Patient Experience with a Gynecologic Oncology-Initiated Genetic Testing Model for Women with Tubo-Ovarian Cancer
Abstract
:1. Introduction
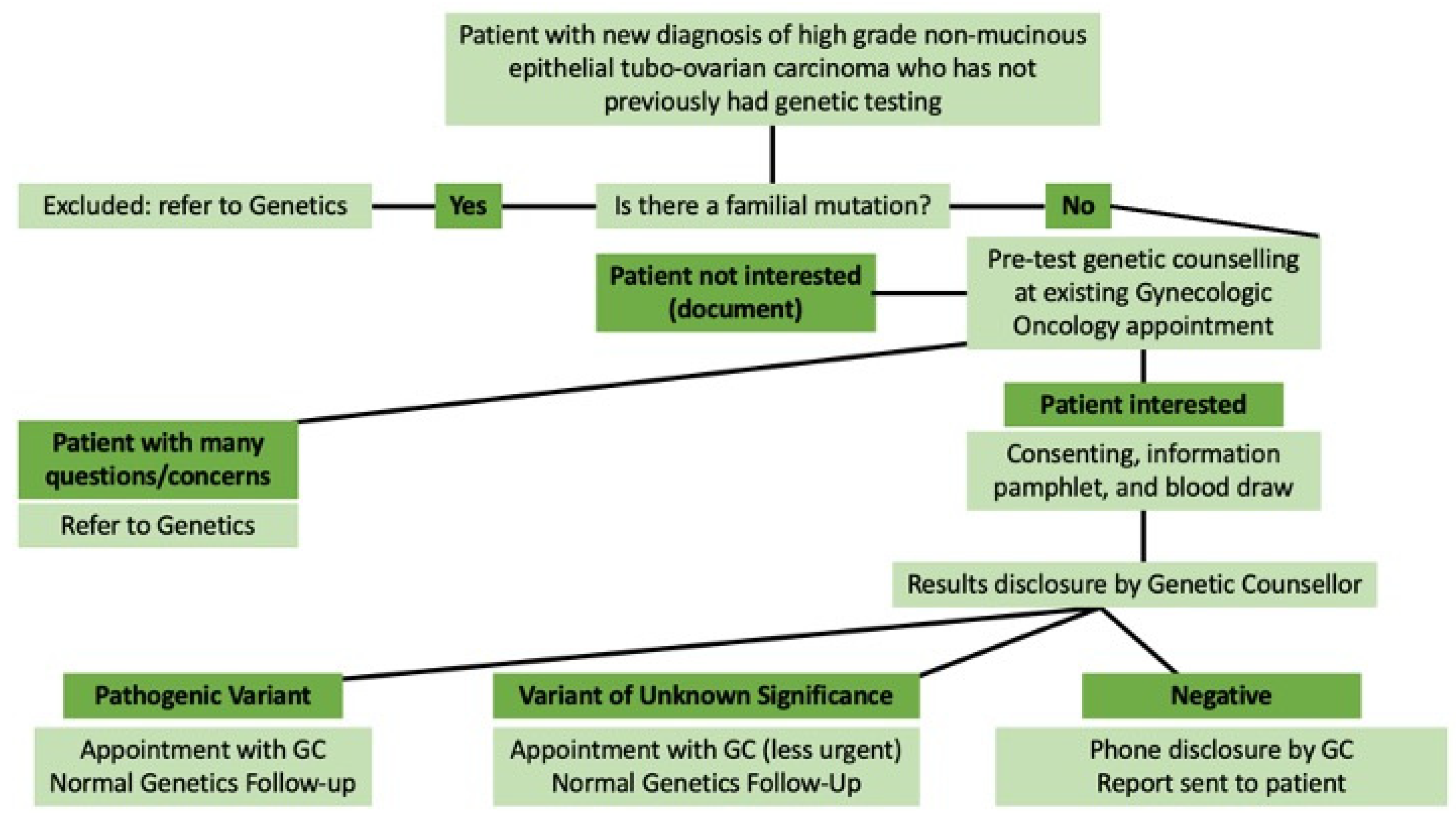
2. Materials and Methods
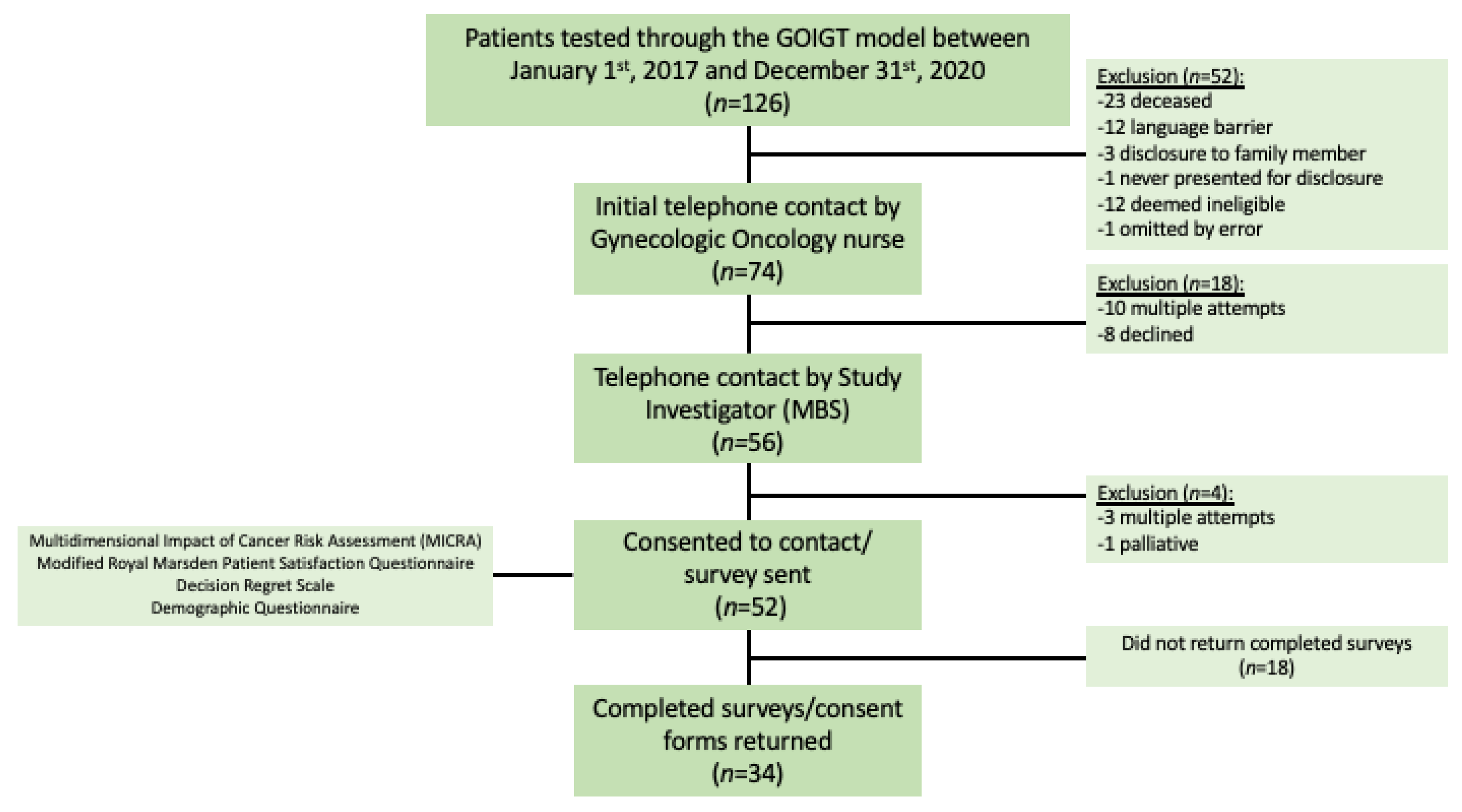
2.1. Study Participants
2.2. Measures
2.3. Data Analysis
3. Results
3.1. Participant Demographics
3.2. Multidimensional Impact of Cancer Risk Assessment
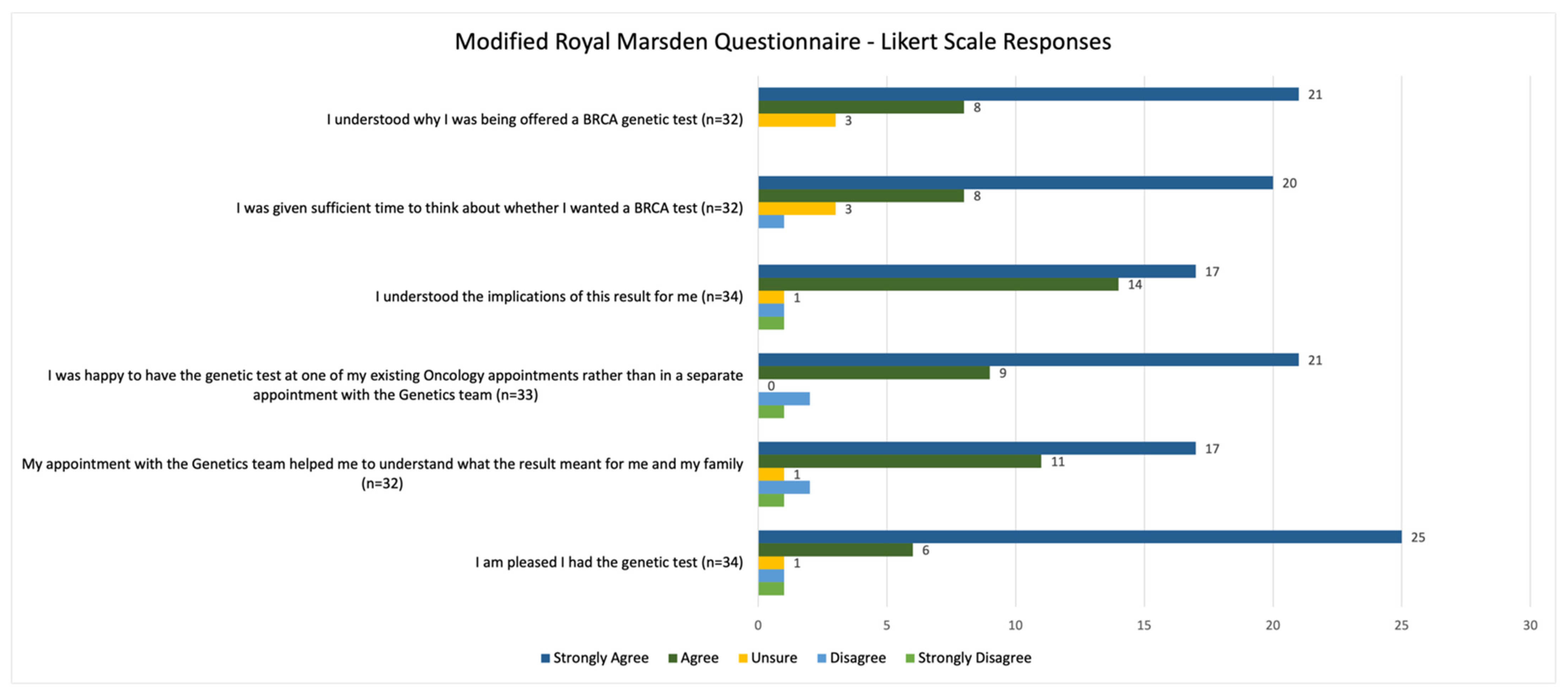
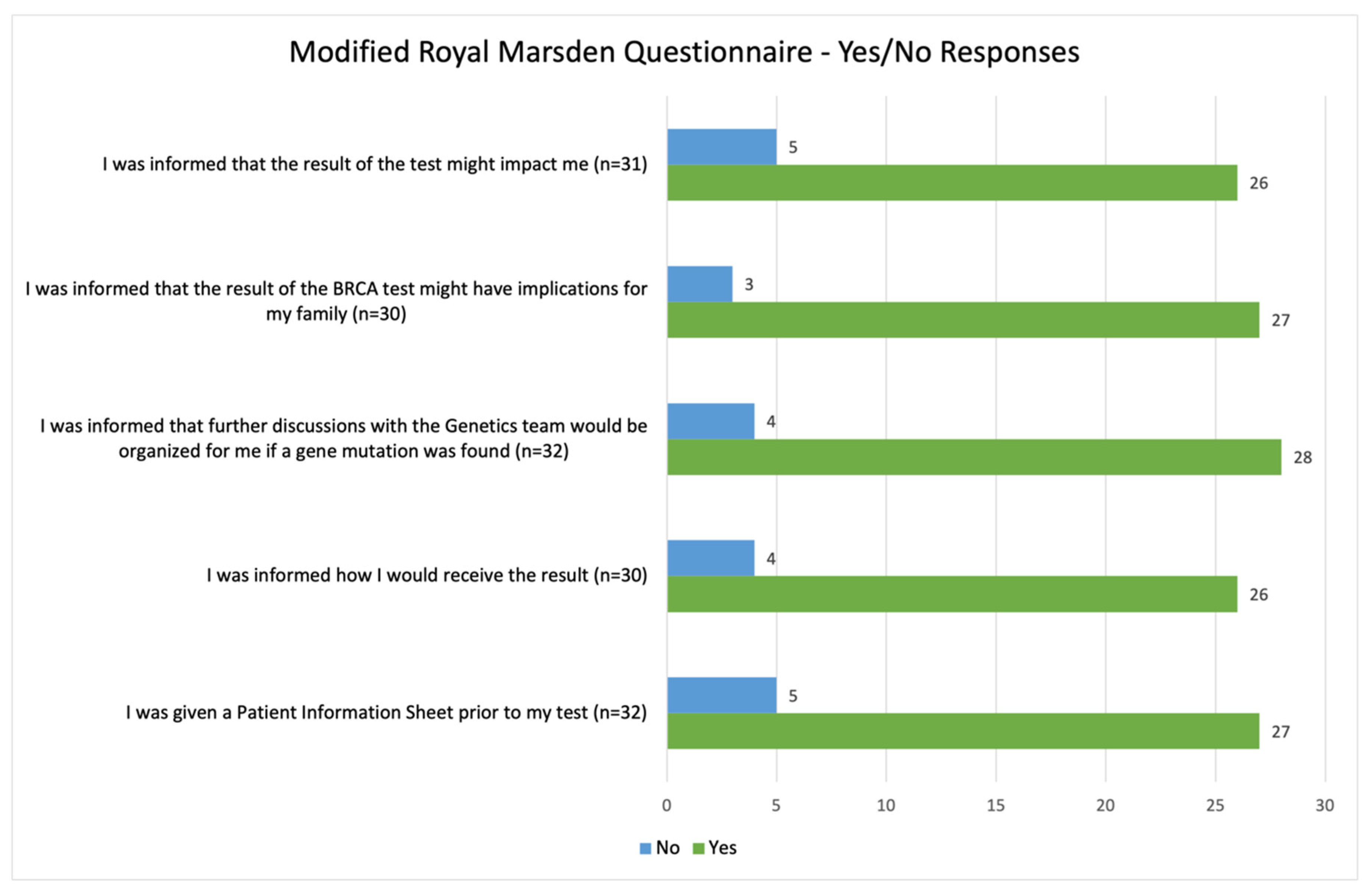
3.3. Modified Royal Marsden Patient Satisfaction Questionnaire
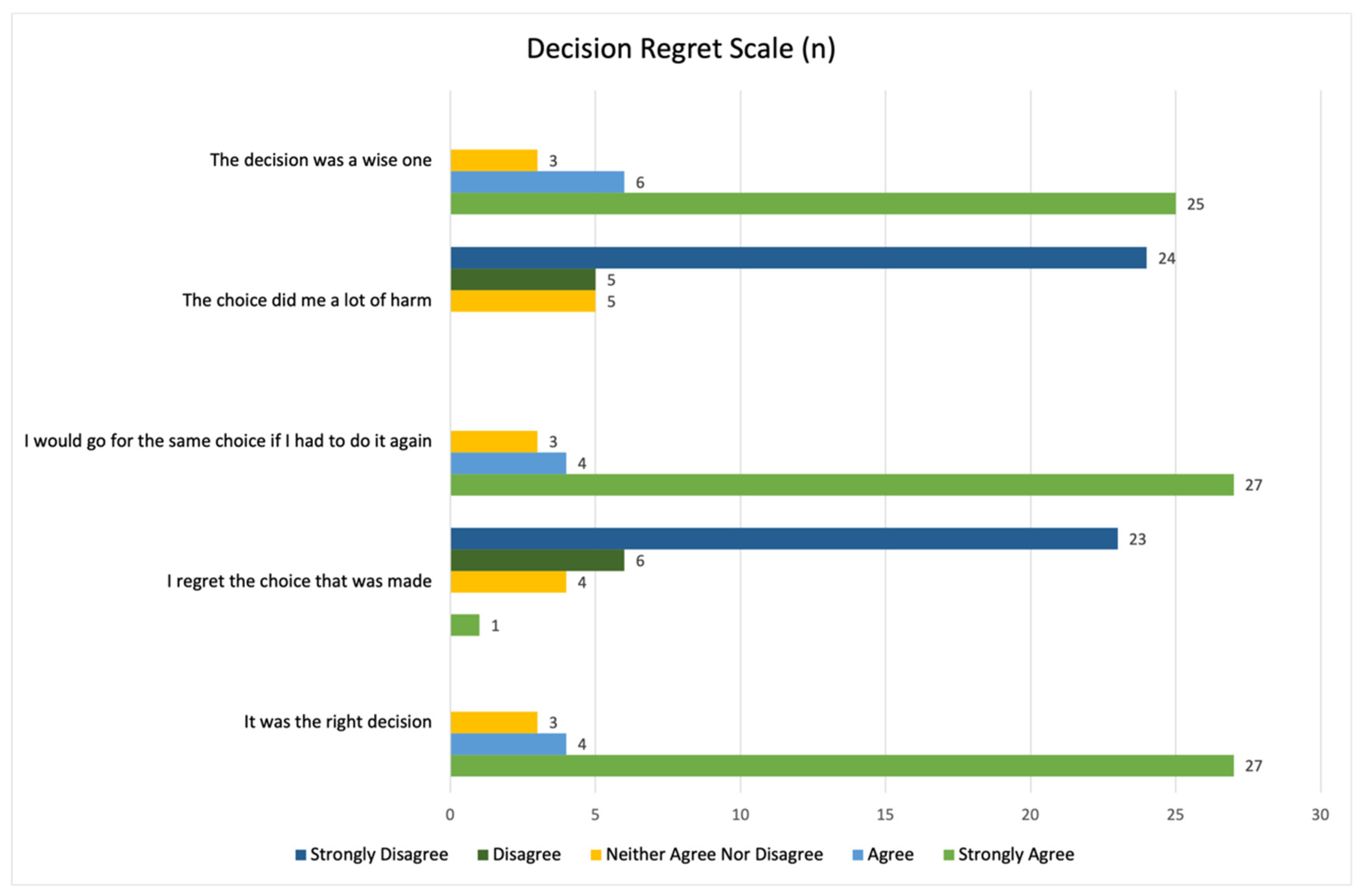
3.4. Decision Regret Scale
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, L.-M.; Berek, J.; Goff, B. Epithelial Carcinoma of the Ovary, Fallopian Tube, and Peritoneum: Clinical Features and Diagnosis. Uptodate. 2017. Available online: https://www.uptodate.com/contents/epithelial-carcinoma-of-the-ovary-fallopian-tube-and-peritoneum-clinical-features-and-diagnosis (accessed on 15 April 2021).
- Mafficini, A.; Simbolo, M.; Parisi, A.; Rusev, B.; Luchini, C.; Cataldo, I.; Piazzola, E.; Sperandio, N.; Turri, G.; Franchi, M.; et al. BRCA somatic and germline mutation detection in paraffin embedded ovarian cancers by next-generation sequencing. Oncotarget 2016, 7, 1076–1083. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norquist, B.M.; Harrell, M.I.; Brady, M.F.; Walsh, T.; Lee, M.K.; Gulsuner, S.; Bernards, S.S.; Casadei, S.; Yi, Q.; Burger, R.A.; et al. Inherited Mutations in Women with Ovarian Carcinoma. JAMA Oncol. 2016, 2, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Akbari, M.R.; Gojska, N.; Narod, S. Coming of Age in Canada: A Study of Population-Based Genetic Testing for Breast and Ovarian Cancer. Curr. Oncol. 2017, 24, 282–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurian, A.W.; Ward, K.C.; Howlader, N.; Deapen, D.; Hamilton, A.S.; Mariotto, A.; Miller, D.; Penberthy, L.S.; Katz, S.J. Genetic Testing and Results in a Population-Based Cohort of Breast Cancer Patients and Ovarian Cancer Patients. J. Clin. Oncol. 2019, 37, 1305–1315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pennington, K.P.; Walsh, T.; Harrell, M.I.; Lee, M.K.; Pennil, C.C.; Rendi, M.H.; Thornton, A.; Norquist, B.M.; Casadei, S.; Nord, A.S.; et al. Germline and Somatic Mutations in Homologous Recombination Genes Predict Platinum Response and Survival in Ovarian, Fallopian Tube, and Peritoneal Carcinomas. Clin. Cancer Res. 2014, 20, 764–775. [Google Scholar] [CrossRef] [Green Version]
- De Picciotto, N.; Cacheux, W.; Roth, A.; Chappuis, P.O.; Labidi-Galy, S.I. Ovarian cancer: Status of homologous recombination pathway as a predictor of drug response. Crit. Rev. Oncol. 2016, 101, 50–59. [Google Scholar] [CrossRef]
- McCuaig, J.M.; Stockley, T.; Shaw, P.; Fung-Kee-Fung, M.; Altman, A.; Bentley, J.; Bernardini, M.Q.; Cormier, B.; Hirte, H.; Kieser, K.; et al. Evolution of genetic assessment for BRCA-associated gynaecologic malignancies: A Canadian multisociety roadmap. J. Med. Genet. 2018, 55, 571–577. [Google Scholar] [CrossRef]
- SGOC. No Woman Left Behind: Toward a Pan-Canadian Strategy for Universal BRCA Testing in Ovarian Cancer [Position Statement]. 2017. Available online: https://g-o-c.org/wp-content/uploads/2015/01/17PosStmt_NWLB_Jan31_FINAL-EN.pdf (accessed on 25 March 2021).
- McGee, J.; Panabaker, K.; Leonard, S.; Ainsworth, P.; Elit, L.; Shariff, S.Z. Genetics Consultation Rates Following a Diagnosis of High-Grade Serous Ovarian Carcinoma in the Canadian Province of Ontario. Int. J. Gynecol. Cancer 2017, 27, 437–443. [Google Scholar] [CrossRef] [Green Version]
- Piedimonte, S.; Power, J.; Foulkes, W.D.; Weber, E.; Palma, L.; Schiavi, A.; Ambrosio, E.; Konci, R.; Gilbert, L.; Jardon, K.; et al. BRCA testing in women with high-grade serous ovarian cancer: Gynecologic oncologist-initiated testing compared with genetics referral. Int. J. Gynecol. Cancer 2020, 30, 1757–1761. [Google Scholar] [CrossRef]
- George, A.; Riddell, D.; Seal, S.; Talukdar, S.; Mahamdallie, S.; Ruark, E.; Cloke, V.; Slade, I.; Kemp, Z.; Gore, M.; et al. Implementing rapid, robust, cost-effective, patient-centred, routine genetic testing in ovarian cancer patients. Sci. Rep. 2016, 6, 29506. [Google Scholar] [CrossRef] [Green Version]
- Senter, L.; O’Malley, D.M.; Backes, F.J.; Copeland, L.J.; Fowler, J.M.; Salani, R.; Cohn, D.E. Genetic consultation embedded in a gynecologic oncology clinic improves compliance with guideline-based care. Gynecol. Oncol. 2017, 147, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Kentwell, M.; Dow, E.; Antill, Y.; Wrede, C.D.; McNally, O.; Higgs, E.; Hamilton, A.; Ananda, S.; Lindeman, G.; Scott, C.L. Mainstreaming cancer genetics: A model integrating germline BRCA testing into routine ovarian cancer clinics. Gynecol. Oncol. 2017, 145, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Rahman, B.; Lanceley, A.; Kristeleit, R.S.; Ledermann, J.; Lockley, M.; McCormack, M.; Mould, T.; Side, L. Mainstreamed genetic testing for women with ovarian cancer: First-year experience. J. Med. Genet. 2019, 56, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Wright, S.; Porteous, M.; Stirling, D.; Lawton, J.; Young, O.; Gourley, C.; Hallowell, N. Patients’ Views of Treatment-Focused Genetic Testing (TFGT): Some Lessons for the Mainstreaming of BRCA1 and BRCA2 Testing. J. Genet. Couns. 2018, 27, 1459–1472. [Google Scholar] [CrossRef] [Green Version]
- Grindedal, E.M.; Jørgensen, K.; Olsson, P.; Gravdehaug, B.; Lurås, H.; Schlichting, E.; Vamre, T.; Wangensteen, T.; Heramb, C.; Mæhle, L. Mainstreamed genetic testing of breast cancer patients in two hospitals in South Eastern Norway. Fam. Cancer 2020, 19, 133–142. [Google Scholar] [CrossRef] [Green Version]
- McCuaig, J.; Thain, E.; Malcolmson, J.; Keshavarzi, S.; Armel, S.; Kim, R. A Comparison of Patient-Reported Outcomes Following Consent for Genetic Testing Using an Oncologist- or Genetic Counselor-Mediated Model of Care. Curr. Oncol. 2021, 28, 1459–1471. [Google Scholar] [CrossRef]
- McLeavy, L.; Rahman, B.; Kristeleit, R.; Ledermann, J.; Lockley, M.; McCormack, M.; Mould, T.; Side, L.; Lanceley, A. Mainstreamed genetic testing in ovarian cancer: Patient experience of the testing process. Int. J. Gynecol. Cancer 2020, 30, 221–226. [Google Scholar] [CrossRef]
- Colombo, N.; Huang, G.; Scambia, G.; Chalas, E.; Pignata, S.; Fiorica, J.; Van Le, L.; Ghamande, S.; González-Santiago, S.; Bover, I.; et al. Evaluation of a Streamlined Oncologist-Led BRCA Mutation Testing and Counseling Model for Patients With Ovarian Cancer. J. Clin. Oncol. 2018, 36, 1300–1307. [Google Scholar] [CrossRef]
- Gilbert, L.; Basso, O.; Sampalis, J.; Karp, I.; Martins, C.; Feng, J.; Piedimonte, S.; Quintal, L.; Ramanakumar, A.V.; Takefman, J.; et al. Assessment of symptomatic women for early diagnosis of ovarian cancer: Results from the prospective DOvE pilot project. Lancet Oncol. 2012, 13, 285–291. [Google Scholar] [CrossRef]
- Cella, D.; Hughes, C.; Peterman, A.; Chang, C.-H.; Peshkin, B.N.; Schwartz, M.D.; Wenzel, L.; Lemke, A.; Marcus, A.C.; Lerman, C. A brief assessment of concerns associated with genetic testing for cancer: The multidimensional impact of cancer risk assessment (MICRA) questionnaire. Health Psychol. 2002, 21, 564–572. [Google Scholar] [CrossRef]
- Brehaut, J.C.; O’Connor, A.M.; Wood, T.; Hack, T.; Siminoff, L.; Gordon, E.; Feldman-Stewart, D. Validation of a Decision Regret Scale. Med. Decis. Mak. 2003, 23, 281–292. [Google Scholar] [CrossRef] [PubMed]
- Plaskocinska, I.; Shipman, H.; Drummond, J.; Thompson, E.; Buchanan, V.; Newcombe, B.; Hodgkin, C.; Barter, E.; Ridley, P.; Ng, R.; et al. New paradigms forBRCA1/BRCA2testing in women with ovarian cancer: Results of the Genetic Testing in Epithelial Ovarian Cancer (GTEOC) study. J. Med. Genet. 2016, 53, 655–661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez, M.M.B.; Menear, M.; Brehaut, J.C.; Légaré, F. Extent and Predictors of Decision Regret about Health Care Decisions. Med. Decis. Mak. 2016, 36, 777–790. [Google Scholar] [CrossRef] [PubMed]
| Participant Demographics | |
|---|---|
| Mean Age (Range) | 64.62 (40–84) |
| Urban vs. Rural, n (%) | Urban: 30 (88.2) |
| Rural: 4 (11.8) | |
| Primary Language, n (%) | English: 20 (58.8) |
| French: 12 (35.3) | |
| English and French: 1 (2.9) | |
| Other: 1 (2.9) | |
| Work Status, n (%) | Retired: 17 (50.0) |
| Disability/Sick Leave: 5 (14.7) | |
| Full-Time: 4 (11.8) | |
| Self-Employed, Part-Time: 1 (2.9) | |
| Self-Employed, Full-Time: 4 (11.8) | |
| Homemaker: 3 (8.8) | |
| Education, n (%) | Technical/Vocational/CEGEP: 11 (32.4) |
| University (Undergraduate): 10 (29.4) | |
| University (Graduate Degree): 6 (17.6) | |
| High School: 6 (17.6) | |
| Elementary School: 1 (2.9) |
| Possible Score Range | Mean (Median, Range) | |
|---|---|---|
| Distress | 0–45 | 3.97 (1.5, 0–19) |
| Uncertainty | 0–20 | 8.35 (7.5, 0–20) |
| Positive Experience | 0–20 | 9.65 (9.5, 0–20) |
| Total MICRA Score | 0–95 | 21.97 (20, 0–42) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sadinsky, M.B.; Power, J.; Ambrosio, E.; Palma, L.; Zeng, X.; Foulkes, W.D.; Weber, E. Patient Experience with a Gynecologic Oncology-Initiated Genetic Testing Model for Women with Tubo-Ovarian Cancer. Curr. Oncol. 2022, 29, 3565-3575. https://doi.org/10.3390/curroncol29050288
Sadinsky MB, Power J, Ambrosio E, Palma L, Zeng X, Foulkes WD, Weber E. Patient Experience with a Gynecologic Oncology-Initiated Genetic Testing Model for Women with Tubo-Ovarian Cancer. Current Oncology. 2022; 29(5):3565-3575. https://doi.org/10.3390/curroncol29050288
Chicago/Turabian StyleSadinsky, Michaela Bercovitch, Joanne Power, Enza Ambrosio, Laura Palma, Xing Zeng, William D. Foulkes, and Evan Weber. 2022. "Patient Experience with a Gynecologic Oncology-Initiated Genetic Testing Model for Women with Tubo-Ovarian Cancer" Current Oncology 29, no. 5: 3565-3575. https://doi.org/10.3390/curroncol29050288
APA StyleSadinsky, M. B., Power, J., Ambrosio, E., Palma, L., Zeng, X., Foulkes, W. D., & Weber, E. (2022). Patient Experience with a Gynecologic Oncology-Initiated Genetic Testing Model for Women with Tubo-Ovarian Cancer. Current Oncology, 29(5), 3565-3575. https://doi.org/10.3390/curroncol29050288





