#COVID19 and #Breastcancer: A Qualitative Analysis of Tweets
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Data Collection
2.3. Data Analysis
2.4. Ethics Approval
3. Results
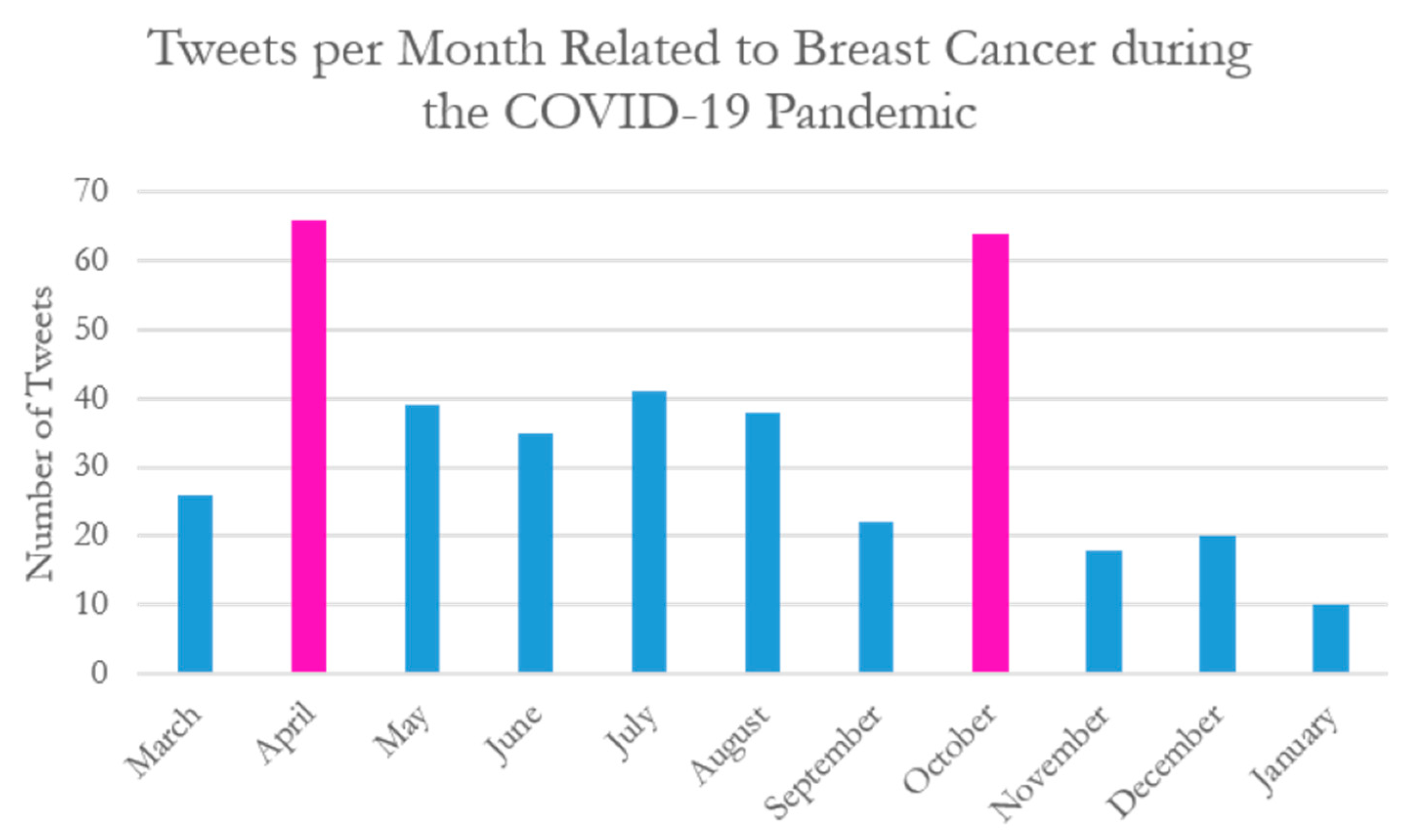
Demographics
- Patient safety—fears of COVID-19 infection
“When Do I Get a Break?” and Other Thoughts: Learning About an Exposure to a New Pandemic https://unfilteredsnapshot.wordpress.com/2020/03/22/when-do-i-get-a-break-and-other-thoughts-learning-about-an-exposure-to-a-new-pandemic/… #COVID19 #BreastCancer #socialdistancing #quarantine.
“Is it safe to seek screening and treatment for #BreastCancer during the #pandemic? @DrElisaPort, Director of the Dubin Breast Center of @TischCancer, answers these common questions: https://fal.cn/3bgX1 #COVID19 #MountSinaiToday”.
“35% of Americans have missed routine cancer screenings bc of #COVID19, leading to a 46% decrease in diagnoses of certain cancers, including #breastcancer. Experts explain why it’s safe & necessary to schedule preventive healthcare even during a #pandemic https://bit.ly/3eiitnm”.
- 2.
- Patient safety—Concerns regarding screening/care delays
“I’ve got #BreastCancer. Will I get the care I need during a pandemic? by @AgainstCures https://healthydebate.ca/opinions/will-i-get-care-during-pandemic… via @healthydebate #COVID19 #cdnhealth #cancer”.
“Experts predict more than 10,000 excess cancer deaths during the next decade as a result of missed screenings during the #COVID19 pandemic. Register for #LifeBridgeHealth’s #Mammothon, an all-day #mammogram screening event. http://bit.ly/2zagGim #breastcancer”—US-based nonprofit healthcare organization.
“#UK #COVID19 and #Breastcancer #Charity says nearly 1m women missed breast #cancer check in #pandemic.
COVID-19 and #lockdown led to an estimated 986,000 Britons not having #mammograms #PublicHealth #Oncology #NHS #healthcare”—UK-based medical consultancy company.
“How have breast cancer patients been impacted by COVID-19 pandemic? Irish Cancer Society says 450 cancers, 1600 pre-cancers have gone undetected during lockdown #cancer #CancerAwareness #COVID19 #breastcancerfree #breastcancer #irishcancersociety”—Irish nonprofit health organization.
“Our new #research w @TamaraHaml. 44% #breastcancer #survivors experienced care #delays at the outset of #COVID19 #pandemic #bcsm @maryam_lustberg @DrAttai @UICAHS @UICancerCenter https://link.springer.com/article/10.1007/s10549-020-05828-7?wt_mc=Internal.Event.1.SEM.ArticleAuthorOnlineFirst…”—US-based health researcher.
“News in brief: The numbers of newly diagnosed cases of six types of cancer, including #BreastCancer & #LungCancer, fall during #COVID19 pandemic, report Harvey Kaufman & colleagues from @QuestDX in @JAMANetworkOpen #COVIDnCancer”—Global health information publishing organization.
“Six months into the #COVID19 pandemic, cancer researchers are beginning to evaluate the impact of treatment delays. @AmCollSurgeons find delays due to COVID-19 appear non-life-threatening for early-stage #BreastCancer.”—UK-based cancer research institute.
- 3.
- Limitations to social supports
“I am battling breast cancer right now. Yes, in the middle of a pandemic. I have to face everything alone, no family allowed in treatment centers. The least we can do is make sure my treatments can continue. #COVID19 #breastcancer”.
“My 29 y/o sister was diagnosed with breast cancer a few wks ago. Why now? Why so young? Why during a pandemic? We can’t be with her physically because her immune system is weak during chemo. Then surgery. Then radiation. #breastcancer #COVID19 #health #BreastCancerAwareness”.
“While the world is battling the #COVID19 pandemic, Jessica Roubitchek was grappling with the possibility her #breastcancer had returned & facing scans alone. Luckily a doctor was there to support when her family couldn’t”.
“Inspiration from our friends @ACS_Alabama. Read how our @AmericanCancer helpline supported Siusan Peek through her journey with Stage II triple negative #breastcancer at age 32, during the current #COVID19 global pandemic. https://facebook.com/notes/american-cancer-society-alabama/recent-cancer-survivor-finds-comfort-in-cancerorg-throughout-cancer-journey-and-/2874963839259139/…”.
- 4.
- Patient trust in health systems and providers
“I do feel, very much, that MD Anderson has my best interest at heart,” says Sally Filler. She shares her story of participating in a breast cancer clinical trial during the COVID-19 pandemic. #COVID19 #BreastCancer #EndCancer”.
“Emma Yeager discusses #BreastCancer treatment amid the #COVID19 pandemic, including her close relationship with her team at The James.”.
“#Cancer screening is done in Tamil Nadu Govt Hospitals despite #COVID19. 789,800 women screened for #BreastCancer and 565,940 screened for #CervicalCancer. Treating non-communicable diseases are not affected by the pandemic. Kudos to TN health! #CancerAwarenessDay @MoHFW_INDIA”.
- Patient and care person perspectives
“Plan for the parts you can plan for. Ask what your hospital/clinic is doing to protect YOU from contracting COVID-19. Remind yourself how resilient you are,’ suggests @NancysPoint. Have you had #breastcancer surgery during the #COVID19 pandemic? #bcsm”.
“Read Loris Kersey’s testimonial with #BreastCancer, who hopes her story will remind people not to skip out on doctor’s visits and #cancer screenings, even during the #Covid19 pandemic. #bcsm”.
“‘This pandemic is going to go away… if you have a #breastcancer diagnosis, it won’t. Go and get your mammogram.’—Suzy, patient advocate #covid19breastcancer”.
“#RT @pozmagazine: RT @covidhealthmag: Cancer Survivor Tig Notaro Turns Her Humor to the Coronavirus Pandemic https://covidhealth.com/article/cancer-survivor-tig-notaro-turns-humor-coronavirus-pandemic… #BreastCancer #COVID19”.
“Planning her wedding during a global pandemic while facing cancer has been Andrea’s reality in 2020. Just before the start of #COVID19, Andrea was diagnosed with #breastcancer. Read more about her journey here: https://bit.ly/3jwiPaN”.
“Loneliness, uncertainty, grief and some unexpected silver linings. Three Women Open Up About What It’s Like to Battle #BreastCancer in the Middle of the #COVID19 Pandemic: https://instyle.com/beauty/health-fitness/breast-cancer-pandemiceffects?utm_source=twitter.com&utm_medium=social&utm_campaign=social-share-article… @Breastcancerorg @ChefGeib @ASBrS @DrJDietz via @kaelynforde for @InStyle”.
“As the husband of a survivor who found out that her friend now has #breastcancer, it underscores the need to support those undergoing treatment during the #COVID19 pandemic. They need prayers and encouragement more than ever”.
“Having lost my aunt to #breastcancer which changed my life in so many ways, even during #COVID19 #pandemic, it is important to get #preventive #health taken care of—and that includes #mammograms/October is #BreastCancerAwareness month! @hcphtx”.
- 2.
- Expert Perspectives
“Starting radiation this month? Your worries may be impacted by the #COVID19 #pandemic, but you’re not alone. Join others in our #breastcancer community on the same treatment path. https://community.breastcancer.org/forum/70/topics/876251…”
“Facing a #breastcancer diagnosis can be overwhelming and terrifying. But during the #COVID19 pandemic, additional challenges arise such as having surgeries delayed or going through the treatment alone. Read more in our #TBCT joint statement.”—@EuropaDonnaEUR.
“We are keeping publishing regular updates on #COVID19 pandemic that can be of help for patients and oncology professionals on our website. It is important to #StayInformed and it is important to #shareknowledge! #bcsm #breastcancer https://abcglobalalliance.org/news-and-useful-resources/coronavirus-2019-and-cancer/…”—@ABCGlobalALL.
“#BreastCancer doesn’t stop! Even in the midst of a pandemic! Thank you @komensanantonio for putting together this fantastic list of community assistance and information resource for patients! #COVID19 #Coronavirus #FlattenTheCurve https://komensanantonio.org/covid-19/”—Private surgical practice.
“This year, #ASCO2020 was held as a virtual conference due to the #COVID19 pandemic. This is a summary of key trials presented at #ASCO, focusing primarily on #breastcancer, #livercancer, and #lungcancer. #nsclc #sclc #hcc #crc #ASCO20 #mesothelioma”.
“Grab this #opportunity to participate in #international #Conference as #webinar #BreastPathology2020 is now an online conference to overcome the issue of this #COVID19 #pandemic #Participate in this webinar by submitting your #articles #breastcancer #oncology”.
“The @ABSGBI has been providing excellent educational webinars across a range of topics for it’s members during the #COVID19 pandemic. If you’re a member don’t miss out, click the link to watch for free! https://buff.ly/2WOJm9Z @RCSnews #breastcancer #webinar #education #surgery”.
“1058 records. An incredible feat by @ABSGBI collaborators—500 new records entered in 5 days! Let’s keep up the momentum in the lead up to the planned first publication of #breastcancer management pathways during the #COVID19 pandemic”.
- Deviations from standard practices
“@SocSurgOnc releases disease site-specific guidelines for delaying #cancer surgeries during #COVID. See the letter from Dr. Bartlett and Dr. Howe here → t.co/CWT0UBEGek #surgonc #breastcancer #breastsurgery #surgery #oncology #bcsm #covid19 t.co/nVtBczEey”.
“Coming up shortly...an educational discussion on best practices in margin assessment & preparing for breast cancer surgeries in the era of COVID-19. Join Us! #breastcancer #breastsurgery #kubtec #mozartsystem #bcsm t.co/6y0s3aapBs t.co/E2N7hTLwKk”.
“Accelerated radiation therapy for #BreastCancer patients at Mayo Clinic help to minimize visits to the hospital and limit exposure to infection during the #COVID19 pandemic. https://mayocl.in/3knUAwG @MayoCancerCare”.
“@itnEditor Results of Journal of the American College of Surgeons study should reassure #breastcancer patients who experienced surgical postponements due to #COVID19 #pandemic”.
“Although delays in surgery may, at times, be inevitable during the pandemic, we feel that the evidence supports making efforts to ensure timely breast cancer surgery when possible. #breastcancer #covid19”.
“Guidelines for breast reconstruction during the COVID-19 pandemic: Are we considering enough evidence? Take a look at this article by Nishant Ganesh Kumar et al., published on ARBS Net: t.co/ra1FLBpDfb #covid19 #breastreconstruction #ASPS #breastsurgery”.
“Almost half of patients w/ #breastcancer experienced a change/delay in workup or treatment during the #COVID19 pandemic. There were significant #racialdisparities although on MVA only age, insurance, and stage were associated with delay. #ASCOQLTY20 #bcsm https://meetinglibrary.asco.org/record/192677/abstract…”.
“Dr Karen Smith and Dr Jean Wright from @sibleyonline discuss the transition to telemedicine visits and the guidelines they’ve co-authored on treating #breastcancer during the #COVID19 pandemic. https://bddy.me/2IH0kUu #breastcancerawarenessmonth”.
“#BreastCancer patients are being forced to wait out the pandemic storm before getting necessary treatments and procedures. Sydney Loney’s is one of those patients, due to #COVID19’s impact on the medical system, her mastectomy has been postponed. https://macleans.ca/opinion/i-have-breast-cancer-and-cant-be-treated-because-of-the-coronavirus/…”.
- 2.
- Pandemic specific research
“Have you received #breastcancer treatment during the #COVID19 pandemic? We would love to hear about your experience in order to learn how we might improve the quality and safety of care. More info below or DM/email @DarciTillbrook d.tillbrook1@leeds.ac.uk”
“MD’s from @TPMGDocCareers Breast Cancer Research Collaborative studied #breastcancer management in #COVID19 pandemic showing more advanced-stage and aggressive types, reductions in time to surgery and time to chemotherapy”.
“Dr. Sielsing presents Netherlands data which complements our #SABCS20 physician survey-hormonal tx use in stg1-3 #breastcancer due to #covid19 pandemic. @COVID19nCCC”.
4. Discussion
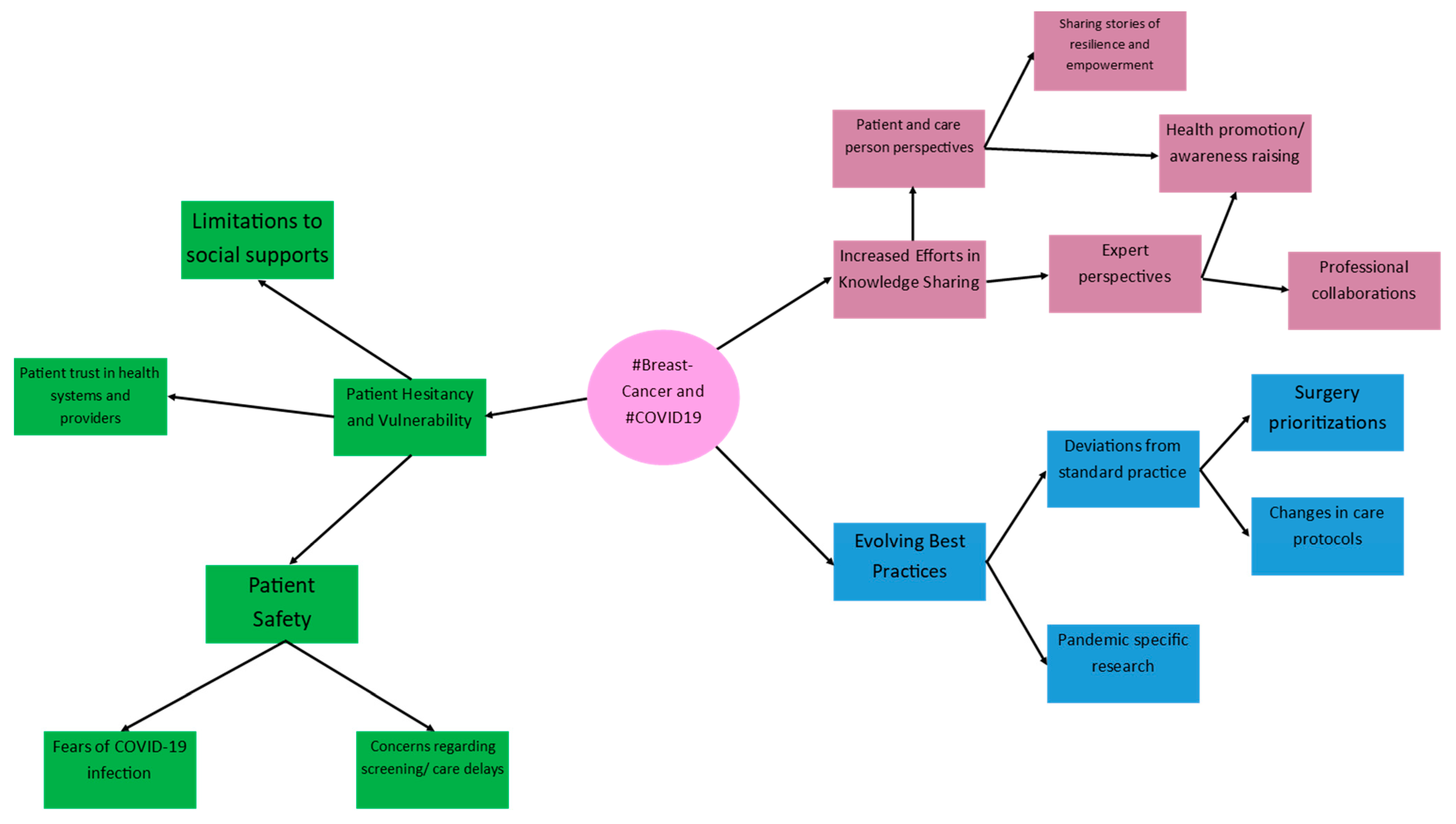
4.1. Patient Hesitancy and Vulnerability
4.2. Increased Efforts in Knowledge Sharing
4.3. Evolving Best Practices
4.4. Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 7 September 2022).
- Government of Canada. Canada’s COVID-19 Vaccine Supply and Donation Strategy. Available online: https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19/vaccines/supply-donation.html (accessed on 8 September 2022).
- Breast Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/breast-cancer (accessed on 7 September 2022).
- Alagoz, O.; Lowry, K.P.; Kurian, A.W.; Mandelblatt, J.S.; Ergun, M.A.; Huang, H.; Lee, S.J.; Schechter, C.B.; Tosteson, A.N.A.; Miglioretti, D.L.; et al. Impact of the COVID-19 Pandemic on Breast Cancer Mortality in the US: Estimates From Collaborative Simulation Modeling. JNCI J. Natl. Cancer Inst. 2021, 113, 1484–1494. [Google Scholar] [CrossRef] [PubMed]
- Dietz, J.R.; Moran, M.S.; Isakoff, S.J.; Kurtzman, S.H.; Willey, S.C.; Burstein, H.J.; Bleicher, R.J.; Lyons, J.A.; Sarantou, T.; Baron, P.L.; et al. Recommendations for Prioritization, Treatment, and Triage of Breast Cancer Patients during the COVID-19 Pandemic. the COVID-19 Pandemic Breast Cancer Consortium. Breast Cancer Res. Treat. 2020, 181, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Curigliano, G.; Cardoso, M.J.; Poortmans, P.; Gentilini, O.; Pravettoni, G.; Mazzocco, K.; Houssami, N.; Pagani, O.; Senkus, E.; Cardoso, F. Recommendations for Triage, Prioritization and Treatment of Breast Cancer Patients during the COVID-19 Pandemic. Breast Off. J. Eur. Soc. Mastology 2020, 52, 8–16. [Google Scholar] [CrossRef]
- Alshakhs, F.; Alanzi, T. The Evolving Role of Social Media in Health-Care Delivery: Measuring the Perception of Health-Care Professionals in Eastern Saudi Arabia. J. Multidiscip. Healthc. 2018, 11, 473–479. [Google Scholar] [CrossRef] [PubMed]
- Attai, D.J.; Cowher, M.S.; Al-Hamadani, M.; Schoger, J.M.; Staley, A.C.; Landercasper, J. Twitter Social Media Is an Effective Tool for Breast Cancer Patient Education and Support: Patient-Reported Outcomes by Survey. J. Med. Internet Res. 2015, 17, e188. [Google Scholar] [CrossRef]
- Pizzuti, A.G.; Patel, K.H.; McCreary, E.K.; Heil, E.; Bland, C.M.; Chinaeke, E.; Love, B.L.; Bookstaver, P.B. Healthcare Practitioners’ Views of Social Media as an Educational Resource. PLoS ONE 2020, 15, e0228372. [Google Scholar] [CrossRef]
- Senapati, A.; Khan, N.; Chebrolu, L.B. Impact of Social Media and Virtual Learning on Cardiology During the COVID-19 Pandemic Era and Beyond. Methodist DeBakey Cardiovasc. J. 2020, 16, 1. [Google Scholar] [CrossRef]
- Green, J.; Thorogood, N. Thematic Content Analysis. In Qualitative Methods for Health Research; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 2018; pp. 258–268. [Google Scholar]
- Oliveira J e Silva, L.; Maldonado, G.; Brigham, T.; Mullan, A.F.; Utengen, A.; Cabrera, D. Evaluating Scholars’ Impact and Influence: Cross-Sectional Study of the Correlation Between a Novel Social Media–Based Score and an Author-Level Citation Metric. J. Med. Internet Res. 2021, 23, e28859. [Google Scholar] [CrossRef]
- Batalden, M.; Batalden, P.; Margolis, P.; Seid, M.; Armstrong, G.; Opipari-Arrigan, L.; Hartung, H. Coproduction of Healthcare Service. BMJ Qual. Saf. 2016, 25, 509–517. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Papautsky, E.L.; Hamlish, T. Patient-Reported Treatment Delays in Breast Cancer Care during the COVID-19 Pandemic. Breast Cancer Res. Treat. 2020, 184, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, H.W.; Chen, Z.; Niles, J.; Fesko, Y. Changes in the Number of US Patients With Newly Identified Cancer Before and During the Coronavirus Disease 2019 (COVID-19) Pandemic. JAMA Netw. Open 2020, 3, e2017267. [Google Scholar] [CrossRef] [PubMed]
- Mehmet, M.; Roberts, R.; Nayeem, T. Using Digital and Social Media for Health Promotion: A Social Marketing Approach for Addressing Co-morbid Physical and Mental Health. Aust. J. Rural Health 2020, 28, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Neiger, B.L.; Thackeray, R.; Van Wagenen, S.A.; Hanson, C.L.; West, J.H.; Barnes, M.D.; Fagen, M.C. Use of Social Media in Health Promotion: Purposes, Key Performance Indicators, and Evaluation Metrics. Health Promot. Pract. 2012, 13, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Ali, K.F. Public Health Education through the Lens of Social Media: Implications in the COVID-19 Era. Sultan Qaboos Univ. Med. J. SQUMJ 2021, 21, e143–e145. [Google Scholar] [CrossRef] [PubMed]
- Armitage, L.; Lawson, B.K.; Whelan, M.E.; Newhouse, N. Paying SPECIAL Consideration to the Digital Sharing of Information during the COVID-19 Pandemic and Beyond. BJGP Open 2020, 4, bjgpopen20X101072. [Google Scholar] [CrossRef]
- Internet Use and COVID-19: How the Pandemic Increased the Amount of Time Canadians Spend Online. Available online: https://www150.statcan.gc.ca/n1/pub/45-28-0001/2021001/article/00027-eng.htm (accessed on 7 September 2022).
- Nakhasi, A.; Bell, S.G.; Passarella, R.J.; Paul, M.J.; Dredze, M.; Pronovost, P.J. The Potential of Twitter as a Data Source for Patient Safety. J. Patient Saf. 2019, 15, e32–e35. [Google Scholar] [CrossRef]
- Shimkhada, R.; Attai, D.; Scheitler, A.; Babey, S.; Glenn, B.; Ponce, N. Using a Twitter Chat to Rapidly Identify Barriers and Policy Solutions for Metastatic Breast Cancer Care: Qualitative Study. JMIR Public Health Surveill. 2021, 7, e23178. [Google Scholar] [CrossRef]
- Fernández, R.S.; Crivelli, L.; Guimet, N.M.; Allegri, R.F.; Pedreira, M.E. Psychological Distress Associated with COVID-19 Quarantine: Latent Profile Analysis, Outcome Prediction and Mediation Analysis. J. Affect. Disord. 2020, 277, 75–84. [Google Scholar] [CrossRef]
- Hawryluck, L.; Gold, W.L.; Robinson, S.; Pogorski, S.; Galea, S.; Styra, R. SARS Control and Psychological Effects of Quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004, 10, 1206–1212. [Google Scholar] [CrossRef]
- Smailhodzic, E.; Boonstra, A.; Langley, D.J. Social Media Enabled Interactions in Healthcare: Towards a Taxonomy. Soc. Sci. Med. 2021, 291, 114469. [Google Scholar] [CrossRef] [PubMed]
- The American Society of Breast Surgeons Official Proceedings, Volume XXIII 2022 Annual Meeting Scientific Session Abstracts. Ann. Surg. Oncol. 2022, 29 (Suppl. 1), 1–330. [CrossRef]
- Hunter-Smith, A.; Cuthbert, C.A.; Fergus, K.; Barbera, L.C.; Efegoma, Y.; Howell, D.; Isherwood, S.; LeVasseur, N.; Scheer, A.; Simmons, C.E.; et al. Examining Social Media Peer Support and Improving Psychosocial Outcomes for Young Women with Breast Cancer. J. Clin. Oncol. 2021, 39, 162. [Google Scholar] [CrossRef]
- Germani, A.; Buratta, L.; Delvecchio, E.; Mazzeschi, C. Emerging Adults and COVID-19: The Role of Individualism-Collectivism on Perceived Risks and Psychological Maladjustment. Int. J. Environ. Res. Public Health 2020, 17, 3497. [Google Scholar] [CrossRef]
- Cavicchioli, M.; Ferrucci, R.; Guidetti, M.; Canevini, M.P.; Pravettoni, G.; Galli, F. What Will Be the Impact of the COVID-19 Quarantine on Psychological Distress? Considerations Based on a Systematic Review of Pandemic Outbreaks. Healthcare 2021, 9, 101. [Google Scholar] [CrossRef]
- Rowlands, I.; Nicholas, D.; Russell, B.; Canty, N.; Watkinson, A. Social Media Use in the Research Workflow. Learn. Publ. 2011, 24, 183–195. [Google Scholar] [CrossRef]
- Waltman, L.; Pinfield, S.; Rzayeva, N.; Oliveira Henriques, S.; Fang, Z.; Brumberg, J.; Greaves, S.; Hurst, P.; Collings, A.; Heinrichs, A.; et al. Scholarly Communication in Times of Crisis: The Response of the Scholarly Communication System to the COVID-19 Pandemic; Report; Research on Research Institute: Springfield, OR, USA, 2021. [Google Scholar] [CrossRef]
- Choo, E.K.; Ranney, M.L.; Chan, T.M.; Trueger, N.S.; Walsh, A.E.; Tegtmeyer, K.; McNamara, S.O.; Choi, R.Y.; Carroll, C.L. Twitter as a Tool for Communication and Knowledge Exchange in Academic Medicine: A Guide for Skeptics and Novices. Med. Teach. 2015, 37, 411–416. [Google Scholar] [CrossRef]
- Rosenberg, H.; Syed, S.; Rezaie, S. The Twitter Pandemic: The Critical Role of Twitter in the Dissemination of Medical Information and Misinformation during the COVID-19 Pandemic. CJEM 2020, 22, 418–421. [Google Scholar] [CrossRef]
- Nik-Bakht, M.; El-Diraby, T.E. Towards Bottom-Up Decision Making and Collaborative Knowledge Generation in Urban Infrastructure Projects Through Online Social Media. In Transparency in Social Media; Computational Social Sciences; Springer: Cham, Switzerland, 2015. [Google Scholar]
- Castillo, L.I.R.; Hadjistavropoulos, T.; Brachaniec, M. The Effectiveness of Social Media in the Dissemination of Knowledge About Pain in Dementia. Pain Med. 2021, 22, 2584–2596. [Google Scholar] [CrossRef]
- Zhou, J.Z.; Lemelman, B.T.; Done, N.; Henderson, M.L.; Macmillan, A.; Song, D.H.; Dorafshar, A.H. Social Media and the Dissemination of Research: Insights from the Most Widely Circulated Articles in Plastic Surgery. Plast. Reconstr. Surg. 2018, 142, 555–561. [Google Scholar] [CrossRef]
- Olmos-Vega, F.M.; Stalmeijer, R.E.; Varpio, L.; Kahlke, R. A Practical Guide to Reflexivity in Qualitative Research: AMEE Guide No. 149. Med. Teach. 2022, 1–11. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Novel Coronavirus (2019-nCoV) Situation Report-13. 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200202-sitrep-13-ncov-v3.pdf?sfvrsn=195f4010_6 (accessed on 15 June 2022).

| Tweeter Background | Number of Tweets (%) |
|---|---|
| Advocacy Organization | 51 (12.6%) |
| Research Organization | 48 (11.9%) |
| Research and Hospital Cancer Center | 45 (11%) |
| Breast Surgeon | 38 (9.4%) |
| Online News/Journals | 36 (8.9%) |
| Cancer Support Centers | 23 (5.7%) |
| Private Industry Organization | 23 (5.7%) |
| Scientist/Researcher/Professor | 18 (4.5%) |
| Charity Foundations | 18 (4.5%) |
| Breast Oncologist | 15 (3.7%) |
| Patient/Survivors | 14 (3.5%) |
| Executives of private companies | 12 (3%) |
| University Hospitals | 11 (2.7%) |
| Healthcare Journalist | 11 (2.7%) |
| Radiation Oncology | 10 (2.5%) |
| Oncoplastic Reconstructive Breast Surgery | 9 (2.2%) |
| Screening Diagnostic Centers | 8 (1.9%) |
| Psychotherapist/Counselor | 7 (1.7%) |
| Patient family member | 4 (0.9%) |
| Breast Pathologists | 2 (0.5%) |
| Region of Tweets | Number of Tweets (%) |
|---|---|
| United States of America | 258 (64%) |
| United Kingdom | 58 (14.4%) |
| Canada | 25 (6.2%) |
| India | 13 (3.2%) |
| Scotland | 9 (2.2%) |
| Europe | 5 (1.2%) |
| Ireland | 5 (1.2%) |
| France | 4 (0.99%) |
| Portugal | 3 (0.74%) |
| Jordan | 3 (0.74%) |
| Australia | 3 (0.74%) |
| China | 2 (0.49%) |
| Mexico | 2 (0.49%) |
| Brazil | 1 (0.24%) |
| Argentina | 1 (0.24%) |
| Colombia | 1 (0.24%) |
| Belgium | 1 (0.24%) |
| Germany | 1 (0.24%) |
| Spain | 1 (0.24%) |
| Italy | 1 (0.24%) |
| Hungary | 1 (0.24%) |
| Switzerland | 1 (0.24%) |
| Sweden | 1 (0.24%) |
| Israel | 1 (0.24%) |
| United Arab Emirates | 1 (0.24%) |
| Lebanon | 1 (0.24%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naganathan, G.; Bilgen, I.; Cleland, J.; Reel, E.; Cil, T. #COVID19 and #Breastcancer: A Qualitative Analysis of Tweets. Curr. Oncol. 2022, 29, 8483-8500. https://doi.org/10.3390/curroncol29110669
Naganathan G, Bilgen I, Cleland J, Reel E, Cil T. #COVID19 and #Breastcancer: A Qualitative Analysis of Tweets. Current Oncology. 2022; 29(11):8483-8500. https://doi.org/10.3390/curroncol29110669
Chicago/Turabian StyleNaganathan, Gayathri, Idil Bilgen, Jordan Cleland, Emma Reel, and Tulin Cil. 2022. "#COVID19 and #Breastcancer: A Qualitative Analysis of Tweets" Current Oncology 29, no. 11: 8483-8500. https://doi.org/10.3390/curroncol29110669
APA StyleNaganathan, G., Bilgen, I., Cleland, J., Reel, E., & Cil, T. (2022). #COVID19 and #Breastcancer: A Qualitative Analysis of Tweets. Current Oncology, 29(11), 8483-8500. https://doi.org/10.3390/curroncol29110669





