Appraisals by Health Technology Assessment Agencies of Economic Evaluations Submitted as Part of Reimbursement Dossiers for Oncology Treatments: Evidence from Canada, the UK, and Australia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Data
2.2. Data Abstraction
2.3. Data Analyses
3. Results
3.1. Number of HTA Submissions Reviewed by CADTH between 2019–2020 Matched with Corresponding HTAs from NICE and PBAC
3.2. Manufacturer Economic Submissions’ Characteristics
3.3. HTA Agency Reporting on Economic Model Characteristics Submitted by Manufacturers
3.4. HTA Agency Reporting on Methods Used to Extrapolate Survival Data in Manufacturers’ Cost-Effectiveness Models
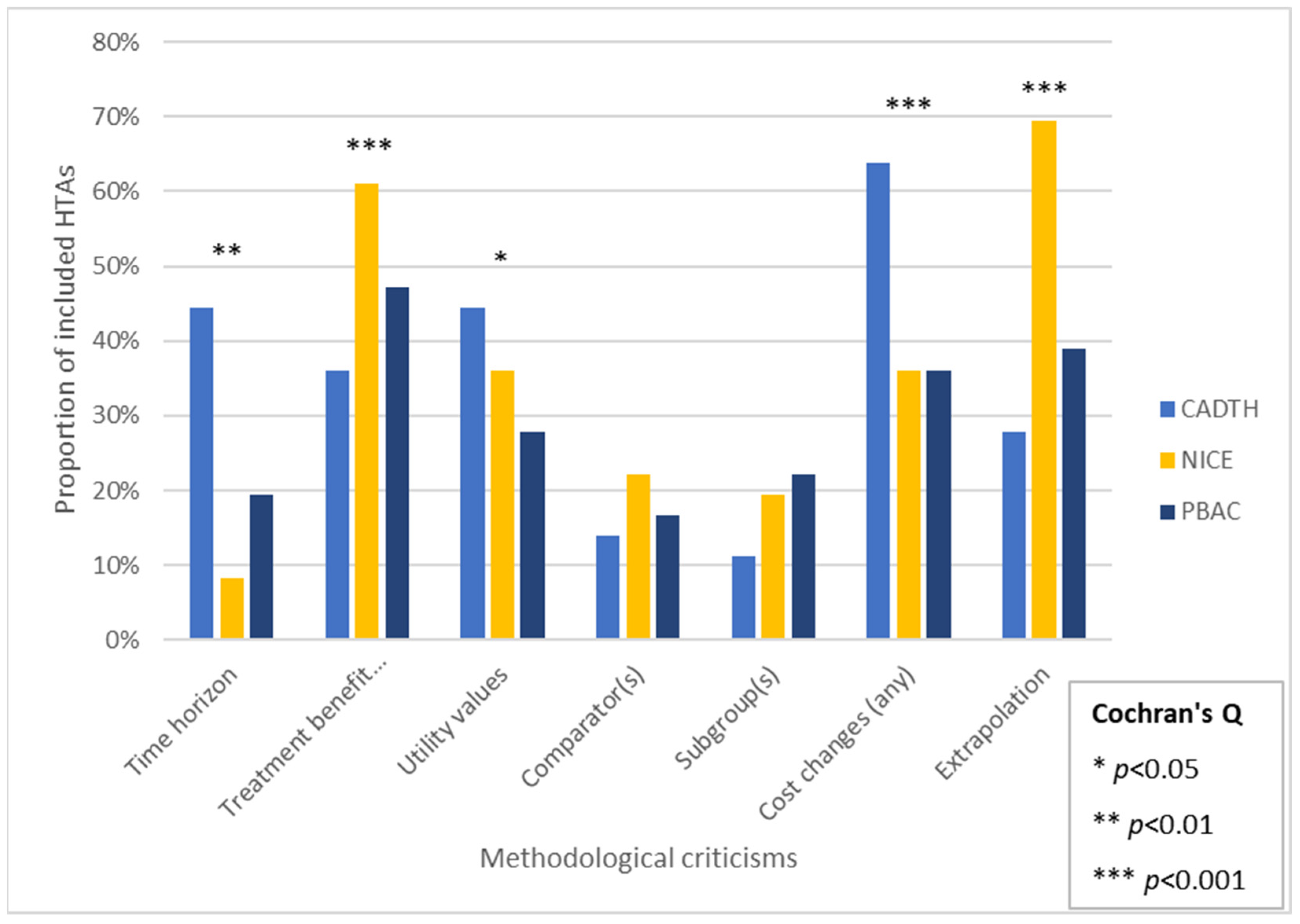
3.5. HTA Agency Reporting on Methodological Criticisms of Manufacturer Economic Submissions
3.6. HTA Agency Reporting on Economic Results, HTA Economic Re-Analyses and Funding Recommendations
4. Discussion
4.1. Summary of Findings
4.2. Previous Studies
4.3. Limitations
4.4. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Allen, N.; Walker, S.R.; Liberti, L.; Salek, S. Health Technology Assessment (HTA) Case Studies: Factors Influencing Divergent HTA Reimbursement Recommendations in Australia, Canada, England, and Scotland. Value Health 2017, 20, 320–328. [Google Scholar] [CrossRef]
- Vreman, R.A.; Mantel-Teeuwisse, A.K.; Hövels, A.M.; Leufkens, H.G.M.; Goettsch, W.G. Differences in Health Technology Assessment Recommendations Among European Jurisdictions: The Role of Practice Variations. Value Health 2020, 23, 10–16. [Google Scholar] [CrossRef]
- European Observatory Health Policy Series. In Improving Healthcare Quality in Europe: Characteristics, Effectiveness and Implementation of Different Strategies; Busse, R., Klazinga, N., Panteli, D., Quentin, W., Eds.; World Health Organization and OECD: Copenhagen, Denmark, 2019. [Google Scholar]
- Canadian Agency for Drugs and Technologies in Health (CADTH). Guidelines for the Economic Evaluation of Health Technologies: Canada, 4th ed.; Canadian Agency for Drugs and Technologies in Health (CADTH): Ottawa, ON, Canada, 2021. Available online: https://www.cadth.ca/about-cadth/how-we-do-it/methods-and-guidelines/guidelines-for-the-economic-evaluation-of-health-technologies-canada (accessed on 29 October 2021).
- National Institute for Health and Care Excellence (NICE). Guide to the Methods of Technology Appraisal 2013; National Institute for Health and Care Excellence (NICE): London, UK, 2013; Available online: https://www.nice.org.uk/process/pmg9/resources/guide-to-the-methods-of-technology-appraisal-2013-pdf-2007975843781 (accessed on 14 November 2021).
- Department of Health AG. Guidelines for Preparing a Submission to the Pharmaceutical Benefits Advisory Committee (PBAC), Version 5.0. Available online: https://pbac.pbs.gov.au/content/information/files/pbac-guidelines-version-5.pdf (accessed on 22 November 2021).
- Ball, G.; Levine, M.; Thabane, L.; Tarride, J.-E. Onwards and Upwards: A Systematic Survey of Economic Evaluation Methods in Oncology. PharmacoEconomics-Open 2021, 5, 397–410. [Google Scholar] [CrossRef]
- Latimer, N.R. Survival analysis for economic evaluations alongside clinical trials—Extrapolation with patient-level data: Inconsistencies, limitations, and a practical guide. Med. Decis. Making 2013, 33, 743–754. [Google Scholar] [CrossRef]
- Husereau, D.; Drummond, M.; Petrou, S.; Carswell, C.; Moher, D.; Greenberg, D.; Augustovski, F.; Briggs, A.H.; Mauskopf, J.; Loder, E. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ 2013, 346, f1049. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, S.D.; Willke, R.J.; Glick, H.; Reed, S.D.; Augustovski, F.; Jonsson, B.; Briggs, A.H.; Sullivan, S. Cost-effectiveness analysis alongside clinical trials II-An ISPOR Good Research Practices Task Force report. Value Health 2015, 18, 161–172. [Google Scholar] [CrossRef]
- Caro, J.J.; Briggs, A.H.; Siebert, U.; Kuntz, K.M. Modeling good research practices–overview: A report of the ISPOR-SMDM Modeling Good Research Practices Task Force–1. Value 2012, 15, 796–803. [Google Scholar] [CrossRef]
- Masucci, L.; Beca, J.; Sabharwal, M.; Hoch, J.S. Methodological Issues in Economic Evaluations Submitted to the Pan-Canadian Oncology Drug Review (pCODR). PharmacoEconomic-Open 2017, 1, 255–263. [Google Scholar] [CrossRef]
- Saluja, R.; Jiao, T.; Koshy, L.; Cheung, M.; Chan, K.K.W. Comparing Manufacturer Submitted and Pan-Canadian Oncology Drug Review Reanalysed Incremental Cost-Effectiveness Ratios for Novel Oncology Drugs. Curr. Oncol. 2021, 28, 606–618. [Google Scholar] [CrossRef] [PubMed]
- Organization for Economic Cooperation and Development (OECD). Purchasing Power Parities (PPP) Indicator. Available online: https://www.oecd-ilibrary.org/finance-and-investment/purchasing-power-parities-ppp/indicator/english_1290ee5a-en (accessed on 10 September 2022).
- Chabot, I.; Rocchi, A. Oncology drug health technology assessment recommendations: Canadian versus UK experiences. ClinicoEconomics Outcomes Res. 2014, 6, 357–367. [Google Scholar] [CrossRef][Green Version]
- Spinner, D.S.; Birt, J.; Walter, J.W.; Bowman, L.; Mauskopf, J.; Drummond, M.F.; Copley-Merriman, C. Do different clinical evidence bases lead to discordant health-technology assessment decisions? An in-depth case series across three jurisdictions. ClinicoEconomics Outcomes Res. 2013, 5, 69–85. [Google Scholar]
- Lexchin, J.; Mintzes, B. Medicine reimbursement recommendations in Canada, Australia, and Scotland. Am. J. Manag. Care 2008, 14, 581–588. [Google Scholar]
- Clement, F.M.; Harris, A.; Li, J.J.; Yong, K.; Lee, K.M.; Manns, B.J. Using effectiveness and cost-effectiveness to make drug coverage decisions: A comparison of Britain, Australia, and Canada. JAMA 2009, 302, 1437–1443. [Google Scholar] [CrossRef] [PubMed]
- Levy, A.R.; Mitton, C.; Johnston, K.M.; Harrigan, B.; Briggs, A.H. International comparison of comparative effectiveness research in five jurisdictions: Insights for the US. PharmacoEconomics 2010, 28, 813–830. [Google Scholar] [CrossRef] [PubMed]
- Rocchi, A.; Miller, E.; Hopkins, R.B.; Goeree, R. Common Drug Review recommendations: An evidence base for expectations? PharmacoEconomics 2012, 30, 229–246. [Google Scholar] [CrossRef] [PubMed]
- Samjoo, I.A.; Grima, D.T. Comparison of Cancer Therapy Reimbursement Decisions Made in Canada to Australia, Sweden and the United Kingdom. Value Health 2013, 16, A153. [Google Scholar] [CrossRef][Green Version]
- Bae, G.; Bae, E.Y.; Bae, S. Same drugs, valued aring comparators and methods used in reimbursement recommendations in Australia, Canada, and Korea. Health Policy 2015, 119, 577–587. [Google Scholar] [CrossRef]
- Odom, D.M.L.; Sherif, B.; Nelson, L.; McSorley, D. Methods to assess the association of patient-reported outcomes and clinical endpoints. In Proceedings of the 20th Annual International Meeting of the International Society for Pharmacoeconomics and Outcomes Research, Philadelphia, PA, USA, 18 May 2015. [Google Scholar]
- Grigore, B.; Ciani, O.; Dams, F.; Federici, C.; de Groot, S.; Mollenkamp, M.; Rabbe, S.; Shatrov, K.; Zemplenyi, A.; Taylor, R.S. Surrogate Endpoints in Health Technology Assessment: An International Review of Methodological Guidelines. PharmacoEconomics 2020, 38, 1055–1070. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.; Tappenden, P.; Robinson, S.; Achilla, E.; Aceituno, D.; Byford, S. Systematic review of the methods of health economic models assessing antipsychotic medication for schizophrenia. PLoS ONE 2020, 15, e0234996. [Google Scholar] [CrossRef]
- Lung, T.W.; Muhunthan, J.; Laba, T.L.; Shiell, A.; Milat, A.; Jan, S. Making guidelines for economic evaluations relevant to public health in Australia. Aust. N. Z. J. Public Health 2017, 41, 115–117. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Smith, M.K.; Khan, O.K.; Yip, S.; Tang, P.A. Comparison between Canadian and British oncology drug review recommendations and their impact on patient access. J. Clin. Oncol. 2017, 35, 6537. [Google Scholar] [CrossRef]
- Gibson, S.A.M.; Beale, R.; Wickstead, M.; Griffiths, M. Parallel scientific advice from NICE and CADTH: Would one submission fit all? Value Health 2019, 22, S501. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence (NICE). NICE Launches Ambitious Strategy to Provide Quicker Access to New Treatments and Innovations. 2021. Available online: https://www.nice.org.uk/news/article/nice-launches-ambitious-strategy-to-provide-quicker-access-to-new-treatments-and-innovations (accessed on 6 December 2021).
- Australian Department of Health and Aged Care. Landmark New Medicines Agreements to Bring Significant Benefits for Australian Patients. Media Release 2021. Available online: https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/landmark-new-medicines-agreements-to-bring-significant-benefits-for-australian-patients (accessed on 17 December 2021).
- Canadian Agency for Drugs and Technologies in Health (CADTH). CADTH Pharmaceutical Reviews Update—Issue 17. Reimbursement Reviews 2020. Available online: https://cadth.ca/cadth-pharmaceutical-reviews-update-issue-17 (accessed on 28 October 2021).
- Mathes, T.; Jacobs, E.; Morfeld, J.-C.; Pieper, D. Methods of international health technology assessment agencies for economic evaluations- a comparative analysis. BMC Health Serv. Res. 2013, 13, 371. [Google Scholar] [CrossRef]
| Characteristic | n | % |
|---|---|---|
| HTA agency (n = 108) | ||
| pCODR | 36 | 33% |
| NICE | 36 | 33% |
| PBAC | 36 | 33% |
| Data source type (n = 108) | ||
| Ph3 | 79 | 67% |
| Ph2 (single arm) | 16 | 15% |
| Mix of Ph3 and Ph2 | 4 | 3% |
| RWE | 0 | 0% |
| Mix of Ph2 and RWE | 5 | 6% |
| Mix of Ph3 and RWE | 4 | 7% |
| Ph4 | 0 | 1% |
| Type of cancer studied (n = 108) | ||
| Leukemia | 15 | 14% |
| Breast | 12 | 11% |
| Lung | 27 | 25% |
| Genitourinary | 9 | 8% |
| Gastrointestinal | 12 | 11% |
| Lymphoma | 6 | 6% |
| Skin and melanoma | 12 | 11% |
| Other | 3 | 3% |
| Myeloma | 3 | 3% |
| Gynecology | 6 | 6% |
| Head and neck | 3 | 3% |
| Neurological | 0 | 0% |
| Cancer stage (n = 108) | ||
| Early/stage I | 12 | 11% |
| Stage II/III | 27 | 25% |
| Stage IV/metastatic | 69 | 64% |
| Reported Characteristic | Number of Studies n (%) | p-Value (χ2) | ||
|---|---|---|---|---|
| CADTH | NICE | PBAC | ||
| Type of analysis | ||||
| CUA | 36 (100%) | 36 (100%) | 30 (83%) | 0.013 |
| CEA | 0 (0%) | 0 (0%) | 0 (0%) | |
| Other (e.g., CMA) | 0 (0%) | 0 (0%) | 6 (17%) | |
| QALYs reported (Y/N) | ||||
| Yes | 34 (94%) | 36 (100%) | 30 (83%) | 0.023 |
| No | 2 (6%) | 0 (0%) | 6 (17%) | |
| Utility value method | ||||
| EQ5D | 15 (42%) | 33 (92%) | 18 (50%) | 0.001 |
| SF36 | 0 (0%) | 0 (0%) | 0 (0%) | |
| HUI | 0 (0%) | 0 (0%) | 0 (0%) | |
| Other | 1 (3%) | 1 (3%) | 4 (11%) | |
| Not reported | 20 (56%) | 2 (6%) | 14 (39%) | |
| Model structure | ||||
| Partitioned survival | 25 (69%) | 25 (69%) | 24 (67%) | 0.112 |
| Markov | 11 (31%) | 10 (28%) | 6 (17%) | |
| Not reported | 0 (0%) | 0 (0%) | 6 (17%) | |
| Decision tree | 0 (0%) | 0 (0%) | 0 (0%) | |
| Combination (decision tree + Markov) | 0 (0%) | 1 (3%) | 0 (0%) | |
| Other | 0 (0%) | 0 (0%) | 0 (0%) | |
| Number of modeled health states | ||||
| Three | 24 (67%) | 29 (81%) | 21 (58%) | 0.516 |
| Four | 2 (6%) | 3 (8%) | 4 (11%) | |
| Five | 4 (11%) | 2 (6%) | 1 (3%) | |
| Six | 1 (3%) | 0 (0%) | 3 (8%) | |
| Seven or more | 0 (0%) | 2 (6%) | 0 (0%) | |
| Not reported | 5 (14%) | 0 (0%) | 7 (19%) | |
| Time horizon (submitted by manufacturer) | ||||
| 1–5 years | 4 (11%) | 0 (0%) | 3 (8%) | <0.001 |
| 6–10 years | 14 (39%) | 4 (11%) | 16 (44%) | |
| 11–20 years | 7 (19%) | 10 (28%) | 3 (8%) | |
| 21–30 years | 3 (8%) | 7 (19%) | 3 (8%) | |
| 31–40 years | 2 (6%) | 6 (17%) | 3 (8%) | |
| 40+ years | 6 (17%) | 8 (22%) | 1 (3%) | |
| Not reported | 0 (0%) | 1 (3%) | 7 (19%) | |
| Indirect treatment comparison (Y/N) | ||||
| Yes | 20 (56%) | 24 (67%) | 20 (56%) | 0.541 |
| No | 16 (44%) | 12 (33%) | 16 (44%) | |
| Equity issues reported | ||||
| Yes | 0 (0%) | 15 (42%) | 0 (0%) | <0.001 |
| No | 36 (100%) | 21 (58%) | 36 (100%) | |
| Handling of uncertainty | ||||
| Deterministic sensitivity analysis | 12 (33%) | 33 (92%) | 9 (25%) | <0.001 |
| Probabilistic sensitivity analysis | 11 (31%) | 36 (100%) | 4 (11%) | <0.001 |
| Scenario analysis | 13 (36%) | 36 (100%) | 27 (75%) | <0.001 |
| Validation (Y/N) | ||||
| Yes | 2 (6%) | 35 (97%) | 0 (0%) | <0.001 |
| No | 34 (94%) | 1 (3%) | 36 (100%) | |
| Reimbursement recommendation | ||||
| Reimburse | 28 (78%) | 34 (94%) | 19 (53%) | <0.001 |
| Reported Characteristic | Number of Studies n (%) | p-Value (χ2) | ||
|---|---|---|---|---|
| CADTH | NICE | PBAC | ||
| Parametric approach | ||||
| Yes | 20 (56%) | 36 (100%) | 28 (78%) | <0.001 |
| No | 16 (44%) | 0 (0%) | 8 (22%) | |
| Standard parametric distributions tested | N = 20 | N = 36 | N = 28 | |
| Yes | 17 (85%) | 36 (100%) | 21 (75%) | 0.008 |
| No | 3 (15%) | 0 (0%) | 7 (25%) | |
| Curve fitting assessment | N = 20 | N = 36 | N = 28 | |
| AIC | 1 (5%) | 2 (6%) | 1 (4%) | <0.001 |
| BIC | 1 (5%) | 0 (0%) | 0 (0%) | |
| Both AIC and BIC | 6 (30%) | 30 (83%) | 8 (29%) | |
| Other | 0 (0%) | 2 (6%) | 1 (4%) | |
| Not reported | 28 (60%) | 2 (6%) | 26 (64%) | |
| PH assumption tested (if appropriate) | N = 20 | N = 36 | N = 28 | |
| Yes | 2 (10%) | 32 (89%) | 9 (32%) | <0.001 |
| No | 18 (90%) | 4 (11%) | 19 (68%) | |
| Fitted parametric curves | N = 20 | N = 36 | N = 28 | |
| Jointly fitted models | 1 (5%) | 20 (56%) | 10 (36%) | <0.001 |
| Separately fitted models | 0 (0%) | 11 (31%) | 4 (14%) | |
| Not reported | 19 (95%) | 5 (14%) | 14 (50%) | |
| Validation of extrapolations | ||||
| Yes | 1 (3%) | 35 (97%) | 6 (17%) | <0.001 |
| No | 35 (97%) | 1 (3%) | 30 (83%) | |
| Scenario analyses of treatment effect | ||||
| Yes | 12 (33%) | 19 (53%) | 11 (31%) | 0.109 |
| No | 24 (67%) | 17 (47%) | 25 (69%) | |
| Use/source of external data justified | ||||
| Yes | 1 (3%) | 20 (56%) | 4 (11%) | <0.001 |
| No | 35 (97%) | 16 (44%) | 32 (89%) | |
| Curves fitted to tail of Kaplan–Meier curves only | ||||
| Yes | 1 (3%) | 4 (11%) | 3 (8%) | 0.389 |
| No | 35 (97%) | 32 (89%) | 33 (92%) | |
| Alternative curve-fitting approaches examined | ||||
| Yes | 3 (8%) | 9 (25%) | 1 (3%) | 0.011 |
| No | 33 (92%) | 27 (75%) | 35 (97%) | |
| Selected Parametric Curve Reported | Treatment | Comparator | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CADTH (n = 20) | NICE (n = 36) | PBAC (n = 28) | CADTH (n = 20) | NICE (n = 36) | PBAC (n = 28) | |||||||
| PFS | OS | PFS | OS | PFS | OS | PFS | OS | PFS | OS | PFS | OS | |
| Weibull | 5% | 10% | 22% | 17% | 11% | 14% | 0% | 5% | 22% | 14% | 11% | 14% |
| Exponential | 0% | 5% | 8% | 25% | 25% | 32% | 0% | 5% | 8% | 25% | 25% | 25% |
| Log-logistic | 0% | 5% | 17% | 19% | 7% | 11% | 0% | 0% | 17% | 19% | 11% | 14% |
| Log-normal | 15% | 5% | 19% | 17% | 32% | 14% | 10% | 5% | 17% | 17% | 25% | 18% |
| Gamma | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 3% | 0% | 0% | 0% |
| Generalized gamma | 0% | 0% | 14% | 6% | 11% | 4% | 0% | 5% | 11% | 3% | 11% | 4% |
| Gompertz | 5% | 0% | 8% | 6% | 0% | 7% | 0% | 0% | 8% | 6% | 0% | 7% |
| Other | 0% | 0% | 0% | 3% | 0% | 0% | 0% | 0% | 0% | 3% | 0% | 0% |
| Not reported | 75% | 75% | 11% | 8% | 14% | 18% | 90% | 80% | 14% | 14% | 18% | 18% |
| HTA Agency | Incremental QALYs | |||||
|---|---|---|---|---|---|---|
| Manufacturer: Base Case | Range | Agency Re-Analysis: Base Case | Range | Average Change | ||
| CADTH (n = 32) | 1.30 | 0.13 to 4.34 | CADTH (n = 28) | 0.78 | 0.08 to 2.25 | −60.3% |
| NICE (n = 21) | 1.17 | 0.07 to 3.44 | NICE (n = 15) | 0.68 | 0.07 to 2.75 | −58.5% |
| PBAC (n = 18) | 1.52 | 0.13 to 6.84 | N/A | N/A | N/A | N/A |
| HTA Agency | ICER | |||||
| Manufacturer: Base Case | Range | Agency Re-Analysis | Range | Average Change | ||
| CADTH (n = 32) | $109,581 | $12,242 to $388,172 | CADTH (n = 32) | $200,923 | $41,414 to $983,977 | 183.4% |
| NICE (n = 27) | $65,778 | $6631 to $137,200 | NICE (n = 26) | $112,891 | $23,744 to $229,381 | 171.6% |
| PBAC (n = 23) | $48,665 | $18,910 to $129,217 | N/A | N/A | N/A | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ball, G.; Levine, M.A.H.; Thabane, L.; Tarride, J.-E. Appraisals by Health Technology Assessment Agencies of Economic Evaluations Submitted as Part of Reimbursement Dossiers for Oncology Treatments: Evidence from Canada, the UK, and Australia. Curr. Oncol. 2022, 29, 7624-7636. https://doi.org/10.3390/curroncol29100602
Ball G, Levine MAH, Thabane L, Tarride J-E. Appraisals by Health Technology Assessment Agencies of Economic Evaluations Submitted as Part of Reimbursement Dossiers for Oncology Treatments: Evidence from Canada, the UK, and Australia. Current Oncology. 2022; 29(10):7624-7636. https://doi.org/10.3390/curroncol29100602
Chicago/Turabian StyleBall, Graeme, Mitchell A. H. Levine, Lehana Thabane, and Jean-Eric Tarride. 2022. "Appraisals by Health Technology Assessment Agencies of Economic Evaluations Submitted as Part of Reimbursement Dossiers for Oncology Treatments: Evidence from Canada, the UK, and Australia" Current Oncology 29, no. 10: 7624-7636. https://doi.org/10.3390/curroncol29100602
APA StyleBall, G., Levine, M. A. H., Thabane, L., & Tarride, J.-E. (2022). Appraisals by Health Technology Assessment Agencies of Economic Evaluations Submitted as Part of Reimbursement Dossiers for Oncology Treatments: Evidence from Canada, the UK, and Australia. Current Oncology, 29(10), 7624-7636. https://doi.org/10.3390/curroncol29100602




