Patterns of Extrathoracic Metastasis in Lung Cancer Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Statistical Analysis
3. Results
3.1. Patient Characteristics
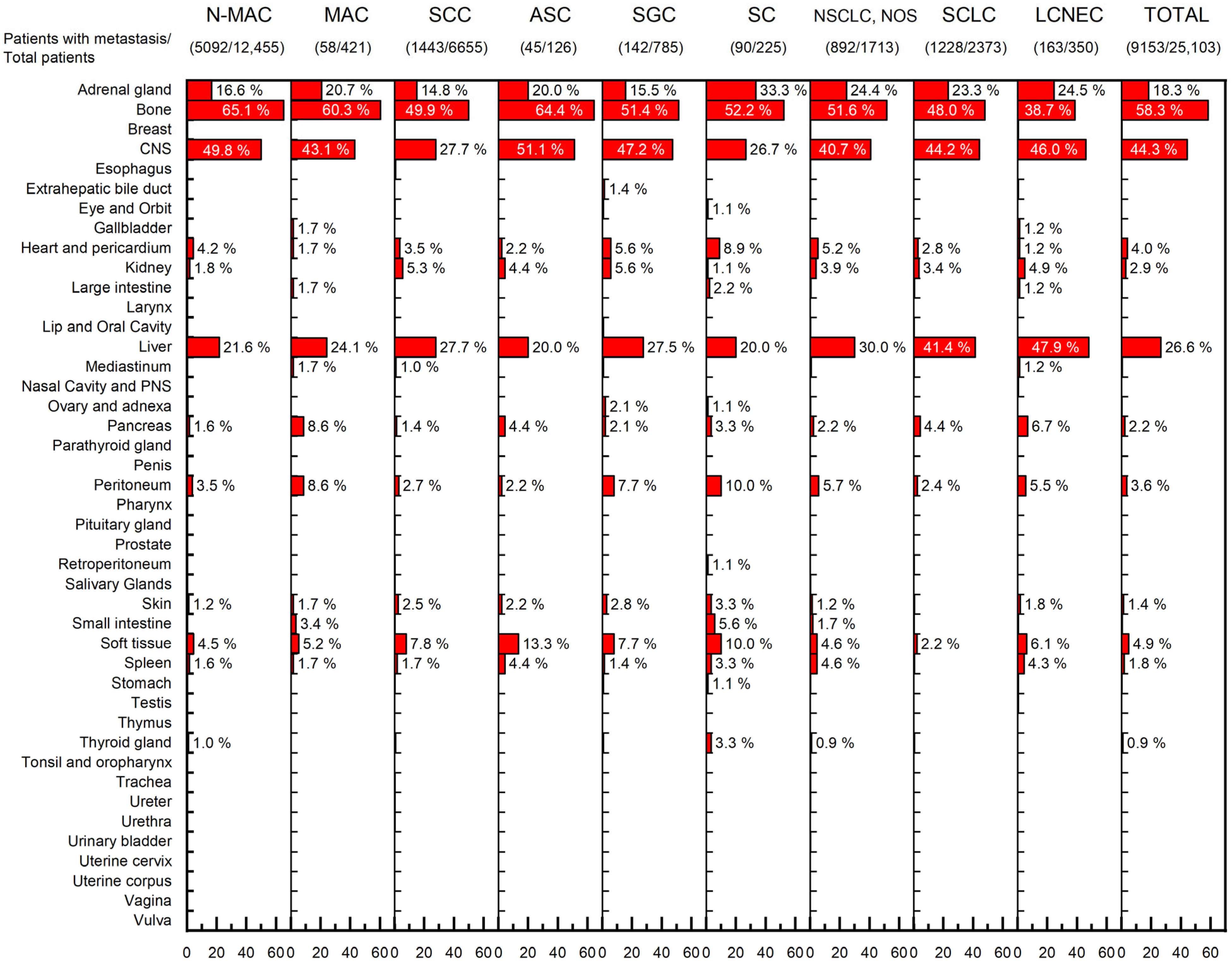
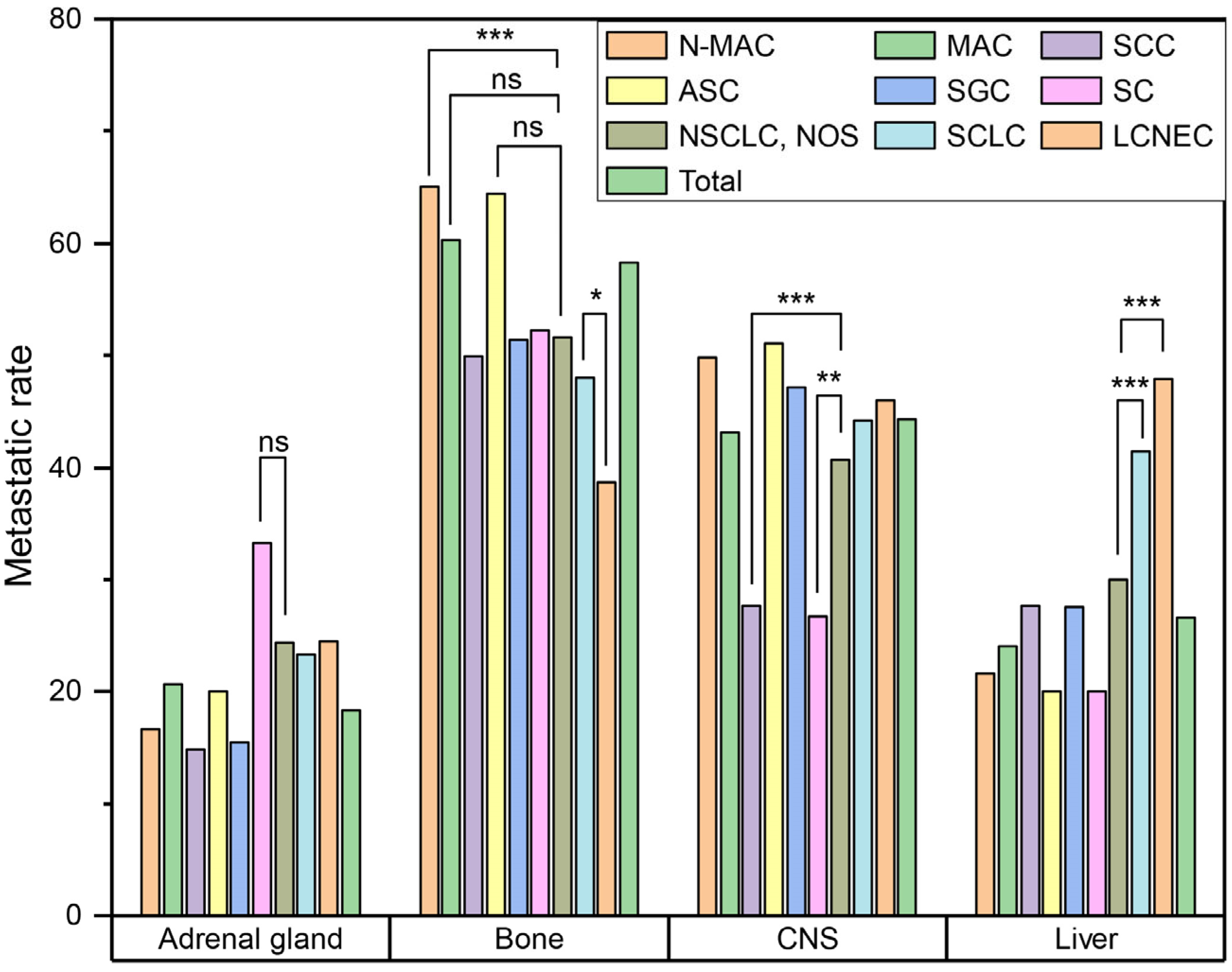
3.2. Metastatic Patterns
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nichols, L.; Saunders, R.; Knollmann, F.D. Causes of Death of Patients with Lung Cancer. Arch. Pathol. Lab. Med. 2012, 136, 1552–1557. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.G.; Kim, H.C.; Choi, C.-M. Recent Trends of Lung Cancer in Korea. Tuberc. Respir. Dis. 2021, 84, 89–95. [Google Scholar] [CrossRef]
- Stein, J.N.; Rivera, M.P.; Weiner, A.; Duma, N.; Henderson, L.; Mody, G.; Charlot, M. Sociodemographic Disparities in the Management of Advanced Lung Cancer: A Narrative Review. J. Thorac. Dis. 2021, 13, 3772–3800. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- van Zijl, F.; Krupitza, G.; Mikulits, W. Initial Steps of Metastasis: Cell Invasion and Endothelial Transmigration. Mutat. Res. 2011, 728, 23. [Google Scholar] [CrossRef]
- Paget, S. The Distribution of Secondary Growths in Cancer of the Breast. Lancet 1889, 133, 571–573. [Google Scholar] [CrossRef]
- Ewing, J. Neoplastic Diseases: A Treatise on Tumours, 3rd ed.; W.B. Saunders Co.: Philadelphia, PA, USA; London, UK, 1928. [Google Scholar]
- Fidler, I.J.; Kripke, M.L. Metastasis Results from Preexisting Variant Cells within a Malignant Tumor. Science 1977, 197, 893–895. [Google Scholar] [CrossRef]
- Weiss, L. Comments on Hematogenous Metastatic Patterns in Humans as Revealed by Autopsy. Clin. Exp. Metastasis 1992, 10, 191–199. [Google Scholar] [CrossRef]
- WHO Classification of Tumours Editorial Board. WHO Classification of Tumours: Thoracic Tumours, 5th ed.; International Agency for Research on Cancer: Lyon, France, 2021. [Google Scholar]
- Riihimäki, M.; Hemminki, A.; Fallah, M.; Thomsen, H.; Sundquist, K.; Sundquist, J.; Hemminki, K. Metastatic Sites and Survival in Lung Cancer. Lung Cancer 2014, 86, 78–84. [Google Scholar] [CrossRef]
- Milovanovic, I.; Stjepanovic, M.; Mitrovic, D. Distribution Patterns of the Metastases of the Lung Carcinoma in Relation to Histological Type of the Primary Tumor: An Autopsy Study. Ann. Thorac. Med. 2017, 12, 191. [Google Scholar] [CrossRef]
- Wang, X.; Wang, Z.; Pan, J.; Lu, Z.Y.; Xu, D.; Zhang, H.J.; Wang, S.H.; Huang, D.Y.; Chen, X.F. Patterns of Extrathoracic Metastases in Different Histological Types of Lung Cancer. Front. Oncol. 2020, 10, 715. [Google Scholar] [CrossRef] [PubMed]
- Quint, L.E.; Tummala, S.; Brisson, L.J.; Francis, I.R.; Krupnick, A.S.; Kazerooni, E.A.; Iannettoni, M.D.; Whyte, R.I.; Orringer, M.B. Distribution of Distant Metastases from Newly Diagnosed Non-Small Cell Lung Cancer. Ann. Thorac. Surg. 1996, 62, 246–250. [Google Scholar] [CrossRef]
- Tamura, T.; Kurishima, K.; Nakazawa, K.; Kagohashi, K.; Ishikawa, H.; Satoh, H.; Hizawa, N. Specific Organ Metastases and Survival in Metastatic Non-Small-Cell Lung Cancer. Mol. Clin. Oncol. 2015, 3, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Xie, S.; Wu, Z.; Qi, Y.; Wu, B.; Zhu, X. The Metastasizing Mechanisms of Lung Cancer: Recent Advances and Therapeutic Challenges. Biomed. Pharmacother. 2021, 138, 111450. [Google Scholar] [CrossRef]
- da Silva, G.T.; Bergmann, A.; Thuler, L.C.S. Incidence and Risk Factors for Bone Metastasis in Non-Small Cell Lung Cancer. Asian Pac. J. Cancer Prev. 2019, 20, 45–51. [Google Scholar] [CrossRef]
- Oliveira, M.B.D.R.; Souza, L.C.; Sampayo, E.J.G.; de Carvalho, G.S.; Mello, F.C.D.Q.; Paschoal, M.E.M. The Impact of Lung Carcinoma Histology on the Frequency of Bone Metastases. Rev. Bras. Ortop. 2019, 54, 524–530. [Google Scholar] [CrossRef]
- Tane, S.; Nishio, W.; Ogawa, H.; Hokka, D.; Tane, K.; Tanaka, Y.; Tauchi, S.; Uchino, K.; Sakai, Y.; Ohbayashi, C.; et al. Clinical Significance of the “not Otherwise Specified” Subtype in Candidates for Resectable Non-Small Cell Lung Cancer. Oncol. Lett. 2014, 8, 1017–1024. [Google Scholar] [CrossRef]
- Ignatius Ou, S.H.; Zell, J.A. Carcinoma NOS Is a Common Histologic Diagnosis and Is Increasing in Proportion among Non-Small Cell Lung Cancer Histologies. J. Thorac. Oncol. 2009, 4, 1202–1211. [Google Scholar] [CrossRef]
- Falk, N.; Weissferdt, A.; Kalhor, N.; Moran, C.A. Primary Pulmonary Salivary Gland-Type Tumors: A Review and Update. Adv. Anat. Pathol. 2016, 23, 13–23. [Google Scholar] [CrossRef]
- Cha, Y.J.; Shim, H.S. Biology of Invasive Mucinous Adenocarcinoma of the Lung. Transl. Lung Cancer Res. 2017, 6, 508–512. [Google Scholar] [CrossRef]
- Waqar, S.N.; Samson, P.P.; Robinson, C.G.; Bradley, J.; Devarakonda, S.; Du, L.; Govindan, R.; Gao, F.; Puri, V.; Morgensztern, D. Non–Small-Cell Lung Cancer With Brain Metastasis at Presentation. Clin. Lung Cancer 2018, 19, e373–e379. [Google Scholar] [CrossRef] [PubMed]
- Kagohashi, K.; Satoh, H.; Ishikawa, H.; Ohtsuka, M.; Sekizawa, K. Liver Metastasis at the Time of Initial Diagnosis of Lung Cancer. Med. Oncol. 2003, 20, 25–28. [Google Scholar] [CrossRef]
- Hoshino, A.; Costa-Silva, B.; Shen, T.-L.; Rodrigues, G.; Hashimoto, A.; Tesic Mark, M.; Molina, H.; Kohsaka, S.; di Giannatale, A.; Ceder, S.; et al. Tumour Exosome Integrins Determine Organotropic Metastasis. Nature 2015, 527, 329–335. [Google Scholar] [CrossRef] [PubMed]
| ADC | SCC | ASC | SGC | SC | NSCLC, NOS | SCLC | LCNEC | Total | ||
|---|---|---|---|---|---|---|---|---|---|---|
| N-MAC | MAC | |||||||||
| Total, n (%) | 12,455 (49.6) | 421 (1.7) | 6655 (26.5) | 126 (0.5) | 785 (3.1) | 225 (0.9) | 1713 (6.8) | 2373 (9.5) | 350 (1.4) | 25,103 (100) |
| Age, median (IQR) | 61 (53–69) | 62 (54–70) | 66 (60–72) | 62 (55–68) | 59 (50–67) | 64 (54–70) | 65 (56–71) | 65 (58–70) | 65 (60–71) | 63 (56–70) |
| Sex, n (%) | ||||||||||
| Male | 6849 (55.0) | 196 (46.6) | 6162 (92.6) | 92 (73.0) | 399 (50.8) | 177 (78.7) | 1344 (78.5) | 2059 (86.8) | 310 (88.6) | 17,594 (70.1) |
| Female | 5606 (45.0) | 225 (53.4) | 493 (7.4) | 34 (27.0) | 386 (49.2) | 48 (21.3) | 369 (21.5) | 314 (13.2) | 40 (11.4) | 7515 (29.9) |
| Metastasis, n (%) | ||||||||||
| Absent | 7363 (59.1) | 363 (86.2) | 5212 (78.3) | 81 (64.3) | 643 (81.9) | 135 (60.0) | 821 (47.9) | 1145 (48.3) | 187 (53.4) | 15,950 (63.5) |
| Present | 5092 (40.9) | 58 (13.8) | 1443 (21.7) | 45 (35.7) | 142 (18.1) | 90 (40.0) | 892 (52.1) | 1228 (51.7) | 163 (46.6) | 9153 (36.5) |
| Number of organs with metastasis, n (%) | ||||||||||
| 1–3 | 4786 (94.0) | 56 (96.6) | 1384 (95.9) | 40 (88.9) | 127 (89.4) | 81 (90.0) | 824 (92.4) | 1163 (94.7) | 146 (89.6) | 8607 (94.0) |
| 4–6 | 301 (5.9) | 2 (3.4) | 59 (4.1) | 4 (8.9) | 13 (9.2) | 8 (8.9) | 64 (7.2) | 64 (5.2) | 17 (10.4) | 532 (5.8) |
| 7+ | 5 (0.1) | 0 (0) | 0 (0) | 1 (2.2) | 2 (1.4) | 1 (1.1) | 4 (0.4) | 1 (0.1) | 0 (0) | 14 (0.2) |
| History of another malignancy | ||||||||||
| No | 11,279 (90.6) | 347 (82.4) | 5936 (89.2) | 117 (92.9) | 662 (84.3) | 198 (88.0) | 1635 (95.4) | 2251 (94.9) | 308 (88.0) | 22,733 (90.6) |
| Yes | 1176 (9.4) | 74 (17.6) | 719 (10.8) | 9 (7.1) | 123 (15.7) | 27 (12.0) | 78 (4.6) | 122 (5.1) | 42 (12.0) | 2370 (9.4) |
| Age in Years, Median (IQR) | Sex, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Absent | Present | p | Absent | Present | p | ||||
| Male | Female | Male | Female | ||||||
| ADC | N-MAC | 62 (54–69) | 60 (52–67) | <0.001 | 3995 (54.3) | 3368 (45.7) | 2854 (56.0) | 2238 (44.0) | 0.048 |
| MAC | 63 (55–70) | 60.5 (53–67) | 0.174 | 163 (44.9) | 200 (55.1) | 33 (56.9) | 25 (43.1) | 0.089 | |
| SCC | 66 (60–72) | 65 (58–70) | <0.001 | 4883 (93.7) | 329 (6.3) | 1279 (88.6) | 164 (11.4) | <0.001 | |
| ASC | 64 (57–70) | 58 (52–66) | 0.029 | 63 (77.8) | 18 (22.2) | 29 (64.4) | 16 (35.6) | 0.106 | |
| SGC | 59 (50–66) | 59 (51–67) | 0.908 | 319 (49.6) | 324 (50.4) | 80 (56.3) | 62 (43.7) | 0.147 | |
| SC | 65 (58–72) | 61 (51–69) | 0.001 | 111 (82.2) | 24 (17.8) | 66 (73.3) | 24 (26.7) | 0.111 | |
| NSCLC, NOS | 66 (59–72) | 63 (55–70) | <0.001 | 674 (82.1) | 147 (17.9) | 670 (75.1) | 222 (24.9) | <0.001 | |
| SCLC | 65 (59–71) | 64 (58–70) | 0.036 | 976 (85.2) | 169 (14.8) | 1083 (88.2) | 145 (11.8) | 0.034 | |
| LCNEC | 66 (61–71) | 65 (60–71) | 0.592 | 166 (88.8) | 21 (11.2) | 144 (88.3) | 19 (11.7) | 0.900 | |
| Total | 64 (57–71) | 62 (54–69) | <0.001 | 11,350 (71.2) | 4600 (28.8) | 6238 (68.2) | 2915 (31.8) | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, H.K.; Han, J.; Kwon, G.Y.; Yeo, M.-K.; Bae, G.E. Patterns of Extrathoracic Metastasis in Lung Cancer Patients. Curr. Oncol. 2022, 29, 8794-8801. https://doi.org/10.3390/curroncol29110691
Park HK, Han J, Kwon GY, Yeo M-K, Bae GE. Patterns of Extrathoracic Metastasis in Lung Cancer Patients. Current Oncology. 2022; 29(11):8794-8801. https://doi.org/10.3390/curroncol29110691
Chicago/Turabian StylePark, Hyung Kyu, Joungho Han, Ghee Young Kwon, Min-Kyung Yeo, and Go Eun Bae. 2022. "Patterns of Extrathoracic Metastasis in Lung Cancer Patients" Current Oncology 29, no. 11: 8794-8801. https://doi.org/10.3390/curroncol29110691
APA StylePark, H. K., Han, J., Kwon, G. Y., Yeo, M.-K., & Bae, G. E. (2022). Patterns of Extrathoracic Metastasis in Lung Cancer Patients. Current Oncology, 29(11), 8794-8801. https://doi.org/10.3390/curroncol29110691






