Medical Assistance in Dying in Oncology Patients: A Canadian Academic Hospital’s Experience
Abstract
1. Introduction
2. Methods
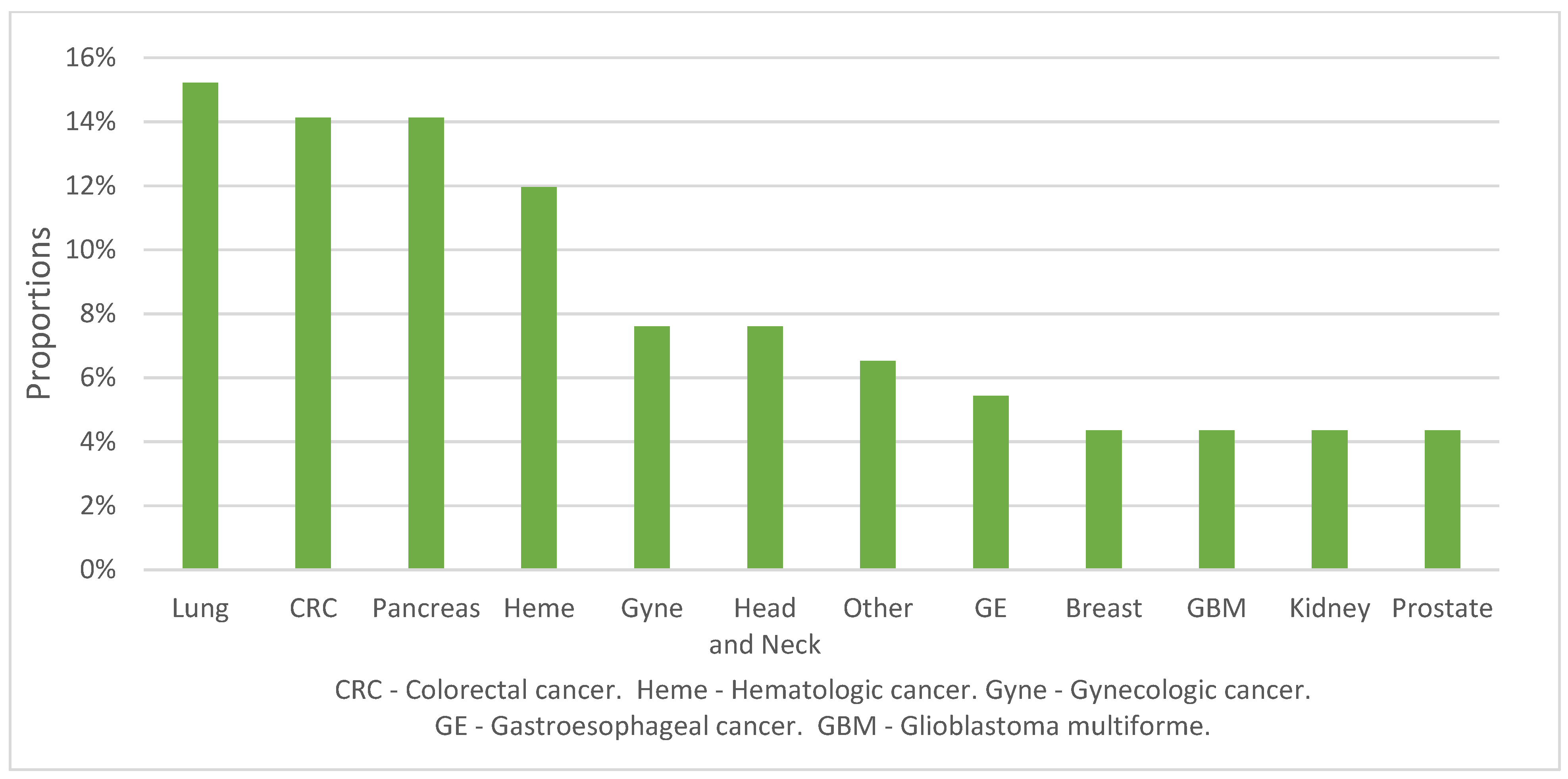
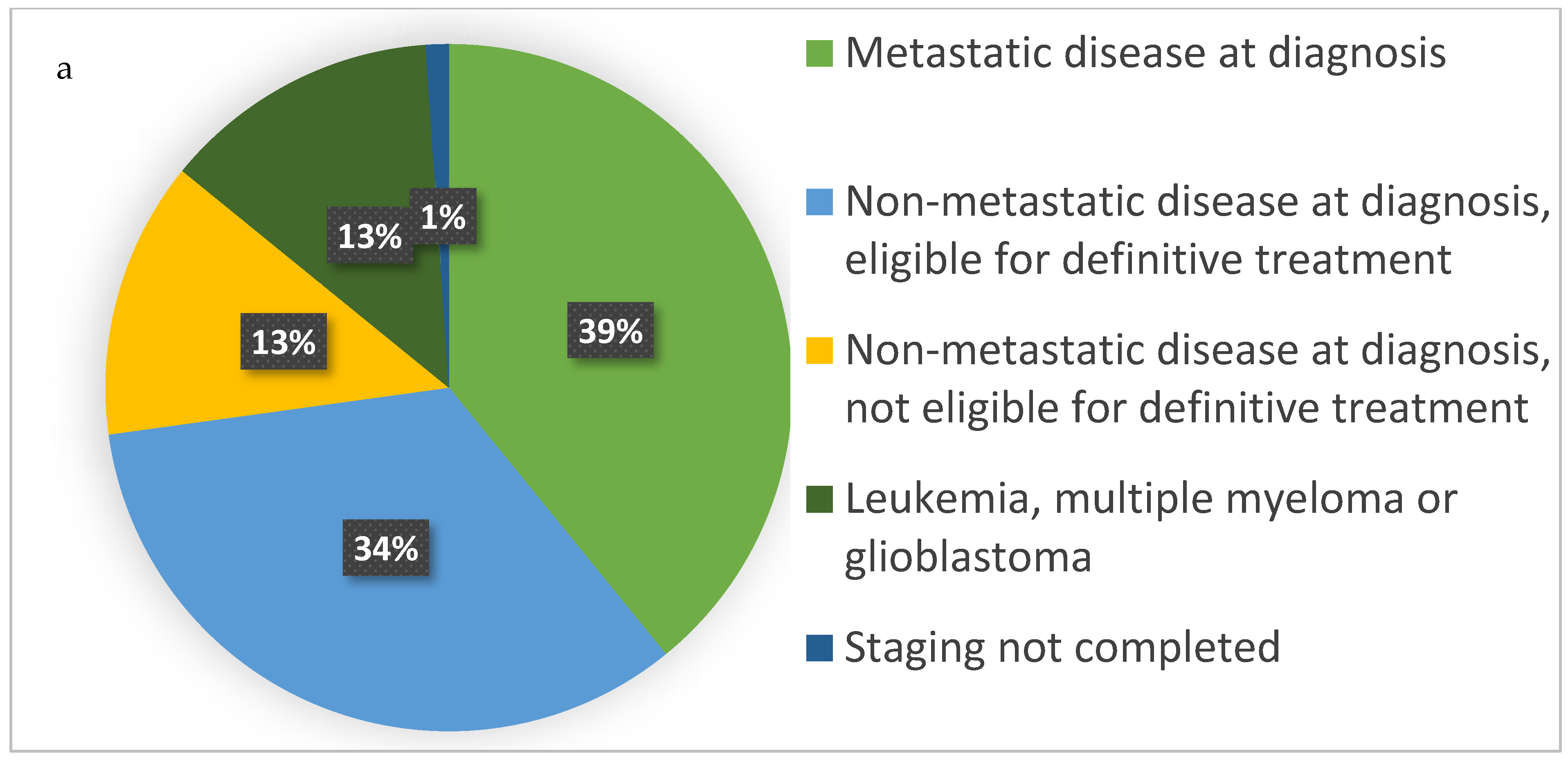
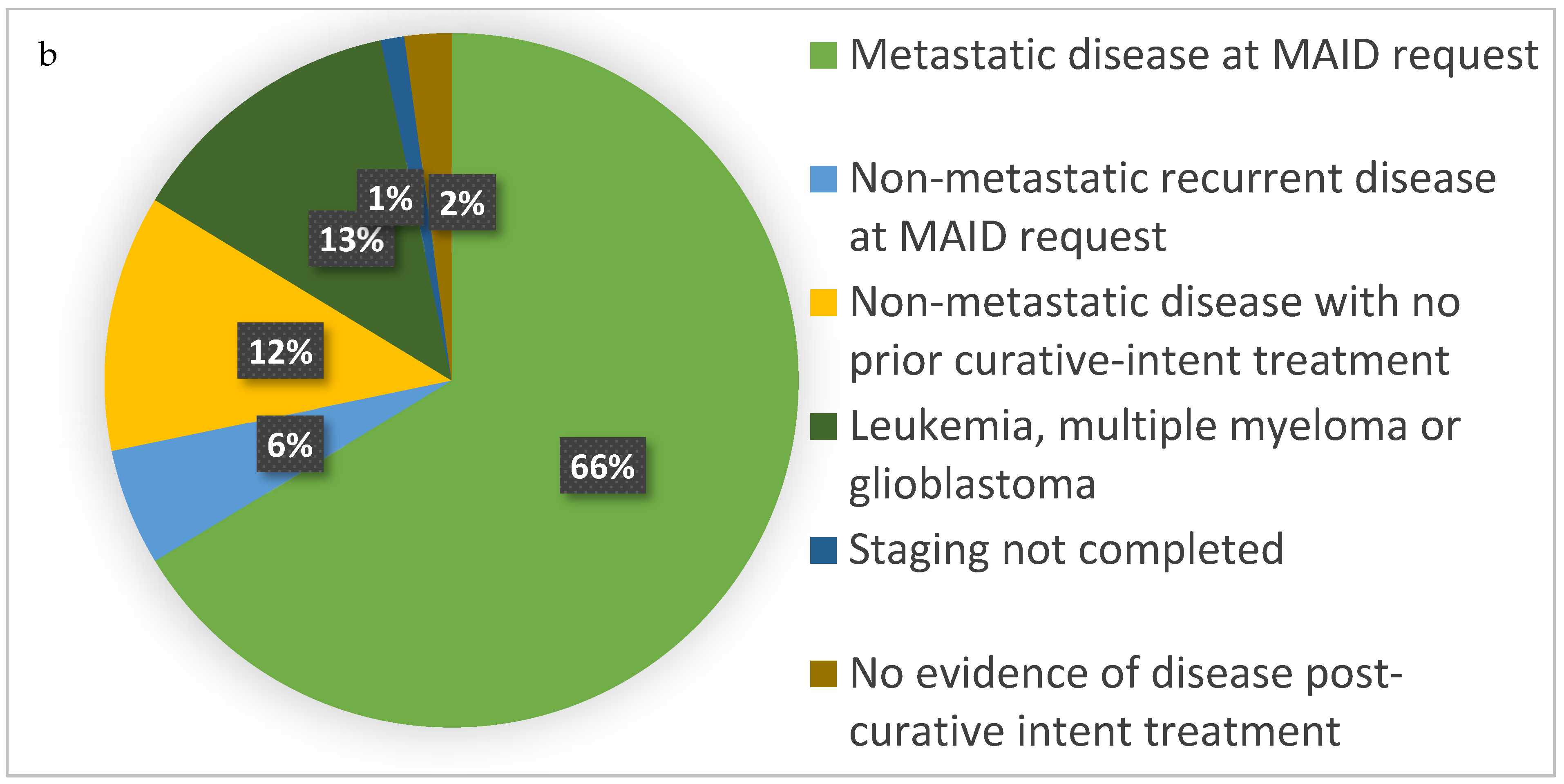
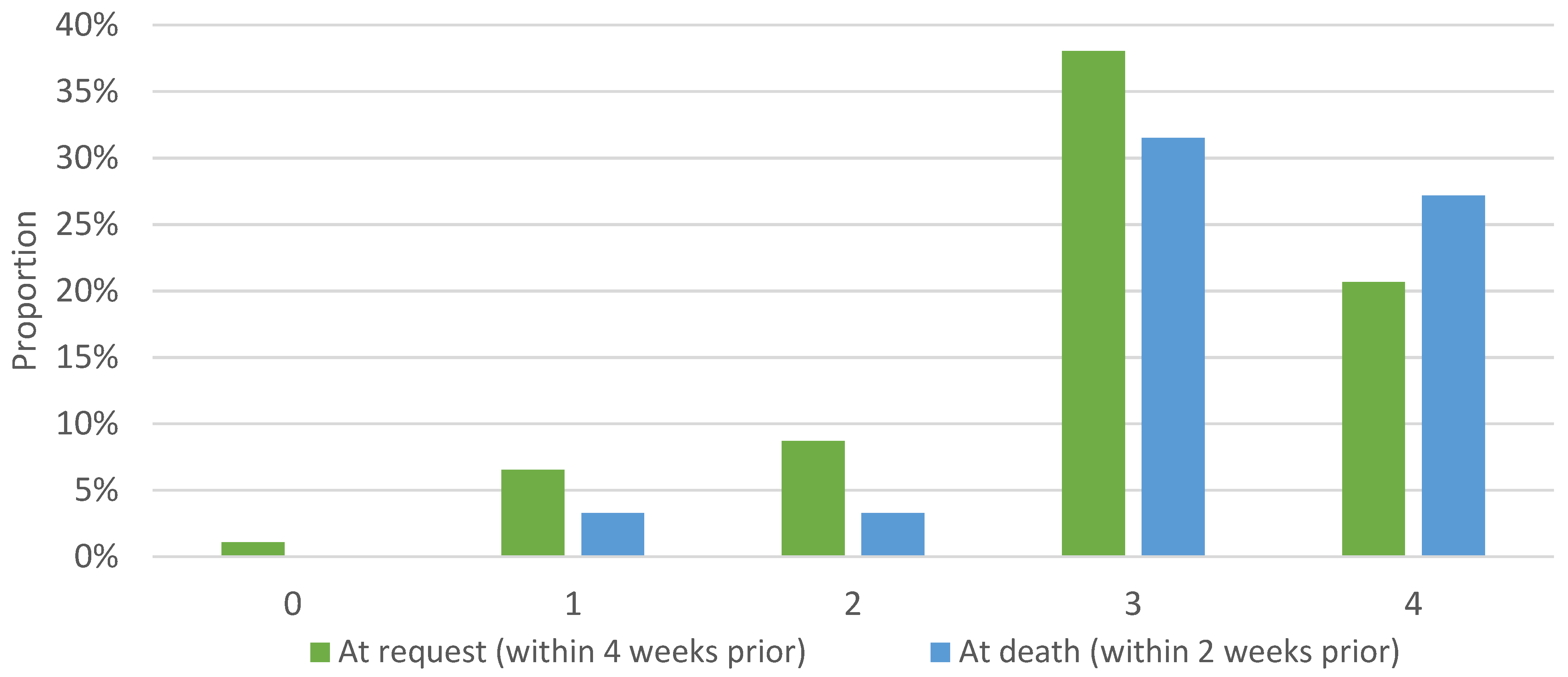
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ball, I.M.; Hodge, B.; Jansen, S.; Nickle, S.; Sibbald, R.W. A Canadian Academic Hospital’s Initial MAID Experience: A Health-Care Systems Review. J. Palliat. Care 2019, 34, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada. Canada’s New Medical Assistance in Dying (MAID) Law. 2021. Available online: https://www.justice.gc.ca/eng/cj-jp/ad-am/bk-di.html (accessed on 28 December 2021).
- Emanuel, E.J.; Onwuteaka-Philipsen, B.D.; Urwin, J.W.; Cohen, J. Attitudes and Practices of Euthanasia and Physician-Assisted Suicide in the United States, Canada, and Europe. JAMA 2016, 316, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Health Canada Second Annual Report on Medical Assistance in Dying in Canada 2020. 2021. Available online: https://www.canada.ca/en/health-canada/services/medical-assistance-dying/annual-report-2020.html (accessed on 14 November 2021).
- Ruijs, C.D.M.; Kerkhof, A.J.F.M.; van der Wal, G.; Onwuteaka-philipsen, B.D. Depression and explicit requests for euthanasia in end-of-life cancer patients in primary care in the netherlands: A longitudinal, prospective study. Fam. Pract. 2011, 28, 393–399. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Van Der Lee, M.L.; Van Der Bom, J.G.; Swarte, N.B.; Heintz, A.P.M.; De Graeff, A.; Van Den Bout, J. Euthanasia and depression: A prospective cohort study among terminally ill cancer patients. J. Clin. Oncol. 2005, 23, 6607–6612. [Google Scholar] [CrossRef] [PubMed]
- Ruijs, C.D.M.; Van Der Wal, G.; Kerkhof, A.J.F.M.; Onwuteaka-Philipsen, B.D. Unbearable suffering and requests for euthanasia prospectively studied in end-of-life cancer patients in primary care. BMC Palliat. Care 2014, 13, 62. [Google Scholar] [CrossRef] [PubMed]
- Georges, J.J.; Onwuteaka-Philipsen, B.D.; van der Wal, G.; van der Heide, A.; van der Maas, P.J. Differences between terminally ill cancer patients who died after euthanasia had been performed and terminally ill cancer patients who did not request euthanasia. Palliat. Med. 2005, 19, 578–586. [Google Scholar] [CrossRef]
- Verkissen, M.N.; Houttekier, D.; Cohen, J.; Schots, R.; Chambaere, K.; Deliens, L. End-of-life decision-making across cancer types: Results from a nationwide retrospective survey among treating physicians. Br. J. Cancer 2018, 118, 1369–1376. [Google Scholar] [CrossRef]
- Pardon, K.; Deschepper, R.; Vander Stichele, R.; Bernheim, J.L.; Mortier, F.; Schallier, D.; Germonpré, P.; Galdermanse, D.; Van Kerckhoven, W.; Deliens, L. Expressed wishes and incidence of euthanasia in advanced lung cancer patients. Eur. Respir. J. 2012, 40, 949–956. [Google Scholar] [CrossRef]
- Evenblij, K.; Pasman, H.R.W.; Van Der Heide, A.; Hoekstra, T.; Onwuteaka-Philipsen, B.D. Factors associated with requesting and receiving euthanasia: A nationwide mortality follow-back study with a focus on patients with psychiatric disorders, dementia, or an accumulation of health problems related to old age. BMC Med. 2019, 17, 1–12. [Google Scholar] [CrossRef]
- Pardon, K.; Chambaere, K.; Pasman, H.R.W.; Deschepper, R.; Rietjens, J.; Deliens, L. Trends in End-of-Life Decision Making in Patients With and Without Cancer. J. Clin. Oncol. 2013, 31, 1450–1457. [Google Scholar] [CrossRef]
- Ganzini, L.; Beer, T.M.; Brouns, M.; Mori, M.; Hsieh, Y.-C. Interest in physician-assisted suicide among Oregon cancer patients. J. Clin. Ethics 2006, 17, 27–38. [Google Scholar]
- Breitbart, W.; Rosenfeld, B.; Pessin, H.; Kaim, M.; Funesti-Esch, J.; Galietta, M.; Nelson, C.J.; Brescia, R. Depression, Hopelessness, and Desire for Hastened Death in Terminally Ill Patients with Cancer. JAMA 2000, 284, 2907–2911. [Google Scholar] [CrossRef] [PubMed]
- Zubrod, C.G.; Schneiderman, M.; Frei, E.; Brindley, C.; Lennard Gold, G.; Shnider, B.; Oviedo, R.; Gorman, J.; Jones, R.; Jonsson, U.; et al. Appraisal of methods for the study of chemotherapy of cancer in man: Comparative therapeutic trial of nitrogen mustard and triethylene thiophosphoramide. J. Chronic Dis. 1960, 11, 7–33. [Google Scholar] [CrossRef]
- Ohnsorge, K.; Gudat, H.; Rehmann-Sutter, C. What a wish to die can mean: Reasons, meanings and functions of wishes to die, reported from 30 qualitative case studies of terminally ill cancer patients in palliative care. BMC Palliat. Care 2014, 13, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Pesut, B.; Thorne, S.; Wright, D.K.; Schiller, C.; Huggins, M.; Puurveen, G.; Chambaere, K. Navigating medical assistance in dying from Bill C-14 to Bill C-7: A qualitative study. BMC Health Serv. Res. 2021, 21, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, L.E.; Craigs, C.L.; West, R.M.; Carder, P.; Hurlow, A.; Millares-Martin, P.; Hall, G.; Bennett, M.I. Is palliative care support associated with better quality end-of-life care indicators for patients with advanced cancer? A retrospective cohort study. BMJ Open 2018, 8, e018284. [Google Scholar] [CrossRef]
- Ferrell, B.R.; Temel, J.S.; Temin, S.; Alesi, E.R.; Balboni, T.A.; Basch, E.M.; Firn, J.I.; Paice, J.A.; Peppercorn, J.M.; Phillips, T.; et al. Integration of Palliative Care into Standard Oncology Care: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2017, 35, 96–112. [Google Scholar] [CrossRef]
- Sizoo, E.M.; Pasman, H.R.W.; Buttolo, J.; Heimans, J.J.; Klein, M.; Deliens, L.; Reijneveld, J.C.; Taphoorn, M.J.B. Decision-making in the end-of-life phase of high-grade glioma patients. Eur. J. Cancer 2012, 48, 226–232. [Google Scholar] [CrossRef]
- Temel, J.S.; Greer, J.A.; Muzikansky, A.; Gallagher, E.R.; Admane, S.; Jackson, V.A.; Dahlin, C.M.; Blinderman, C.D.; Jacobsen, J.; Pirl, W.F.; et al. Early Palliative Care for Patients with Metastatic Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2010, 363, 733–742. [Google Scholar] [CrossRef] [PubMed]
- Parajuli, J.; Tark, A.; Jao, Y.L.; Hupcey, J. Barriers to palliative and hospice care utilization in older adults with cancer: A systematic review. J. Geriatr. Oncol. 2020, 11, 8–16. [Google Scholar] [CrossRef]
- Conlon, M.S.; Caswell, J.M.; Santi, S.A.; Ballantyne, B.; Meigs, M.L.; Knight, A.; Earle, C.C.; Hartman, M. Access to Palliative Care for Cancer Patients Living in a Northern and Rural Environment in Ontario, Canada: The Effects of Geographic Region and Rurality on End-of-Life Care in a Population-Based Decedent Cancer Cohort. Clin. Med. Insights Oncol. 2019, 13, 1179554919829500. [Google Scholar] [CrossRef] [PubMed]
- Earp, M.A.; Sinnarajah, A.; Kerba, M.; Tang, P.A.; Rodriguez-Arguello, J.; King, S.; Watanabe, S.M.; Simon, J.E. Opportunity is the greatest barrier to providing palliative care to advanced colorectal cancer patients: A survey of oncology clinicians. Curr. Oncol. 2018, 25, e480. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.E.; Girgis, A.; Paul, C.L.; Currow, D.C. Palliative care referral practices and perceptions: The divide between metropolitan and non-metropolitan general practitioners. Palliat. Support. Care 2011, 9, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Kayastha, N.; LeBlanc, T.W. When to Integrate Palliative Care in the Trajectory of Cancer Care. Curr. Treat. Options Oncol. 2020, 21, 41. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, S.M.; Fairchild, A.; Pituskin, E.; Borgersen, P.; Hanson, J.; Fassbender, K. Improving access to specialist multidisciplinary palliative care consultation for rural cancer patients by videoconferencing: Report of a pilot project. Support. Care Cancer 2013, 21, 1201–1207. [Google Scholar] [CrossRef]
- Read Paul, L.; Salmon, C.; Sinnarajah, A.; Spice, R. Web-based videoconferencing for rural palliative care consultation with elderly patients at home. Support. Care Cancer 2019, 27, 3321–3330. [Google Scholar] [CrossRef]
- Garfan, S.; Alamoodi, A.H.; Zaidan, B.B.; Al-Zobbi, M.; Hamid, R.A.; Alwan, J.K.; Ahmaro, I.Y.Y.; Khalid, E.T.; Jumaah, F.M.; Albahri, O.S.; et al. Telehealth utilization during the Covid-19 pandemic: A systematic review. Comput. Biol. Med. 2021, 138, 104878. [Google Scholar] [CrossRef]
- Physician Billing Codes in Response to COVID-19|CIHI. Available online: https://www.cihi.ca/en/physician-billing-codes-in-response-to-covid-19 (accessed on 22 February 2022).
- Li, M.; Shapiro, G.K.; Klein, R.; Barbeau, A.; Rydall, A.; Bell, J.A.H.; Nissim, R.; Hales, S.; Zimmermann, C.; Wong, R.K.S.; et al. Medical Assistance in Dying in patients with advanced cancer and their caregivers: A mixed methods longitudinal study protocol. BMC Palliat. Care 2021, 20, 1–13. [Google Scholar] [CrossRef]
- LoPresti, M.A.; Dement, F.; Gold, H.T. End-of-Life Care for People with Cancer from Ethnic Minority Groups: A Systematic Review. Am. J. Hosp. Palliat. Med. 2016, 33, 291–305. [Google Scholar] [CrossRef]
| Personal Data | Frequency | Proportions |
|---|---|---|
| Age | (n = 92) | |
| <39 | 1 | 1% |
| 40–49 | 4 | 4% |
| 50–59 | 4 | 4% |
| 60–69 | 27 | 29% |
| 70–79 | 31 | 34% |
| 80–89 | 21 | 23% |
| >90 | 4 | 4% |
| Sex | (n = 92) | |
| Female | 50 | 54% |
| Male | 42 | 46% |
| Residence | (n = 92) | |
| Partner | 43 | 47% |
| Alone | 37 | 40% |
| Children | 8 | 9% |
| Parents | 2 | 2% |
| Other | 2 | 2% |
| Distressing Symptoms Reported | Incidence | Proportion |
|---|---|---|
| pain | 56 | 61% |
| fatigue | 35 | 38% |
| dyspnea | 25 | 27% |
| weakness | 23 | 25% |
| nausea | 19 | 21% |
| lack of appetite | 19 | 21% |
| declining functional status | 15 | 16% |
| dysphagia | 9 | 10% |
| incontinence | 5 | 5% |
| confusion | 5 | 5% |
| depression | 5 | 5% |
| other | 27 | 29% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, T.; Liu, W.; Leung, A.; Jia, S.; Lee, P.; Liu, L.; Mutsaers, A.; Miller, S.; Honarmand, K.; Malik, S.; et al. Medical Assistance in Dying in Oncology Patients: A Canadian Academic Hospital’s Experience. Curr. Oncol. 2022, 29, 9407-9415. https://doi.org/10.3390/curroncol29120739
Liu T, Liu W, Leung A, Jia S, Lee P, Liu L, Mutsaers A, Miller S, Honarmand K, Malik S, et al. Medical Assistance in Dying in Oncology Patients: A Canadian Academic Hospital’s Experience. Current Oncology. 2022; 29(12):9407-9415. https://doi.org/10.3390/curroncol29120739
Chicago/Turabian StyleLiu, Tony, Wei Liu, Aaron Leung, Sangyang Jia, Patsy Lee, Luke Liu, Adam Mutsaers, Sue Miller, Kimia Honarmand, Shiraz Malik, and et al. 2022. "Medical Assistance in Dying in Oncology Patients: A Canadian Academic Hospital’s Experience" Current Oncology 29, no. 12: 9407-9415. https://doi.org/10.3390/curroncol29120739
APA StyleLiu, T., Liu, W., Leung, A., Jia, S., Lee, P., Liu, L., Mutsaers, A., Miller, S., Honarmand, K., Malik, S., Qu, M., & Ball, I. (2022). Medical Assistance in Dying in Oncology Patients: A Canadian Academic Hospital’s Experience. Current Oncology, 29(12), 9407-9415. https://doi.org/10.3390/curroncol29120739





