Cognitive Trajectories in Older Patients with Cancer Undergoing Radiotherapy—A Prospective Observational Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Assessments
2.3. Statistical Approach
2.4. Ethical Considerations
3. Results
3.1. Study Recruitment and Patient Characteristics
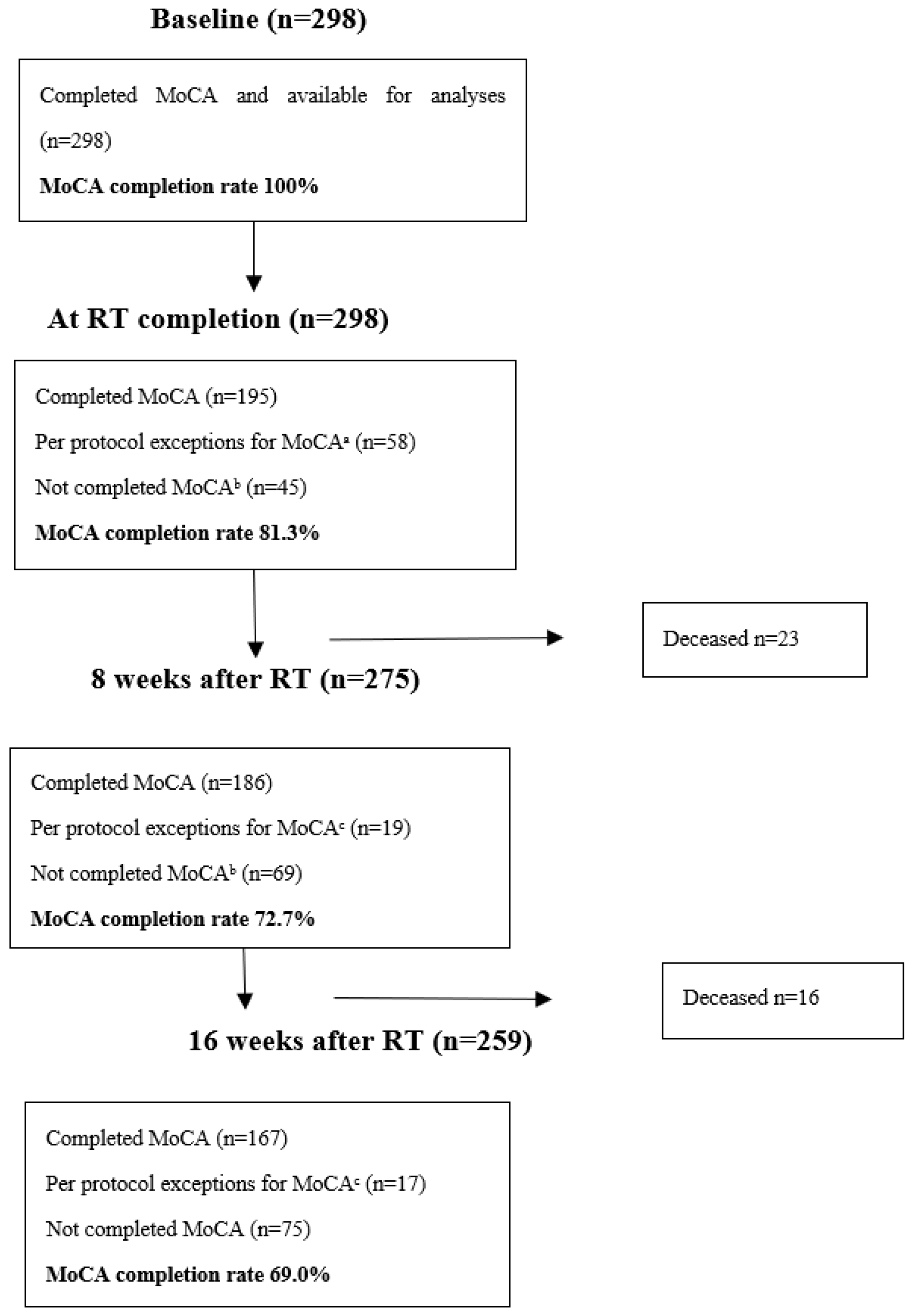
3.2. MoCA Completion Rates, Scores, and Comparison to Norwegian Normative Data
3.3. Factors Associated with Baseline MoCA Scores
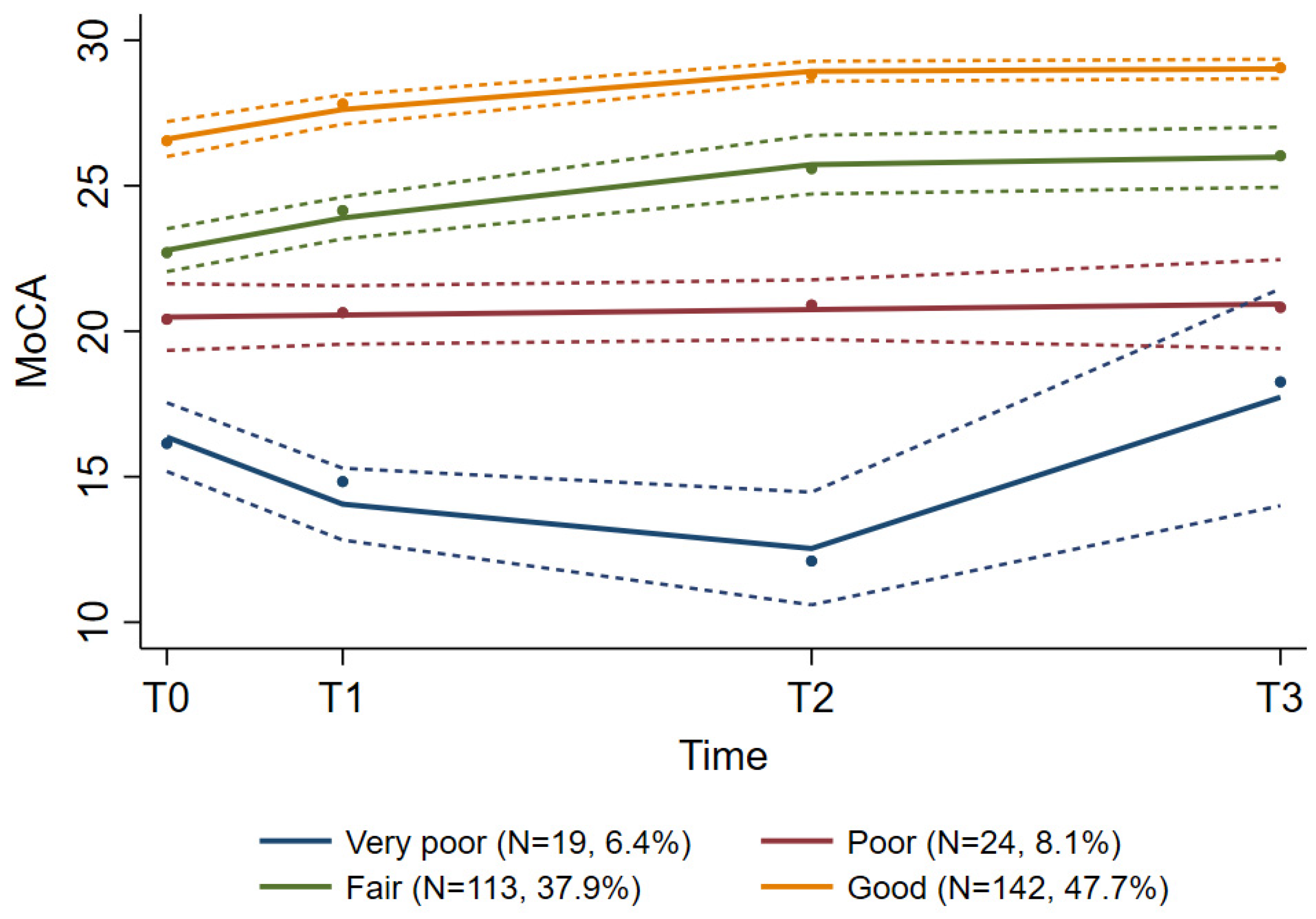
3.4. MoCA Score Trajectories
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Raji, M.A.; Kuo, Y.F.; Freeman, J.L.; Goodwin, J.S. Effect of a dementia diagnosis on survival of older patients after a diagnosis of breast, colon, or prostate cancer: Implications for cancer care. Arch. Intern. Med. 2008, 168, 2033–2040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohile, S.G.; Mohamed, M.R.; Xu, H.; Culakova, E.; Loh, K.P.; Magnuson, A.; Flannery, M.A.; Obrecht, S.; Gilmore, N.; Ramsdale, E.; et al. Evaluation of geriatric assessment and management on the toxic effects of cancer treatment (GAP70+): A cluster-randomised study. Lancet 2021, 398, 1894–1904. [Google Scholar] [CrossRef]
- Magnuson, A.; Ahles, T.; Chen, B.T.; Mandelblatt, J.; Janelsins, M.C. Cognitive Function in Older Adults With Cancer: Assessment, Management, and Research Opportunities. J. Clin. Oncol. 2021, 39, 2138–2149. [Google Scholar] [CrossRef]
- Ahles, T.A.; Root, J.C. Cognitive Effects of Cancer and Cancer Treatments. Annu. Rev. Clin. Psychol. 2018, 14, 425–451. [Google Scholar] [CrossRef] [PubMed]
- Loh, K.P.; Janelsins, M.C.; Mohile, S.G.; Holmes, H.M.; Hsu, T.; Inouye, S.K.; Karuturi, M.S.; Kimmick, G.G.; Lichtman, S.M.; Magnuson, A.; et al. Chemotherapy-related cognitive impairment in older patients with cancer. J. Geriatr. Oncol. 2016, 7, 270–280. [Google Scholar] [CrossRef] [Green Version]
- Országhová, Z.; Mego, M.; Chovanec, M. Long-Term Cognitive Dysfunction in Cancer Survivors. Front. Mol. Biosci. 2021, 8, 770413. [Google Scholar] [CrossRef]
- Lange, M.; Joly, F.; Vardy, J.; Ahles, T.; Dubois, M.; Tron, L.; Winocur, G.; De Ruiter, M.B.; Castel, H. Cancer-related cognitive impairment: An update on state of the art, detection, and management strategies in cancer survivors. Ann. Oncol. 2019, 30, 1925–1940. [Google Scholar] [CrossRef] [Green Version]
- Mandelblatt, J.S.; Zhou, X.; Small, B.J.; Ahn, J.; Zhai, W.; Ahles, T.; Extermann, M.; Graham, D.; Jacobsen, P.B.; Jim, H.; et al. Deficit Accumulation Frailty Trajectories of Older Breast Cancer Survivors and Non-Cancer Controls: The Thinking and Living with Cancer Study. J. Natl. Cancer Inst. 2021, 113, 1053–1064. [Google Scholar] [CrossRef]
- Mandelblatt, J.S.; Jacobsen, P.B.; Ahles, T. Cognitive effects of cancer systemic therapy: Implications for the care of older patients and survivors. J. Clin. Oncol. 2014, 32, 2617–2626. [Google Scholar] [CrossRef] [Green Version]
- Magnuson, A.; Mohile, S.; Janelsins, M. Cognition and Cognitive Impairment in Older Adults with Cancer. Curr. Geriatr. Rep. 2016, 5, 213–219. [Google Scholar] [CrossRef] [Green Version]
- Lange, M.; Heutte, N.; Rigal, O.; Noal, S.; Kurtz, J.E.; Lévy, C.; Allouache, D.; Rieux, C.; Lefel, J.; Clarisse, B.; et al. Decline in Cognitive Function in Older Adults with Early-Stage Breast Cancer after Adjuvant Treatment. Oncologist 2016, 21, 1337–1348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fried, T.R.; Bradley, E.H.; Towle, V.R.; Allore, H. Understanding the treatment preferences of seriously ill patients. N. Engl. J. Med. 2002, 346, 1061–1066. [Google Scholar] [CrossRef] [PubMed]
- Hurria, A.; Somlo, G.; Ahles, T. Renaming “chemobrain”. Cancer Investig. 2007, 25, 373–377. [Google Scholar] [CrossRef] [PubMed]
- NCCN, National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. Older Adult Oncology Version 1.2022. Available online: https://www.nccn.org/professionals/physician_gls/pdf/senior.pdf (accessed on 7 April 2022).
- Soussain, C.; Ricard, D.; Fike, J.R.; Mazeron, J.J.; Psimaras, D.; Delattre, J.Y. CNS complications of radiotherapy and chemotherapy. Lancet 2009, 374, 1639–1651. [Google Scholar] [CrossRef]
- Kirkhus, L.; Saltyte Benth, J.; Rostoft, S.; Gronberg, B.H.; Hjermstad, M.J.; Selbaek, G.; Wyller, T.B.; Harneshaug, M.; Jordhoy, M.S. Geriatric assessment is superior to oncologists’ clinical judgement in identifying frailty. Br. J. Cancer 2017, 117, 470–477. [Google Scholar] [CrossRef]
- Chodosh, J.; Petitti, D.B.; Elliott, M.; Hays, R.D.; Crooks, V.C.; Reuben, D.B.; Galen Buckwalter, J.; Wenger, N. Physician recognition of cognitive impairment: Evaluating the need for improvement. J. Am. Geriatr. Soc. 2004, 52, 1051–1059. [Google Scholar] [CrossRef]
- Rostoft, S.; van den Bos, F.; Pedersen, R.; Hamaker, M.E. Shared decision-making in older patients with cancer—What does the patient want? J. Geriatr. Oncol. 2021, 12, 339–342. [Google Scholar] [CrossRef]
- Wildiers, H.; Heeren, P.; Puts, M.; Topinkova, E.; Janssen-Heijnen, M.L.; Extermann, M.; Falandry, C.; Artz, A.; Brain, E.; Colloca, G.; et al. International Society of Geriatric Oncology consensus on geriatric assessment in older patients with cancer. J. Clin. Oncol. 2014, 32, 2595–2603. [Google Scholar] [CrossRef] [Green Version]
- Mohile, S.G.; Dale, W.; Somerfield, M.R.; Schonberg, M.A.; Boyd, C.M.; Burhenn, P.S.; Canin, B.; Cohen, H.J.; Holmes, H.M.; Hopkins, J.O.; et al. Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Chemotherapy: ASCO Guideline for Geriatric Oncology. J. Clin. Oncol. 2018, 36, 2326–2347. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bedirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Rambeau, A.; Beauplet, B.; Laviec, H.; Licaj, I.; Leconte, A.; Chatel, C.; Le Bon, P.; Denhaerynck, J.; Clarisse, B.; Frenkiel, N.; et al. Prospective comparison of the Montreal Cognitive Assessment (MoCA) and the Mini Mental State Examination (MMSE) in geriatric oncology. J. Geriatr. Oncol. 2019, 10, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Burhenn, P.S.; McCarthy, A.L.; Begue, A.; Nightingale, G.; Cheng, K.; Kenis, C. Geriatric assessment in daily oncology practice for nurses and allied health care professionals: Opinion paper of the Nursing and Allied Health Interest Group of the International Society of Geriatric Oncology (SIOG). J. Geriatr. Oncol. 2016, 7, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Loh, K.P.; Soto-Perez-de-Celis, E.; Hsu, T.; de Glas, N.A.; Battisti, N.M.L.; Baldini, C.; Rodrigues, M.; Lichtman, S.M.; Wildiers, H. What Every Oncologist Should Know About Geriatric Assessment for Older Patients with Cancer: Young International Society of Geriatric Oncology Position Paper. J. Oncol. Pract. 2018, 14, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Tuch, G.; Soo, W.K.; Luo, K.Y.; Frearson, K.; Oh, E.L.; Phillips, J.L.; Agar, M.; Lane, H. Cognitive Assessment Tools Recommended in Geriatric Oncology Guidelines: A Rapid Review. Curr. Oncol. 2021, 28, 3987–4003. [Google Scholar] [CrossRef]
- Eriksen, G.F.; Šaltytė Benth, J.; Grønberg, B.H.; Rostoft, S.; Kirkhus, L.; Kirkevold, Ø.; Hjelstuen, A.; Slaaen, M. Geriatric impairments are prevalent and predictive of survival in older patients with cancer receiving radiotherapy: A prospective observational study. Acta Oncol. 2021, 61, 393–402. [Google Scholar] [CrossRef]
- Innlandet Fylkeskommune. Fakta om Innlandet. Available online: https://innlandetfylke.no/om-fylkeskommunen/om-innlandet/fakta-om-innlandet/ (accessed on 31 March 2022).
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Fayers, P.; Aaronson, N.K.; Bordal, K.; Groenvold, M.; Curran, D.; Bottomley, A.; on behalf of the EORTC Quality of Life Group. The EORTC QLQ-30 Scoring Manual, 3rd ed.; European Organisation for Research and Treatment of Cancer: Brussels, Belgium, 2001. [Google Scholar]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Sheikh, J.I.; Yesavage, J.A. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clin. Gerontol. J. Aging Ment. Health 1986, 5, 165–173. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Harker, J.O.; Salva, A.; Guigoz, Y.; Vellas, B. Screening for undernutrition in geriatric practice: Developing the short-form mini-nutritional assessment (MNA-SF). J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef] [Green Version]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Gladman, J.R.; Lincoln, N.B.; Adams, S.A. Use of the extended ADL scale with stroke patients. Age Ageing 1993, 22, 419–424. [Google Scholar] [CrossRef] [PubMed]
- MoCA Cognitive Assessment. Available online: https://www.mocatest.org/ (accessed on 22 April 2022).
- Helse, A.O. MoCA Calculator. Available online: https://www.aldringoghelse.no/mocacalculator/ (accessed on 30 March 2022).
- Engedal, K.; Gjøra, L.; Benth, J.; Wagle, J.; Rønqvist, T.K.; Selbæk, G. The Montreal Cognitive Assessment: Normative Data from a Large, Population-Based Sample of Cognitive Healthy Older Adults in Norway-The HUNT Study. J. Alzheimers Dis. 2022, 86, 589–599. [Google Scholar] [CrossRef] [PubMed]
- O’Driscoll, C.; Shaikh, M. Cross-Cultural Applicability of the Montreal Cognitive Assessment (MoCA): A Systematic Review. J. Alzheimers Dis. 2017, 58, 789–801. [Google Scholar] [CrossRef]
- Kenny, R.A.; Coen, R.F.; Frewen, J.; Donoghue, O.A.; Cronin, H.; Savva, G.M. Normative values of cognitive and physical function in older adults: Findings from the Irish Longitudinal Study on Ageing. J. Am. Geriatr. Soc. 2013, 61 (Suppl. 2), S279–S290. [Google Scholar] [CrossRef]
- Waldron-Perrine, B.; Axelrod, B.N. Determining an appropriate cutting score for indication of impairment on the Montreal Cognitive Assessment. Int. J. Geriatr. Psychiatry 2012, 27, 1189–1194. [Google Scholar] [CrossRef]
- Davis, D.H.; Creavin, S.T.; Yip, J.L.; Noel-Storr, A.H.; Brayne, C.; Cullum, S. Montreal Cognitive Assessment for the detection of dementia. Cochrane Database Syst. Rev. 2021, 7, Cd010775. [Google Scholar] [CrossRef]
- Borland, E.; Nägga, K.; Nilsson, P.M.; Minthon, L.; Nilsson, E.D.; Palmqvist, S. The Montreal Cognitive Assessment: Normative Data from a Large Swedish Population-Based Cohort. J. Alzheimers Dis. 2017, 59, 893–901. [Google Scholar] [CrossRef] [Green Version]
- Wefel, J.S.; Vardy, J.; Ahles, T.; Schagen, S.B. International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol. 2011, 12, 703–708. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Auyeung, T.W.; Lee, J.S.; Kwok, T.; Woo, J. Physical frailty predicts future cognitive decline—A four-year prospective study in 2737 cognitively normal older adults. J. Nutr. Health Aging 2011, 15, 690–694. [Google Scholar] [CrossRef] [PubMed]
- Robertson, D.A.; Savva, G.M.; Kenny, R.A. Frailty and cognitive impairment--a review of the evidence and causal mechanisms. Ageing Res. Rev. 2013, 12, 840–851. [Google Scholar] [CrossRef] [PubMed]
- Njegovan, V.; Hing, M.M.; Mitchell, S.L.; Molnar, F.J. The hierarchy of functional loss associated with cognitive decline in older persons. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M638–M643. [Google Scholar] [CrossRef] [PubMed]
- Pergolotti, M.; Battisti, N.M.L.; Padgett, L.; Sleight, A.G.; Abdallah, M.; Newman, R.; Van Dyk, K.; Covington, K.R.; Williams, G.R.; van den Bos, F.; et al. Embracing the complexity: Older adults with cancer-related cognitive decline-A Young International Society of Geriatric Oncology position paper. J. Geriatr. Oncol. 2020, 11, 237–243. [Google Scholar] [CrossRef] [Green Version]
- Hurria, A.; Rosen, C.; Hudis, C.; Zuckerman, E.; Panageas, K.S.; Lachs, M.S.; Witmer, M.; van Gorp, W.G.; Fornier, M.; D’Andrea, G.; et al. Cognitive function of older patients receiving adjuvant chemotherapy for breast cancer: A pilot prospective longitudinal study. J. Am. Geriatr. Soc. 2006, 54, 925–931. [Google Scholar] [CrossRef]
- Mandelblatt, J.S.; Stern, R.A.; Luta, G.; McGuckin, M.; Clapp, J.D.; Hurria, A.; Jacobsen, P.B.; Faul, L.A.; Isaacs, C.; Denduluri, N.; et al. Cognitive impairment in older patients with breast cancer before systemic therapy: Is there an interaction between cancer and comorbidity? J. Clin. Oncol. 2014, 32, 1909–1918. [Google Scholar] [CrossRef] [Green Version]
- Ahles, T.A.; Hurria, A. New Challenges in Psycho-Oncology Research IV: Cognition and cancer: Conceptual and methodological issues and future directions. Psychooncology 2018, 27, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Ahles, T.A.; Schofield, E.; Li, Y.; Ryan, E.; Root, J.C.; Patel, S.K.; McNeal, K.; Gaynor, A.; Tan, H.; Katheria, V.; et al. Relationship between cognitive functioning and frailty in older breast cancer survivors. J. Geriatr. Oncol. 2022, 13, 27–32. [Google Scholar] [CrossRef]
- Magnuson, A.; Lei, L.; Gilmore, N.; Kleckner, A.S.; Lin, F.V.; Ferguson, R.; Hurria, A.; Wittink, M.N.; Esparaz, B.T.; Giguere, J.K.; et al. Longitudinal Relationship Between Frailty and Cognition in Patients 50 Years and Older with Breast Cancer. J. Am. Geriatr. Soc. 2019, 67, 928–936. [Google Scholar] [CrossRef]
- Shibayama, O.; Yoshiuchi, K.; Inagaki, M.; Matsuoka, Y.; Yoshikawa, E.; Sugawara, Y.; Akechi, T.; Wada, N.; Imoto, S.; Murakami, K.; et al. Association between adjuvant regional radiotherapy and cognitive function in breast cancer patients treated with conservation therapy. Cancer Med. 2014, 3, 702–709. [Google Scholar] [CrossRef]
- O’Donovan, A.; Leech, M.; Gillham, C. Assessment and management of radiotherapy induced toxicity in older patients. J. Geriatr. Oncol. 2017, 8, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Szumacher, E.; Sattar, S.; Neve, M.; Do, K.; Ayala, A.P.; Gray, M.; Lee, J.; Alibhai, S.; Puts, M. Use of Comprehensive Geriatric Assessment and Geriatric Screening for Older Adults in the Radiation Oncology Setting: A Systematic Review. Clin. Oncol. 2018, 30, 578–588. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, K.; Rossetti, H.; Hynan, L.S.; Carter, K.; Falkowski, J.; Lacritz, L.; Cullum, C.M.; Weiner, M. Changes in Montreal Cognitive Assessment Scores Over Time. Assessment 2017, 24, 772–777. [Google Scholar] [CrossRef]
- Repetto, L.; Fratino, L.; Audisio, R.A.; Venturino, A.; Gianni, W.; Vercelli, M.; Parodi, S.; Dal Lago, D.; Gioia, F.; Monfardini, S.; et al. Comprehensive geriatric assessment adds information to Eastern Cooperative Oncology Group performance status in elderly cancer patients: An Italian Group for Geriatric Oncology Study. J. Clin. Oncol. 2002, 20, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Hurria, A.; Togawa, K.; Mohile, S.G.; Owusu, C.; Klepin, H.D.; Gross, C.P.; Lichtman, S.M.; Gajra, A.; Bhatia, S.; Katheria, V.; et al. Predicting chemotherapy toxicity in older adults with cancer: A prospective multicenter study. J. Clin. Oncol. 2011, 29, 3457–3465. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Total N = 298 | Very Poor Group N = 19 | Poor Group N = 24 | Fair Group N = 113 | Good Group N = 142 | p-Value | |
|---|---|---|---|---|---|---|
| Age Mean (SD) Gender, n (%) Male Female Education, n (%) (1 missing) Compulsory Secondary College or university Comorbidity, CCI Mean (SD) Number of daily medications Mean (SD) Geriatric depression scale ≥5, n (%) No Yes | 73.6 (6.3) 157 (52.7) 141 (47.3) 90 (30.3) 120 (40.4) 87 (29.3) 1.1 (1.3) 5.4 (3.6) 236 (79.2) 62 (20.8) | 77.7 (7.6) 12 (63.2) 7 (36.8) 6 (33.3) 11 (61.1) 1 (5.6) 1.5 (1.4) 8.7 (4.4) 12 (63.2) 7 (36.8) | 76.3 (6.4) 9 (37.5) 15 (62.5) 17 (70.8) 5 (20.8) 2 (8.3) 1.4 (1.5) 7.2 (4.0) 17 (70.8) 7 (29.2) | 74.7 (6.4) 73 (64.6) 40 (35.4) 42 (38.2) 44 (40.0) 24 (21.8) 1.3 (1.6) 5.7 (3.7) 88 (77.9) 25 (22.1) | 71.8 (5.5) 63 (44.4) 79 (55.6) 25 (17.6) 58 (40.8) 59 (41.5) 0.8 (1.0) 4.5 (2.9) 119 (83.8) 23 (16.2) | <0.001 2 0.004 1 <0.001 1 0.003 2 <0.001 2 0.115 1 |
| Number of physical impairments Mean (SD) (3 missing) Fatigue Mean (SD) (3 missing) RT treatment intent, n (%) Curative Palliative Previous cancer treatment, n (%) Endocrine therapy Other systematic cancer therapy Cancer surgery/RT Brain cancer/brain metastases, n (%) No Yes | 1.3 (1.4) 37.4 (25.3) 162 (54.4) 136 (45.6) 57 (19.1) 90 (30.2) 182 (61.1) 282 (94.6) 16 (5.4) | 3.2 (1.6) 3 45.1 (24.3) 3 (15.8) 16 (84.2) 1 (5.3) 8 (42.1) 10 (52.6) 16 (84.2) 3 (15.8) | 1.9 (1.8) 38.9 (27.6) 13 (54.2) 11 (45.8) 7 (29.2) 5 (20.8) 16 (66.7) 22 (91.7) 2 (8.3) | 1.5 (1.5) 4 38.2 (26.7) 47 (41.6) 66 (58.4) 27 (23.9) 33 (29.2) 60 (53.1) 108 (95.6) 5 (4.4) | 0.8 (0.9) 35.5 (23.9) 99 (69.7) 43 (30.3) 22 (15.5) 44 (31.0) 96 (67.6) 136 (95.8) 6 (4.2) | <0.001 2 0.449 2 <0.001 1 0.079 1 0.499 1 0.091 1 0.169 1 |
| MoCA Domains | Maximum Score Possible | Mean Score | Standard Deviation | % with Less than Maximum Score |
|---|---|---|---|---|
| Visuospatial abilities | 5 | 3.8 | 1.3 | 65.1 |
| Naming of objects | 3 | 2.9 | 0.4 | 9.4 |
| Attention and concentration | 6 | 5.2 | 1.1 | 46.6 |
| Language | 3 | 2.1 | 0.8 | 68.1 |
| Abstraction | 2 | 1.3 | 0.7 | 59.1 |
| Working memory | 5 | 2.2 | 1.6 | 91.9 |
| Orientation to time and place | 6 | 5.8 | 0.7 | 13.8 |
| Total (n = 278 a) | Completers (n = 167) | Non-Completers (n = 111) | p-Value b | Non-Completers, Deceased (n = 36) | Non-Completers, Alive (n = 75) |
|---|---|---|---|---|---|
| Baseline MoCA score, mean (SD) Age, mean (SD) Gender, n (%) Male Female Education, n (%) (1 missing) Compulsory Secondary College or university Comorbidity, CCI, mean (SD) Number of daily medications, mean (SD) Geriatric depression scale ≥5, n (%) No Yes | 24.7 (3.3) 72.9 (5.9) 81 (48.5) 86 (51.5) 48 (28.7) 68 (40.7) 51 (30.5) 1.0 (1.3) 5.0 (3.5) 136 (81.4) 31 (18.6) | 22.9 (4.1) 74.2 (6.7) 63 (56.8) 48 (43.2) 33 (29.7) 47 (42.3) 30 (27.0) 1.2 (1.5) 6.1 (3.7) 82 (73.9) 29 (26.1) | ˂0.001 c 0.107 c 0.177 d 0.843 d 0.246 c 0.020c 0.133 d | 21.9 (4.5) 74.2 (7.1) 26 (72.2) 10 (27.8) 12 (33.3) 15 (41.7) 9 (25.0) 1.6 (1.4) 7.6 (3.4) 26 (72.2) 10 (27.8) | 23.4 (3.8) 74.2 (6.5) 37 (49.3) 38 (50.7) 21 (28.0) 32 (42.7) 21 (28.0) 1.0 (1.5) 5.3 (3.7) 56 (74.7) 19 (25.3) |
| Number of physical impairments, mean (SD), (3 missing) Fatigue, mean (SD) (3 missing) RT treatment intent, n (%) Curative Palliative Previous cancer treatment, n (%) Endocrine therapy Other systematic cancer therapy Cancer surgery/RT Cancer/metastases in the brain, n (%) No Yes | 0.9 (1.1) 34.3 (23.9) 111 (66.5) 56 (33.5) 38 (22.8) 42 (25.1) 115 (68.9) 162 (97.0) 5 (3.0) | 1.9 (1.7) 43.1 (27.2) 40 (36.0) 71 (64.0) 15 (13.5) 42 (37.8) 56 (50.5) 101 (91.0) 10 (9.0) | ˂0.001 c 0.005 c ˂0.001 d 0.163 d 0.024 d 0.002 d 0.030 d | 2.5 (1.6) 58.7 (22.8) 2 (5.6) 34 (94.4) 4 (11.1) 19 (52.8) 16 (44.4) 28 (77.8) 8 (22.2) | 1.6 (1.6) 35.7 (26.0) 38 (50.7) 37 (49.3) 11 (14.7) 23 (30.7) 40 (53.3) 73 (97.3) 2 (2.7) |
| Covariate | Unadjusted Models | Adjusted Model | ||
|---|---|---|---|---|
| RC (95% CI) | p-Value | RC (95% CI) | p-Value | |
| Age Gender, Female Education, n Compulsory Secondary College or university Comorbidity, CCI Number of daily medications Geriatric depression scale ≥5 | −0.22 (−0.28; −0.16) 0.72 (−0.12; 1.57) 0 1.42 (0.47; 2.37) 3.35 (2.32; 4.38) −0.63 (−0.94; −0.33) −0.37 (−0.48; −0.25) −1.48 (−2.51; −0.45) | <0.001 0.094 0.004 <0.001 <0.001 <0.001 0.005 | −0.13 (−0.19; −0.07) 0.28 (−0.49; 1.05) 0 0.73 (−0.11; 1.57) 2.41 (1.50; 3.33) 0.02 (−0.30; 0.33) −0.11 (−0.24; 0.02) −0.26 (−1.25; 0.74) | <0.001 0.479 0.089 <0.001 0.924 0.107 0.613 |
| Number of physical impairments Fatigue RT treatment intent, Palliative Previous cancer treatment Endocrine therapy Other systematic cancer therapy Cancer surgery/RT Cancer/metastases in the brain | −1.23 (−1.49; −0.97) −0.02 (−0.04; −0.003) −1.84 (−2.67; −1.02) −0.12 (−1.20; 0.96) 0.43 (−0.49; 1.36) 0.89 (0.03; 1.76) −0.98 (−2.85; 0.88) | <0.001 0.021 <0.001 0.822 0.360 0.043 0.300 | −0.82 (−1.16; −0.48) 0.01 (−0.004; 0.03) −0.54 (−1.41; 0.33) 0.14 (−0.81; 1.08) 0.55 (−0.32; 1.42) 0.09 (−0.69; 0.87) −0.06 (−1.70; 1.58) | <0.001 0.141 0.223 0.778 0.216 0.817 0.940 |
| Very Poor N = 19 (6.4%) | Poor N = 24 (8.1%) | Fair N = 113 (37.9%) | Good N = 142 (47.7%) | |||||
|---|---|---|---|---|---|---|---|---|
| RC (SE) | p-Value | RC (SE) | p-Value | RC (SE) | p-Value | RC (SE) | p-Value | |
| Intercept Linear Quadratic MoCA a T0 T1 T2 T3 | 16.36 (0.60) −0.93 (0.24) 0.05 (0.01) 16.4 14.1 12.5 17.7 | <0.001 <0.001 <0.001 | 20.49 (0.58) 0.02 (0.05) 20.5 20.6 20.7 20.9 | <0.001 0.641 | 22.79 (0.37) 0.41 (0.08) −0.01 (0.004) 22.8 23.9 25.7 26.0 | <0.001 <0.001 0.004 | 26.68 (0.23) 0.43 (0.07) −0.01 (0.003) 26.6 27.6 28.9 29.0 | <0.001 <0.001 <0.001 |
| Av.prob. | 0.84 | 0.86 | 0.79 | 0.91 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eriksen, G.F.; Šaltytė Benth, J.; Grønberg, B.H.; Rostoft, S.; Kirkevold, Ø.; Bergh, S.; Hjelstuen, A.; Rolfson, D.; Slaaen, M. Cognitive Trajectories in Older Patients with Cancer Undergoing Radiotherapy—A Prospective Observational Study. Curr. Oncol. 2022, 29, 5164-5178. https://doi.org/10.3390/curroncol29070409
Eriksen GF, Šaltytė Benth J, Grønberg BH, Rostoft S, Kirkevold Ø, Bergh S, Hjelstuen A, Rolfson D, Slaaen M. Cognitive Trajectories in Older Patients with Cancer Undergoing Radiotherapy—A Prospective Observational Study. Current Oncology. 2022; 29(7):5164-5178. https://doi.org/10.3390/curroncol29070409
Chicago/Turabian StyleEriksen, Guro Falk, Jūratė Šaltytė Benth, Bjørn Henning Grønberg, Siri Rostoft, Øyvind Kirkevold, Sverre Bergh, Anne Hjelstuen, Darryl Rolfson, and Marit Slaaen. 2022. "Cognitive Trajectories in Older Patients with Cancer Undergoing Radiotherapy—A Prospective Observational Study" Current Oncology 29, no. 7: 5164-5178. https://doi.org/10.3390/curroncol29070409
APA StyleEriksen, G. F., Šaltytė Benth, J., Grønberg, B. H., Rostoft, S., Kirkevold, Ø., Bergh, S., Hjelstuen, A., Rolfson, D., & Slaaen, M. (2022). Cognitive Trajectories in Older Patients with Cancer Undergoing Radiotherapy—A Prospective Observational Study. Current Oncology, 29(7), 5164-5178. https://doi.org/10.3390/curroncol29070409





