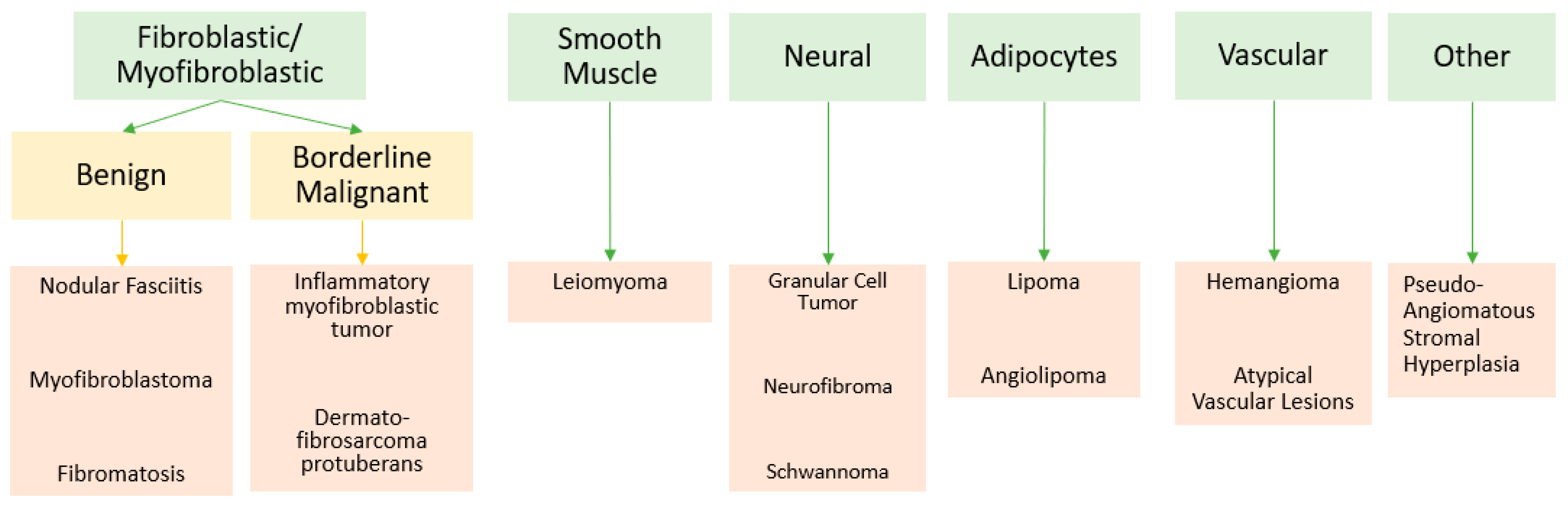
Mesenchymal Tumors of the Breast: Fibroblastic/Myofibroblastic Lesions and Other Lesions
Abstract
1. Introduction
Objectives and Methods
2. Fibroblastic/Myofibroblastic Lesions
2.1. Nodular Fasciitis
Summary of Updates
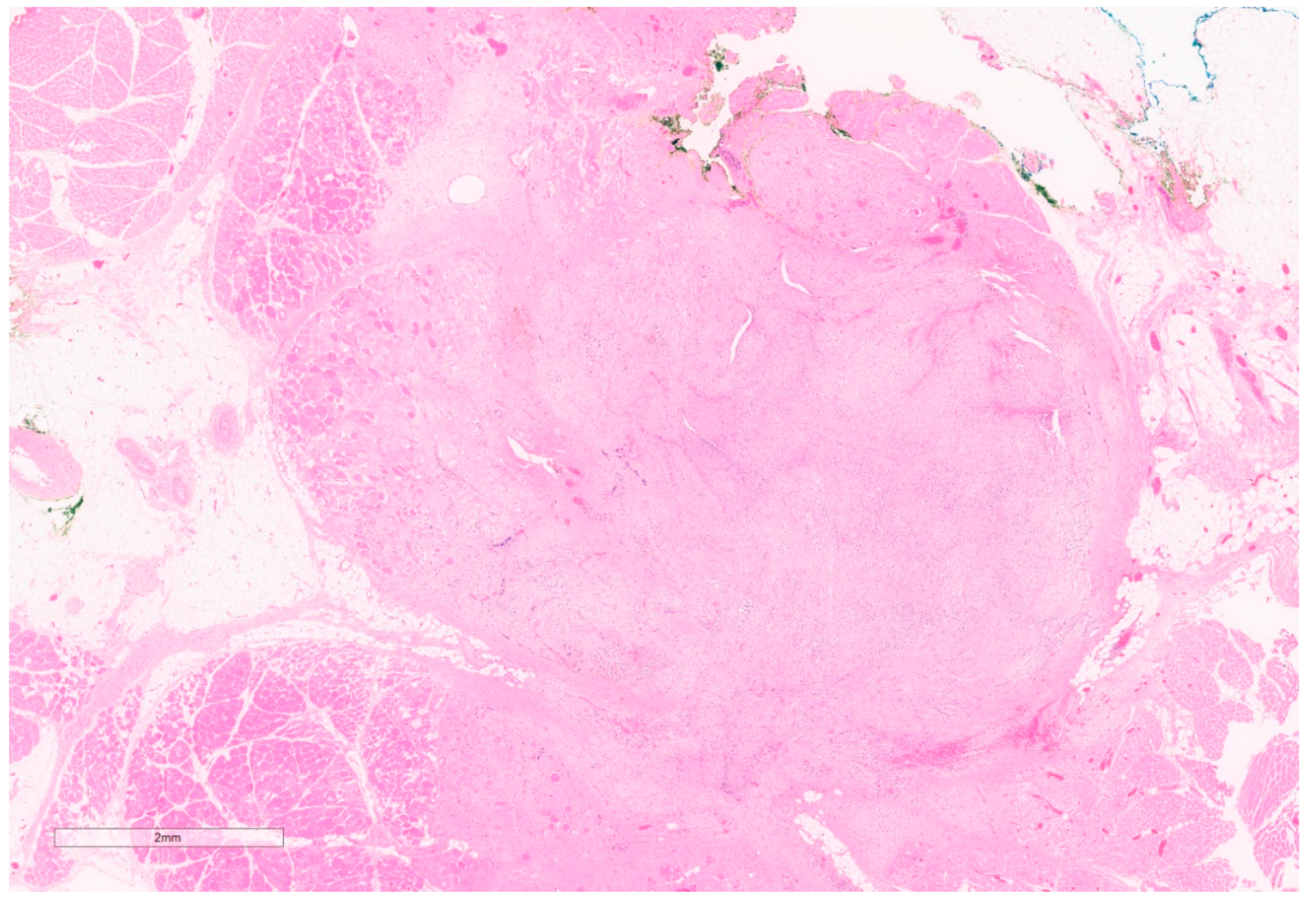
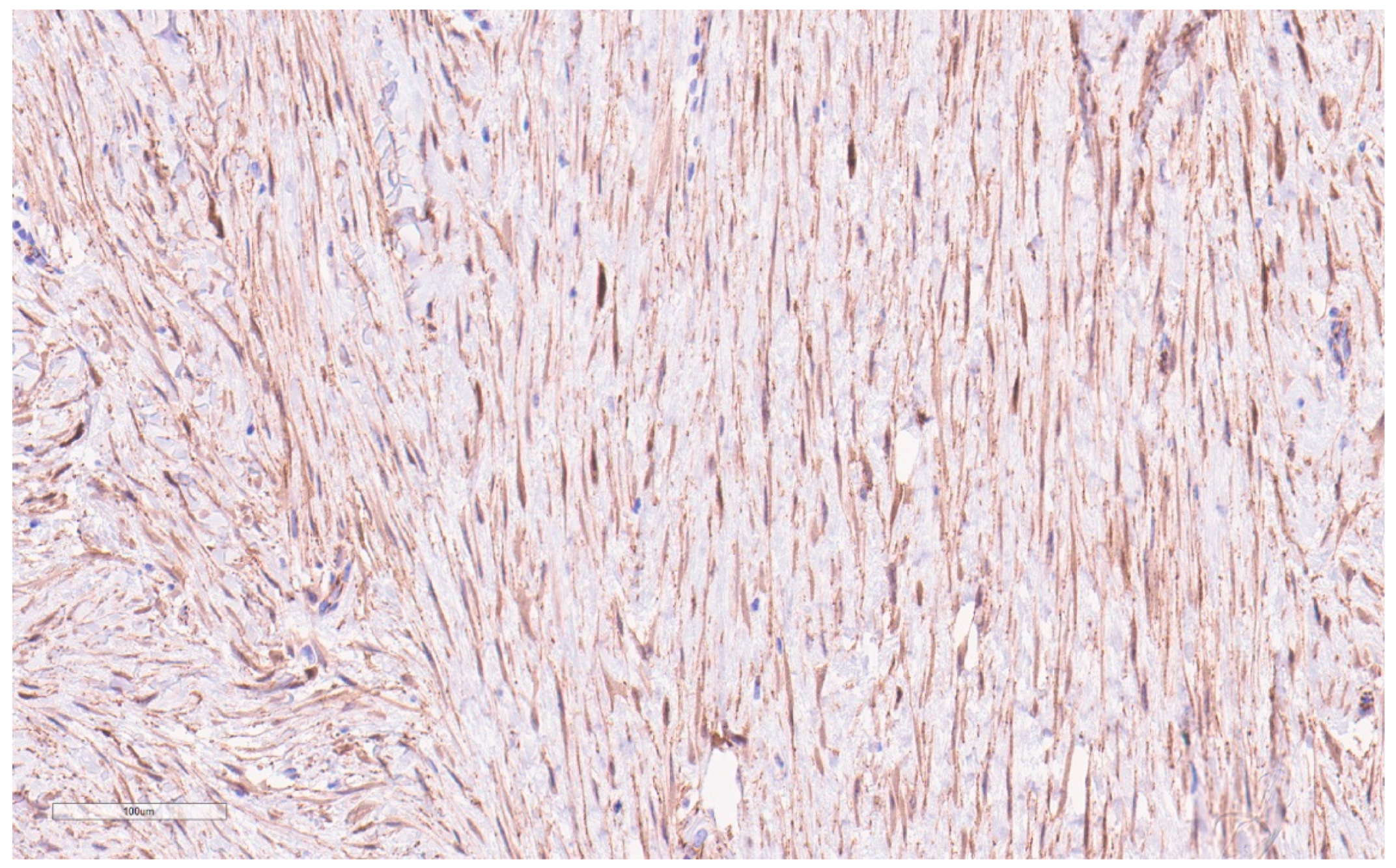
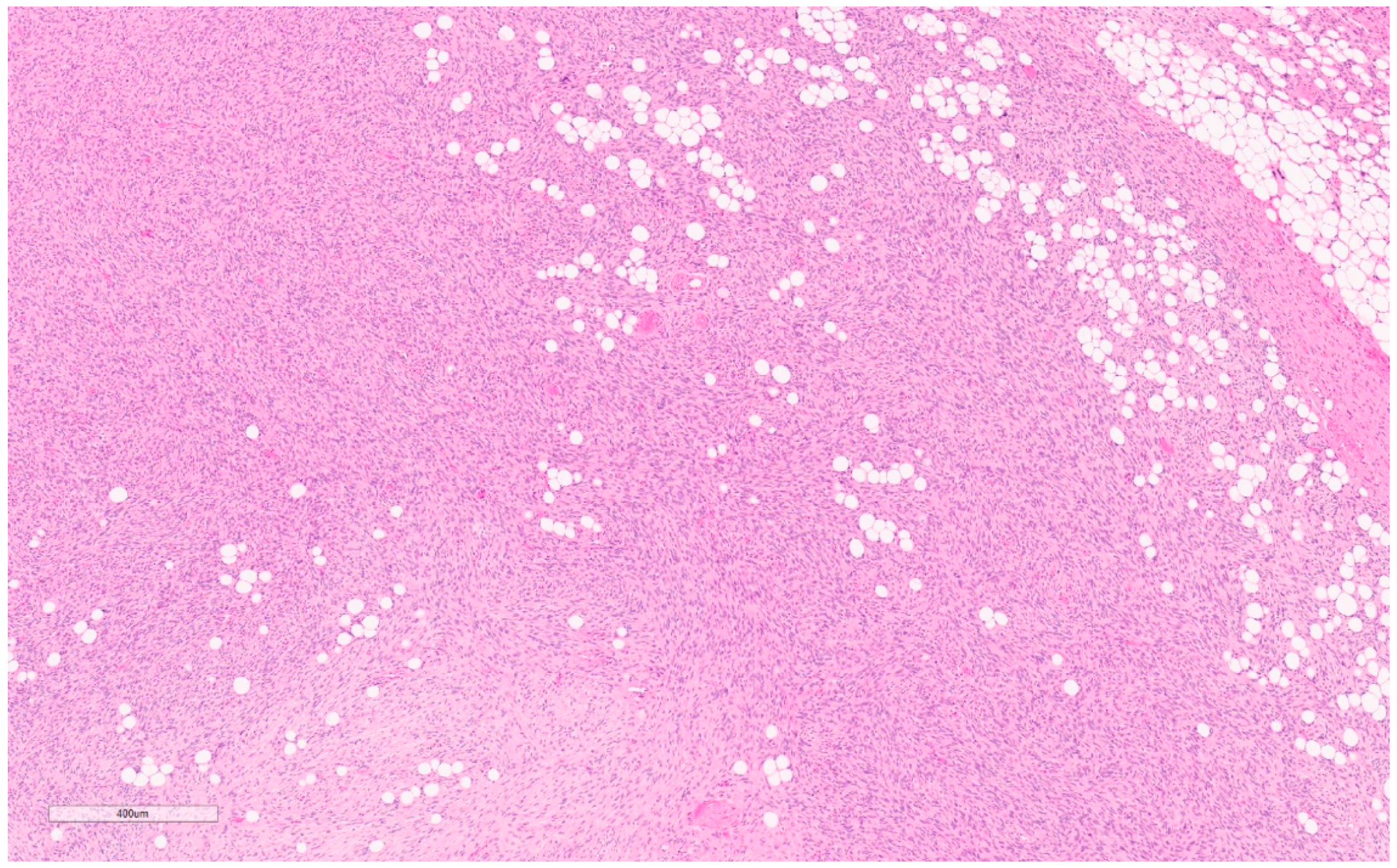
2.2. Myofibroblastoma
Summary of Updates
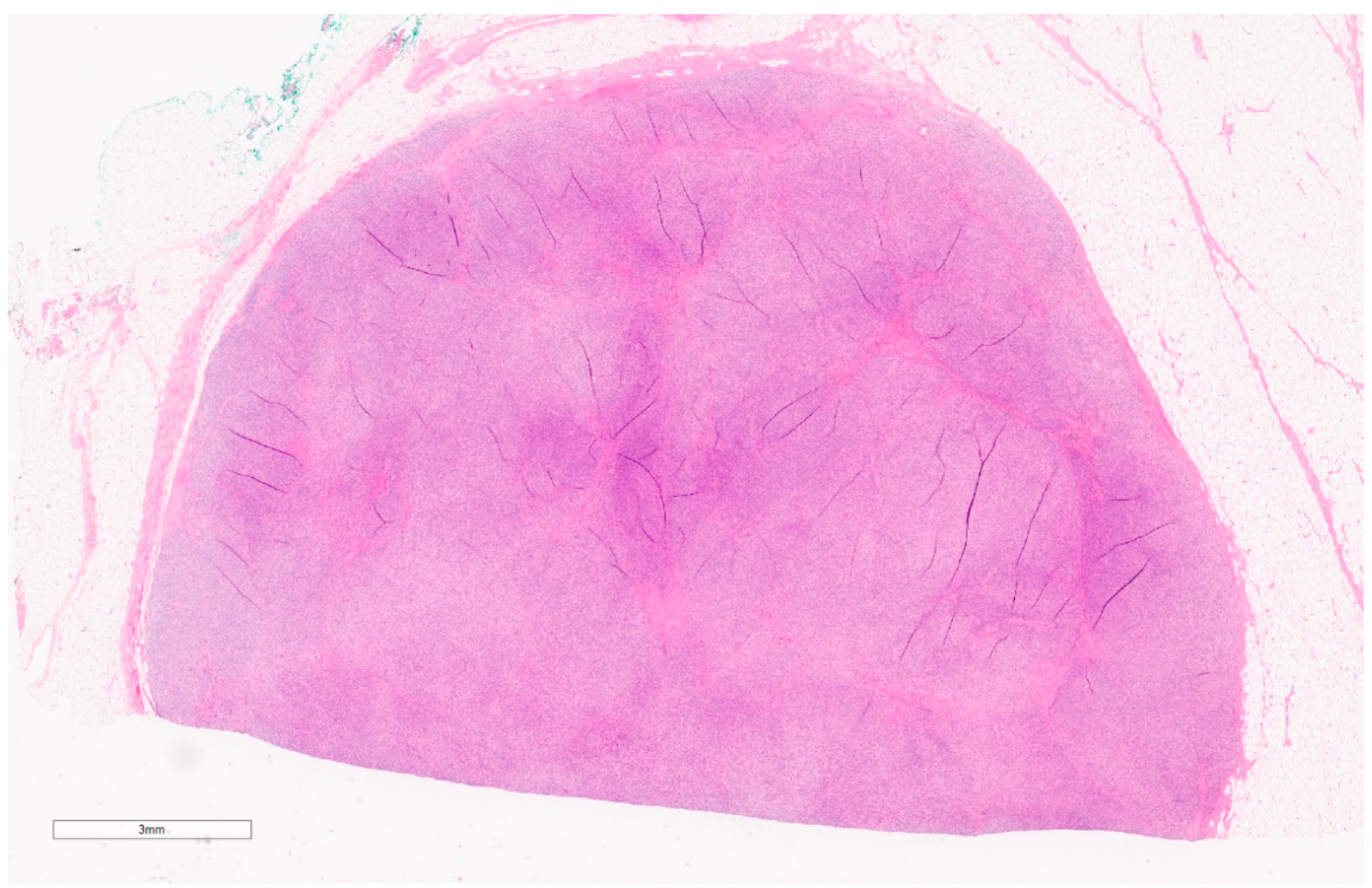
2.3. Fibromatosis/Desmoid Tumor
Summary of Updates
2.4. Inflammatory Myofibroblastic Tumors
Summary of Updates
2.5. Dermatofibrosarcoma Protuberans
Summary of Progress
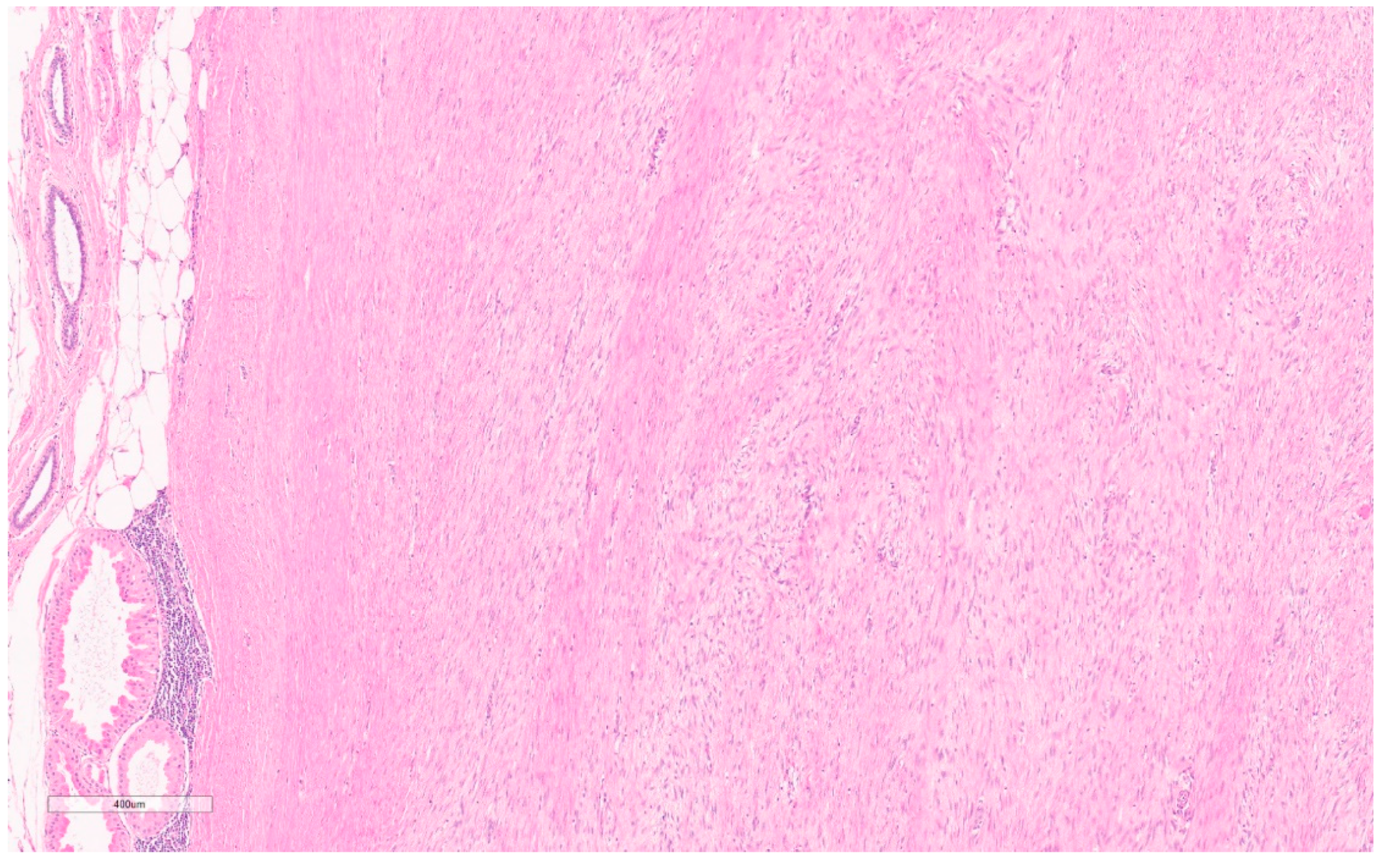
3. Benign Smooth Muscle
3.1. Leiomyoma
- (1)
- Cutaneous: primarily a dermatological diagnosis [62], outside the scope of this review.
- (2)
- (3)
Summary of Updates
4. Peripheral Nerve Sheath Tumors
4.1. Neurofibroma
- Diffuse: these are locally invasive, growing as plaque-like lesions in the subcutaneous tissue [77].
Summary of Updates
4.2. Granular Cell Tumors
Summary of Updates
4.3. Schwannoma
Summary of Updates
5. Benign Adipocytic
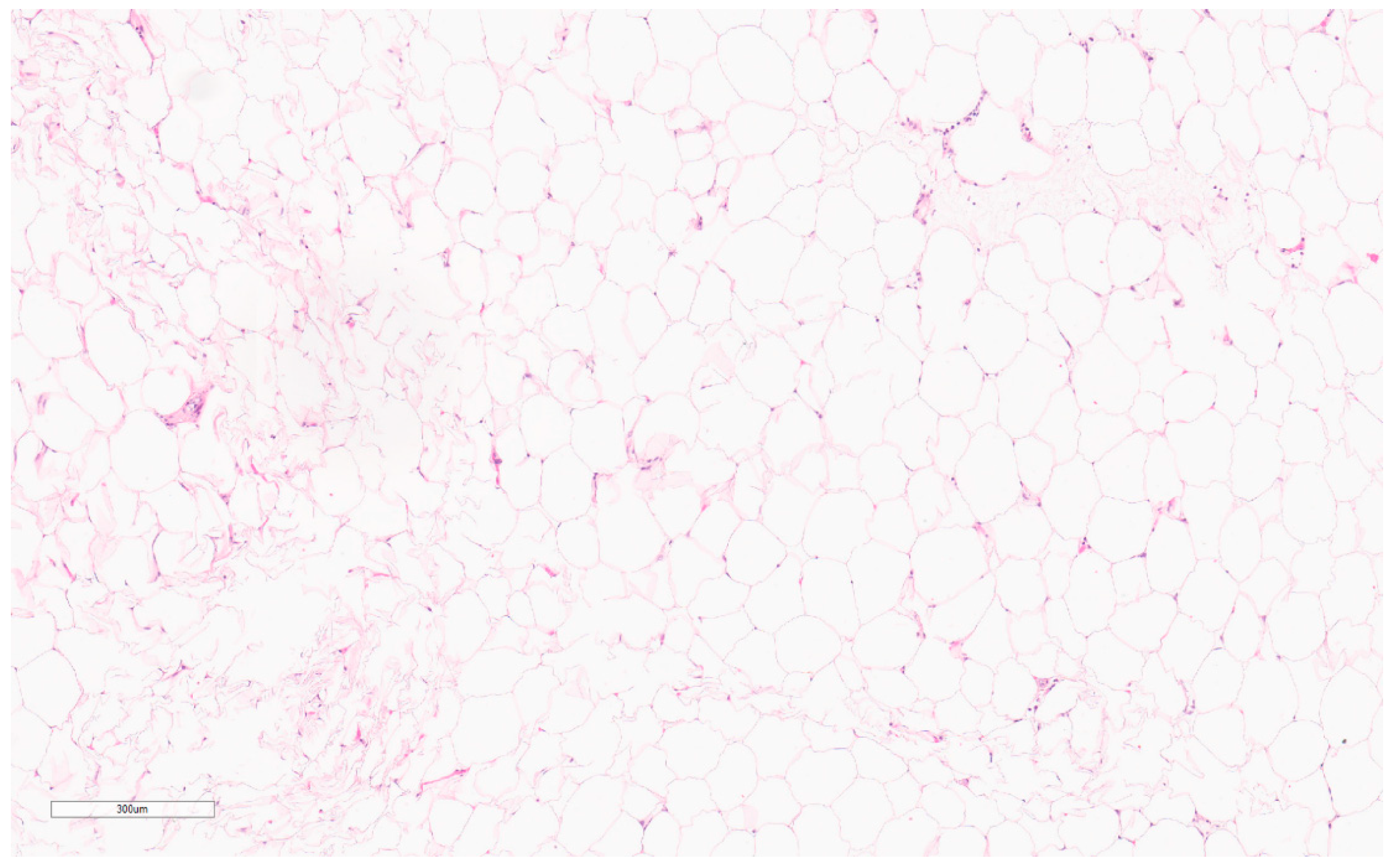
5.1. Lipoma
Summary of Progress
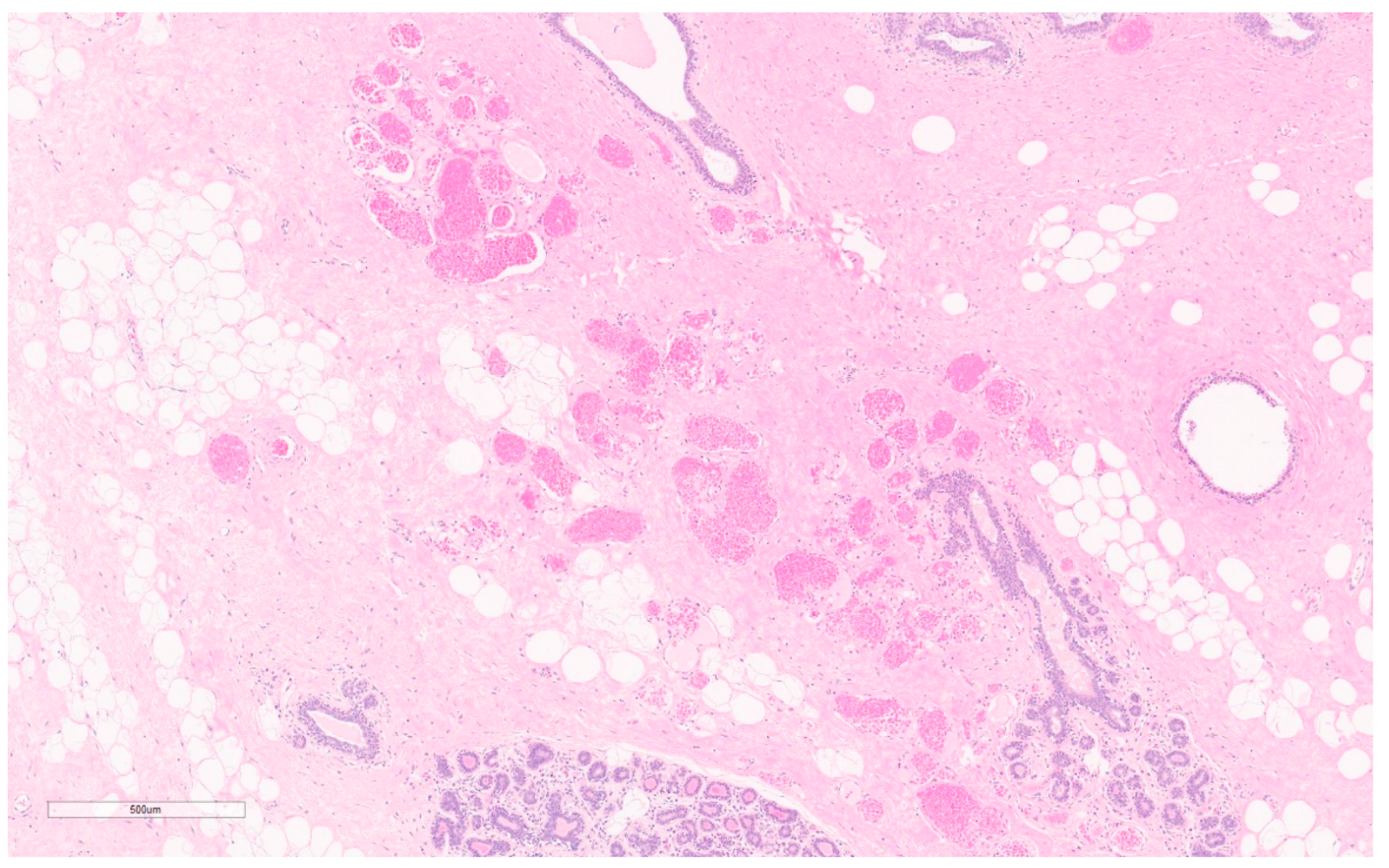
5.2. Angiolipoma
Summary of Updates
6. Benign Vascular
6.1. Hemangioma
Summary of Updates
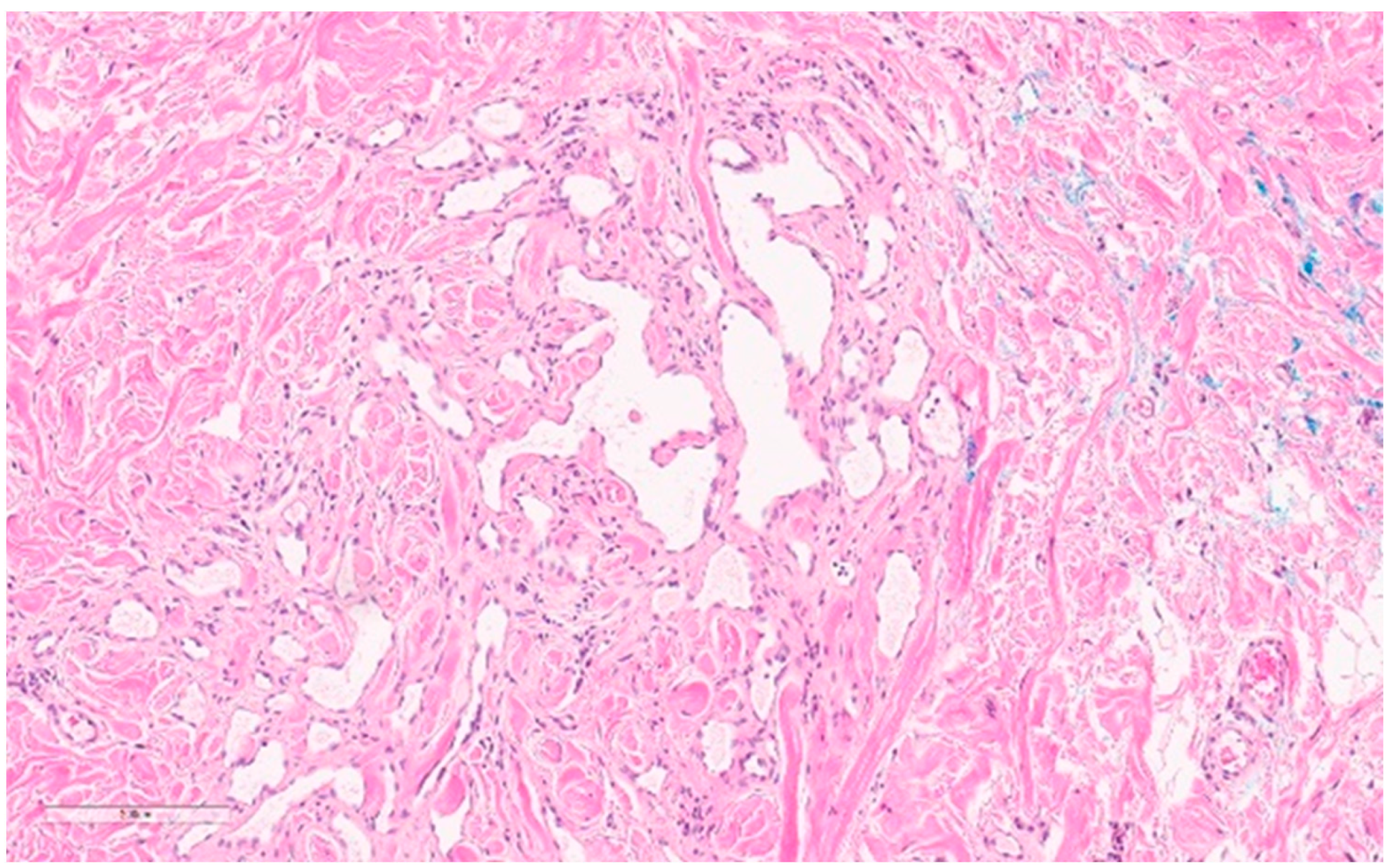
6.2. Atypical Vascular Lesion
Summary of Updates
7. Other
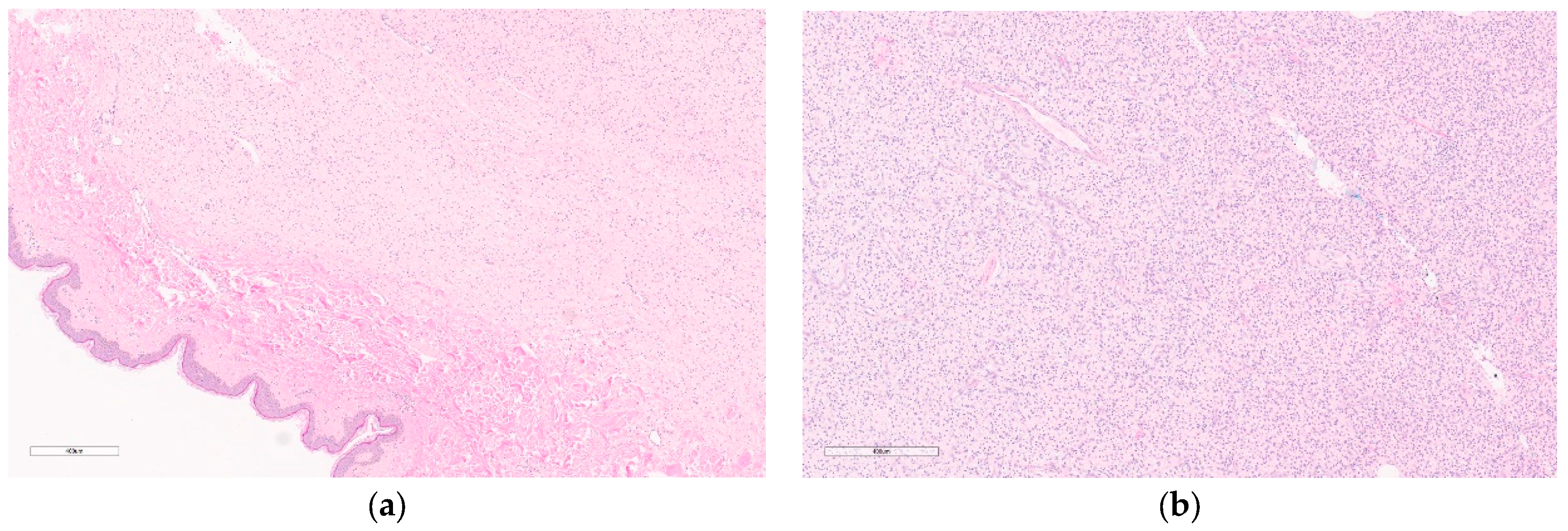
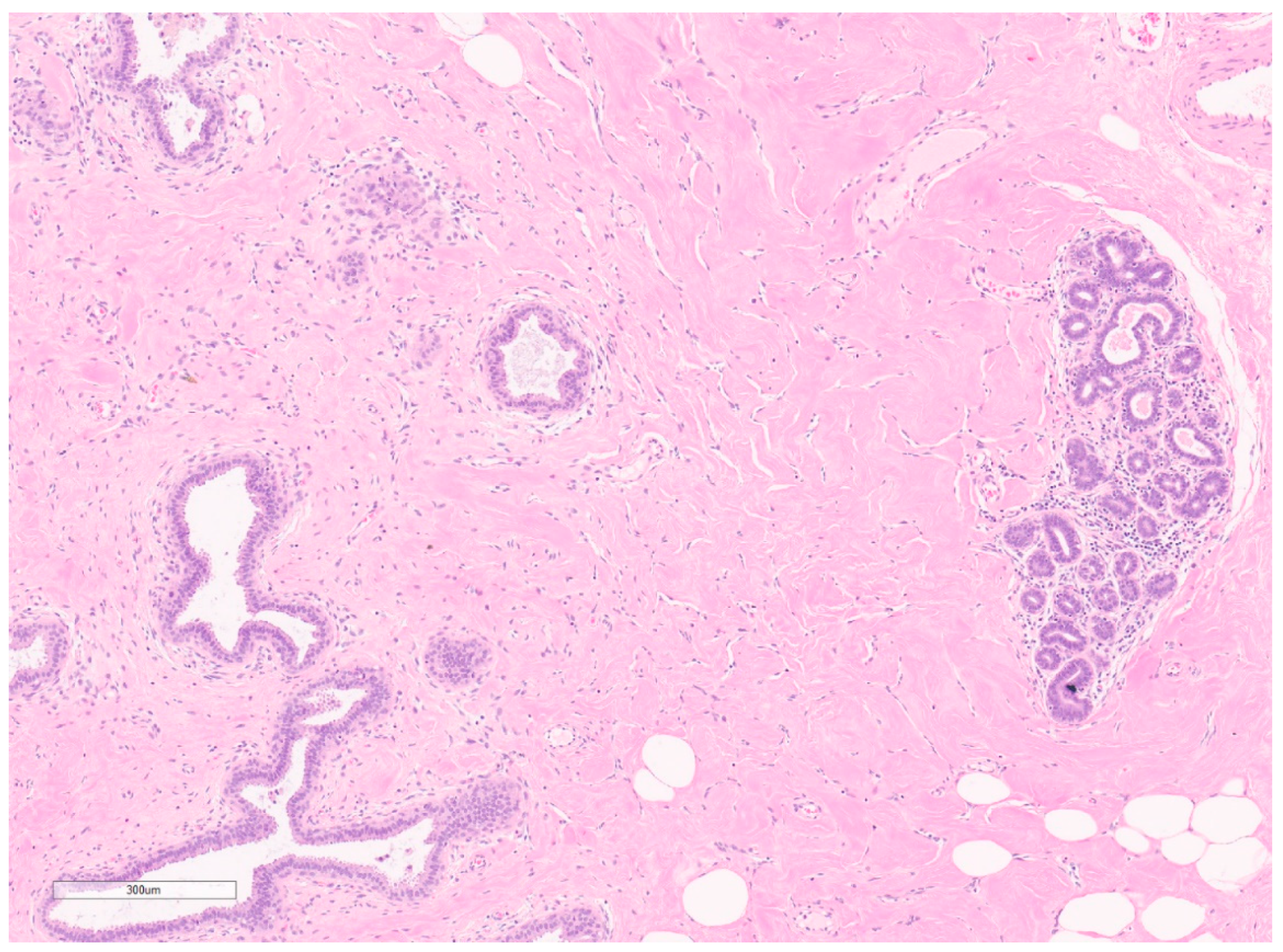
7.1. Pseudoangiomatous Stromal Hyperplasia
7.1.1. Summary of Updates
7.1.2. Summary Tables
Author Contributions
Funding
Conflicts of Interest
References
- Boldt, C. MD Anderson and the Rare Cancer Research Foundation Launch Collaboration to Accelerate the Development of Treatments for Rare Cancers. MD Anderson Newsroom. 2021. Available online: https://www.mdanderson.org/newsroom/md-anderson-rare-cancer-research-foundation-launch-collaboration-accelerate-development-treatments-rare-cancers.h00-159464001.html#:~:text=The%20initiative%20aims%20to%20fully,contribute%20breakthroughs%20to%20the%20field (accessed on 18 February 2023).
- Konwaler, B.E.; Keasbey, L.; Kaplan, L. Subcutaneous Pseudosarcomatous Fibromatosis (Fasciitis). Am. J. Clin. Pathol. 1955, 25, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Hara, H.; Fujita, I.; Fujimoto, T.; Hanioka, K.; Akisue, T.; Kurosaka, M. Nodular Fasciitis of the Hand in a Young Athlete. A Case Report. Upsala J. Med. Sci. 2010, 115, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Yin, X.; Wen, Y.; Ru, G.; Meng, X. Nodular Fasciitis of the Breast: Report of Two Cases Illustrating the Diagnostic Implications for USP6 Gene Rearrangement and Brief Review of the Literature. Exp. Mol. Pathol. 2021, 123, 104690. [Google Scholar] [CrossRef] [PubMed]
- Cloutier, J.M.; Kunder, C.A.; Charville, G.W.; Hosfield, E.M.; García, J.J.; Brown, R.A.; Troxell, M.L.; Allison, K.H.; Bean, G.R. Nodular Fasciitis of the Breast: Clinicopathologic and Molecular Characterization with Identification of Novel USP6 Fusion Partners. Mod. Pathol. 2021, 34, 1865–1875. [Google Scholar] [CrossRef]
- Paliogiannis, P.; Cossu, A.; Palmieri, G.; Scognamillo, F.; Pala, C.; Nonnis, R.; Sotgiu, G.; Fois, A.; Palomba, G.; Attene, F. Breast Nodular Fasciitis: A Comprehensive Review. Breast Care 2016, 11, 270–274. [Google Scholar] [CrossRef]
- Lin, W.; Bao, L. Nodular Fasciitis of the Breast: The Report of Three Cases. BMC Women’s Health 2022, 22, 54. [Google Scholar] [CrossRef]
- Lee, K.J.; Jin, W.; Kim, G.Y.; Rhee, S.J.; Park, S.Y.; Park, J.S.; Ryu, K.N. Sonographic Features of Superficial-Type Nodular Fasciitis in the Musculoskeletal System. J. Ultrasound Med. 2015, 34, 1465–1471. [Google Scholar] [CrossRef]
- Knight, J.A.; Hunt, K.N.; Carter, J. Nodular Fasciitis of the Breast in an Elderly Woman. Radiol. Case Rep. 2017, 12, 642–644. [Google Scholar] [CrossRef]
- Shimizu, T.K.; Gibbs, P.; Orrison, S.; Ma, A. Nodular Fasciitis of the Breast. Breast J. 2020, 26, 1054–1055. [Google Scholar] [CrossRef]
- Hayashi, H.; Nishikawa, M.; Watanabe, R.; Sawaki, M.; Kobayashi, H.; Shibata, A.; Kikumori, T.; Nagasaka, T.; Imai, T. Nodular Fasciitis of the Breast. Breast Cancer 2007, 14, 337–339. [Google Scholar] [CrossRef]
- Erinanc, H.; Turk, E. The Rare Benign Lesion That Mimics a Malignant Tumor in Breast Parenchyma: Nodular Fasciitis of the Breast. Case Rep. Pathol. 2018, 2018, 1612587. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.M.; Chou, M.M. USP6-Induced Neoplasms: The Biologic Spectrum of Aneurysmal Bone Cyst and Nodular Fasciitis. Hum. Pathol. 2014, 45, 1–11. [Google Scholar] [CrossRef]
- Hiemcke-Jiwa, L.S.; van Gorp, J.M.; Fisher, C.; Creytens, D.; van Diest, P.J.; Flucke, U. USP6 -Associated Neoplasms: A Rapidly Expanding Family of Lesions. Int. J. Surg. Pathol. 2020, 28, 816–825. [Google Scholar] [CrossRef] [PubMed]
- Kang, A.; Kumar, J.B.; Thomas, A.; Bourke, A.G. A Spontaneously Resolving Breast Lesion: Imaging and Cytological Findings of Nodular Fasciitis of the Breast with FISH Showing USP6 Gene Rearrangement. BMJ Case Rep. 2015, bcr2015213076. [Google Scholar] [CrossRef] [PubMed]
- Oh, B.H.; Kim, J.; Zheng, Z.; Roh, M.R.; Chung, K.Y. Treatment of Nodular Fasciitis Occurring on the Face. Ann. Dermatol. 2015, 27, 694. [Google Scholar] [CrossRef]
- Graham, B.S.; Barrett, T.L.; Goltz, R.W. Nodular Fasciitis: Response to Intralesional Corticosteroids. J. Am. Acad. Dermatol. 1999, 40, 490–492. [Google Scholar] [CrossRef]
- Wargotz, E.S.M.; Weiss, S.W.M.; Norris, H.J.M. Myofibroblastoma of the Breast: Sixteen Cases of a Distinctive Benign Mesenchymal Tumor. Am. J. Surg. Pathol. 1987, 11, 493–502. [Google Scholar] [CrossRef]
- McMenamin, M.E.; Fletcher, C.D.M. Mammary-Type Myofibroblastoma of Soft Tissue: A Tumor Closely Related to Spindle Cell Lipoma. Am. J. Surg. Pathol. 2001, 25, 1022–1029. [Google Scholar] [CrossRef]
- Howitt, B.E.; Fletcher, C.D. Mammary-Type Myofibroblastoma: Clinicopathologic Characterization in a Series of 143 Cases. Am. J. Surg. Pathol. 2016, 40, 361–367. [Google Scholar] [CrossRef]
- Kumar, R.M.S.; Lotfollahzadeh, S. Breast Myofibroblastoma. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: http://www.ncbi.nlm.nih.gov/books/NBK585040/ (accessed on 27 February 2023).
- Hyun, K.J.; Son, J.H.; Kim, W.G. Myofibroblastoma of the Breast in Postmenopausal Women: Two Case Reports with Imaging Findings and Review of the Literature. J. Clin. Ultrasound 2020, 48, 279–282. [Google Scholar] [CrossRef]
- Partridge, S.C.; DeMartini, W.B.; Kurland, B.F.; Eby, P.R.; White, S.W.; Lehman, C.D. Quantitative Diffusion-Weighted Imaging as an Adjunct to Conventional Breast MRI for Improved Positive Predictive Value. Am. J. Roentgenol. 2009, 193, 1716–1722. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, S.; Gucin, Z.; Erdogan, E.B. Epithelioid Myofibroblastoma in an Old-Male Breast: A Case Report with MRI Findings. Case Rep. Radiol. 2015, 2015, 934163. [Google Scholar] [CrossRef] [PubMed]
- Metry, M.; Shaaban, M.; Youssef, M.; Carr, M. Myofibroblastoma of the Breast: Literature Review and Case Report. Case Rep. Oncol. Med. 2016, 2016, 1714382. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zong, S.; Cui, Y.; Yue, Y. Misdiagnosis of Aggressive Fibromatosis of the Abdominal Wall: A Case Report and Literature Review. Medicine 2018, 97, e9925. [Google Scholar] [CrossRef] [PubMed]
- Alman, B.; Attia, S.; Baumgarten, C.; Benson, C.; Blay, J.Y.; Bonvalot, S.; Breuing, J.; Cardona, K.; Casali, P.G.; van Coevorden, F.; et al. The Management of Desmoid Tumours: A Joint Global Consensus-Based Guideline Approach for Adult and Paediatric Patients. Eur. J. Cancer 2020, 127, 96–107. [Google Scholar] [CrossRef]
- Russell, D.H.; Montgomery, E.A.; Susnik, B. Low to Intermediate (Borderline) Grade Breast Spindle Cell Lesions on Needle Biopsy: Diagnostic Approach and Clinical Management. Adv. Anat. Pathol. 2022, 29, 309–323. [Google Scholar] [CrossRef]
- Ha, K.Y.; Deleon, P.; Hamilton, R. Breast Fibromatosis Mimicking Breast Carcinoma. Bayl. Univ. Med. Cent. Proc. 2013, 26, 22–24. [Google Scholar] [CrossRef]
- Kasper, B.; Baumgarten, C.; Bonvalot, S.; Haas, R.; Haller, F.; Hohenberger, P.; Moreau, G.; van der Graaf, W.T.A.; Gronchi, A. Management of Sporadic Desmoid-Type Fibromatosis: A European Consensus Approach Based on Patients’ and Professionals’ Expertise—A Sarcoma Patients EuroNet and European Organisation for Research and Treatment of Cancer/Soft Tissue and Bone Sarcoma Group Initiative. Eur. J. Cancer 2015, 51, 127–136. [Google Scholar] [CrossRef]
- Boland, M.R.; Nugent, T.; Nolan, J.; O’Mahony, J.; O’Keeffe, S.; Gillham, C.C.; Maguire, A.; Geraghty, J.; McCartan, D.; Evoy, D.; et al. Fibromatosis of the Breast: A 10-Year Multi-Institutional Experience and Review of the Literature. Breast Cancer 2021, 28, 168–174. [Google Scholar] [CrossRef]
- Kasper, B.; Dimitrakopoulou-Strauss, A.; Pilz, L.R.; Strauss, L.G.; Sachpekidis, C.; Hohenberger, P. Positron Emission Tomography as a Surrogate Marker for Evaluation of Treatment Response in Patients with Desmoid Tumors under Therapy with Imatinib. BioMed Res. Int. 2013, 2013, 389672. [Google Scholar] [CrossRef]
- Colombo, C.; Miceli, R.; Le Péchoux, C.; Palassini, E.; Honoré, C.; Stacchiotti, S.; Mir, O.; Casali, P.G.; Dômont, J.; Fiore, M.; et al. Sporadic Extra Abdominal Wall Desmoid-Type Fibromatosis: Surgical Resection Can Be Safely Limited to a Minority of Patients. Eur. J. Cancer 2015, 51, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Fiore, M.; Colombo, C.; Radaelli, S.; Callegaro, D.; Palassini, E.; Barisella, M.; Morosi, C.; Baldi, G.G.; Stacchiotti, S.; Casali, P.G.; et al. Hormonal Manipulation with Toremifene in Sporadic Desmoid-Type Fibromatosis. Eur. J. Cancer 2015, 51, 2800–2807. [Google Scholar] [CrossRef] [PubMed]
- Skapek, S.X.; Anderson, J.R.; Hill, D.A.; Henry, D.; Spunt, S.L.; Meyer, W.; Kao, S.; Hoffer, F.A.; Grier, H.E.; Hawkins, D.S.; et al. Safety and Efficacy of High-Dose Tamoxifen and Sulindac for Desmoid Tumor in Children: Results of a Children’s Oncology Group (COG) Phase II Study: Tamoxifen and Sulindac for Desmoid Tumor. Pediatr. Blood Cancer 2013, 60, 1108–1112. [Google Scholar] [CrossRef] [PubMed]
- Gounder, M.M.; Mahoney, M.R.; Van Tine, B.A.; Ravi, V.; Attia, S.; Deshpande, H.A.; Gupta, A.A.; Milhem, M.M.; Conry, R.M.; Movva, S.; et al. Sorafenib for Advanced and Refractory Desmoid Tumors. N. Engl. J. Med. 2018, 379, 2417–2428. [Google Scholar] [CrossRef]
- Kasper, B.; Ratan, R.; Alcindor, T.; Schoeffski, P.; Van Der Graaf, W.T.A.; Wilky, B.A.; Riedel, R.F.; Lim, A.; Smith, L.M.; Moody, S.; et al. LBA2 ‘DeFi: A Phase 3, Randomized Controlled Trial of Nirogacestat versus Placebo for Progressing Desmoid Tumours (DT)’ Presented by Bernd Kasper during Presidential Symposium 1 on Saturday, 10 September, 16:30 to 18:00 CEST in Paris Auditorium. Ann. Oncol. 2022, 33 (Suppl. S7), S1435–S1436. [Google Scholar] [CrossRef]
- Ingley, K.M.; Burtenshaw, S.M.; Theobalds, N.C.; White, L.M.; Blackstein, M.E.; Gladdy, R.A.; Thipphavong, S.; Gupta, A.A. Clinical Benefit of Methotrexate plus Vinorelbine Chemotherapy for Desmoid Fibromatosis (DF) and Correlation of Treatment Response with MRI. Cancer Med. 2019, 8, 5047–5057. [Google Scholar] [CrossRef]
- Garbay, D.; Le Cesne, A.; Penel, N.; Chevreau, C.; Marec-Berard, P.; Blay, J.Y.; Debled, M.; Isambert, N.; Thyss, A.; Bompas, E.; et al. Chemotherapy in Patients with Desmoid Tumors: A Study from the French Sarcoma Group (FSG). Ann. Oncol. 2012, 23, 182–186. [Google Scholar] [CrossRef]
- De Camargo, V.P.; Keohan, M.L.; D’Adamo, D.R.; Antonescu, C.R.; Brennan, M.F.; Singer, S.; Ahn, L.S.; Maki, R.G. Clinical Outcomes of Systemic Therapy for Patients with Deep Fibromatosis (Desmoid Tumor). Cancer 2010, 116, 2258–2265. [Google Scholar] [CrossRef]
- Constantinidou, A.; Jones, R.L.; Scurr, M.; Al-Muderis, O.; Judson, I. Pegylated Liposomal Doxorubicin, an Effective, Well-Tolerated Treatment for Refractory Aggressive Fibromatosis. Eur. J. Cancer 2009, 45, 2930–2934. [Google Scholar] [CrossRef]
- Liu, J.; Ng, D.; Lee, J.; Stalley, P.; Hong, A. Chest Wall Desmoid Tumours Treated with Definitive Radiotherapy: A Plan Comparison of 3D Conformal Radiotherapy, Intensity-Modulated Radiotherapy and Volumetric-Modulated Arc Radiotherapy. Radiat. Oncol. 2016, 11, 34. [Google Scholar] [CrossRef]
- Gronchi, A.; Miah, A.B.; Dei Tos, A.P.; Abecassis, N.; Bajpai, J.; Bauer, S.; Biagini, R.; Bielack, S.; Blay, J.Y.; Bolle, S.; et al. Soft Tissue and Visceral Sarcomas: ESMO–EURACAN–GENTURIS Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up☆. Ann. Oncol. 2021, 32, 1348–1365. [Google Scholar] [CrossRef] [PubMed]
- Pettinato, G.; Manivel, J.C.; De rosa, N.; Dehner, L.P. Inflammatory Myofibroblastic Tumor (Plasma Cell Granuloma): Clinicopathologic Study of 20 Cases with Immunohistochemical and Ultrastructural Observations. Am. J. Clin. Pathol. 1990, 94, 538–546. [Google Scholar] [CrossRef]
- Markopoulos, C.; Charalampoudis, P.; Karagiannis, E.; Antonopoulou, Z.; Mantas, D. Inflammatory Myofibroblastic Tumor of the Breast. Case Rep. Surg. 2015, 2015, 705127. [Google Scholar] [CrossRef] [PubMed]
- Palaskar, S.; Koshti, S.; Maralingannavar, M.; Bartake, A. Inflammatory Myofibroblastic Tumor. Contemp. Clin. Dent. 2011, 2, 274–277. [Google Scholar] [CrossRef] [PubMed]
- Lovly, C.M.; Gupta, A.; Lipson, D.; Otto, G.; Brennan, T.; Chung, C.T.; Borinstein, S.C.; Ross, J.S.; Stephens, P.J.; Miller, V.A.; et al. Inflammatory Myofibroblastic Tumors Harbor Multiple Potentially Actionable Kinase Fusions. Cancer Discov. 2014, 4, 889–895. [Google Scholar] [CrossRef]
- Siraj, F.; Kaur, M.; Dalal, V.; Sonam, J. Inflammatory Myofibroblastic Tumor of the Breast Mimicking Malignancy in an Elderly Male. Ochsner J. 2017, 17, 277–279. [Google Scholar]
- Choi, E.J.; Jin, G.Y.; Chung, M.J.; Moon, W.S.; Youn, H.J. Primary Inflammatory Myofibroblastic Tumors of the Breast with Metastasis: Radiographic and Histopathologic Predictive Factors. J. Breast Cancer 2015, 18, 200–205. [Google Scholar] [CrossRef]
- Ai, H.; Ma, J.; Cheng, X.; Cheng, F. Imaging Findings of Inflammatory Myofibroblastic Tumors in the Breast: A Case Description and Literature Analysis. Quant. Imaging Med. Surg. 2022, 12, 5474–5480. [Google Scholar] [CrossRef]
- Rao, N.; Iwenofu, H.; Tang, B.; Woyach, J.; Liebner, D.A. Inflammatory Myofibroblastic Tumor Driven by Novel NUMA1-ALK Fusion Responds to ALK Inhibition. J. Natl. Compr. Cancer Netw. 2018, 16, 115–121. [Google Scholar] [CrossRef]
- Dimas, D.; Boutas, I.; Potiris, A.; Koufopoulos, N.; Balalis, D.; Sitara, K.; Danglis, F.; Misitzis, I. Dermatofibrosarcoma Protuberans of the Breast: A Case Study. Mol. Clin. Oncol. 2021, 14, 50. [Google Scholar] [CrossRef]
- Malan, M.; Xuejingzi, W.; Quan, S.J. The Efficacy of Mohs Micrographic Surgery over the Traditional Wide Local Excision Surgery in the Cure of Dermatofibrosarcoma Protuberans. Pan Afr. Med. J. 2019, 33, 297. [Google Scholar] [CrossRef] [PubMed]
- Monnier, D.; Vidal, C.; Martin, L.; Danzon, A.; Pelletier, F.; Puzenat, E.; Algros, M.P.; Blanc, D.; Laurent, R.; Humbert, P.H.; et al. Dermatofibrosarcoma Protuberans: A Population-Based Cancer Registry Descriptive Study of 66 Consecutive Cases Diagnosed between 1982 and 2002. J. Eur. Acad. Dermatol. Venereol. 2006, 20, 1237–1242. [Google Scholar] [CrossRef] [PubMed]
- Cabral, R.; Wilford, M.; Ramdass, M. Dermatofibrosarcoma Protuberans Associated with Trauma: A Case Report. Mol. Clin. Oncol. 2020, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Snow, S.N.; Gordon, E.M.; Larson, P.O.; Bagheri, M.M.; Bentz, M.L.; Sable, D.B. Dermatofibrosarcoma Protuberans: A Report on 29 Patients Treated by Mohs Micrographic Surgery with Long-Term Follow-up and Review of the Literature. Cancer 2004, 101, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Dickson, B.C.; Hornick, J.L.; Fletcher, C.D.M.; Demicco, E.G.; Howarth, D.J.; Swanson, D.; Zhang, L.; Sung, Y.-S.; Antonescu, C.R. Dermatofibrosarcoma Protuberans with a Novel COL6A3-PDGFD Fusion Gene and Apparent Predilection for Breast. Genes Chromosom. Cancer 2018, 57, 437–445. [Google Scholar] [CrossRef]
- Frances, C.W.; Escallon, J.; Cukier, M.; Tsang, M.E.; Hameed, U. (Eds.) Surgical Oncology Manual; Springer International Publishing: Cham, Switzerland, 2016. [Google Scholar] [CrossRef]
- Meguerditchian, A.-N.; Wang, J.; Lema, B.; Kraybill, W.G.; Zeitouni, N.C.; Kane, J.M. Wide Excision or Mohs Micrographic Surgery for the Treatment of Primary Dermatofibrosarcoma Protuberans. Am. J. Clin. Oncol. 2010, 33, 300–303. [Google Scholar] [CrossRef] [PubMed]
- Beaziz, J.; Battistella, M.; Delyon, J.; Farges, C.; Marco, O.; Pages, C.; Le Maignan, C.; Da Meda, L.; Basset-Seguin, N.; Resche-Rigon, M.; et al. Long-Term Outcome of Neoadjuvant Tyrosine Kinase Inhibitors Followed by Complete Surgery in Locally Advanced Dermatofibrosarcoma Protuberans. Cancers 2021, 13, 2224. [Google Scholar] [CrossRef]
- Llombart, B.; Serra-Guillén, C.; Monteagudo, C.; Guerrero, J.A.L.; Sanmartín, O. Dermatofibrosarcoma Protuberans: A Comprehensive Review and Update on Diagnosis and Management. Semin. Diagn. Pathol. 2013, 30, 13–28. [Google Scholar] [CrossRef]
- Thakur, V.; Kumar, S.; Aggarwal, D.; Bishnoi, A.; Radotra, B.D. Leiomyoma Cutis of Breast. Breast J. 2020, 26, 1853–1854. [Google Scholar] [CrossRef]
- Sampaio, G.P.; Koch, M.V.; Boechat, M.; Matos, V.E.; Santos, A.A.S.M.D.D. Leiomyoma of the Breast: An Uncommon Tumor. Radiol. Bras. 2016, 49, 343–344. [Google Scholar] [CrossRef]
- Cho, H.J.; Kim, S.H.; Kang, B.J.; Kim, H.; Song, B.J.; Lee, A.W. Leiomyoma of the Nipple Diagnosed by MRI. Acta Radiol. Short Rep. 2012, 1, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Ku, J.; Campbell, C.; Bennett, I. Leiomyoma of the Nipple. Breast J. 2006, 12, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Kafadar, M.T.; Yalçın, M.; Gök, M.A.; Aktaş, A.; Yürekli, T.S.; Arslan, A.İ. Intraparenchymal Leiomyoma of the Breast: A Rare Location for an Infrequent Tumor. Eur. J. Breast Health 2017, 13, 156–158. [Google Scholar] [CrossRef] [PubMed]
- Minami, S.; Matsuo, S.; Azuma, T.; Uga, T.; Hayashi, T.; Eguchi, S.; Kanematsu, T. Parenchymal Leiomyoma of the Breast: A Case Report with Special Reference to Magnetic Resonance Imaging Findings and an Update Review of Literature. Breast Cancer 2011, 18, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Brandão, R.G.; Elias, S.; Nazário, A.C.P.; Assunção, M.D.C.G.A.; Papa, C.C.E.; Facina, G. Leiomyoma of the Breast Parenchyma: A Case Report and Review of the Literature. Sao Paulo Med. J. 2018, 136, 177–181. [Google Scholar] [CrossRef]
- Shah, S.D.; Gupta, A.; Roy, S.; Mukhopadhyay, S. Intraparenchymal Leiomyoma of the Breast: A Case Report. Indian J. Surg. 2013, 75 (Suppl. S1), 88–89. [Google Scholar] [CrossRef]
- Heyer, H.; Ohlinger, R.; Schimming, A.; Schwesinger, G.; Grunwald, S. Parenchymal Leiomyoma of the Breast—Clinical, Sonographic, Mammographic and Histological Features. Ultraschall Der Med.—Eur. J. Ultrasound 2005, 27, 55–58. [Google Scholar] [CrossRef]
- Menko, F.H.; Maher, E.R.; Schmidt, L.S.; Middelton, L.A.; Aittomäki, K.; Tomlinson, I.; Richard, S.; Linehan, W.M. Hereditary Leiomyomatosis and Renal Cell Cancer (HLRCC): Renal Cancer Risk, Surveillance and Treatment. Fam. Cancer 2014, 13, 637–644. [Google Scholar] [CrossRef]
- Long, M.; Hu, X.L.; Zhao, G.; Liu, Y.; Hu, T. Intraparenchymal Breast Leiomyoma and Atypical Leiomyoma. BMC Women’s Health 2022, 22, 119. [Google Scholar] [CrossRef]
- Ngwisanyi, W.; Tshimbidi, G.; Keyter, M.; Beim, C. Nipple-Areolar Complex: Commonest Site of Breast Leiomyoma. South Afr. J. Surg. 2022, 60, 213–215. [Google Scholar] [CrossRef]
- Sherman, J.E.; Smith, J.W. Neurofibromas of the Breast and Nipple-Areolar Area. Ann. Plast. Surg. 1981, 7, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Thompson, S.; Kaplan, S.S.; Poppiti, R.J.; Collado-Mesa, F.; Rabinovich, K. Solitary Neurofibroma of the Breast. Radiol. Case Rep. 2012, 7, 462. [Google Scholar] [CrossRef] [PubMed]
- Ferner, R.E.; OʼDoherty, M.J. Neurofibroma and Schwannoma. Curr. Opin. Neurol. 2002, 15, 679–684. [Google Scholar] [CrossRef] [PubMed]
- Lynn, M.; Krauland, K. Neurofibroma. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: http://www.ncbi.nlm.nih.gov/books/NBK539707/ (accessed on 21 January 2023).
- Yin, C.; Porembka, J.H.; Hwang, H.; Hayes, J.C. Neurofibroma in the Breast: Diagnosis and Management Considerations. J. Breast Imaging 2021, 3, 363–368. [Google Scholar] [CrossRef]
- Rotili, A.; De Maria, F.; Di Venosa, B.; Ghioni, M.; Pizzamiglio, M.; Cassano, E.; Moratti, M. Solitary Breast Neurofibroma: Imaging Aspects. Ecancermedicalscience 2018, 12, 800. [Google Scholar] [CrossRef]
- Bongiorno, M.R.; Doukaki, S.; Aricò, M. Neurofibromatosis of the Nipple-Areolar Area: A Case Series. J. Med. Case Rep. 2010, 4, 22. [Google Scholar] [CrossRef]
- Nasri, S.; Benmoussa, Y.; Abbou, W.; Mirali, H.; Aichouni, N.; Skiker, I. Imaging Appearance of Isolated Diffuse Neurofibroma of Nipple Areolar Area: A Case Report. Pan Afr. Med. J. 2021, 39. [Google Scholar] [CrossRef]
- Higham, C.S.; Dombi, E.; Rogiers, A.; Bhaumik, S.; Pans, S.; Connor, S.E.; Miettinen, M.; Sciot, R.; Tirabosco, R.; Brems, H.; et al. The Characteristics of 76 Atypical Neurofibromas as Precursors to Neurofibromatosis 1 Associated Malignant Peripheral Nerve Sheath Tumors. Neuro-oncology 2018, 20, 818–825. [Google Scholar] [CrossRef]
- Miettinen, M.M.; Antonescu, C.R.; Fletcher, C.D.; Kim, A.; Lazar, A.J.; Quezado, M.M.; Reilly, K.M.; Stemmer-Rachamimov, A.; Stewart, D.R.; Viskochil, D.; et al. Histopathologic Evaluation of Atypical Neurofibromatous Tumors and Their Transformation into Malignant Peripheral Nerve Sheath Tumor in Patients with Neurofibromatosis 1—A Consensus Overview. Hum. Pathol. 2017, 67, 1–10. [Google Scholar] [CrossRef]
- Meyer, A.; Billings, S.D. What’s New in Nerve Sheath Tumors. Virchows Arch. 2020, 476, 65–80. [Google Scholar] [CrossRef]
- Watik, F.; Harrad, M.; Sami, Z.; Mahdaoui, S.; Boufettal, H.; Samouh, N. Breast Neurofibroma: A Case Report. Int. J. Surg. Case Rep. 2022, 98, 107533. [Google Scholar] [CrossRef] [PubMed]
- Bernthal, N.M.; Putnam, A.; Jones, K.B.; Viskochil, D.; Randall, R.L. The Effect of Surgical Margins on Outcomes for Low Grade MPNSTs and Atypical Neurofibroma: Outcomes of Intermediate Nerve Sheath Tumors. J. Surg. Oncol. 2014, 110, 813–816. [Google Scholar] [CrossRef] [PubMed]
- Maani, N.; Westergard, S.; Yang, J.; Scaranelo, A.M.; Telesca, S.; Thain, E.; Schachter, N.F.; McCuaig, J.M.; Kim, R.H. NF1 Patients Receiving Breast Cancer Screening: Insights from The Ontario High Risk Breast Screening Program. Cancers 2019, 11, 707. [Google Scholar] [CrossRef] [PubMed]
- Olivier, L.; Naraynsingh, V.; Hassranah, D.; Cassim, C. Abrikossoff Tumor Clinically Mimicking Carcinoma in Accessory Axillary Breast Tissue. Cureus 2022, 14, e21733. [Google Scholar] [CrossRef] [PubMed]
- Abreu, N.; Filipe, J.; André, S.; Marques, J.C. Granular Cell Tumor of the Breast: Correlations between Imaging and Pathology Findings. Radiol. Bras. 2020, 53, 105–111. [Google Scholar] [CrossRef]
- Moffa, G.; Galati, F.; Panzironi, G.; Rizzo, V.; Kripa, E.; Pediconi, F. Granular Cell Tumor of the Breast: Tip and Tricks on Conventional and Magnetic Resonance Imaging. Breast J. 2021, 27, 178–180. [Google Scholar] [CrossRef]
- Meani, F.; Di Lascio, S.; Wandschneider, W.; Montagna, G.; Vitale, V.; Zehbe, S.; Harder, Y.; Parvex, S.L.; Spina, P.; Canonica, C.; et al. Granular Cell Tumor of the Breast: A Multidisciplinary Challenge. Crit. Rev. Oncol. Hematol. 2019, 144, 102828. [Google Scholar] [CrossRef]
- Daniel, N.; Lannan, F.; Childs, J. Granular Cell Tumor. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: http://www.ncbi.nlm.nih.gov/books/NBK563150/ (accessed on 28 February 2023).
- Bosmans, F.; Dekeyzer, S.; Vanhoenacker, F. Granular Cell Tumor: A Mimicker of Breast Carcinoma. J. Belg. Soc. Radiol. 2021, 105, 18. [Google Scholar] [CrossRef]
- Scaranelo, A.M.; Bukhanov, K.; Crystal, P.; Mulligan, A.M.; O’malley, F.P. Granular Cell Tumour of the Breast: MRI Findings and Review of the Literature. Br. J. Radiol. 2007, 80, 970–974. [Google Scholar] [CrossRef]
- Wang, H.; Feng, D.; Zou, T.; Liu, Y.; Wu, X.; Zou, J.; Huang, R. Contrast-Enhanced Ultrasound of Granular Cell Tumor in Breast: A Case Report with Review of the Literature. Front. Oncol. 2022, 12, 894261. [Google Scholar] [CrossRef]
- Kohashi, T.; Kataoka, T.; Haruta, R.; Sugino, K.; Marubayashi, S.; Yahata, H.; Asahara, T.; Fujii, S.; Arihiro, K.; Dohi, K. Granular Cell Tumor of the Breast: Report of a Case. Hiroshima J. Med. Sci. 1999, 48, 31–33. [Google Scholar] [PubMed]
- Pareja, F.; Brandes, A.H.; Basili, T.; Selenica, P.; Geyer, F.C.; Fan, D.; Da Cruz Paula, A.; Kumar, R.; Brown, D.N.; Gularte-Mérida, R.; et al. Loss-of-Function Mutations in ATP6AP1 and ATP6AP2 in Granular Cell Tumors. Nat. Commun. 2018, 9, 3533. [Google Scholar] [CrossRef] [PubMed]
- Enomoto, A.; Terasaki, M.; Murase, Y.; Kitagawa, Y.; Shimizu, A.; Ohashi, R.; Terasaki, Y. Malignant Granular Cell Tumors: Combining Cytological and Pathological Findings for a Definitive Diagnosis. Diagn. Cytopathol. 2022, 50, E217–E222. [Google Scholar] [CrossRef] [PubMed]
- Dehner, C.A.; Schroeder, M.C.; Lyu, Y.; Bell, R.; Borcherding, D.C.; Moon, T.; Hirbe, A.; Chrisinger, J.S.A. Molecular Characterization of Multifocal Granular Cell Tumors. Am. J. Surg. Pathol. 2022, 47, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Swamy, N.; Jennings, P.; Taylor, R.; Harter, S.B.; Kumarapeli, A.R.; Bryant-Smith, G. Revisiting the Inscrutable Granular Cell Tumors in the Breast and Beyond: An Institutional Experience: The Inscrutable Granular Cell Tumor. Arch. Breast Cancer 2022, 9, 204–212. [Google Scholar] [CrossRef]
- Gultekin, S.H.; Cody, H.S.; Hoda, S.A. Schwannoma of the Breast. South. Med. J. 1996, 89, 238–239. [Google Scholar] [CrossRef] [PubMed]
- Collins, R.; Gau, G. Neurilemmoma presenting as a lump in the breast. Br. J. Surg. 2005, 60, 242–243. [Google Scholar] [CrossRef]
- Dialani, V.; Hines, N.; Wang, Y.; Slanetz, P. Breast Schwannoma. Case Rep. Med. 2011, 2011, 930841. [Google Scholar] [CrossRef]
- Lee, H.S.; Jung, E.J.M.; Kim, J.M.; Kim, J.Y.; Kim, I.K.; Kim, T.H.; Jang, J.Y.; Woo, J.W.; Lee, J.; Park, T.; et al. Schwannoma of the breast presenting as a painful lump. Medicine 2021, 100, e27903. [Google Scholar] [CrossRef]
- Shiryazdi, S.M.; Dahaj, F.S.; Yazdi, A.A.; Shishehbor, F. An uncommon breast lump with the diagnosis of schwannoma. Ann. Surg. 2019, 92, 1–3. [Google Scholar]
- Hamdy, O.; Raafat, S.; Saleh, G.A.; Hamdy, M. Small breast Schwannoma in an old female; A case report. Breast Dis. 2019, 38, 81–83. [Google Scholar] [CrossRef] [PubMed]
- Salihoglu, A.; Esatoglu, S.N.; Eskazan, A.E.; Halac, M.; Aydin, S.O. Breast schwannoma in a patient with diffuse large B-cell lymphoma: A case report. J. Med. Case Rep. 2012, 6, 423. [Google Scholar] [CrossRef] [PubMed]
- Duehrkoop, M.; Frericks, B.; Ankel, C.; Boettcher, C.; Hartmann, W.; Pfitzner, B.M. Two case reports: Breast schwannoma and a rare case of an axillary schwannoma imitating an axillary lymph node metastasis. Radiol. Case Rep. 2021, 16, 2154–2157. [Google Scholar] [CrossRef] [PubMed]
- Xi, X.; Wang, X.; Yue, X.; Chen, Y. Inferior inner quadrant schwannoma of the breast: A rare case report. Asian J. Surg. 2022, 46, 1395–1396. [Google Scholar] [CrossRef] [PubMed]
- Parikh, Y.; Sharma, K.J.; Parikh, S.J.; Hall, D. Intramammary schwannoma: A palpable breast mass. Radiol. Case Rep. 2016, 11, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Halteh, P.; Patel, A.; Eskreis-Winkler, S.; D’Alfonso, T.M. Schwannoma of the breast: A common tumor in an uncommon location. Breast J. 2018, 24, 206–207. [Google Scholar] [CrossRef]
- Fujii, T.; Yajima, R.; Morita, H.; Tsutsumi, S.; Asao, T.; Kuwano, H. A Rare Case of Anterior Chest Wall Schwannoma Masquerading as a Breast Tumor. Int. Surg. 2014, 99, 196–199. [Google Scholar] [CrossRef]
- Ayadi-Kaddour, A.; Helal, I.; Kechaou, S.; El Mezni, F. Diagnosis of breast schwannoma on per-cutaneous breast biopsy. La Tunis. Med. 2015, 93, 479–480. [Google Scholar]
- Ashoor, A.; Lissidini, G.; Girardi, A.; Mirza, M.; Baig, M.S. Breast Shwannoma—Time to explore alternative management strategy? Ann. Diagn. Pathol. 2021, 54, 151773. [Google Scholar] [CrossRef]
- Thejaswini, M.; Padmaja, K.; Srinivasamurthy, V.; Rao, M.S. Solitary intramammary schwannoma mimicking phylloides tumor: Cytological clues in the diagnosis. J. Cytol. 2012, 29, 258–260. [Google Scholar] [CrossRef]
- Datta, S. A Rare Case of Chest Wall Schwannoma with Destruction of Rib, Masquerading as A Breast Mass. J. Clin. Diagn. Res. 2014, 8, FD01–FD02. [Google Scholar] [CrossRef] [PubMed]
- Casey, P.; Stephens, M.; Kirby, R.M. A Rare Cystic Breast Lump-Schwannoma of the Breast. Breast J. 2012, 18, 491–492. [Google Scholar] [CrossRef] [PubMed]
- Yadav, K.K.; Poudel, N.; Acharya, K.; Yadav, R.K.; Pathak, P.; Hirachan, S. Right breast schwannoma in a male: A rare case report. Int. J. Surg. Case Rep. 2022, 99, 107667. [Google Scholar] [CrossRef] [PubMed]
- Patwardhan, U.M.; Vu, M.T.; Soballe, P.W. Multiple Schwannomas in a Patient with Gynecomastia. Breast J. 2017, 23, 360–362. [Google Scholar] [CrossRef]
- Ramdani, H.; El Haddad, S.; Chat, L.; Souadka, A.; Allali, N. Axillary schwannoma mimicking a breast cancer lymph node metastasis. Breast J. 2021, 27, 387–388. [Google Scholar] [CrossRef]
- Vieira, R.A.D.C.; de Oliveira, L.C.N.; Martins, R.M.; Falcão-Junior, P.C. Schwannoma associated with breast cancer mimicking axillary metastasis. Breast J. 2020, 26, 2412–2413. [Google Scholar] [CrossRef]
- Uchida, N.; Yokoo, H.; Kuwano, H. Schwannoma of the Breast: Report of a Case. Surg. Today 2005, 35, 238–242. [Google Scholar] [CrossRef]
- Lissidini, G.; Papa, G.; Girardi, A.; Ashoor, A.A.; Nicosia, L.; Rossi, D.E.; Toesca, A.; Arnone, P.; Caldarella, P.; Veronesi, P. Schwannoma of the axillary region. Imaging findings, clinical pitfalls, and misdiagnosis. Breast J. 2021, 27, 273–275. [Google Scholar] [CrossRef]
- Díaz, P.S.; Martín, M.H.; Cordero, M.S.; Aguilar, M.S. Schwannoma mamario: Un diagnóstico inesperado por resonancia magnética. Radiologia 2018, 60, 85–89. [Google Scholar] [CrossRef]
- Carlson, M.L.; Link, M.J. Vestibular Schwannomas. N. Engl. J. Med. 2021, 384, 1335–1348. [Google Scholar] [CrossRef]
- Johnson, S.; Kano, H.; Faramand, A.; Pease, M.; Nakamura, A.; Hassib, M.; Spencer, D.; Sisterson, N.; Faraji, A.H.; Arai, Y.; et al. Long term results of primary radiosurgery for vestibular schwannomas. J. Neuro-Oncol. 2019, 145, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Kolb, L.; Yarrarapu, S.N.S.; Ameer, M.A.; Rosario-Collazo, J.A. Lipoma. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: http://www.ncbi.nlm.nih.gov/books/NBK507906/ (accessed on 18 February 2023).
- Busbaih, Z.; Saleh, A.A.A.; AlMaghlouth, M.K.; Albeladi, A.M.; Alali, T.; AlGhadeer, M.S.; Odeh, A. Giant Breast Lipoma: A Case Report. Cureus 2022, 14, e22304. [Google Scholar] [CrossRef] [PubMed]
- Bouroumane, M.R.; Khalil, R.; Khalil, H.; Jalal, H. Breast lipoma with central fat necrosis: Case report. Pan Afr. Med. J. 2016, 25, 235. [Google Scholar] [CrossRef] [PubMed]
- Lanng, C.; Eriksen, B.; Hoffmann, J. Lipoma of the breast: A diagnostic dilemma. Breast 2004, 13, 408–411. [Google Scholar] [CrossRef]
- Sutaria, A.M.; Kapoor, A.M.; Sharma, Y.K.M.; Gupta, A.M. Deoxycholic Acid Injection in the Management of Difficult-to-Remove Subcutaneous Lipomas. Dermatol. Surg. 2022, 48, 367–368. [Google Scholar] [CrossRef]
- Ramasamy, K.D.; Jesudass, J.M.; Appaka, C.V.J.K.M.; Tripathee, S.; Sivanesan, S.M. Novel Technique for Obtaining Aesthetic Results in Multiple Lipomatosis Surgery. Plast. Reconstr. Surg.—Glob. Open 2022, 10, e4399. [Google Scholar] [CrossRef]
- Piccolo, D.; Mutlag, M.H.; Pieri, L.; Fusco, I.; Conforti, C.; Crisman, G.; Bonan, P. Lipoma management with a minimally invasive 1,444 nm Nd:YAG laser technique. Front. Med. 2022, 9, 1011468. [Google Scholar] [CrossRef]
- Noel, J.-C.; Van Geertruyden, J.; Engohan-Aloghe, C. Angiolipoma of the Breast in a Male: A Case Report and Review of the Literature. Int. J. Surg. Pathol. 2011, 19, 813–816. [Google Scholar] [CrossRef]
- Howard, W.R. Angiolipoma. Arch. Dermatol. 1960, 82, 924–931. [Google Scholar] [CrossRef]
- Lin, J.J.; Lin, F. Two Entities in Angiolipoma. A Study of 459 Cases of Lipoma with Review of Literature on Infil-trating Angiolipoma. Cancer 1974, 34, 720–727. [Google Scholar] [CrossRef]
- Kravtsov, O.; Techawatanaset, K.; Cherian, S.; Jorns, J.M. Benign vascular lesions and angiolipomas of the breast: Radiologic-pathologic correlation. Breast J. 2020, 26, 1906–1908. [Google Scholar] [CrossRef] [PubMed]
- Kryvenko, O.N.; Chitale, D.; VanEgmond, E.M.; Gupta, N.S.; Schultz, D.; Lee, M.W. Angiolipoma of the Female Breast: Clinicomorphological Correlation of 52 Cases. Int. J. Surg. Pathol. 2011, 19, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Walsh, C.M.; Yang, L.; Park, J.M.; Askeland, R.W.; Fajardo, L.L. Angiolipoma of the Breast in a Transgender Patient. Breast J. 2014, 20, 662–663. [Google Scholar] [CrossRef] [PubMed]
- Dilege, E.; Bozkurt, E.; Kulle, C.B.; Bulutay, P.; Agcaoglu, O. A Rare Tumor of the Male Breast ‘Angiolipoma’ Case Report and Review of Literature. Ann. Ital. Di Chir. 2022, 11, S2239253X22036945. [Google Scholar]
- Zuhair, A.-R.; Maroun, A.-R.; Inna, N. Angiolipoma of the Breast in a Male. Breast J. 2015, 21, 685–686. [Google Scholar] [CrossRef]
- Jain, R.; Bitterman, P.; Lamzabi, I.; Reddy, V.B.; Gattuso, P. Androgen Receptor Expression in Vascular Neoplasms of the Breast. Appl. Immunohistochem. Mol. Morphol. 2014, 22, 132–135. [Google Scholar] [CrossRef]
- Ozturk, M.; Polat, A.V.; Bekci, T.; Sullu, Y. Angiolipoma of the Breast: Multi-modality Imaging Findings. Breast J. 2016, 22, 698–700. [Google Scholar] [CrossRef]
- Sebastiano, C.; Gennaro, L.; Brogi, E.; Morris, E.; Bowser, Z.L.; Antonescu, C.R.; Pareja, F.; Brennan, S.; Murray, M.P. Benign vascular lesions of the breast diagnosed by core needle biopsy do not require excision. Histopathology 2017, 71, 795–804. [Google Scholar] [CrossRef]
- Kaur, N.; Kaushal, V.; Kaushik, R.; Gulati, A. Angiolipoma of the mammary region: A report of two cases. J. Health Spec. 2013, 1, 100. [Google Scholar] [CrossRef]
- Babiss, E.; Cheng, E.; Mema, E. Radiologic and Pathologic Correlation for Angiolipomas of the Breast. J. Breast Imaging 2022, 4, 177–182. [Google Scholar] [CrossRef]
- Johnston, C.C. Hemangioma of the Male Breast: A Case Report. Am. J. Cancer 1936, 27, 341–343. [Google Scholar] [CrossRef]
- Yoga, A.; Lyapichev, K.A.; Baek, D.; Gomez-Fernandez, C.R. Hemangioma of a Male Breast: Case Report and Review of the Literature. Am. J. Case Rep. 2018, 19, 1425–1429. [Google Scholar] [CrossRef] [PubMed]
- Kunimoto, K.; Yamamoto, Y.; Jinnin, M. ISSVA Classification of Vascular Anomalies and Molecular Biology. Int. J. Mol. Sci. 2022, 23, 2358. [Google Scholar] [CrossRef] [PubMed]
- Chou, C.-P.; Huang, J.-S.; Wang, J.-S.; Pan, H.-B. Contrast-enhanced ultrasound features of breast capillary hemangioma: A case report and review of literature. J. Ultrasound 2022, 25, 103–106. [Google Scholar] [CrossRef]
- Aydın, O.U.; Soylu, L.; Ercan, A.I.; Bilezikci, B.; Özbaş, S. Cavernous Hemangioma in the Breast. J. Breast Health 2015, 11, 199–201. [Google Scholar] [CrossRef]
- Zhang, H.; Han, M.; Varma, K.; Dabbs, D.J. Follow-up outcomes of benign vascular lesions of breast diagnosed on core needle biopsy: A study of 117 cases. Breast J. 2019, 25, 401–407. [Google Scholar] [CrossRef]
- Schickman, R.; Leibman, A.; Handa, P.; Kornmehl, A.; Abadi, M. Mesenchymal breast lesions. Clin. Radiol. 2015, 70, 567–575. [Google Scholar] [CrossRef]
- Tuan, H.X.; Duc, N.M.; Huy, N.A.; Tri, C.M.; Quyen, H.-T.D.; Trung, N.T.; Dieu, A.N.; Dung, P.X. Giant breast cavernous hemangioma. Radiol. Case Rep. 2023, 18, 697–700. [Google Scholar] [CrossRef]
- Aslan, Ö.; Oktay, A.; Serin, G.; Yeniay, L.; Aghamirzayev, O. Breast Hemangioma Evaluation with Magnetic Resonance Imaging: A Rare Case Report. Eur. J. Breast Health 2022, 18, 190–194. [Google Scholar] [CrossRef]
- Du, J.; Wang, L.; Wan, C.-F.; Hua, J.; Fang, H.; Chen, J.; Li, F.-H. Differentiating benign from malignant solid breast lesions: Combined utility of conventional ultrasound and contrast-enhanced ultrasound in comparison with magnetic resonance imaging. Eur. J. Radiol. 2012, 81, 3890–3899. [Google Scholar] [CrossRef]
- Frey, J.D.; Levine, P.G.; Darvishian, F.; Shapiro, R.L. Angiosarcoma of the Breast Masquerading as Hemangioma: Exploring Clinical and Pathological Diagnostic Challenges. Arch. Plast. Surg. 2015, 42, 261–263. [Google Scholar] [CrossRef] [PubMed]
- Hoda, S.A.; Cranor, M.L.; Rosen, P.P. Hemangiomas of the Breast With Atypical Histological Features Further Analysis of Histological Subtypes Confirming Their Benign Character. Am. J. Surg. Pathol. 1992, 16, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Mantilla, J.G.; Koenigsberg, T.; Reig, B.; Shapiro, N.; Villanueva-Siles, E.; Fineberg, S. Core Biopsy of Vascular Neoplasms of the Breast. Am. J. Surg. Pathol. 2016, 40, 1424–1434. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.T.; Kirkegaard, D.D.; Bocian, J.J. Angiosarcoma of the Breast. Cancer 1980, 46, 368–371. [Google Scholar] [CrossRef]
- Rupec, M.; Batzenschlager, I. Pseudoangiosarcoma (Masson). A histological study (author’s transl). Z. Fur Hautkrankh. 1981, 56, 1360–1363. [Google Scholar]
- Mesurolle, B.; Sygal, V.; Lalonde, L.; Lisbona, A.; Dufresne, M.-P.; Gagnon, J.H.; Kao, E. Sonographic and Mammographic Appearances of Breast Hemangioma. Am. J. Roentgenol. 2008, 191, W17–W22. [Google Scholar] [CrossRef]
- Salemis, N.S. Sinusoidal hemangioma of the breast: Diagnostic evaluation management and literature review. Gland. Surg. 2017, 6, 105–109. [Google Scholar] [CrossRef]
- Gotland, N.; Loya, A.; Lanng, C.; Rønning, H.; Tvedskov, T.F. Radiation Induced Atypical Vascular Lesion in the Breast. Clin. Breast Cancer 2022, 22, e874–e876. [Google Scholar] [CrossRef]
- Ronen, S.; Ivan, D.; Torres-Cabala, C.A.; Curry, J.L.; Tetzlaff, M.T.; Aung, P.P.; Nagarajan, P.; Suster, S.; Prieto, V.G. Post-radiation vascular lesions of the breast. J. Cutan. Pathol. 2019, 46, 52–58. [Google Scholar] [CrossRef]
- Patton, K.T.; Deyrup, A.T.; Weiss, S.W. Atypical Vascular Lesions After Surgery and Radiation of the Breast. Am. J. Surg. Pathol. 2008, 32, 943–950. [Google Scholar] [CrossRef]
- Fraga-Guedes, C.; Gobbi, H.; Mastropasqua, M.G.; Rocha, R.M.; Botteri, E.; Toesca, A.; Viale, G. Clinicopathological and immunohistochemical study of 30 cases of post-radiation atypical vascular lesion of the breast. Breast Cancer Res. Treat. 2014, 146, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Brenn, T.M.; Fletcher, C.D.M.M. Radiation-Associated Cutaneous Atypical Vascular Lesions and Angiosarcoma: Clinicopathologic Analysis of 42 Cases. Am. J. Surg. Pathol. 2005, 29, 983–996. [Google Scholar] [CrossRef] [PubMed]
- Jaunoo, S.; Thrush, S.; Dunn, P. Pseudoangiomatous stromal hyperplasia (PASH): A brief review. Int. J. Surg. 2011, 9, 20–22. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.N.; Glazebrook, K.N.; Reynolds, C. Pseudoangiomatous Stromal Hyperplasia: Imaging Findings With Pathologic and Clinical Correlation. Am. J. Roentgenol. 2010, 195, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, R.E.; Sciotto, C.G.; Weidner, N. Pseudoangiomatous hyperplasia of mammary stroma. Some observations regarding its clinicopathologic spectrum. Cancer 1989, 63, 1154–1160. [Google Scholar] [CrossRef]
- Badve, S.; Sloane, J. Pseudoangiomatous hyperplasia of male breast. Histopathology 1995, 26, 463–466. [Google Scholar] [CrossRef]
- Surace, A.; Liberale, V.; D’Alonzo, M.; Pecchio, S.; Baù, M.G.; Biglia, N. Pseudoangiomatous Stromal Hyperplasia (PASH) of the Breast: An Uncommon Finding in an Uncommon Patient. Am. J. Case Rep. 2020, 21, e919856-1–e919856-3. [Google Scholar] [CrossRef]
- Anderson, C.; Ricci, A.; Pedersen, C.A.; Cartun, R.W. Immunocytochemical Analysis of Estrogen and Progesterone Receptors in Benign Stromal Lesions of the Breast. Am. J. Surg. Pathol. 1991, 15, 145–149. [Google Scholar] [CrossRef]
- Estes, A.; Cao, L.; Miller, M.E. Pseudoangiomatous stromal hyperplasia: Overview and clinical management. Ann. Breast Surg. 2020, 4, 22. [Google Scholar] [CrossRef]
- Yoon, K.H.; Koo, B.; Lee, K.B.; Lee, H.; Lee, J.; Kim, J.Y.; Park, H.S.; Park, S.; Kim, S.I.; Cho, Y.U.; et al. Optimal treatment of pseudoangiomatous stromal hyperplasia of the breast. Asian J. Surg. 2020, 43, 735–741. [Google Scholar] [CrossRef]
- Parameswaran, P.R.; Renganathan, R.; Subramaniam, P.; Thakur, V. Radiological Spectrum of Pseudoangiomatous Stromal Hyperplasia of Breast—A Case Series. Indian J. Radiol. Imaging 2022, 32, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Drinka, E.K.; Bargaje, A.; Erşahin, H.; Patel, P.; Salhadar, A.; Sinacore, J.; Rajan, P. Pseudoangiomatous Stromal Hyperplasia (PASH) of the Breast. Int. J. Surg. Pathol. 2012, 20, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Degnim, A.C.; Frost, M.H.; Radisky, D.C.; Anderson, S.S.; Vierkant, R.A.; Boughey, J.C.; Pankratz, V.S.; Ghosh, K.; Hartmann, L.C.; Visscher, D.W. Pseudoangiomatous Stromal Hyperplasia and Breast Cancer Risk. Ann. Surg. Oncol. 2010, 17, 3269–3277. [Google Scholar] [CrossRef] [PubMed]
- Tahmasebi, S.; Zadeh, A.K.R.; Zangouri, V.; Akrami, M.; Johari, M.G.; Talei, A. Pseudoangiomatous stromal hyperplasia of the breast: A case report. Clin. Case Rep. 2022, 10, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Raj, S.D.; Sahani, V.G.; Adrada, B.E.; Scoggins, M.E.; Albarracin, C.T.; Woodtichartpreecha, P.; Monetto, F.E.P.; Whitman, G.J. Pseudoangiomatous Stromal Hyperplasia of the Breast: Multimodality Review With Pathologic Correlation. Curr. Probl. Diagn. Radiol. 2017, 46, 130–135. [Google Scholar] [CrossRef]
- Nia, E.S.; Adrada, B.E.; Whitman, G.J.; Candelaria, R.P.; Krishnamurthy, S.; Bassett, R.L.; Arribas, E.M. MRI features of pseudoangiomatous stromal hyperplasia with histopathological correlation. Breast J. 2021, 27, 242–247. [Google Scholar] [CrossRef]
- Rao, R.; Ludwig, K.; Bailey, L.; Berry, T.S.; Buras, R.; Degnim, A.; Fayanju, O.M.; Froman, J.; Golesorkhi, N.; Greenburg, C.; et al. Select Choices in Benign Breast Disease: An Initiative of the American Society of Breast Surgeons for the American Board of Internal Medicine Choosing Wisely®® Campaign. Ann. Surg. Oncol. 2018, 25, 2795–2800. [Google Scholar] [CrossRef]






| Tumor Type | Presentation | Imaging Appearance | Biopsy | Pathology | Molecular Markers | Management | Prognosis |
|---|---|---|---|---|---|---|---|
| Nodular Fasciitis | Broad age range (20–80 years) Painless Rapid Growth Trauma 10–15% | US: hypoechoic, spiculated MG: hyperdense with indistinct margins | CNB may be sufficient with concordance and expert pathology Excisional biopsy usually needed |
| Positive: SMA FISH: + USP6 fusion gene (MYH9) | Excision—No research on required margins Increasing evidence to support observation of intra-lesional steroids (stemming from extra-mammary sources) | No metastases Low risk for recurrence |
Common Differentials and Features Differentiating them from NF:
| |||||||
| Myofibro-blastoma | 50–60 years old Male predominance Painless Slow-growing | US: well-circumscribed, homogenous, hyperechoic MG: well-circumscribed, coarse calcifications MRI: hyperintense on T2 and homogenous with septations | FNA insufficient CNB is usually sufficient Excisional biopsies rarely needed |
| Positive: Desmin, CD34 (often co-expressed) Variably positive: CD10CD99, ER/PR, H-caldesmon Negative: S100, HMB45, EMA, pancyotkeratin Loss of RB1 expression (deletion on chromosome 13) | Local excision No studies on observation—natural history unknown | Two case reports of local recurrence No metastases |
Common Differentials and Features Differentiating them from Myofibroblastoma:
| |||||||
| Fibromatosis | 30–40 years old Painless Mobile Skin changes and nipple changes common | US: poorly defined, hypoechoic with echogenic rims and posterior shadows MG: high density, spiculated, rarely calcified MRI: report larger sizes than US/MG (should be the primary diagnostic method) | FNA insufficient CNB almost always sufficient Excisional biopsy only if review by expert pathologist is inconclusive |
| Positive: Beta-katenin mutation SMA (Weak, focal) Variably positive: Desmin, S100, CD34 Negative: Cytokeratin, p63, ER/PR | Active surveillance: MRI (or CT) every 3–6months for 1–2 years. If progression is noted proceed with medical management. Tyrosine kinase inhibitors OR methotrexate with vinorelbine If ongoing progression, change medical management or consider radiation. Surgery is a last resort. Tumor will usually recur and surgery is deforming. | Variable depending on treatment regimen Recurrence extremely common with resection |
Common Differentials and Features Differentiating them from Fibromatosis:
| |||||||
| Tumor Type | Presentation | Imaging Appearance | Biopsy | Pathology | Molecular Markers | Management | Prognosis |
|---|---|---|---|---|---|---|---|
| IMT | Young women Painless Slow-growing | US: lobulated, hypoechoic MG: hyperdense, calcifications may occur MRI: unclear margins, lobulated, rapid enhancement | CNB usually sufficient Excisional biopsy should be done with wide margins if diagnosis is suspected |
| Positive: SMA, MSA, vimentin, desmin Stain ALK1—positive in 50–60% can confirm diagnosis If ALK1 negative, ROS1/NTRK3 stain can confirm diagnosis Variably positive: cytokeratins Negative: p63, CD117, CD34, S100 | Wide local excision with negative margins No evidence to support axillary surgery Extra-mammary cases have support from ALK inhibitors – consider in aggressive disease | Rare reports of metastases Up to 25% recurrence rates |
Common Differentials and Features Differentiating them from IMT:
| |||||||
| DFSP | 20–30years old Slow-growing Painless Plaque/papule on the skin, centered in the dermis | US: parallel to the skin, plaque MG: hyperdense with no calcifications Note: can appear parenchymal on imaging | Biopsy: CNB or punch biopsy Excisional could also be considered |
| Positive: CD34, WT1 Negative: keratin, S100, SMA, desmin 90% have translocation t (17:22) from fusion of COL1A1 with PDFGB | Wide local excision No indication for axillary surgery Moh’s microsurgery is controversial and not useful in the breast Limited sensitivity to chemotherapy and radiation Imatinib can be considered (borderline resectable) | 2–25% recurrence rates Metastasis occurs only with fibrosarcomatous progression (FS-DFSP)—occurs in 10–14% |
Common Differentials and Features Differentiating them from DFSP:
| |||||||
| Tumor Type | Presentation | Imaging Appearance | Pathology | Molecular Markers | Management | Prognosis |
|---|---|---|---|---|---|---|
| Leiomyoma | 40–50 years old Slow-growing Painful—especially with cold and palpation | US: solid, homogenous, hypoechoic and well-circumscribed MG: homogenous dense lesions with well-defined margins and no calcifications MRI: well-circumscribed, whorl-appearing, low T1 intensity and low-intermediate T2 intensity with gradual enhancement |
| Positive: desmin, SMA, h-caldesmon Negative: CD34, p63, S100, keratins | Multiple leiomyomas: test for HLRCC syndrome Wide excision to negative margins (most described) | Natural history in the breast is poorly understood Considered similar to extra-mammary locations: indolent, non-aggressive No recurrences, malignant transformation |
| Neurofibroma | 20–30 years old Male and female Often in NAC or pectoralis fascia Usually associated with NF1 | US: superficial, circumscribed, hypoechoic nodules MG: hyperdense, well-circumscribed MRI: hypo- or iso- intense on T1 and hyperintesnse and heterogenous on T2 |
| Positive: S100 and SOX10 Variably positive: CD34 | Excision to negative margins Margins impact recurrences (for atypical lesions) Refer all for genetic counselling (assess for NF1) | Few local recurrences Note: NF1 patients have two times the lifetime increased risk of epithelial breast cancer |
| GCT | Painless, firm masses Upper inner quadrants ¼ identified through screening | US: hypoechoic with irregular borders MG: spiculated distortions without calcifications MRI: low T1 intensity, difficult to visualize on T2, variably enhancing PET: useful for differentiating benign GCTs from malignant |
| Positive: S100, SOX10 and CD 68 | Excision to negative margins | Local recurrences
Surveillance recommended but no evidence for frequency and duration |
| Schwannoma | Rare in the breast Pain to palpation of a mass Associated with NF2 | US: variable due to areas of degeneration or hemorrhage MG: variable, may be occult MRI: isointense on T1 and heterogenous on T2 |
| Positive: S100 and SOX10 suspect malignancy with loss of p16 | Surgical enucleation is usually sufficient Extra-mammary evidence for gamma knife surgery | Local recurrences possible No metastases Rare malignant transformation |
| Leiomyoma | 40–50 years old Slow-growing Painful—especially with cold and palpation | US: solid, homogenous, hypoechoic and well-circumscribed MG: homogenous dense lesions with well-defined margins and no calcifications MRI: well-circumscribed, whorl-appearing, low T1 intensity and low-intermediate T2 intensity with gradual enhancement |
| Positive: desmin, SMA, h-caldesmon Negative: CD34, p63, S100, keratins | Multiple leiomyomas: test for HLRCC syndrome Wide excision to negative margins (most described) | Natural history in the breast is poorly understood Considered similar to extra-mammary locations: indolent, non-aggressive No recurrences, malignant transformation |
| Neurofibroma | 20–30 years old Male and female Often in NAC or pectoralis fascia Usually associated with NF1 | US: superficial, circumscribed, hypoechoic nodules MG: hyperdense, well-circumscribed MRI: hypo- or iso- intense on T1 and hyperintesnse and heterogenous on T2 |
| Positive: S100 and SOX10 Variably positive: CD34 | Excision to negative margins Margins impact recurrences (for atypical lesions) Refer all for genetic counselling (assess for NF1) | Few local recurrences Note: NF1 patients have two times the lifetime increased risk of epithelial breast cancer |
| GCT | Painless, firm masses Upper inner quadrants ¼ identified through screening | US: hypoechoic with irregular borders MG: spiculated distortions without calcifications MRI: low T1 intensity, difficult to visualize on T2, variably enhancing PET: useful for differentiating benign GCTs from malignant |
| Positive: S100, SOX10 and CD 68 | Excision to negative margins | Local recurrences
Surveillance recommended but no evidence for frequency and duration |
| Schwannoma | Rare in the breast Pain to palpation of a mass Associated with NF2 | US: variable due to areas of degeneration or hemorrhage MG: variable, may be occult MRI: isointense on T1 and heterogenous on T2 |
| Positive: S100 and SOX10 suspect malignancy with loss of p16 | Surgical enucleation is usually sufficient Extra-mammary evidence for gamma knife surgery | Local recurrences possible No metastases Rare malignant transformation |
| Lipoma | Most common tumor of human body 30–50years old Risk factors: obesity, dyslipidemia, diabetes Slow-growing masses | US: hypoechoic and avascular MG: radiolucent with a thin capsule with calcifications Imaging is indicated in mammary lipomas (not always necessary extra-mammary locations) | CNB indicated if imaging is not classic. Challenging due to adjacent adipose tissue Normal adipose tissue with small nuclei, interspersed septa Many histologic subtypes | Observation Weight loss may decrease size Injections of deoxycholate injections decreases size by 75% Removal to rule out liposarcoma (size, growth pattern, pain and fixation) The entire capsule should be removed if excising. | No metastases Recurrences may occur, if excision incomplete | |
| Angiolipoma | 50–70 years old More common in women Painless singular mass Often screen detected | US: well circumscribed, homogenous and hyperechoic MG: occult or circumscribed isodense, no calcifications MRI: low signal intensity on T1 and high signal intensity on T2 | CNB is usually sufficient Mature adipose tissue Branching capillary vessels, clustered at the periphery Hyaline microthrombi | Positive: CD34, CD31, ER, S100, androgen receptor Focally positive: SMA | Excision not necessary with radio-pathologic concordance Undefined surveillance strategy Cellular subtype of angiolipoma—excision is indicated to rule out low grade angiosarcoma | No history of malignant transformation or recurrence |
| Hemangioma | 50 years old Female predilection Seen in 11% of autopsies Superficial palpable masses with skin discoloration Often incidental on screening mammography | US: variable definitions, difficult to differentiate from complex cysts or fibroadenomas MG: non-specific, well-circumscribed, can have calcifications related to phleboliths MRI: circumscribed masses with fibrous septa, fast enhancement and washout | Expect bleeding with biopsy FNA inconclusive and hypocellular CNB usually needed Dilated vascular spaces with thin-walled venous vessels | Rarely useful—very similar to angiosarcoma | Excision indicated- to rule out angiosarcoma and for risk of malignant transformation Note: much of this comes from older literature. More studies are needed. If not excising, should have radio-pathologic concordance and should be on surveillance. | Low malignant transformation No metastases |
| Atypical Vascular Lesion | 50 years old Must have history of radiation Single of multiple purple or brown papules Usually <5 mm | Usually uninformative | CNB or punch biopsy suggested Anastomosing lymphatic or capillary vessels in the dermis Flat to hobnailed endothelial cells Hyperchromatic nuclei | c-myc has 100% specificity but 80–90% sensitivity | Excise to negative margins | 10–20% recurrence rates Malignant transformation is rare, but th field defect from radiation exposure confers a higher risk of angiosarcoma |
| Pseudo-angiomatous Stromal Hyperplasia | Pre-menopausal women Risk factors: hormonal exposure including contraceptives, pregnancy, hormone replacement, gynaecomastia | Incidental PASH: occult Nodular PASH: US: hypoechoic, well circumscribed MG: hyperdense, well circumscribed Diffuse: heterogenous, lace-like on US | FNA is often acellular and not useful CNB are adequate—no evidence that it underestimates angiosarcoma as PASH Complex inter-anastomosing channels with spindle cells No erythrocytes In true vascular spaces | Positive: CD34, PR and AR Variably positive: desmin, vimentin, SMA | Most lesions can be observed (no clear surveillance regimen) Surgical excision for PASH > 3 cm, radio-pathologic discordance or serial enlargement No consensus on margins | No malignant transformation Recurrence rates 9–22% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Azam, R.; Mrkonjic, M.; Gupta, A.; Gladdy, R.; Covelli, A.M. Mesenchymal Tumors of the Breast: Fibroblastic/Myofibroblastic Lesions and Other Lesions. Curr. Oncol. 2023, 30, 4437-4482. https://doi.org/10.3390/curroncol30050338
Azam R, Mrkonjic M, Gupta A, Gladdy R, Covelli AM. Mesenchymal Tumors of the Breast: Fibroblastic/Myofibroblastic Lesions and Other Lesions. Current Oncology. 2023; 30(5):4437-4482. https://doi.org/10.3390/curroncol30050338
Chicago/Turabian StyleAzam, Riordan, Miralem Mrkonjic, Abha Gupta, Rebecca Gladdy, and Andrea M. Covelli. 2023. "Mesenchymal Tumors of the Breast: Fibroblastic/Myofibroblastic Lesions and Other Lesions" Current Oncology 30, no. 5: 4437-4482. https://doi.org/10.3390/curroncol30050338
APA StyleAzam, R., Mrkonjic, M., Gupta, A., Gladdy, R., & Covelli, A. M. (2023). Mesenchymal Tumors of the Breast: Fibroblastic/Myofibroblastic Lesions and Other Lesions. Current Oncology, 30(5), 4437-4482. https://doi.org/10.3390/curroncol30050338






