The Effect of Surgeon Volume on the Outcome of Laser Vaporization: A Single-Center Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Eligibility
2.2. Clinical Variables
2.3. Outcome Measures
2.4. Treatment Follow-Up
2.5. Study Definitions
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wright, J.D.; Chen, L.; Tergas, A.I.; Melamed, A.; St Clair, C.M.; Hou, J.Y.; Khoury-Collado, F.; Gockley, A.; Accordino, M.; Hershman, D.L. Overuse of Cervical Cancer Screening Tests Among Women With Average Risk in the United States From 2013 to 2014. JAMA Netw. Open 2021, 4, e218373. [Google Scholar] [CrossRef] [PubMed]
- Fontham, E.T.H.; Wolf, A.M.D.; Church, T.R.; Etzioni, R.; Flowers, C.R.; Herzig, A.; Guerra, C.E.; Oeffinger, K.C.; Shih, Y.T.; Walter, L.C.; et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J. Clin. 2020, 70, 321–346. [Google Scholar] [CrossRef] [PubMed]
- Kyrgiou, M.; Athanasiou, A.; Kalliala, I.E.J.; Paraskevaidi, M.; Mitra, A.; Martin-Hirsch, P.P.; Arbyn, M.; Bennett, P.; Paraskevaidis, E. Obstetric outcomes after conservative treatment for cervical intraepithelial lesions and early invasive disease. Cochrane Database Syst. Rev. 2017, 2017, CD012847. [Google Scholar] [CrossRef] [PubMed]
- Tainio, K.; Athanasiou, A.; Tikkinen, K.A.O.; Aaltonen, R.; Cardenas, J.; Hernandes; Glazer-Livson, S.; Jakobsson, M.; Joronen, K.; Kiviharju, M.; et al. Clinical course of untreated cervical intraepithelial neoplasia grade 2 under active surveillance: Systematic review and meta-analysis. BMJ 2018, 360, k499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perkins, R.B.; Guido, R.S.; Castle, P.E.; Chelmow, D.; Einstein, M.H.; Garcia, F.; Huh, W.K.; Kim, J.J.; Moscicki, A.B.; Nayar, R.; et al. 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors. J. Low. Genit. Tract Dis. 2020, 24, 102–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petry, K.U. Management options for cervical intraepithelial neoplasia. Best Pract. Res. Clin. Obstet. Gynaecol. 2011, 25, 641–651. [Google Scholar] [CrossRef]
- Mitra, D.A.; Tzafetas, D.M.; Lyons, D.D.; Fotopoulou, P.C.; Paraskevaidis, P.E.; Kyrgiou, D.M. Cervical intraepithelial neoplasia: Screening and management. Br. J. Hosp. Med. 2016, 77, C118–C123. [Google Scholar] [CrossRef]
- Nam, K.H.; Kwon, J.Y.; Kim, Y.H.; Park, Y.W. Pregnancy outcome after cervical conization: Risk factors for preterm delivery and the efficacy of prophylactic cerclage. J. Gynecol. Oncol. 2010, 21, 225–229. [Google Scholar] [CrossRef] [Green Version]
- Kyrgiou, M.; Koliopoulos, G.; Martin-Hirsch, P.; Arbyn, M.; Prendiville, W.; Paraskevaidis, E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: Systematic review and meta-analysis. Lancet 2006, 367, 489–498. [Google Scholar] [CrossRef]
- Forsmo, S.; Hansen, M.H.; Jacobsen, B.K.; Oian, P. Pregnancy outcome after laser surgery for cervical intraepithelial neoplasia. Acta Obstet. Gynecol. Scand. 1996, 75, 139–143. [Google Scholar] [CrossRef]
- Yoon, B.S.; Seong, S.J.; Song, T.; Kim, M.L.; Kim, M.K. Risk factors for treatment failure of CO2 laser vaporization in cervical intraepithelial neoplasia 2. Arch. Gynecol. Obstet. 2014, 290, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, M.F.; Tortolero-Luna, G.; Cook, E.; Whittaker, L.; Rhodes-Morris, H.; Silva, E. A randomized clinical trial of cryotherapy, laser vaporization, and loop electrosurgical excision for treatment of squamous intraepithelial lesions of the cervix. Obstet. Gynecol. 1998, 92, 737–744. [Google Scholar] [CrossRef] [PubMed]
- Bahadoer, R.R.; Dijkstra, E.A.; van Etten, B.; Marijnen, C.A.M.; Putter, H.; Kranenbarg, E.M.; Roodvoets, A.G.H.; Nagtegaal, I.D.; Beets-Tan, R.G.H.; Blomqvist, L.K.; et al. Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): A randomised, open-label, phase 3 trial. Lancet Oncol. 2021, 22, 29–42. [Google Scholar] [CrossRef]
- Boyd, L.R.; Novetsky, A.P.; Curtin, J.P. Effect of surgical volume on route of hysterectomy and short-term morbidity. Obstet. Gynecol. 2010, 116, 909–915. [Google Scholar] [CrossRef]
- Wallenstein, M.R.; Ananth, C.V.; Kim, J.H.; Burke, W.M.; Hershman, D.L.; Lewin, S.N.; Neugut, A.I.; Lu, Y.S.; Herzog, T.J.; Wright, J.D. Effect of surgical volume on outcomes for laparoscopic hysterectomy for benign indications. Obstet. Gynecol. 2012, 119, 709–716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsuo, K.; Matsuzaki, S.; Mandelbaum, R.S.; Matsushima, K.; Klar, M.; Grubbs, B.H.; Roman, L.D.; Wright, J.D. Hospital surgical volume and perioperative mortality of pelvic exenteration for gynecologic malignancies. J. Surg. Oncol. 2019, 121, 402–409. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [Green Version]
- Drukker, L.; Hants, Y.; Farkash, R.; Grisaru-Granovsky, S.; Shen, O.; Samueloff, A.; Sela, H.Y. Impact of surgeon annual volume on short-term maternal outcome in cesarean delivery. Am. J. Obstet. Gynecol. 2016, 215, 85.e1–85.e8. [Google Scholar] [CrossRef] [Green Version]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [Green Version]
- Kodama, K.; Yahata, H.; Okugawa, K.; Tomonobe, H.; Yasutake, N.; Yoshida, S.; Yagi, H.; Yasunaga, M.; Ohgami, T.; Onoyama, I.; et al. Prognostic outcomes and risk factors for recurrence after laser vaporization for cervical intraepithelial neoplasia: A single-center retrospective study. Int. J. Clin. Oncol. 2021, 26, 770–776. [Google Scholar] [CrossRef]
- Fallani, M.G.; Penna, C.; Fambrini, M.; Marchionni, M. Laser CO2 vaporization for high-grade cervical intraepithelial neoplasia: A long-term follow-up series. Gynecol. Oncol. 2003, 91, 130–133. [Google Scholar] [CrossRef]
- Mikami, M.; Ikeda, M.; Sato, H.; Iwase, H.; Enomoto, T.; Kobayashi, Y.; Katabuchi, H. The use of conization to identify and treat severe lesions among prediagnosed CIN1 and 2 patients in Japan. J. Gynecol. Oncol. 2018, 29, e46. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, K.; Matsuzaki, S.; Mandelbaum, R.S.; Chang, E.J.; Klar, M.; Matsushima, K.; Grubbs, B.H.; Roman, L.D.; Wright, J.D. Minimally invasive radical hysterectomy for early-stage cervical cancer: Volume-outcome relationship in the early experience period. Gynecol. Oncol. 2020, 158, 390–396. [Google Scholar] [CrossRef]
- Matsuzaki, S.; Klar, M.; Chang, E.J.; Matsuzaki, S.; Maeda, M.; Zhang, R.H.; Roman, L.D.; Matsuo, K. Minimally Invasive Surgery and Surgical Volume-Specific Survival and Perioperative Outcome: Unmet Need for Evidence in Gynecologic Malignancy. J. Clin. Med. 2021, 10, 4787. [Google Scholar] [CrossRef] [PubMed]
- Mowat, A.; Maher, C.; Ballard, E. Surgical outcomes for low-volume vs high-volume surgeons in gynecology surgery: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2016, 215, 21–33. [Google Scholar] [CrossRef] [Green Version]
- Wright, J.D.; Lewin, S.N.; Deutsch, I.; Burke, W.M.; Sun, X.; Herzog, T.J. The influence of surgical volume on morbidity and mortality of radical hysterectomy for cervical cancer. Am. J. Obstet. Gynecol. 2011, 205, 225.e1–225.e7. [Google Scholar] [CrossRef]
- Wright, J.D.; Hershman, D.L.; Burke, W.M.; Lu, Y.S.; Neugut, A.I.; Lewin, S.N.; Herzog, T.J. Influence of surgical volume on outcome for laparoscopic hysterectomy for endometrial cancer. Ann. Surg. Oncol. 2012, 19, 948–958. [Google Scholar] [CrossRef]
- DeMott, R.K. Laser vs cryotherapy for CIN and a LEEP of faith. JAMA 1993, 269, 46. [Google Scholar] [CrossRef]
- Ruiz, M.P.; Chen, L.; Hou, J.Y.; Tergas, A.I.; St Clair, C.M.; Ananth, C.V.; Neugut, A.I.; Hershman, D.L.; Wright, J.D. Effect of Minimum-Volume Standards on Patient Outcomes and Surgical Practice Patterns for Hysterectomy. Obstet. Gynecol. 2018, 132, 1229–1237. [Google Scholar] [CrossRef]
- Wright, J.D. The Volume-Outcome Paradigm for Gynecologic Surgery: Clinical and Policy Implications. Clin. Obstet. Gynecol. 2020, 63, 252–265. [Google Scholar] [CrossRef]
- Queiroz, A.C.M.; Fabri, V.; Mantoan, H.; Sanches, S.M.; Guimaraes, A.P.G.; Ribeiro, A.R.G.; da Nogueira Silveira Lima, J.P.; Chen, M.J.; Baiocchi, G.; da Costa, A. Risk factors for pelvic and distant recurrence in locally advanced cervical cancer. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 235, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Ronsini, C.; Anchora, L.P.; Restaino, S.; Fedele, C.; Arciuolo, D.; Teodorico, E.; Bizzarri, N.; Zannoni, G.F.; Ferrandina, G.; Scambia, G.; et al. The role of semiquantitative evaluation of lympho-vascular space invasion in early stage cervical cancer patients. Gynecol. Oncol. 2021, 162, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Falcaro, M.; Castanon, A.; Ndlela, B.; Checchi, M.; Soldan, K.; Lopez-Bernal, J.; Elliss-Brookes, L.; Sasieni, P. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: A register-based observational study. Lancet 2021, 398, 2084–2092. [Google Scholar] [CrossRef]
- Ma, C.; Zhang, Y.; Li, R.; Mao, H.; Liu, P. Risk of parametrial invasion in women with early stage cervical cancer: A meta-analysis. Arch. Gynecol. Obstet. Arch. Gynecol. Obstet. 2018, 297, 573–580. [Google Scholar] [CrossRef] [PubMed]
| Patient Characteristics at Baseline | Values |
|---|---|
| Age, years | 36 (18–60) |
| BMI, kg/m2 | 20.5 (14.8–31.1) |
| Prior treatment | 25 (9.3) |
| Preoperative cytology | |
| ASC-US | 19 (7.0%) |
| LSIL | 51 (18.9%) |
| ASC-H | 12 (4.4%) |
| HSIL | 187 (69.3%) |
| AGC-NOS | 1 (0.5%) |
| Parity, n (%) | |
| 0 | 187 (69.3%) |
| ≥1 | 83 (30.7%) |
| HPV infection | |
| Positive | 158 (58.5%) |
| Negative | 6 (2.2%) |
| Not examined | 106 (39.3%) |
| Smoking, n (%) | |
| Yes | 120 (44.4%) |
| No | 150 (55.6%) |
| Use of contraception | |
| Yes | 14 (5.2%) |
| No | 256 (94.8%) |
| Surgeon volume | |
| High | 189 (70.0%) |
| Low | 81 (30.0%) |
| Persist or Rec | Yes | No | p-Value |
|---|---|---|---|
| n = 38 | n = 232 | ||
| Age | |||
| <50 | 34 (14.3%) | 208 (85.7%) | 0.99 |
| ≥50 | 4 (14.2%) | 24 (85.8%) | |
| Parity | |||
| 0 | 23 (12.3%) | 164 (87.3%) | 0.26 |
| ≥1 | 15 (18.1%) | 68 (81.9%) | |
| BMI | |||
| ≤25 | 37 (14.6%) | 217 (85.4%) | 0.71 |
| >25 | 1 (6.3%) | 15 (93.7%) | |
| Smoking | |||
| Yes | 16 (13.3%) | 104 (86.7%) | 0.86 |
| No | 22 (44%) | 128 (56%) | |
| OC | |||
| Yes | 1 (7.1%) | 13 (92.9%) | 0.70 |
| No | 37 (14.5%) | 219 (85.5%) | |
| Prior treatment | |||
| Yes | 2 (8%) | 23 (92%) | 0.74 |
| No | 36 (14.7%) | 209 (85.3%) | |
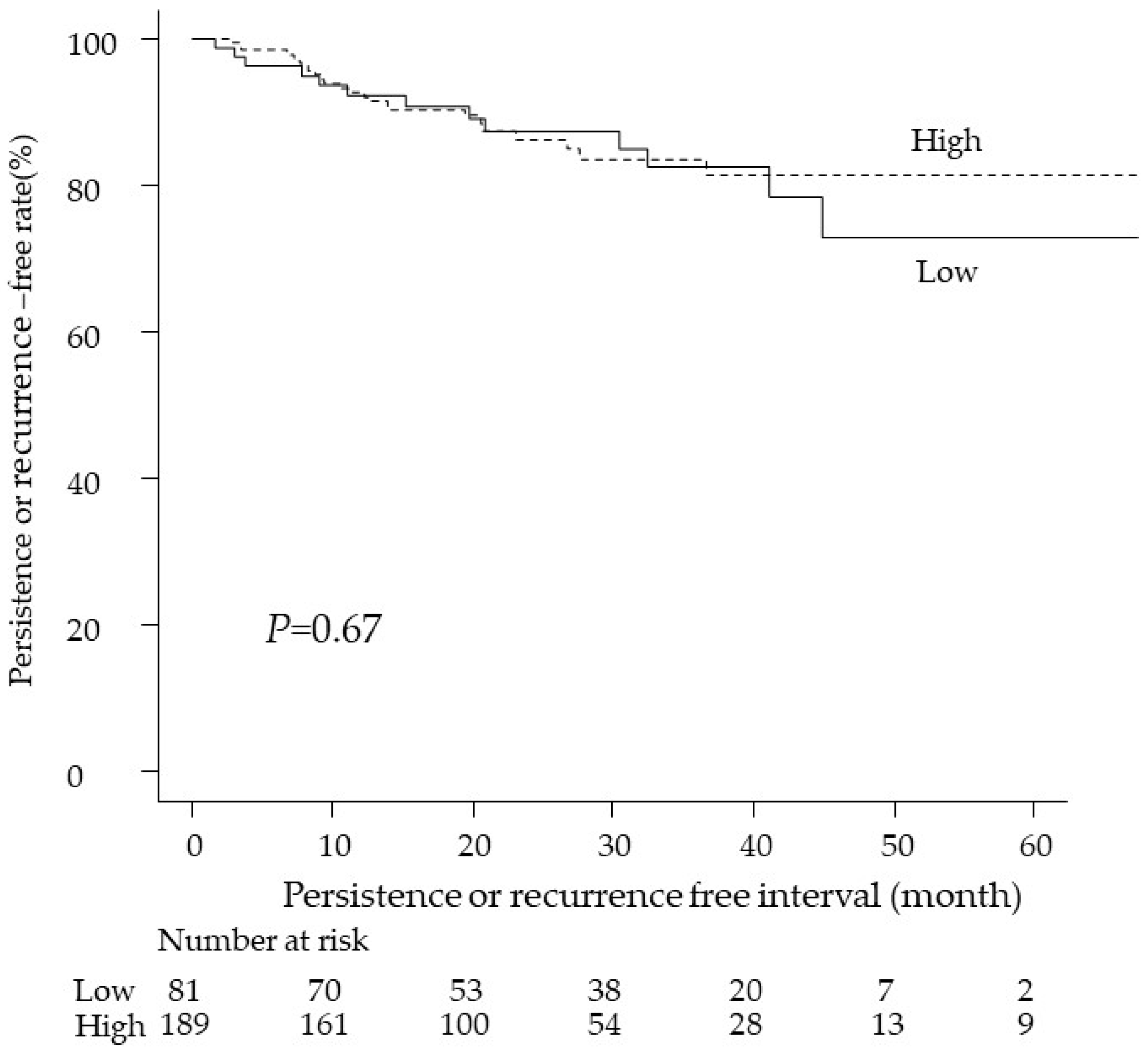
| Surgeon volume | |||
| High | 24 (12.7%) | 165 (87.3%) | 0.054 |
| Low | 14 (17.3%) | 67 (82.7%) |
| High | Low | p-Value | |
|---|---|---|---|
| n = 189 | n = 81 | ||
| Age | 36 (18–60) | 36 (21–53) | 0.56 |
| BMI | 20.1 (14.8–31.1) | 19.7 (16.2–26.7) | 0.44 |
| Parity | 0.25 | ||
| 0 | 135 (71.4%) | 52 (64.2%) | |
| ≥1 | 54 (28.6%) | 29 (35.8%) | |
| HPV | 0.29 | ||
| Positive | 131 (69.3%) | 27 (33.3%) | |
| Negative | 4 (2.1%) | 2 (2.5%) | |
| Not examined | 54 (28.6%) | 52 (64.2%) | |
| Smoking | 0.23 | ||
| Yes | 89 (47.1%) | 31 (38.3%) | |
| No | 100 (52.9%) | 50 (61.7%) | |
| OC | 0.56 | ||
| Yes | 11 (5.8%) | 3 (3.7%) | |
| No | 178 (94.2%) | 78 (96.3%) | |
| Prior treatment | 0.64 | ||
| Yes | 19 (10.1%) | 6 (7.4%) | |
| No | 170 (89.9%) | 75 (92.6%) | |
| Complications | 11 (5.8%) | 2 (2.5%) | 0.36 |
| Persist or rec | 24 (12.7%) | 14 (17.3%) | 0.34 |
| Univariate | Multivariate | ||||
|---|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | ||
| Age | <50 | 1 | 0.83 | 1 | 0.64 |
| ≥50 | 1.12 (0.40–3.17) | 1.29 (0.45- 3.69) | |||
| BMI | ≤25 | 1 | 0.47 | 1 | 0.44 |
| >25 | 0.48 (0.066–3.53) | 0.45 (0.062–3.69) | |||
| Surgeon volume | Low | 1 | 0.67 | 1 | 0.68 |
| High | 0.86 (0.47–1.68) | 0.87 (0.44–1.69) | |||
| Prior treatment | No | 1 | 0.24 | 1 | 0.21 |
| Yes | 0.42 (0.10–1.76) | 0.40 (0.096–1.69) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maeda, M.; Hisa, T.; Matsuzaki, S.; Lee, M.; Mabuchi, S.; Kamiura, S. The Effect of Surgeon Volume on the Outcome of Laser Vaporization: A Single-Center Retrospective Study. Curr. Oncol. 2022, 29, 3770-3779. https://doi.org/10.3390/curroncol29050302
Maeda M, Hisa T, Matsuzaki S, Lee M, Mabuchi S, Kamiura S. The Effect of Surgeon Volume on the Outcome of Laser Vaporization: A Single-Center Retrospective Study. Current Oncology. 2022; 29(5):3770-3779. https://doi.org/10.3390/curroncol29050302
Chicago/Turabian StyleMaeda, Michihide, Tsuyoshi Hisa, Shinya Matsuzaki, Misooja Lee, Seiji Mabuchi, and Shoji Kamiura. 2022. "The Effect of Surgeon Volume on the Outcome of Laser Vaporization: A Single-Center Retrospective Study" Current Oncology 29, no. 5: 3770-3779. https://doi.org/10.3390/curroncol29050302
APA StyleMaeda, M., Hisa, T., Matsuzaki, S., Lee, M., Mabuchi, S., & Kamiura, S. (2022). The Effect of Surgeon Volume on the Outcome of Laser Vaporization: A Single-Center Retrospective Study. Current Oncology, 29(5), 3770-3779. https://doi.org/10.3390/curroncol29050302





