Poor Efficacy of Immune Checkpoint Inhibitors Plus Chemotherapy in Lung Cancer Patients with EGFR/ERBB2 Exon 20 Insertion
Abstract
:1. Introduction
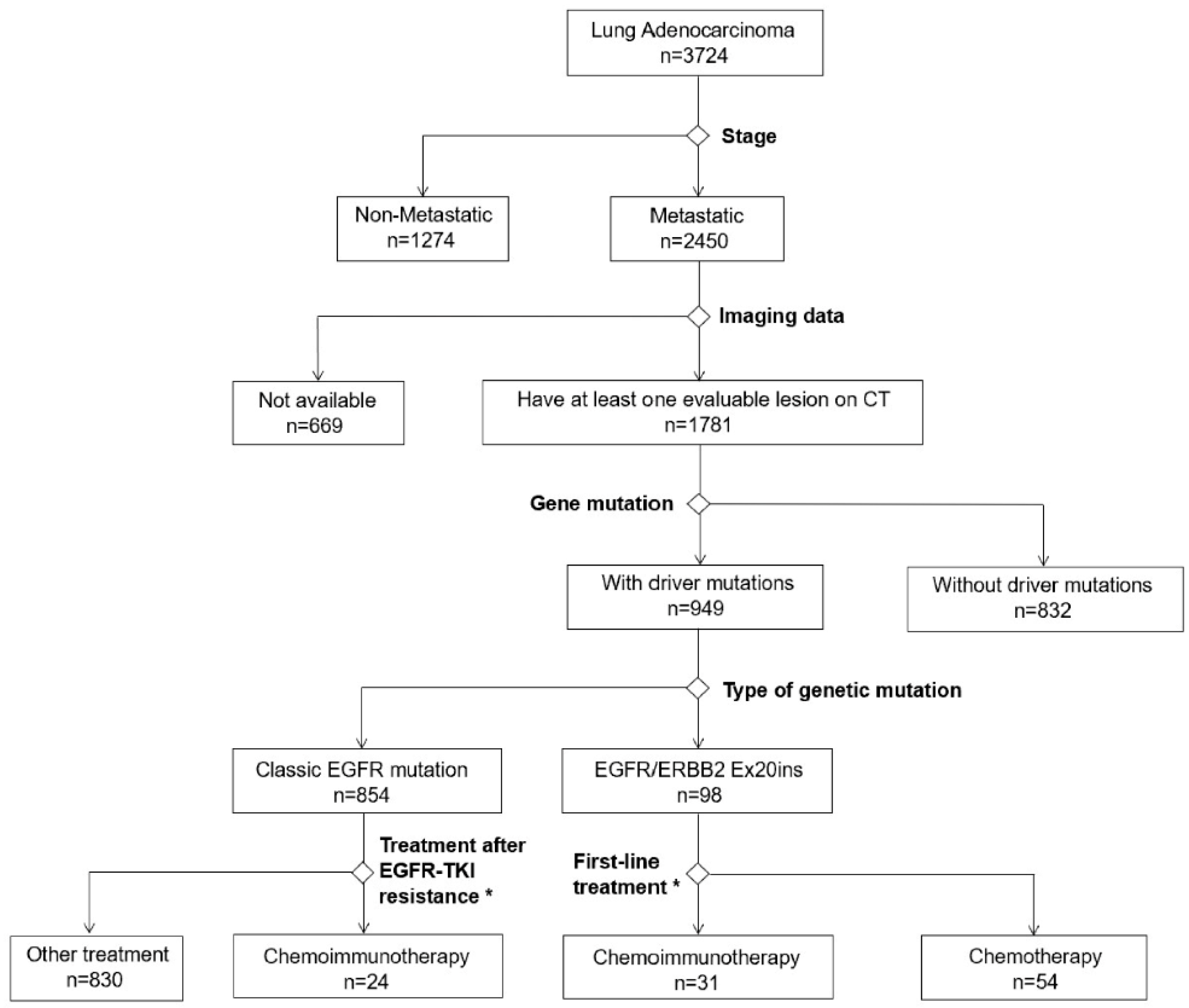
2. Methods
2.1. Patients
2.2. Treatments
2.3. Genetic and PD-L1 Testing
2.4. Response Assessment
2.5. Statistical Analyses
3. Results
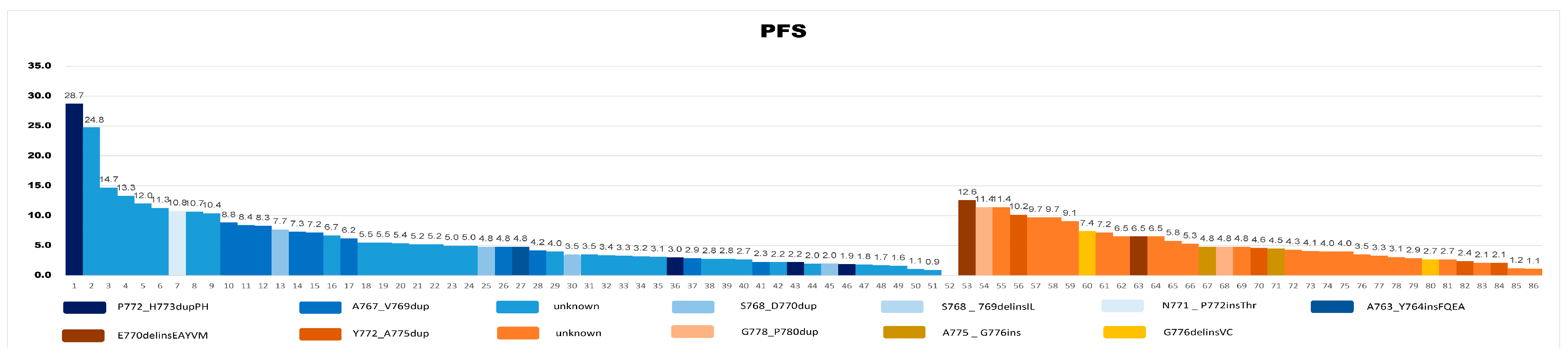
3.1. Genetic Aberrations in EGFR or ERBB2 Ex20ins
3.2. EGFR/ERBB2 Ex20ins Showed Poor Responses to Immunochemotherapy
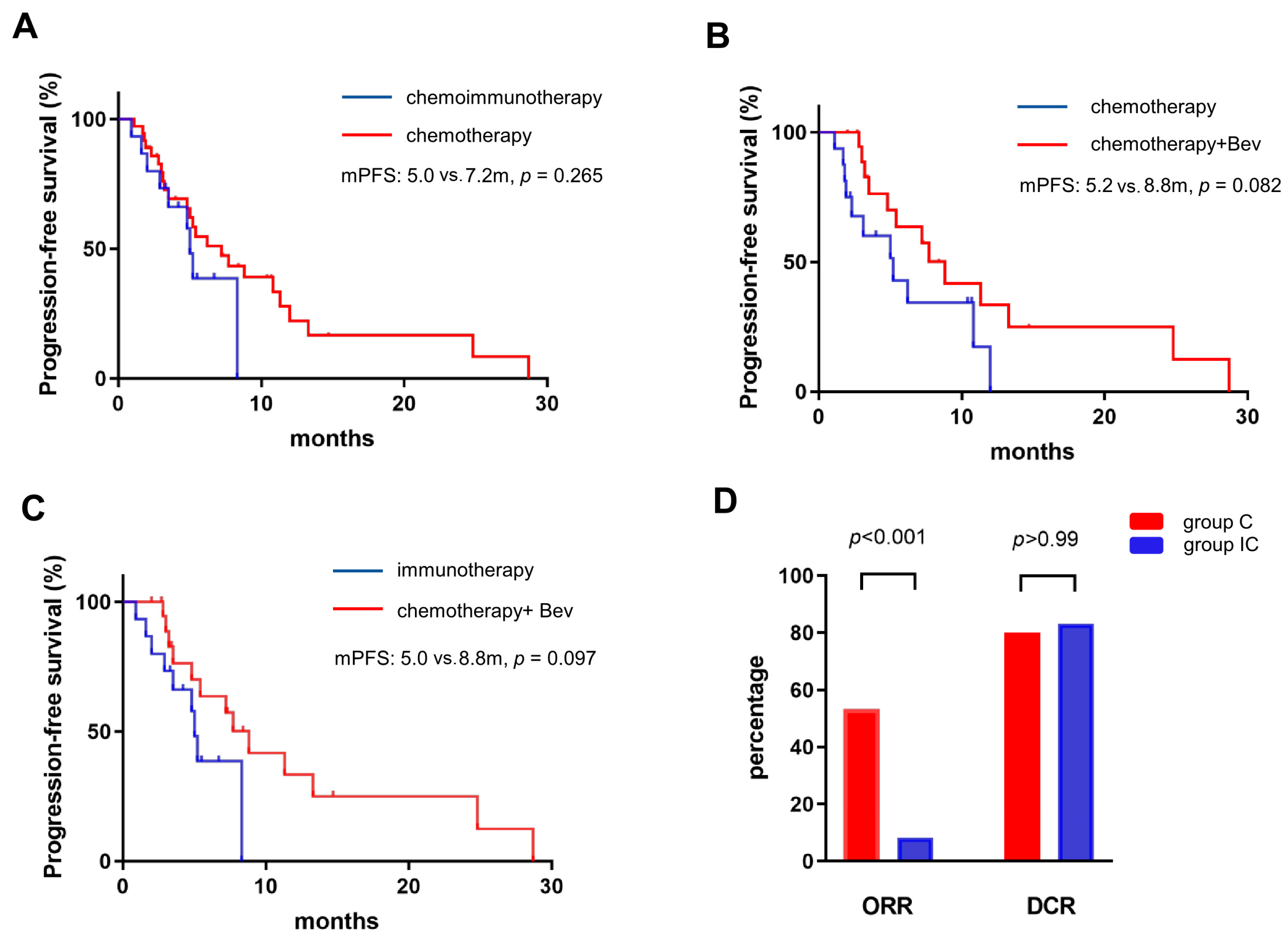
3.3. Survival Analysis for EGFR/ERBB2 Ex20ins
3.4. Chemo- or Immunochemo-Therapy for EGFR Ex20ins
3.5. Chemo- or Immunochemo-Therapy for ERBB2 Ex20ins
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yasuda, H.; Kobayashi, S.; Costa, D.B. EGFR exon 20 insertion mutations in non-small-cell lung cancer: Preclinical data and clinical implications. Lancet Oncol. 2012, 13, e23–e31, Erratum in: Lancet Oncol. 2011, 12, 1182. [Google Scholar] [CrossRef] [PubMed]
- Riess, J.W.; Gandara, D.R.; Frampton, G.M.; Madison, R.; Peled, N.; Bufill, J.A.; Dy, G.K.; Ou, S.I.; Stephens, P.J.; McPherson, J.D.; et al. Diverse EGFR Exon 20 Insertions and Co-Occurring Molecular Alterations Identified by Comprehensive Genomic Profiling of NSCLC. J. Thorac. Oncol. 2018, 13, 1560–1568. [Google Scholar] [CrossRef] [PubMed]
- Cardona, A.F.; Rojas, L.; Zatarain-Barrón, Z.L.; Freitas, H.C.; Granados, S.T.; Castillo, O.; Oblitas, G.; Corrales, L.; Castro, C.D.; Ruiz-Patiño, A.; et al. EGFR exon 20 insertion in lung adenocarcinomas among Hispanics (geno1.2-CLICaP). Lung Cancer 2018, 125, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Li, J.; Xu, H.; Yang, Y.; Yang, L.; Xu, F.; Xia, B.; Zhu, V.W.; Nagasaka, M.; Yang, Y.; et al. EGFR exon 20 insertion mutations in Chinese advanced non-small cell lung cancer patients: Molecular heterogeneity and treatment outcome from nationwide real-world study. Lung Cancer 2020, 145, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Mazières, J.; Peters, S.; Lepage, B.; Cortot, A.B.; Barlesi, F.; Beau-Faller, M.; Besse, B.; Blons, H.; Mansuet-Lupo, A.; Urban, T.; et al. Lung cancer that harbors an HER2 mutation: Epidemiologic characteristics and therapeutic perspectives. J. Clin. Oncol. 2013, 31, 1997–2003. [Google Scholar] [CrossRef]
- Lau, S.C.M.; Fares, A.F.; Le, L.W.; Mackay, K.M.; Soberano, S.; Chan, S.W.; Smith, E.; Ryan, M.; Tsao, M.S.; Bradbury, P.A.; et al. Subtypes of EGFR- and HER2-Mutant Metastatic NSCLC Influence Response to Immune Checkpoint Inhibitors. Clin. Lung Cancer 2021, 22, 253–259. [Google Scholar] [CrossRef]
- Prelaj, A.; Bottiglieri, A.; Proto, C.; Lo Russo, G.; Signorelli, D.; Ferrara, R.; Galli, G.; De Toma, A.; Viscardi, G.; Brambilla, M.; et al. Poziotinib for EGFR and HER2 exon 20 insertion mutation in advanced NSCLC: Results from the expanded access program. Eur. J. Cancer 2021, 149, 235–248. [Google Scholar] [CrossRef]
- Leal, J.L.; Alexander, M.; Itchins, M.; Wright, G.M.; Kao, S.; Hughes, B.G.M.; Pavlakis, N.; Clarke, S.; Gill, A.J.; Ainsworth, H.; et al. EGFR Exon 20 Insertion Mutations: Clinicopathological Characteristics and Treatment Outcomes in Advanced Non-Small Cell Lung Cancer. Clin. Lung Cancer 2021, 22, e859–e869. [Google Scholar] [CrossRef]
- Stephens, P.; Hunter, C.; Bignell, G.; Edkins, S.; Davies, H.; Teague, J.; Stevens, C.; O’Meara, S.; Smith, R.; Parker, A.; et al. Lung cancer: Intragenic ERBB2 kinase mutations in tumours. Nature 2004, 431, 525–526. [Google Scholar] [CrossRef]
- Tian, P.; Zeng, H.; Ji, L.; Ding, Z.; Ren, L.; Gao, W.; Fan, Z.; Li, L.; Le, X.; Li, P.; et al. Lung adenocarcinoma with ERBB2 exon 20 insertions: Comutations and immunogenomic features related to chemoimmunotherapy. Lung Cancer 2021, 160, 50–58. [Google Scholar] [CrossRef]
- Recondo, G.; Facchinetti, F.; Olaussen, K.A.; Besse, B.; Friboulet, L. Making the first move in EGFR-driven or ALK-driven NSCLC: First-generation or next-generation TKI? Nat. Rev. Clin. Oncol. 2018, 15, 694–708. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.J.; Li, J.; Xu, H.Y.; Sun, Y.; Liu, L.; Li, H.S.; Yang, L.; Zhang, Y.; Li, G.H.; Wang, Y. Osimertinib for Chinese advanced non-small cell lung cancer patients harboring diverse EGFR exon 20 insertion mutations. Lung Cancer 2021, 152, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.P.; Aredo, J.V.; Padda, S.K.; Ramchandran, K.J.; Wakelee, H.A.; Das, M.S.; Neal, J.W. EGFR exon 20 Insertion NSCLC and Response to Platinum-Based Chemotherapy. Clin. Lung Cancer 2022, 23, e148–e153. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.W.; Wang, W.X.; Wang, D.; Wang, Q.M.; Pu, X.X.; Zhu, Y.C.; Huang, J.H.; Yu, Z.Y.; Cui, Z.L.; Chen, X.H.; et al. Pemetrexed-based chemotherapy for non-small-cell lung cancer patients with EGFR exon 20 insertion mutation: A multicenter study. Transl. Lung Cancer Res. 2020, 9, 1853–1861. [Google Scholar] [CrossRef] [PubMed]
- Chelabi, S.; Mignard, X.; Leroy, K.; Monnet, I.; Brosseau, S.; Theou-Anton, N.; Massiani, M.-A.; Friard, S.; Duchemann, B.; Fabre, E.; et al. EGFR Exon 20 Insertion in Metastatic Non-Small-Cell Lung Cancer: Survival and Clinical Efficacy of EGFR Tyrosine-Kinase Inhibitor and Chemotherapy. Cancers 2021, 13, 5132. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, L.; Rodríguez-Abreu, D.; Gadgeel, S.; Esteban, E.; Felip, E.; De Angelis, F.; Domine, M.; Clingan, P.; Hochmair, M.J.; Powell, S.F.; et al. KEYNOTE-189 Investigators. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 378, 2078–2092. [Google Scholar] [CrossRef]
- Mok, T.S.K.; Wu, Y.L.; Kudaba, I.; Kowalski, D.M.; Cho, B.C.; Turna, H.Z.; Castro, G., Jr. Srimuninnimit, V.; Laktionov, K.K.; Bondarenko, I.; et al. KEYNOTE-042 Investigators. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): A randomised, open-label, controlled, phase 3 trial. Lancet 2019, 393, 1819–1830. [Google Scholar] [CrossRef]
- Metro, G.; Baglivo, S.; Bellezza, G.; Mandarano, M.; Gili, A.; Marchetti, G.; Toraldo, M.; Molica, C.; Reda, M.S.; Tofanetti, F.R.; et al. Sensitivity to Immune Checkpoint Blockade in Advanced Non-Small Cell Lung Cancer Patients with EGFR Exon 20 Insertion Mutations. Genes 2021, 12, 679. [Google Scholar] [CrossRef]
- Chen, K.; Pan, G.; Cheng, G.; Zhang, F.; Xu, Y.; Huang, Z.; Fan, Y. Immune microenvironment features and efficacy of PD-1/PD-L1 blockade in non-small cell lung cancer patients with EGFR or HER2 exon 20 insertions. Thorac. Cancer 2021, 12, 218–226. [Google Scholar] [CrossRef]
- Hastings, K.; Yu, H.A.; Wei, W.; Sanchez-Vega, F.; DeVeaux, M.; Choi, J.; Rizvi, H.; Lisberg, A.; Truini, A.; Lydon, C.A.; et al. EGFR mutation subtypes and response to immune checkpoint blockade treatment in non-small-cell lung cancer. Ann. Oncol. 2019, 30, 1311–1320. [Google Scholar] [CrossRef]
- Saalfeld, F.C.; Wenzel, C.; Christopoulos, P.; Merkelbach-Bruse, S.; Reissig, T.M.; Laßmann, S.; Thiel, S.; Stratmann, J.A.; Marienfeld, R.; Berger, J.; et al. Efficacy of Immune Checkpoint Inhibitors Alone or in Combination With Chemotherapy in NSCLC Harboring ERBB2 Mutations. J. Thorac. Oncol. 2021, 16, 1952–1958. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Xian, X.; Tian, P.; Li, W.; Wang, K.; Li, Y. Efficacy of Combination Chemo-Immunotherapy as a First-Line Treatment for Advanced Non-Small-Cell Lung Cancer Patients With HER2 Alterations: A Case Series. Front. Oncol. 2021, 11, 633522. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wang, Z.; Fang, J.; Yu, Q.; Han, B.; Cang, S.; Chen, G.; Mei, X.; Yang, Z.; Ma, R.; et al. Efficacy and Safety of Sintilimab Plus Pemetrexed and Platinum as First-Line Treatment for Locally Advanced or Metastatic Nonsquamous NSCLC: A Randomized, Double-Blind, Phase 3 Study (Oncology pRogram by InnovENT anti-PD-1-11). J. Thorac. Oncol. 2020, 15, 1636–1646. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Yang, G.; Xu, H.; Yang, L.; Qiu, W.; Wang, Y. Treatment outcome and clinical characteristics of HER2 mutated advanced non-small cell lung cancer patients in China. Thorac. Cancer 2020, 11, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Guisier, F.; Dubos-Arvis, C.; Viñas, F.; Doubre, H.; Ricordel, C.; Ropert, S.; Janicot, H.; Bernardi, M.; Fournel, P.; Lamy, R.; et al. Efficacy and Safety of Anti-PD-1 Immunotherapy in Patients With Advanced NSCLC With BRAF, HER2, or MET Mutations or RET Translocation: GFPC 01-2018. J. Thorac. Oncol. 2020, 15, 628–636. [Google Scholar] [CrossRef]
- Zhou, C.; Chen, G.; Huang, Y.; Zhou, J.; Lin, L.; Feng, J.; Wang, Z.; Shu, Y.; Shi, J.; Hu, Y.; et al. CameL Study Group. Camrelizumab plus carboplatin and pemetrexed versus chemotherapy alone in chemotherapy-naive patients with advanced non-squamous non-small-cell lung cancer (CameL): A randomised, open-label, multicentre, phase 3 trial. Lancet Respir. Med. 2021, 9, 305–314. [Google Scholar] [CrossRef]
- Lu, S.; Wang, J.; Yu, Y.; Yu, X.; Hu, Y.; Ai, X.; Ma, Z.; Li, X.; Zhuang, W.; Liu, Y.; et al. Tislelizumab Plus Chemotherapy as First-Line Treatment for Locally Advanced or Metastatic Nonsquamous NSCLC (RATIONALE 304): A Randomized Phase 3 Trial. J. Thorac. Oncol. 2021, 16, 1512–1522. [Google Scholar] [CrossRef]
- Choudhury, N.J.; Schoenfeld, A.J.; Flynn, J.; Falcon, C.J.; Rizvi, H.; Rudin, C.M.; Kris, M.G.; Arcila, M.E.; Heller, G.; Yu, H.A.; et al. Response to Standard Therapies and Comprehensive Genomic Analysis for Patients with Lung Adenocarcinoma with EGFR Exon 20 Insertions. Clin. Cancer Res. 2021, 27, 2920–2927. [Google Scholar] [CrossRef]
- Gonzalvez, F.; Vincent, S.; Baker, T.E.; Gould, A.E.; Li, S.; Wardwell, S.D.; Nadworny, S.; Ning, Y.; Zhang, S.; Huang, W.S.; et al. Mobocertinib (TAK-788): A Targeted Inhibitor of EGFR Exon 20 Insertion Mutants in Non-Small Cell Lung Cancer. Cancer Discov. 2021, 11, 1672–1687. [Google Scholar] [CrossRef]
- Geng, D.; Guo, Q.; Huang, S.; Zhang, H.; Guo, S.; Li, X. Clinical and molecular characteristics of epidermal growth factor receptor exon 20 insertion mutations in non-small-cell lung cancer. Clin. Transl. Oncol. 2022, 24, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Riely, G.J.; Neal, J.W.; Camidge, D.R.; Spira, A.I.; Piotrowska, Z.; Costa, D.B.; Tsao, A.S.; Patel, J.D.; Gadgeel, S.M.; Bazhenova, L.; et al. Activity and Safety of Mobocertinib (TAK-788) in Previously Treated Non-Small Cell Lung Cancer with EGFR Exon 20 Insertion Mutations from a Phase I/II Trial. Cancer Discov. 2021, 11, 1688–1699, Erratum in: Cancer Discov. 2023, 13, 2107. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.takeda.com/newsroom/newsreleases/2023/Takeda-Provides-Update-on-EXKIVITY-mobocertinib/ (accessed on 1 November 2023).
- Park, K.; Haura, E.B.; Leighl, N.B.; Mitchell, P.; Shu, C.A.; Girard, N.; Viteri, S.; Han, J.Y.; Kim, S.W.; Lee, C.K.; et al. Amivantamab in EGFR Exon 20 Insertion-Mutated Non-Small-Cell Lung Cancer Progressing on Platinum Chemotherapy: Initial Results From the CHRYSALIS Phase I Study. J. Clin. Oncol. 2021, 39, 3391–3402. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Tang, K.J.; Cho, B.C.; Liu, B.; Paz-Ares, L.; Cheng, S.; Kitazono, S.; Thiagarajan, M.; Goldman, J.W.; Sabari, J.K.; et al. PAPILLON Investigators. Amivantamab plus Chemotherapy in NSCLC with EGFR Exon 20 Insertions. N. Engl. J. Med. 2023; Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | ERBB2/EGFR Ex20ins | EGFR Classic Mutations | Adenocarcinoma * | |
|---|---|---|---|---|
| n = 31 | n = 24 | n = 141 | p | |
| Age | ||||
| ≥60 | 13 (41.9%) | 11 (45.8%) | 88 (62.4%) | 0.056 |
| <60 | 18 (58.1%) | 13 (54.2%) | 53 (37.6%) | |
| Gender | ||||
| Male | 17 (54.8%) | 13 (54.2%) | 112 (79.4%) | 0.002 |
| Female | 14 (45.2%) | 11 (45.8%) | 29 (20.6%) | |
| ECOG | ||||
| 0 | 22 (71.0%) | 5 (20.8%) | 100 (70.9%) | 0.001 |
| ≥1 | 9 (29.0%) | 19 (79.2%) | 41 (19.1%) | |
| Smoking | ||||
| Yes | 4 (12.9%) | 4 (16.7%) | 71 (50.4%) | 0.001 |
| No | 27 (87.1%) | 20 (83.3%) | 70 (49.6%) | |
| PD-L1 expression | ||||
| ≥1% | 12 (38.7%) | 14 (58.3%) | 70 (49.6%) | 0.553 |
| Negative | 7 (22.6%) | 3 (12.5%) | 19 (13.5%) | |
| Unknown | 12 (38.7%) | 7 (29.2%) | 52 (36.9%) | |
| Previous treatment | ||||
| TKI | 4 (12.9%) | 24 (100%) | 0 | |
| No | 27 (87.1%) | 0 | 141 (100%) | |
| Previous treatment | NA | |||
| Chemo/ICI | 0 | 0 | 0 | |
| No | 31 (100%) | 24 (100%) | 141 (100%) | |
| ICIs | NA | |||
| PD-1 | 31 (100%) | 24 (100%) | 141 (100%) | |
| PD-L1/CTLA-4 | 0 | 0 | 0 | |
| Chemotherapy | NA | |||
| Platin-based | 31 (100%) | 24 (100%) | 141 (100%) | |
| other | 0 | 0 | 0 | |
| Brain metastases | 0.085 | |||
| Yes | 8 (25.8%) | 11 (45.8%) | 34 (24.1%) | |
| No | 23 (74.2%) | 13 (54.2%) | 107 (75.9%) |
| Characteristics | Patients | EGFR EX20ins IC | EGFR EX20ins C | p | ERBB2 EX20ins IC | ERBB2 EX20ins C | p |
|---|---|---|---|---|---|---|---|
| 85 | 15 (17.6%) | 36 (42.4%) | 16 (18.8%) | 18 (21.2%) | |||
| Age | 0.971 | 0.703 | |||||
| ≥60 | 36 | 8 (53.3%) | 19 (52.8%) | 5 (31.2%) | 4 (22.2%) | ||
| <60 | 49 | 7 (46.7%) | 17 (47.2%) | 11 (68.8%) | 14 (77.8%) | ||
| Gender | 0.078 | >0.99 | |||||
| Male | 39 | 9 (60.0%) | 12 (33.3%) | 8 (50.0%) | 10 (55.6%) | ||
| Female | 46 | 6 (40.0%) | 24 (66.7%) | 8 (50.0%) | 8 (44.4%) | ||
| ECOG | 0.513 | 0.681 | |||||
| 0 | 57 | 12 (80.0%) | 25 (69.4%) | 10 (62.5%) | 10 (55.6%) | ||
| ≥1 | 28 | 3 (20.0%) | 11 (30.6%) | 6 (37.5%) | 8 (44.4%) | ||
| Smoking history | >0.99 | 0.125 | |||||
| Yes | 17 | 2 (13.3%) | 6 (16.7%) | 2 (12.5%) | 7 (38.9%) | ||
| No | 68 | 13 (86.7%) | 30 (83.3%) | 14 (87.5%) | 11 (61.1%) | ||
| Pathology | >0.99 | >0.99 | |||||
| adenocarcinoma | 83 | 15 (100%) | 35 (97.2%) | 15 (93.8%) | 18 (100%) | ||
| Other | 2 | 0 | 1 (2.8%) | 1 (6.2%) | 0 | ||
| Treatment * | NA | ||||||
| Pembrolizumab + chemo | 9 | 3 (20.0%) | 6 (37.5%) | ||||
| Toripalimab + chemo | 1 | 0 | 1 (6.2%) | ||||
| Sintilimab + chemo | 5 | 2 (13.3%) | 3 (18.8%) | ||||
| Camrelizumab + chemo | 13 | 8 (53.3%) | 5 (31.2%) | ||||
| Tislelizumab + chemo | 3 | 2 (13.3%) | 1 (6.2%) | ||||
| AC/P+ Bev | 21 | 13 (36.1%) | 8 (44.4%) | ||||
| AC/P | 28 | 20 (55.6%) | 8 (44.4%) | ||||
| TC/P+ Bev | 2 | 2 (5.6%) | 0 | ||||
| TC/P | 3 | 1 (2.8%) | 2 (11.1%) | ||||
| Brain metastases | 0.749 | 0.681 | |||||
| Yes | 23 | 4 (26.7%) | 12 (33.3%) | 4 (25.0%) | 3 (16.7%) | ||
| No | 62 | 11 (73.3%) | 24 (66.7%) | 12 (75.0%) | 15 (83.3%) | ||
| Liver metastases | 0.657 | >0.99 | |||||
| Yes | 16 | 1 (6.7%) | 5 (13.9%) | 5 (31.2%) | 5 (27.8%) | ||
| No | 69 | 14 (93.3%) | 31 (86.1%) | 11 (68.8%) | 13 (72.2%) |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Factors | p Value | HR (95%CI) | p Value | HR (95%CI) |
| Age (<60 y vs. ≥60 y) | 0.289 | 1.402 (0.840–2.340) | ||
| Gender (male vs. female) | 0.466 | 0.910 (0.546–1.517) | ||
| Smoking history (yes vs. no) | 0.941 | 0.912 (0.492–1.691) | ||
| PS (0 vs. ≥1) | 0.044 | 0.673 (0.386–1.173) | 0.064 | 0.599 (0.348–1.030) |
| Ex20ins (EGFR vs. ERBB2) | 0.286 | 0.763 (0.451–1.293) | ||
| Brain metastasis (yes vs. no) | 0.340 | 1.315 (0.721–2.400) | ||
| Liver metastasis (yes vs. no) | 0.029 | 1.965 (0.883–4.372) | 0.031 | 2.053 (1.067–3.953) |
| PD-L1 expression (0% vs. ≥1%) | 0.410 | 0.767 (0.394–1.496) | ||
| Treatment (PCI vs. PC) | 0.066 | 1.592 (0.888–2.853) | 0.037 | 1.866 (1.037–3.354) |
| Patients | Mutation | Treatment | Line | mPFS | mOS | ORR | DCR | |
|---|---|---|---|---|---|---|---|---|
| Shah et al. [14] | N = 18 | EGFR Ex20ins | Platinum-based chemotherapy | First/second | 7.1 m | 3.2 y | 39% | NR |
| Xu et al. [15] | N = 77 | EGFR Ex20ins | Pemetrexed-based chemotherapy | First | 5.5 m | 25 m | 41.56% | 75.32% |
| Chelabi et al. [16] | N = 27 | EGFR Ex20ins | Chemotherapy | First | 6.5 m | NR | 41% | 82% |
| Xu et al. [25] | N = 37 | ERBB2 Ex20ins | Chemotherapy | First | 5.5 m | NR | NR | NR |
| Wang et al. [29] | N = 49 | EGFR Ex20ins | Platinum-based chemotherapy | First | 7.6 m | 19.9 m | NR | NR |
| Lau et al. [7] | N = 6 | EGFR Ex20ins | PD-1/PD-L1 | First/second/third | 4.8 m | NR | 50% | 66.7% |
| Tian et al. [11] | N = 13 | ERBB2 Ex20ins | Chemo-ICI | First/second | 8.0 m | NR | 31% | 77% |
| Metro et al. [19] | N = 15 | EGFR Ex20ins | ICI or chemo-ICI | First/second/third | 2.0 m | 5.3 m | 6.7% | 13.3% |
| Chen et al. [20] | N = 9 | EGFR Ex20ins | PD-1/PD-L1 | NR | NR | NR | 22.2% | NR |
| Chen et al. [20] | N = 6 | ERBB2 Ex20ins | PD-1/PD-L1 | NR | NR | NR | 0% | NR |
| Hastings et al. [21] | N = 28 | EGFR Ex20ins | ICI | First/second/third | 1.9 m | 5.5 m | 15.2% | 32.1% |
| Choudhury et al. [30] | N = 12 | EGFR Ex20ins | Chemo-ICI | First/second/third | 7 m | NR | NR | NR |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, Y.; Fu, Y.; Chen, Y.; Li, Q.; Liu, T.; Ding, Z. Poor Efficacy of Immune Checkpoint Inhibitors Plus Chemotherapy in Lung Cancer Patients with EGFR/ERBB2 Exon 20 Insertion. Curr. Oncol. 2023, 30, 9929-9939. https://doi.org/10.3390/curroncol30110721
Zheng Y, Fu Y, Chen Y, Li Q, Liu T, Ding Z. Poor Efficacy of Immune Checkpoint Inhibitors Plus Chemotherapy in Lung Cancer Patients with EGFR/ERBB2 Exon 20 Insertion. Current Oncology. 2023; 30(11):9929-9939. https://doi.org/10.3390/curroncol30110721
Chicago/Turabian StyleZheng, Yue, Yang Fu, Yueyun Chen, Qing Li, Ting Liu, and Zhenyu Ding. 2023. "Poor Efficacy of Immune Checkpoint Inhibitors Plus Chemotherapy in Lung Cancer Patients with EGFR/ERBB2 Exon 20 Insertion" Current Oncology 30, no. 11: 9929-9939. https://doi.org/10.3390/curroncol30110721
APA StyleZheng, Y., Fu, Y., Chen, Y., Li, Q., Liu, T., & Ding, Z. (2023). Poor Efficacy of Immune Checkpoint Inhibitors Plus Chemotherapy in Lung Cancer Patients with EGFR/ERBB2 Exon 20 Insertion. Current Oncology, 30(11), 9929-9939. https://doi.org/10.3390/curroncol30110721




