The Feasibility of Immunocryosurgery in the Treatment of Non-Superficial, Facial Basal Cell Carcinoma That Relapsed after Standard Surgical Excision: An Experience Report from Two Centers
Abstract
1. Introduction
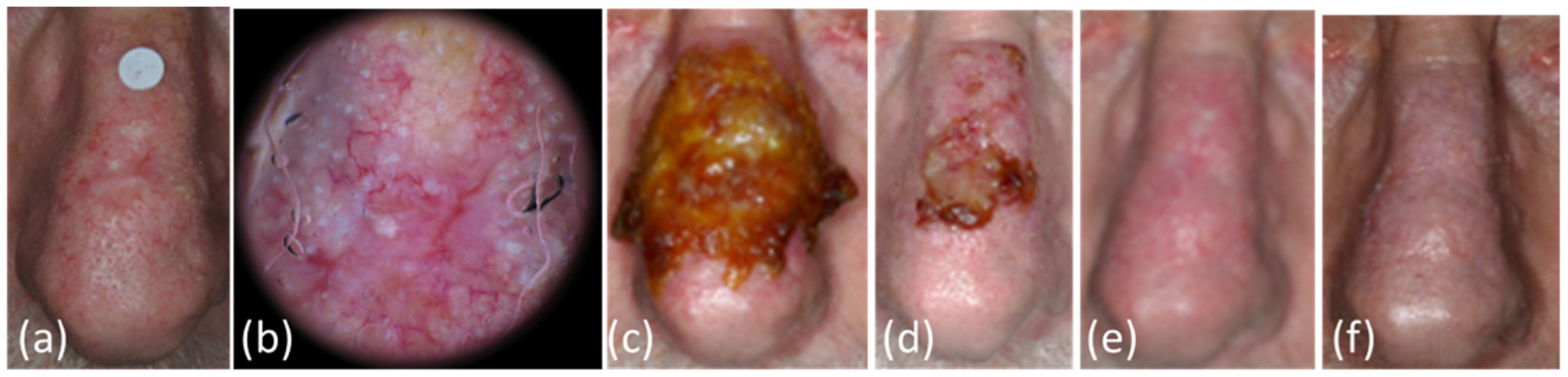
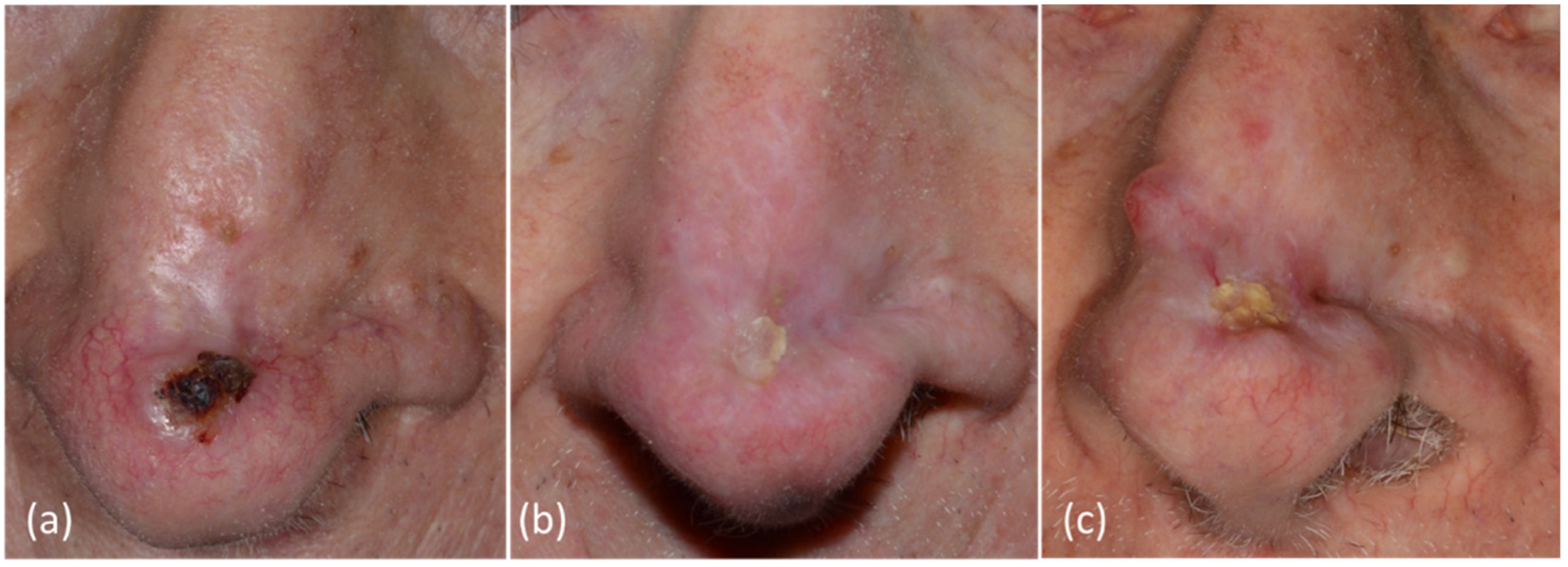
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gaitanis, G.; Bassukas, I.D. A Review of Immunocryosurgery and a Practical Guide to Its Applications. Diseases 2021, 9, 71. [Google Scholar] [CrossRef] [PubMed]
- Gaitanis, G.; Bassukas, I.D. Immunocryosurgery for non-superficial basal cell carcinoma: A prospective, open-label phase III study for tumours ≤2 cm in diameter. Acta Derm.-Venereol. 2014, 94, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Gaitanis, G.; Bassukas, I.D. Immunocryosurgery for non-superficial basal cell carcinomas ≤20 mm in maximal diameter: Five-year follow-up. J. Geriatr. Oncol. 2019, 10, 475–478. [Google Scholar] [CrossRef] [PubMed]
- Mosterd, K.; Krekels, G.A.; Nieman, F.H.; Ostertag, J.U.; Essers, B.A.B.; Dirksen, C.D.; Steijlen, P.M.; Vermeulen, A.; Neumann, H.; Kelleners-Smeets, N.W.J. Surgical excision versus Mohs’ micrographic surgery for primary and recurrent basal-cell carcinoma of the face: A prospective randomised controlled trial with 5-years’ follow-up. Lancet Oncol. 2008, 9, 1149–1156. [Google Scholar] [CrossRef]
- Bassukas, I.D.; Gaitanis, G. Combination of cryosurgery and topical imiquimod: Does timing matter for successful immunocryosurgery? Cryobiology 2009, 59, 116–117. [Google Scholar] [CrossRef]
- Gaitanis, G.; Alexopoulos, E.C.; Bassukas, I.D. Cryosurgery is more effective in the treatment of primary, non-superficial basal cell carcinomas when applied during and not prior to a five week imiquimod course: A randomized, prospective, open-label study. Eur. J. Dermatol. 2011, 21, 952–958. [Google Scholar] [CrossRef]
- Nomikos, K.; Lampri, E.; Spyridonos, P.; Bassukas, I.D. Alterations in the inflammatory cells infiltrating basal cell carcinomas during immunocryosurgery. Arch. Dermatol. Res. 2019, 311, 499–504. [Google Scholar] [CrossRef]
- Gaitanis, G.; Ganiatsa, A.; Vartholomatos, G.; Karamoutsios, A.; Pappas, P.; Bassukas, I.D. Immunocryosurgery for basal cell carcinoma: Impact on circulating CD4 + CD25 high T regulatory cells and serum cytokines. Eur. J. Dermatol. 2020, 30, 605–606. [Google Scholar] [CrossRef]
- Nakuçi, M.; Bassukas, I.D. Office-based treatment of basal cell carcinoma with immunocryosurgery: Feasibility and efficacy. Acta Dermatovenerol. Alp. Panon. Adriat. 2013, 22, 35–38. [Google Scholar]
- Gaitanis, G.; Bassukas, I.D. Immunocryosurgery-An effective combinational modality for Bowen’s disease. Dermatol. Ther. 2016, 29, 334–337. [Google Scholar] [CrossRef]
- Tsironi, T.; Gaitanis, G.; Pappas, C.; Koutlas, V.; Dounousi, E.; Bassukas, I.D. Immunocryosurgery is a safe and feasible treatment for basal cell carcinoma and Bowen disease in renal transplant recipients. Dermatol. Ther. 2022, 35, e15405. [Google Scholar] [CrossRef] [PubMed]
- Oro-Ayude, M.; Gonzalez-Sixto, B.; Faraldo-Lorenzo, J.M.; Feal, C.; Flórez, A. Periocular lentigo maligna successfully treated with immunocryosurgery. Dermatol. Ther. 2021, 34, e14561. [Google Scholar] [CrossRef] [PubMed]
- Matas-Nadal, C.; Sòria, X.; García-de-la-Fuente, M.R.; Huerva, V.; Ortega, E.; Vilardell, F.; Gatius, S.; Casanova, J.M.; Martí, R.M. Immunocryosurgery as monotherapy for lentigo maligna or combined with surgical excision for lentigo maligna melanoma. J. Dermatol. 2018, 45, 564–570. [Google Scholar] [CrossRef]
- Voulgari, P.V.; Gaitanis, G.; Markatseli, T.E.; Kempf, W.; Bassukas, I.D. In transit recurrence of merkel cell carcinoma associated with polyarthritis effectively treated with immunocryosurgery. Acta Derm. Venereol. 2014, 94, 739–740. [Google Scholar] [CrossRef] [PubMed]
- Gaitanis, G.; Vlachos, C.; Bassukas, I.D. Individualized, Adjuvant-Intensified Immunocryosurgery for the Treatment of Squamous Cell Carcinoma in the Oldest Old: An Exploratory Case Series. Actas Dermosifiliogr. 2022, 113, 750–753. [Google Scholar] [CrossRef]
- Gaitanis, G.; Kalogeropoulos, C.D.; Bassukas, I.D. Cryosurgery during Imiquimod (Immunocryosurgery) for Periocular Basal Cell Carcinomas: An Efficacious Minimally Invasive Treatment Alternative. Dermatology 2016, 232, 17–21. [Google Scholar] [CrossRef]
- Ceder, H.; Grönberg, M.; Paoli, J. Mohs micrographic surgery for primary versus recurrent or incompletely excised facial high-risk basal cell carcinomas. Acta Derm.-Venereol. 2021, 101, adv00381. [Google Scholar] [CrossRef]
- Trakatelli, M.; Morton, C.; Nagore, E.; Ulrich, C.; Del Marmol, V.; Peris, K.; Basset-Seguin, N. Update of the European guidelines for basal cell carcinoma management. Eur. J. Dermatol. 2014, 24, 312–329. [Google Scholar] [CrossRef]
- Linos, E.; Schroeder, S.A.; Chren, M.M. Potential overdiagnosis of basal cell carcinoma in older patients with limited life expectancy. J. Am. Med. Assoc. 2014, 312, 997–998. [Google Scholar] [CrossRef]
- Gaitanis, G.; Nomikos, K.; Vava, E.; Alexopoulos, E.C.; Bassukas, I.D. Immunocryosurgery for basal cell carcinoma: Results of a pilot, prospective, open-label study of cryosurgery during continued imiquimod application. J. Eur. Acad. Dermatol. Venereol. 2009, 23, 1427–1430. [Google Scholar] [CrossRef]
- Gaitanis, G.; Nomikos, K.; Vlachos, C.; Bassukas, I.D. Immunocryosurgery for patients with therapeutically challenging basal cell carcinomas: Report of two representative cases. J. Dermatol. Treat. 2012, 23, 70–71. [Google Scholar] [CrossRef] [PubMed]
- Bath-Hextall, F.; Ozolins, M.; Armstrong, S.J.; Colver, G.B.; Perkins, W.; Miller, P.S.J.; Williams, H.C. Surgical excision versus imiquimod 5% cream for nodular and superficial basal-cell carcinoma (SINS): A multicentre, non-inferiority, randomised controlled trial. Lancet Oncol. 2014, 15, 96–105. [Google Scholar] [CrossRef]
- Peris, K.; Fargnoli, M.C.; Garbe, C.; Kaufmann, R.; Bastholt, L.; Seguin, N.B.; Bataille, V.; Del Marmol, V.; Dummer, R.; Harwood, C.A.; et al. Diagnosis and treatment of basal cell carcinoma: European consensus-based interdisciplinary guidelines. Eur. J. Cancer 2019, 118, 10–34. [Google Scholar] [CrossRef] [PubMed]
- Peris, K.; Licitra, L.; Ascierto, P.A.; Corvò, R.; Simonacci, M.; Picciotto, F.; Gualdi, G.; Pellacani, G.; Santoro, A. Identifying locally advanced basal cell carcinoma eligible for treatment with vismodegib: An expert panel consensus. Future Oncol. 2015, 11, 703–712. [Google Scholar] [CrossRef] [PubMed]
- Sekulic, I.A.; Yoo, S.; Kudchadkar, R.; Guillen, J.; Rogers, G.; Chang, A.L.S.; Guenthner, S.; Raskin, B.; Dawson, K.; Mun, Y.; et al. Real-world assessment and treatment of locally advanced basal cell carcinoma: Findings from the RegiSONIC disease registry. PLoS ONE 2022, 17, e0262151. [Google Scholar] [CrossRef]
- Bichakjian, C.K.; Olencki, T.; Aasi, S.Z.; Alam, M.; Andersen, J.S.; Berg, D.; Bowen, G.M.; Cheney, R.T.; Daniels, G.A.; Glass, L.F.; et al. Basal Cell Skin Cancer, Version 1.2016, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2016, 14, 574–597. [Google Scholar] [CrossRef]
- Pellegrini, C.; Maturo, M.; Di Nardo, L.; Ciciarelli, V.; Gutiérrez García-Rodrigo, C.; Fargnoli, M.C. Understanding the Molecular Genetics of Basal Cell Carcinoma. Int. J. Mol. Sci. 2017, 18, 2485. [Google Scholar] [CrossRef]
- Lomas, A.; Leonardi-Bee, J.; Bath-Hextall, F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br. J. Dermatol. 2012, 166, 1069–1080. [Google Scholar] [CrossRef]
- Schön, M.P.; Schön, M. Imiquimod: Mode of action. Br. J. Dermatol. 2007, 157 (Suppl. S2), 8–13. [Google Scholar] [CrossRef]
- Hanna, E.; Abadi, R.; Abbas, O. Imiquimod in dermatology: An overview. Int. J. Dermatol. 2016, 55, 831–844. [Google Scholar] [CrossRef]
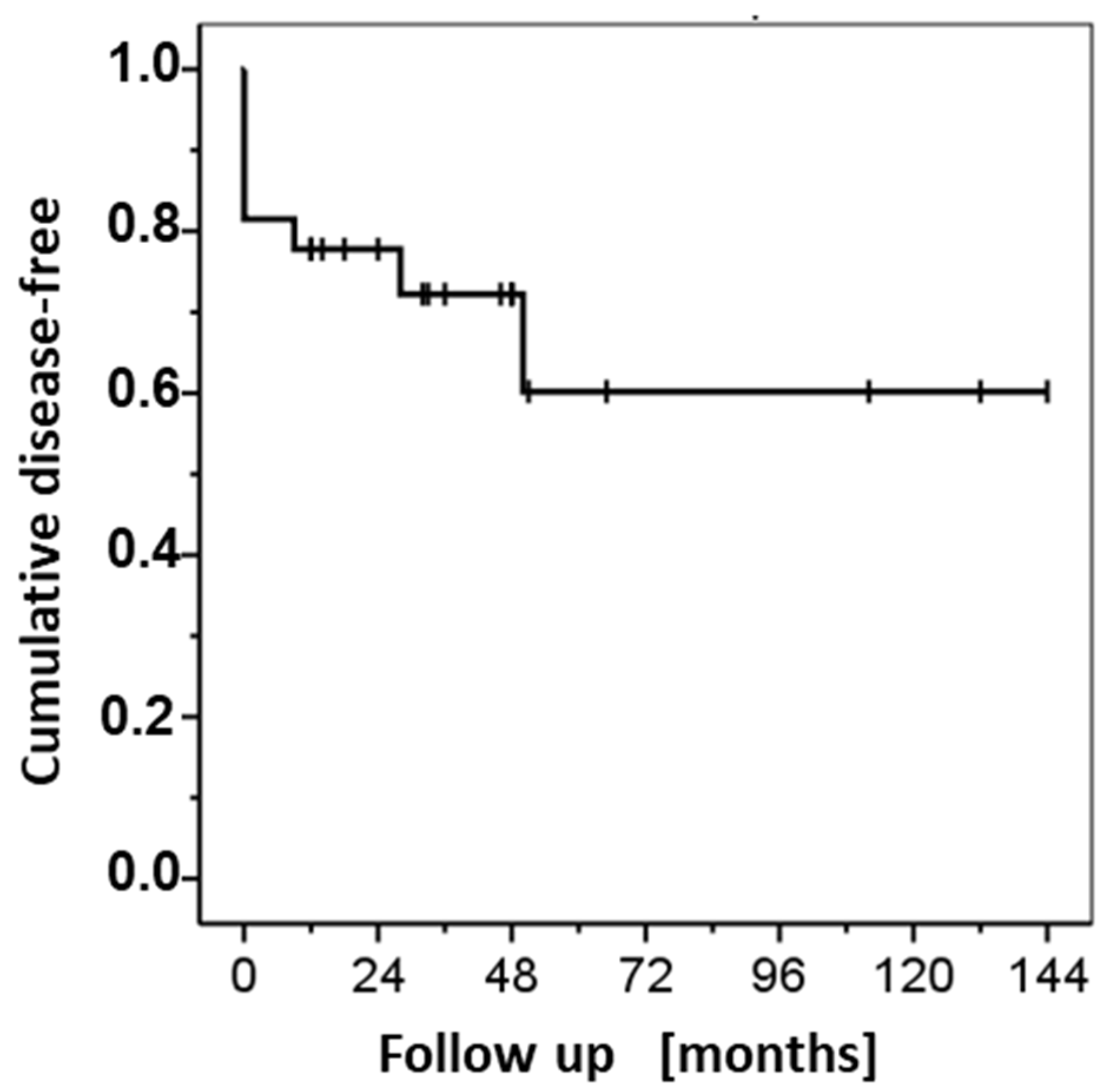
| Follow-up [months] | Cases in Follow-up (% of Initial Cases) | BCC Sites not Disease Free (in Interval) | Disease-Free [S.E.] % | |
|---|---|---|---|---|
| All Cases (n = 27) | Cleared BCC (n = 22) # | |||
| 0 * | 22 (81.5) | 5 | 81.5 [7.5] | 100 |
| 12 | 21 (77.8) | 1 &,$ | 77.8 [8.0] | 95.5 [4.4] |
| 18 | 16 (59.3) | 0 | ||
| 24 | 15 (55.6) | 0 | ||
| 36 | 11 (40.7) | 1 &,† | 72.2 [9.2] | |
| 48 | 9 (33.3) | 0 | ||
| 60 | 4 (14.8) | 1 &,$ | 60.2 [13.4] | 81.8 [13.2] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaitanis, G.; Zampeta, A.; Tsintzou, P.; Fillis, G.; Seretis, K.; Feldmeyer, L.; Bassukas, I. The Feasibility of Immunocryosurgery in the Treatment of Non-Superficial, Facial Basal Cell Carcinoma That Relapsed after Standard Surgical Excision: An Experience Report from Two Centers. Curr. Oncol. 2022, 29, 8475-8482. https://doi.org/10.3390/curroncol29110668
Gaitanis G, Zampeta A, Tsintzou P, Fillis G, Seretis K, Feldmeyer L, Bassukas I. The Feasibility of Immunocryosurgery in the Treatment of Non-Superficial, Facial Basal Cell Carcinoma That Relapsed after Standard Surgical Excision: An Experience Report from Two Centers. Current Oncology. 2022; 29(11):8475-8482. https://doi.org/10.3390/curroncol29110668
Chicago/Turabian StyleGaitanis, Georgios, Athanasia Zampeta, Panagiota Tsintzou, Grigorios Fillis, Konstantinos Seretis, Laurence Feldmeyer, and Ioannis Bassukas. 2022. "The Feasibility of Immunocryosurgery in the Treatment of Non-Superficial, Facial Basal Cell Carcinoma That Relapsed after Standard Surgical Excision: An Experience Report from Two Centers" Current Oncology 29, no. 11: 8475-8482. https://doi.org/10.3390/curroncol29110668
APA StyleGaitanis, G., Zampeta, A., Tsintzou, P., Fillis, G., Seretis, K., Feldmeyer, L., & Bassukas, I. (2022). The Feasibility of Immunocryosurgery in the Treatment of Non-Superficial, Facial Basal Cell Carcinoma That Relapsed after Standard Surgical Excision: An Experience Report from Two Centers. Current Oncology, 29(11), 8475-8482. https://doi.org/10.3390/curroncol29110668





