https://www.epicentro.iss.it/en/coronavirus/sars-cov-2-dashboard (accessed on 7 March 2023).
- Country Overview Report: Week 9 2023. Available online: https://covid19-country-overviews.ecdc.europa.eu/variants_of_concern.html (accessed on 7 March 2023).
- AdviseDx SARS-CoV-2 IgG II. Package Insert. Abbott Laboratories. 2021. Available online: https://www.fda.gov/media/146371/download (accessed on 7 March 2023).
- Saker, K.; Escuret, V.; Pitiot, V.; Massardier-Pilonchéry, A.; Paul, S.; Mokdad, B.; Langlois-Jacques, C.; Rabilloud, M.; Goncalves, D.; Fabien, N.; et al. Evaluation of Commercial Anti-SARS-CoV-2 Antibody Assays and Comparison of Standardized Titers in Vaccinated Health Care Workers. J. Clin. Microbiol. 2022, 60, e0174621. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, W.; Xu, R.; Berger, N.A. SARS-CoV-2 primary and breakthrough infections in patients with cancer: Implications for patient care. Best Pract. Res. Clin. Haematol. 2022, 35, 101384. [Google Scholar] [CrossRef] [PubMed]
- Prevalenza e Distribuzione Delle Varianti di SARS-CoV-2 di Interesse per la Sanità Pubblica in Italia. Available online: https://www.epicentro.iss.it/coronavirus/pdf/sars-cov-2-monitoraggio-varianti-rapporti-periodici-3-febbraio-2023.pdf (accessed on 7 March 2023).
- Fendler, A.; de Vries, E.G.; GeurtsvanKessel, C.H.; Haanen, J.B.; Wörmann, B.; Turajlic, S.; von Lilienfeld-Toal, M. COVID-19 vaccines in patients with cancer: Immunogenicity, efficacy and safety. Nat. Rev. Clin. Oncol. 2022, 19, 385–401. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.; Stowe, J.; Kirsebom, F.; Toffa, S.; Rickeard, T.; Gallagher, E.; Gower, C.; Kall, M.; Groves, N.; O’Connell, A.M.; et al. Covid-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant. N. Engl. J. Med. 2022, 386, 1532–1546. [Google Scholar] [CrossRef]
- Lee, M.; Quinn, R.; Pradhan, K.; Fedorov, K.; Levitz, D.; Fromowitz, A.; Thakkar, A.; Shapiro, L.C.; Kabarriti, R.; Ruiz, R.E.; et al. Impact of COVID-19 on case fatality rate of patients with cancer during the Omicron wave. Cancer Cell 2022, 40, 343–345. [Google Scholar] [CrossRef]
- Mair, M.J.; Mitterer, M.; Gattinger, P.; Berger, J.M.; Trutschnig, W.; Bathke, A.C.; Gansterer, M.; Berghoff, A.S.; Laengle, S.; Gottmann, L.; et al. Enhanced SARS-CoV-2 breakthrough infections in patients with hematologic and solid cancers due to Omicron. Cancer Cell 2022, 40, 444–446. [Google Scholar] [CrossRef]
- Piñana, J.L.; Vazquez, L.; Calabuig, M.; López-Corral, L.; Martin-Martin, G.; Villalon, L.; Sanz-Linares, G.; Conesa-Garcia, V.; Sanchez-Salinas, A.; Gago, B.; et al. One-year breakthrough SARS-CoV-2 infection and correlates of protection in fully vaccinated hematological patients. Blood Cancer J. 2023, 13, 8. [Google Scholar] [CrossRef]
- Chien, K.S.; Peterson, C.; Young, E.; Chihara, D.; Manasanch, E.E.; Ramdial, J.; Thompson, P.A. Outcomes of Breakthrough COVID-19 Infections in Patients with Hematologic Malignancies. Blood Adv. 2023, 25, bloodadvances.2022008827. [Google Scholar] [CrossRef]
- Gleiss, A.; Oberbauer, R.; Heinze, G. An unjustified benefit: Immortal time bias in the analysis of time-dependent events. Transpl. Int. 2018, 31, 125–130. [Google Scholar] [CrossRef]
- Cohen, I.; Campisi-Pfinto, S.; Rozenberg, O.; Colodner, R.; Bar-Sela, G. The Humoral Response of Patients with Cancer to Breakthrough COVID-19 Infection or the Fourth BNT162b2 Vaccine Dose. Oncologist 2023, 28, oyad003. [Google Scholar] [CrossRef]
- Ehmsen, S.; Pedersen, R.M.; Bang, L.L.; Asmussen, A.; Kragh, A.; Holm, D.K.; Sydenham, T.V.; Jensen, T.G.; Jeppesen, S.S.; Frederiksen, H.; et al. BQ.1.1, XBB.1, and XBB.1.5 neutralization after bivalent mRNA COVID-19 booster in patients with cancer. Cancer Cell 2023, 41, 649–650. [Google Scholar] [CrossRef] [PubMed]
- Thakkar, A.; Pradhan, K.; Duva, B.; Carreno, J.M.; Sahu, S.; Thiruthuvanathan, V.; Campbell, S.; Gallego, S.; Bhagat, T.D.; Rivera, J.; et al. Study of efficacy and longevity of immune response to third and fourth doses of COVID-19 vaccines in patients with cancer: A single arm clinical trial. Elife 2023, 12, e83694. [Google Scholar] [CrossRef] [PubMed]
- Booth, S.; Curley, H.M.; Varnai, C.; Arnold, R.; Lee, L.Y.W.; Campton, N.A.; Cook, G.; Purshouse, K.; Aries, J.; Innes, A.; et al. Key findings from the UKCCMP cohort of 877 patients with haematological malignancy and COVID-19: Disease control as an important factor relative to recent chemotherapy or anti-CD20 therapy. Br. J. Haematol. 2022, 196, 892–901. [Google Scholar] [CrossRef]
- Lee, L.Y.W.; Tilby, M.; Starkey, T.; Ionescu, M.C.; Burnett, A.; Hattersley, R.; Khan, S.; Little, M.; Liu, J.K.H.; Platt, J.R.; et al. Association of SARS-CoV-2 Spike Protein Antibody Vaccine Response with Infection Severity in Patients With Cancer: A National COVID Cancer Cross-sectional Evaluation. JAMA Oncol. 2023, 9, 188–196. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | All Patients, N = 230 (100%) |
| Age | |
| mean (SD), years | 65.4 (10.5) |
| -≤55 years | 46 (20.0%) |
| ->55 years | 184 (80.0%) |
| Sex | |
| -female | 131 (56.9%) |
| -male | 99 (43.1%) |
| ECOG PS | |
| 0 | 98 (42.6%) |
| -1 | 113 (49.1%) |
| -2 | 19 (8.3%) |
| Cancer type | |
| -breast | 62 (26.9%) |
| -lung | 56 (24.3%) |
| -kidney | 10 (4.3%) |
| -prostate | 8 (3.5) |
| -colorectal | 41 (17.8%) |
| -urothelial | 8 (3.5%) |
| -pancreatic | 10 (4.3%) |
| -gastric | 5 (2.2%) |
| -skin (Melanoma or Merkelcell) | 5 (2.2%) |
| -gynecological | 9 (3.9% |
| -head and neck | 2 (0.9%) |
| -brain | 7 (3.0%) |
| -other a | 7 (3.0%) |
| Extent of disease | |
| -locally advanced | 5 (2.2%) |
| -metastatic | 225 (97.8%) |
| Treatment setting | |
| -advanced disease, first line | 161 (70.0%) |
| -advanced disease, second or later line | 69 (30.0%) |
| Type of last active treatment | |
| -targeted therapy | 91 (39.6%) |
| -cytotoxic chemotherapy | 64 (27.8%) |
| -immune checkpoint inhibitors | 35 (15.2%) |
| -hormonal therapy | 14 (6.1%) |
| -cytotoxic chemotherapy and biological therapy | 26 (11.3%) |
| Time from last active treatment and booster vaccination | |
| -median (IQR), days | 10 (2–18) |
| Corticosteroid therapy b | 41 (17.8%) |
| Characteristics | All Patients, N = 230 (100%) |
| Age | |
| mean (SD), years | 65.4 (10.5) |
| ≤55 years | 46 (20.0%) |
| >55 years | 184 (80.0%) |
| Sex | |
| female | 131 (56.9%) |
| male | 99 (43.1%) |
| ECOG PS | |
| 0 | 98 (42.6%) |
| -1 | 113 (49.1%) |
| -2 | 19 (8.3%) |
| Cancer type | |
| breast | 62 (26.9%) |
| lung | 56 (24.3%) |
| kidney | 10 (4.3%) |
| prostate | 8 (3.5) |
| colorectal | 41 (17.8%) |
| urothelial | 8 (3.5%) |
| pancreatic | 10 (4.3%) |
| gastric | 5 (2.2%) |
| skin (Melanoma or Merkelcell) | 5 (2.2%) |
| gynecological | 9 (3.9% |
| head and neck | 2 (0.9%) |
| brain | 7 (3.0%) |
| other a | 7 (3.0%) |
| Extent of disease | |
| locally advanced | 5 (2.2%) |
| metastatic | 225 (97.8%) |
| Treatment setting | |
| advanced disease, first line | 161 (70.0%) |
| advanced disease, second or later line | 69 (30.0%) |
| Type of last active treatment | |
| targeted therapy | 91 (39.6%) |
| cytotoxic chemotherapy | 64 (27.8%) |
| immune checkpoint inhibitors | 35 (15.2%) |
| hormonal therapy | 14 (6.1%) |
| cytotoxic chemotherapy and biological therapy | 26 (11.3%) |
| Time from last active treatment and booster vaccination | |
| median (IQR), days | 10 (2–18) |
| Corticosteroid therapy b | 41 (17.8%) |
| Covariates | OR (95% CI) | p Value |
|---|---|---|
| Sex | ||
| -male vs. female | 0.25 (0.07–0.85) | 0.027 |
| Age (years) | ||
| ->55 vs. ≤55 | 0.44 (0.13–1.44) | 0.177 |
| Cancer type | ||
| -breast | 1 | - |
| -lung | 14.62 (2.31–92.43) | 0.004 |
| -colorectal | 4.84 (0.87–26.71) | 0.07 |
| -others | 3.31 (0.66–16.50) | 0.143 |
| ECOG PS | ||
| -0 a | 1 | - |
| -1 | 1.35 (0.46–3.99) | 0.581 |
| -2 | 0.97 (0.13–7.32) | 0.982 |
| Treatment setting | ||
| -advanced, first line vs. second or later line | 2.22 (0.74–6.62) | 0.343 |
| Corticosteroid therapy | ||
| -yes vs. no | 1.50 (0.36–6.62) | 0.572 |
| Type of active treatment | ||
| -targeted therapy a | 1 | - |
| -cytotoxic chemotherapy | 8.72 (2.14–35.48) | 0.002 |
| -immune checkpoint inhibitors | 2.02 (0.40–10.23) | 0.394 |
| -hormonal therapy | 1.37 (0.07–23.96) | 0.827 |
| -cytotoxic chemotherapy and biologics | 13.47 (1.89–98.89) | 0.009 |
| Antibody response | ||
| -high response vs. low response | 0.004 (0.001–0.019) | <0.001 |
| Additional booster vaccine dosing | ||
| -yes vs. no | 0.73 (0.21–2.23) | 0.625 |
| Covariates | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| V-TTF, Months | p Value a | HR (95% CI) | p Value b | |
| (95% CI) | ||||
| Sex | 0.832 | - | - | |
| -female | 11.8 (7.1–16.6) | |||
| -male | 7.6 (4.3–10.9) | |||
| Age (years) | 0.477 | - | - | |
| -≤55 | 5.4 (2.1–8.7) | |||
| ->55 | 9.8 (6.0–13.5) | |||
| Cancer type | 0.001 | 0.115 | ||
| -others | 12.1 (8.2–16.0) | 1 | ||
| -lung cancer | 5.0 (3.1–7.0) | 1.36 (0.92–2.00) | ||
| ECOG PS | <0.001 | <0.001 | ||
| -0 or 1 | 11.8 (7.8–15.8) | 1 | ||
| -2 | 2.4 (1.6–3.1) | 3.00 (1.75–5.14) | ||
| Treatment setting | 0.171 | - | - | |
| -advanced, first line | 11.8 (7.4–16.21) | |||
| -advanced second or later line | 6.4 (4.2–8.6) | |||
| Corticosteroid therapy | <0.001 | 0.014 | ||
| -no | 12.2 (7.7–16.6) | 1 | ||
| -yes | 3.0 (1.9–4.0) | 1.68 (1.11–2.55) | ||
| Type of active treatment | <0.001 | 0.039 | ||
| -cytotoxic-chemotherapy-based | 5.2 (3.8–6.6) | 1 | ||
| -any other | 14.4 (10.4–16.3) | 1.44 (1.01– 2.06) | ||
| COVID-19 infection | <0.001 | <0.001 | ||
| -no | 16.2 (14.3–17.0) | 1 | ||
| -yes | 3.1 (2.3–3.6) | 5.66 (3.29–9.74) | ||
| Antibody response | <0.001 | 0.017 | ||
| -high response | 14.6 (11.9–16.3) | 1 | ||
| -low response | 3.6 (3.0–4.5) | 1.88 (1.11–3.19) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nelli, F.; Fabbri, A.; Virtuoso, A.; Giannarelli, D.; Giron Berrios, J.R.; Marrucci, E.; Fiore, C.; Schirripa, M.; Signorelli, C.; Chilelli, M.G.; et al. Effects of Antibody Response after Booster Vaccination on SARS-CoV-2 Breakthrough Infections and Disease Outcomes in Advanced Cancer Patients: A Prospective Analysis of the Vax-on-Third Study. Curr. Oncol. 2023, 30, 5103-5115. https://doi.org/10.3390/curroncol30050386
Nelli F, Fabbri A, Virtuoso A, Giannarelli D, Giron Berrios JR, Marrucci E, Fiore C, Schirripa M, Signorelli C, Chilelli MG, et al. Effects of Antibody Response after Booster Vaccination on SARS-CoV-2 Breakthrough Infections and Disease Outcomes in Advanced Cancer Patients: A Prospective Analysis of the Vax-on-Third Study. Current Oncology. 2023; 30(5):5103-5115. https://doi.org/10.3390/curroncol30050386
Chicago/Turabian StyleNelli, Fabrizio, Agnese Fabbri, Antonella Virtuoso, Diana Giannarelli, Julio Rodrigo Giron Berrios, Eleonora Marrucci, Cristina Fiore, Marta Schirripa, Carlo Signorelli, Mario Giovanni Chilelli, and et al. 2023. "Effects of Antibody Response after Booster Vaccination on SARS-CoV-2 Breakthrough Infections and Disease Outcomes in Advanced Cancer Patients: A Prospective Analysis of the Vax-on-Third Study" Current Oncology 30, no. 5: 5103-5115. https://doi.org/10.3390/curroncol30050386
APA StyleNelli, F., Fabbri, A., Virtuoso, A., Giannarelli, D., Giron Berrios, J. R., Marrucci, E., Fiore, C., Schirripa, M., Signorelli, C., Chilelli, M. G., Primi, F., Pessina, G., Natoni, F., Silvestri, M. A., & Ruggeri, E. M. (2023). Effects of Antibody Response after Booster Vaccination on SARS-CoV-2 Breakthrough Infections and Disease Outcomes in Advanced Cancer Patients: A Prospective Analysis of the Vax-on-Third Study. Current Oncology, 30(5), 5103-5115. https://doi.org/10.3390/curroncol30050386





