Combination of Electrochemotherapy with Radiotherapy: A Comprehensive, Systematic, PRISMA-Compliant Review of Efficacy and Potential Radiosensitizing Effects in Tumor Control
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Protocol Registration and Guidelines
2.2. Bibliographic Search
2.3. Inclusion Criteria
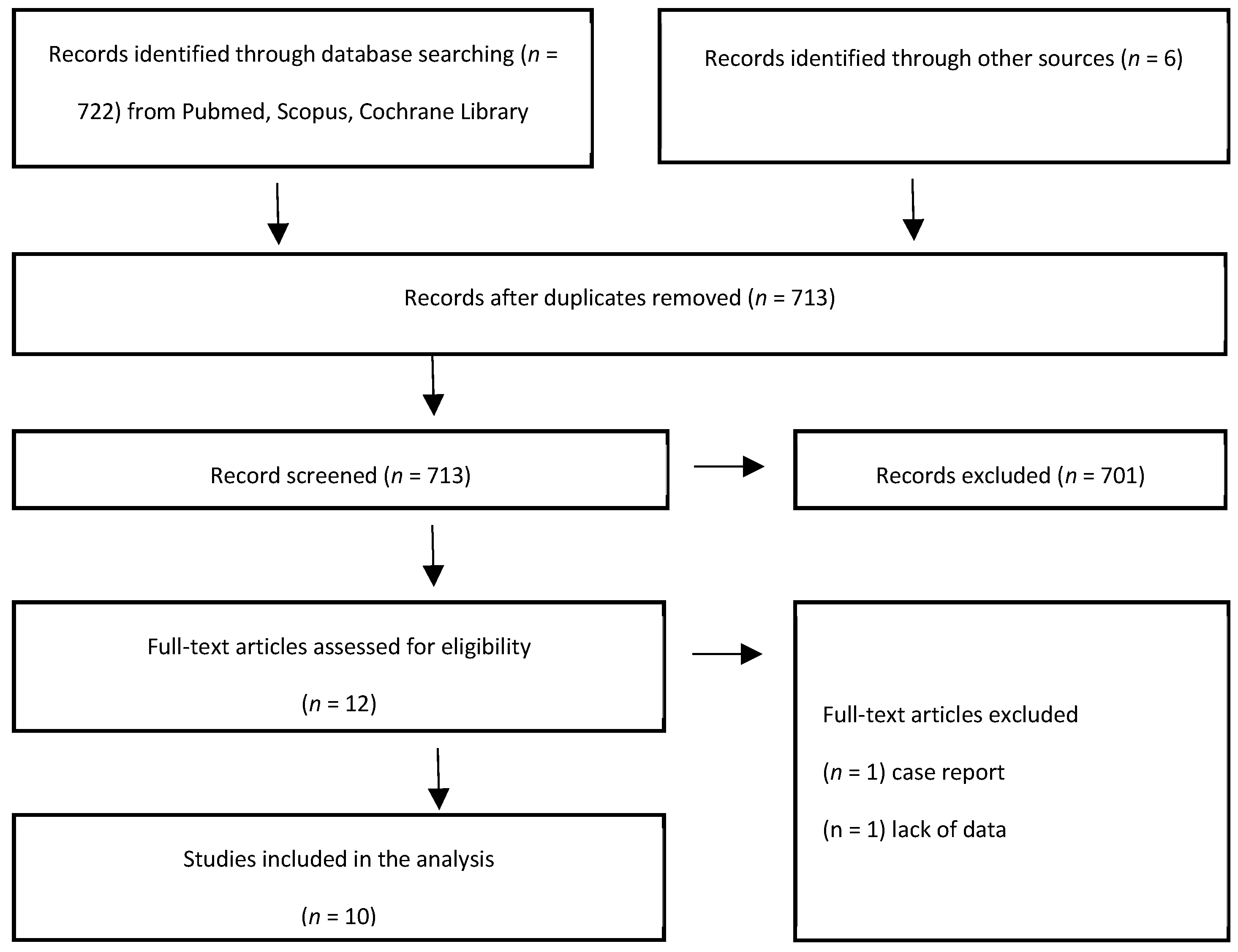
2.4. Study Selection
2.5. Data Extraction
2.6. Quality Assessment
3. Results
3.1. Search Results
3.2. Characteristics of Included Studies
3.3. Tumor and Treatment Characteristics
3.4. Tumor Control and Toxicity in In Vitro Studies
3.5. Tumor Response and Toxicity in In Vivo Studies
3.6. Quality Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Telarovic, I.; Wenger, R.H.; Pruschy, M. Interfering with Tumor Hypoxia for Radiotherapy Optimization. J. Exp. Clin. Cancer Res. 2021, 40, 197. [Google Scholar] [CrossRef] [PubMed]
- Boulefour, W.; Rowinski, E.; Louati, S.; Sotton, S.; Wozny, A.S.; Acosta, P.B.; Mery, B.; Rodriguez-Lafrasse, C.; Magne, N. A Review of the Role of Hypoxia in Radioresistance in Cancer Therapy. Med. Sci. Monit. 2021, 27, e934116-1–e934116-7. [Google Scholar]
- Cadossi, R.; Ronchetti, M.; Cadossi, M. Locally enhanced chemotherapy by electroporation: Clinical experiences and perspective of use of electrochemotherapy. Future Oncol. 2014, 10, 877–890. [Google Scholar] [CrossRef] [PubMed]
- Orlowski, S.; Belehradek, J., Jr.; Paoletti, C.; Mir, L.M. Transient electropermeabilization of cells in culture. Increase of the cytotoxicity of anticancer drugs. Biochem. Phrmacol. 1988, 37, 4727–4733. [Google Scholar] [CrossRef]
- Marty, M.; Sersa, G.; Garbay, J.R.; Gehl, J.; Collins, C.G.; Snoj, M.; Billard, V.; Geertsen, P.F.; Larkin, J.O.; Miklavcic, D.; et al. Electrochemothrapy, an easy, highly effective and safe treatment of cutaneous and subcutaneous metastases: Results of ESOPE (European Standard Operating Procedures of Electrochemotherapy) study. Eur. J. Cancer Suppl. 2006, 4, 3–13. [Google Scholar] [CrossRef]
- Rezaee, Z.; Yadollahpour, A.; Rashidi, S.; Kunwar, P.S. Radiosensitizing Effect of Electrochemotherapy: A Systematic Review of Protocols and Efficiency. Curr. Drug Targets 2017, 18, 1893–1903. [Google Scholar] [CrossRef]
- Pakhomov, A.G.; Miklavcic, D.; Markov, M.S. Advanced Electroporation Techniques in Biology and Medicine, 1st ed.; CRC Press: Boca Raton, FL, USA, 2010. [Google Scholar]
- Centre for Reviews and Dissemination, University of York. PROSPERO: International Prospective Register of Systematic Reviews. Available online: https://www.crd.york.ac.uk/prospero (accessed on 8 October 2019).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Shil, P.; Sanghvi, S.H.; Vidyasagar, P.B.; Mishra, K.P. Enhancement of Radiation Cytotoxicity in Murine Cancer Cells by Electroporation: In Vitro and in Vivo Studies. J. Environ. Pathol. Toxicol. Oncol. 2005, 24, 291–298. [Google Scholar] [CrossRef]
- Shil, P.; Kumar, A.; Vidyasagar, P.B.; Mishra, K.P. Electroporation enhances radiation and doxorubicin-induced toxicity in solid tumor in vivo. J. Environ. Pathol. Toxicol. Oncol. 2006, 25, 625–632. [Google Scholar] [CrossRef]
- Raeisi, E.; Aghamiri, S.M.; Bandi, A.; Rahmatpour, N.; Firoozabadi, S.M.; Kafi-Abad, S.A.; Mir, L.M. The Antitumor Efficiency of Combined Electrochemotherapy and Single Dose Irradiation on a Breast Cancer Tumor Model. Radiol. Oncol. 2012, 46, 226–232. [Google Scholar] [CrossRef][Green Version]
- Yadollahpour, A.; Rezaee, Z.; Bayati, V.; Tahmasebi Birgani, M.J.; Negad Dehbashi, F. Radiotherapy Enhancement with Electroporation in Human Intestinal Colon Cancer HT-29 Cells. Asian Pac. J. Cancer Prev. 2018, 19, 1259–1262. [Google Scholar] [PubMed]
- Kranjc, S.; Cemazar, M.; Grosel, A.; Sentjurc, M.; Sersa, G. Radiosensitising effect of electrochemotherapy with bleomycin in LPB sarcoma cells and tumors in mice. BMC Cancer 2005, 5, 115. [Google Scholar] [CrossRef] [PubMed]
- Kranjc, S.; Cemazar, M.; Grosel, A.; Scancar, J.; Sersa, G. Electroporation of LPB sarcoma cells in vitro and tumors in vivo increases the radiosensitizing effect of cisplatin. Anticancer Res. 2003, 23, 275–281. [Google Scholar] [PubMed]
- Kranjc, S.; Tevz, G.; Kamensek, U.; Vidic, S.; Cemazar, M.; Sersa, G. Radiosensitizing effect of electrochemotherapy in a fractionated radiation regimen in radiosensitive murine sarcoma and radioresistant adenocarcinoma tumor model. Radiat. Res. 2009, 172, 677–685. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Maxim, P.G.; Carson, J.J.; Ning, S.; Knox, S.J.; Boyer, A.L.; Hsu, C.P.; Benaron, D.A.; Walleczek, J. Enhanced effectiveness of radiochemotherapy with tirapazamine by local application of electric pulses to tumors. Radiat. Res. 2004, 162, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Sersa, G.; Kranjc, S.; Cemazar, M. Improvement of combined modality therapy with cisplatin and radiation using electroporation of tumors. Int. J. Radiat. Oncol. Biol. Phys. 2000, 46, 1037–1041. [Google Scholar] [CrossRef]
- Kranjc, S.; Čemažar, M.; Grošel, A.; Pipan, Z.; Serša, G. Effect of electroporation on radiosensitization with cisplatin in two cell lines with different chemo- and radiosensitivity. Radiol. Oncol. 2003, 37, 101–107. [Google Scholar]
- Vaupel, P.; Piazena, H.; Notter, M.; Thomsen, A.R.; Grosu, A.L.; Scholkmann, F.; Pockley, A.G.; Multhoff, G. From Localized Mild Hyperthermia to Improved Tumor Oxygenation: Physiological Mechanisms Critically Involved in Oncologic Thermo-Radio-Immunotherapy. Cancers 2023, 15, 1394. [Google Scholar] [CrossRef]
- Hrycushko, B.A.; Chopra, R.; Sayre, J.W.; Richardson, J.A.; Folkert, M.R.; Timmerman, R.D.; Medin, P.M. Local Hypothermia as a Radioprotector of the Rectal Wall During Prostate Stereotactic Body Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2017, 98, 75–82. [Google Scholar] [CrossRef]
- Cirincione, R.; Di Maggio, F.M.; Forte, G.I.; Minafra, L.; Bravatà, V.; Castiglia, L.; Cavalieri, V.; Borasi, G.; Russo, G.; Lio, D.; et al. High-Intensity Focused Ultrasound- and Radiation Therapy-Induced Immuno-Modulation: Comparison and Potential Opportunities. Ultrasound Med. Biol. 2017, 43, 398–411. [Google Scholar] [CrossRef]
- Burton, S.A.; Paljug, W.R.; Kalnicki, S.; Werts, E.D. Hypothermia-enhanced human tumor cell radiosensitivity. Cryobiology 1997, 35, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, H.A.; Villar, R.C. Radiotherapy and Immune Response: The Systemic Effects of a Local Treatment. Clinics 2018, 73 (Suppl. S1), e557s. [Google Scholar]
- Ursic, K.; Kos, S.; Kamensek, U.; Cemazar, M.; Scancar, J.; Bucek, S.; Kranjc, S.; Staresinic, B.; Sersa, G. Comparable effectiveness and immunomodulatory actions of oxaliplatin and cisplatin in electrochemotherapy of murine melanoma. Bioelectrochemistry 2018, 119, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Stewart, F.A.; Bartelink, H. The combination of radiotherapy and chemotherapy. In Basic Clinical Radiobiology, 3rd ed.; Steel, G.G., Ed.; Arnold: London, UK, 2002; pp. 217–230. [Google Scholar]
- Brade, A.M.; Allibhai, Z. Radiation Sensitizers. In Advances in Radiation Oncology in Lung Cancer; Springer: Berlin/Heidelberg, Germany, 2011; pp. 213–222. [Google Scholar]
- Overgaard, J.; Hansen, H.S.; Overgaard, M.; Bastholt, L.; Berthelsen, A.; Specht, L.; Lindeløv, B.; Jørgensen, K. A randomized double-blind phase III study of nimorazole as a hypoxic radiosensitizer of primary radiotherapy in supraglottic larynx and pharynx carcinoma. Results of the Danish Head and Neck Cancer Study (DAHANCA) Protocol 5–85. Radiother. Oncol. 1998, 46, 135–146. [Google Scholar] [CrossRef]
- Gong, L.; Zhang, Y.; Liu, C.; Zhang, M.; Han, S. Application of Radiosensitizers in Cancer Radiotherapy. Int. J. Nanomed. 2021, 16, 1083–1102. [Google Scholar] [CrossRef]
- Goffinet, D.R.; Bagshaw, M.A. Clinical use of radiation sensitizing agents. Cancer Treat. Rev. 1974, 1, 15–26. [Google Scholar] [CrossRef]
| Author/Year | Tumor Cells |
|---|---|
| Kranjc S, 2003 [15] | LPB murine sarcoma cells |
| Kranjc S, 2003 [15] | SCK murine mammary carcinoma cells and EAT-E cells |
| Kranjc S, 2005 [14] | LPB murine sarcoma cells and tumors |
| Shil P, 2005 [10] | Murine fibrosarcoma |
| Yadollahpour A, 2018 [13] | Human colorectal cancer cell line HT-29 |
| Author/Year | Study Type | Tumor Cells Histology |
|---|---|---|
| Sersa G, 2000 [18] | Preclinical | Ehrlich-Lettre ascites carcinoma in CBA mice |
| Kranjc S, 2003 [15] | Preclinical | LPB murine sarcoma |
| Maxim P.G, 2004 [17] | Preclinical | Squamous cell carcinoma in C3H mice |
| Kranjc S, 2005 [14] | Preclinical | LPB murine sarcoma |
| Shil P, 2005 [10] | Preclinical | Murine fibrosarcoma |
| Shil P, 2006 [11] | Preclinical | Murine fibrosarcoma |
| Kranjc S, 2009 [16] | Preclinical | Sarcoma SA-1 and mammary adenocarcinoma CaNT in CBA and A/J mice |
| Raeisi E, 2012 [12] | Preclinical | Invasive ductal carcinoma tumors in Balb/C mice |
| ECT/EP Treatment | IR Treatment | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author/Year | Drug | n° Pulses | Intensity (V/cm) | Duration (µs) | Frequency (Hz) | Tot Dose (Gy) | Dose/Fract (Gy) | Rad Type | Dose Rate (Gy/Min) | Kilo/Mega Voltage |
| Kranjc S, 2003 [15] | CDDP | 8 | 1200 | 100 | 1 | 2–8 | 2–8 | X-ray | 2 | 220 kV |
| Kranjc S, 2003 [15] | CDDP | 8 | 1000 | 100 | 1 | 2–8 | 2–8 | X-ray | 2 | 220 kV |
| Kranjc S, 2005 [14] | BLM | 8 | 1200 | 100 | 1 | 2–8 | 2–8 | X-ray | 2 | 220 kV |
| Shil P, 2005 [10] | NONE | 8 × 10 | 1000 | 200 | 1 | 2 | 2 | Co60 γ-rays | 0.37 | 1.25 MV |
| Yadollahpour A, 2018 [13] | NONE | 1 | 1200 | 100 | NR | 0–8 | 0–8 | X-ray | 3 | 6 MV |
| ECT/EP Treatment | IR Treatment | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author/Year | Drug | RoA | n° Pulses | Intensity (V/cm) | Duration (µs) | Frequency (Hz) | Total Dose (Gy) | Dose/Fraction (Gy) | Radiation Type | Dose Rate (Gy/Min) | Kilo/Mega Voltage |
| Sersa G, 2000 [18] | CDDP | IV | 8 | 1300 | 100 | 1 | 15 | 15 | X-ray | 2.1 | 220 kV |
| Kranjc S, 2003 [15] | CDDP | IV | 8 | 1300 | 100 | 1 | 5–50 | 5–50 | X-ray | 2.1 | 220 kV |
| Maxim P.G, 2004 [17] | TPZ | IP | 8 | 1200 | 100 | 1 | 7 | 7 | X-ray | 0.83 | 250 kV |
| Kranjc S, 2005 [14] | BLM | IV | 8 | 1200 | 100 | 1 | 5–50 | 5–50 | X-ray | 2.1 | 220 kV |
| Shil P, 2005 [10] | NONE | NA | 8 × 10 | 1000 | 200 | 1 | 2 | 2 | Co60 γ-rays | 0.37 | 1.25 MV |
| Shil P, 2006 [11] | DOX | IT | 8 × 10 | 1000 | 200 | 1 | 2 | 2 | Co60 γ-rays | 0.37 | 1.25 MV |
| Kranjc S, 2009 [16] | BLM | IV | 4 × 2 | 1300 | 100 | 1 | 10–20 | 2–20 | X-ray | 2.2 | 220 kV |
| Raeisi E, 2012 [12] | CDDP | IT | 4 × 2 | 1000 | 100 | 1 | 3\5 | 3\5 | Co60 γ-rays | 0.6 (3 Gy)–0.71 (5 Gy) | 1.25 MV |
| Author/Year | Treatment Groups | IC50 (µg/mL) | LD50 (Gy) | Cell Viability | EF | |
|---|---|---|---|---|---|---|
| Kranjc S., 2003 [15] | CDDP | 120 | - | - | - | |
| CDDP + EP | 4 | - | - | - | ||
| CDDP + IR | 23 | - | - | - | ||
| CDDP + EP + IR | 2 | - | - | - | ||
| IR | - | - | - | - | ||
| EP + IR | - | - | - | - | ||
| CONTROLS | - | - | - | - | ||
| EP | - | - | - | - | ||
| Kranjc S., 2003 [15] | CDDP | SCK 14.8 | EAT-E 48.5 | - | - | - |
| CDDP + EP | 3.4 | 2.2 | - | - | - | |
| CDDP + IR | 8.0 | 22 | - | - | - | |
| CDDP + EP + IR | 0.9 | 0.9 | - | - | - | |
| Kranjc S., 2005 [14] | CONTROLS | - | - | - | - | |
| IR | - | - | - | - | ||
| BLM + IR | - | - | - | 1.19 | ||
| EP + IR | - | - | - | 1.25 | ||
| BLM + EP + IR | - | - | - | 1.53 | ||
| Shil P., 2005 [10] | - | - | 5% reduction | - | ||
| Yadollahpour A., 2018 [13] | IR | - | 3.97 | - | - | |
| EP + IR | - | 2.9 | - | - | ||
| Author/Year | Treatment Groups | TCD50 (Gy) | DT (Days) | TGD (Days) | OR (%) | EF | Decreased Tumor Volume vs. Controls (%) | Toxicity | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Sersa G., 2000 [18] | CONTROLS | - | 3.9 | Nr | - | - | - | - | ||
| CDDP | - | 5.4 | 1.5 | - | - | - | - | |||
| EP | - | 4.5 | 0.6 | - | - | - | - | |||
| IR | - | 17.4 | 13.5 | - | - | - | - | |||
| CDDP + EP | - | 13.4 | 9.5 | - | - | - | - | |||
| CDDP + IR | - | 19.5 | 15.6 | - | - | - | - | |||
| CDDP + EP + IR | - | 44.5 | 40.6 | - | - | - | - | |||
| EP + IR | - | 24.2 | 20.3 | - | - | - | - | |||
| Kranjc S., 2003 [15] | CDDP | - | - | - | - | - | - | - | ||
| CDDP + EP | - | - | - | - | - | - | - | |||
| CDDP + IR | 19.6 | - | - | - | 1.1 | - | - | |||
| CDDP + EP + IR | 14.2 | - | - | - | 1.6 | - | - | |||
| IR | 22.1 | - | - | - | - | - | - | |||
| EP + IR | 23.5 | - | - | - | 0.9 | - | - | |||
| CONTROLS | - | - | - | - | - | - | - | |||
| EP | - | - | - | - | - | - | - | |||
| Maxim P.G., 2004 [17] | CONTROLS | - | - | large tumors | small tumors | - | - | - | - | |
| TPZ | - | - | 1.0 | 2.0 | - | - | - | - | ||
| TPZ + EP | - | - | 7.5 | 7.5 | - | - | - | - | ||
| TPZ + IR | - | - | 10.5 | 7.0 | - | - | - | - | ||
| TPZ + EP + IR | - | - | 17.5 | 13.0 | - | - | - | - | ||
| EP + IR | - | - | 3.5 | 3.0 | - | - | - | - | ||
| Kranjc S., 2005 [14] | CONTROLS | - | - | - | - | - | - | - | - | hair loss in the irradiated area |
| IR | 23.1 | - | - | - | - | - | - | - | ||
| BLM + IR | 22.8 | - | - | - | - | - | 1.0 | - | ||
| EP + IR | 22.1 | - | - | - | - | - | 1.0 | - | ||
| BLM + EP + IR | 12.4 | - | - | - | - | - | 1.9 | - | ||
| Shil P., 2005 [10] | CONTROLS | - | - | - | - | - | - | - | ||
| EP | - | - | - | - | - | - | - | |||
| IR | - | - | - | - | - | - | - | |||
| EP + IR | - | - | - | - | - | 51 | - | |||
| Shil P., 2006 [11] | CONTROLS | - | 1.28 | nr | - | - | - | - | ||
| VEHICLE CONTROL | - | 1.30 | nr | - | - | - | - | |||
| EP | - | 2 | 0.72 | - | - | 85 | - | |||
| IR | - | 1.82 | 0.54 | - | - | 82 | - | |||
| DOX | - | 1.94 | 0.66 | - | - | 88 | - | |||
| DOX + EP | - | 2.5 | 1.22 | - | - | 57 | - | |||
| IR + EP | - | 2.78 | 1.5 | - | - | - | - | |||
| DOX + IR | - | 2.48 | 1.2 | - | - | 52.5 | - | |||
| IR + DOX + EP | - | 3 | 1.72 | - | - | 49 | - | |||
| Kranjc S., 2009 [16] | CONTROLS | - | (SA-1) 2.1 | (CaNT) 2.2 | (SA-1) | (CaNT) | - | - | - | IR (SD vs. FD): more toxicity on normal skin and more body weight loss |
| EP | - | 3.8 | 3.6 | 1.7 | 1.4 | - | - | - | ||
| BLM | - | 3.2 | 2.6 | 1.1 | 0.4 | - | - | - | ||
| BLM + EP | - | 22.3 | 17.8 | 20.2 | 15.6 | - | - | - | ||
| IR (SD) | - | 15 | 17.1 | 12.9 | 14.9 | - | - | - | ||
| BLM + IR (SD) | - | 15.1 | 17.7 | 13.0 | 15.5 | - | - | - | ||
| EP + IR (SD) | - | 15.4 | 17.3 | 13.3 | 15.1 | - | - | - | ||
| BLM + EP + IR (SD) | - | 40.1 | 39.5 | 38.0 | 37.3 | - | - | - | ||
| IR (FD) | - | 7.0 | 10.3 | 4.9 | 8.1 | - | - | - | ||
| BLM + IR (FD) | - | 7.4 | 11.6 | 5.3 | 9.4 | - | - | - | ||
| EP + IR (FD) | - | 8.5 | 10.8 | 6.4 | 8.6 | - | - | - | ||
| BLM + EP + IR (FD) | - | 32.5 | 32.2 | 30.4 | 30.0 | - | - | - | ||
| Raeisi E., 2012 [12] | CONTROLS | - | 4.6 | nr | - | - | - | hair loss in irradiated area | ||
| CDDP | - | 10.6 | 5.5 | - | - | - | ||||
| EP | - | 6.6 | 2.0 | - | - | - | ||||
| CDDP + EP | - | 20.1 | 15.5 | - | - | - | ||||
| IR (3 Gy) | - | 15.7 | 11.1 | - | - | - | ||||
| CDDP + IR (3 Gy) | - | 15.9 | 11.3 | - | - | - | ||||
| CDDP + EP + IR (3 Gy) | - | 30.3 | 25.7 | - | - | - | ||||
| EP + IR (3 Gy) | - | 13.4 | 8.8 | - | - | - | ||||
| IR (5 Gy) | - | 25.2 | 20.6 | - | - | - | ||||
| CDDP + IR (5 Gy) | - | 25.6 | 21.0 | - | - | - | ||||
| CDDP + EP + IR (5 Gy) | - | 43.2 | 38.6 | - | - | - | ||||
| EP + IR (5 Gy) | - | 22.4 | 17.8 | - | - | - | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferioli, M.; Perrone, A.M.; Buwenge, M.; Arcelli, A.; Vadala’, M.; Fionda, B.; Malato, M.C.; De Iaco, P.; Zamagni, C.; Cammelli, S.; et al. Combination of Electrochemotherapy with Radiotherapy: A Comprehensive, Systematic, PRISMA-Compliant Review of Efficacy and Potential Radiosensitizing Effects in Tumor Control. Curr. Oncol. 2023, 30, 9895-9905. https://doi.org/10.3390/curroncol30110719
Ferioli M, Perrone AM, Buwenge M, Arcelli A, Vadala’ M, Fionda B, Malato MC, De Iaco P, Zamagni C, Cammelli S, et al. Combination of Electrochemotherapy with Radiotherapy: A Comprehensive, Systematic, PRISMA-Compliant Review of Efficacy and Potential Radiosensitizing Effects in Tumor Control. Current Oncology. 2023; 30(11):9895-9905. https://doi.org/10.3390/curroncol30110719
Chicago/Turabian StyleFerioli, Martina, Anna M. Perrone, Milly Buwenge, Alessandra Arcelli, Maria Vadala’, Bruno Fionda, Maria C. Malato, Pierandrea De Iaco, Claudio Zamagni, Silvia Cammelli, and et al. 2023. "Combination of Electrochemotherapy with Radiotherapy: A Comprehensive, Systematic, PRISMA-Compliant Review of Efficacy and Potential Radiosensitizing Effects in Tumor Control" Current Oncology 30, no. 11: 9895-9905. https://doi.org/10.3390/curroncol30110719
APA StyleFerioli, M., Perrone, A. M., Buwenge, M., Arcelli, A., Vadala’, M., Fionda, B., Malato, M. C., De Iaco, P., Zamagni, C., Cammelli, S., Tagliaferri, L., & Morganti, A. G. (2023). Combination of Electrochemotherapy with Radiotherapy: A Comprehensive, Systematic, PRISMA-Compliant Review of Efficacy and Potential Radiosensitizing Effects in Tumor Control. Current Oncology, 30(11), 9895-9905. https://doi.org/10.3390/curroncol30110719








