Disparities in All-Cause Mortality in Older Patients with Colorectal Cancer According to Disability Status: A Nationwide Analysis
Abstract
1. Introduction
2. Methods
2.1. Data and Study Population
2.2. Variables
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xi, Y.; Xu, P. Global colorectal cancer burden in 2020 and projections to 2040. Transl. Oncol. 2021, 14, 101174. [Google Scholar] [CrossRef] [PubMed]
- Baek, S.K.; Lee, J.S.; Hwang, I.G.; Kim, J.G.; Kim, T.W.; Sohn, S.K.; Kang, M.Y.; Lee, S.-C. Clinical characteristics and survival of colorectal cancer patients in Korea stratified by age. Korean J. Intern. Med. 2021, 36, 985–991. [Google Scholar] [CrossRef]
- Keum, N.; Giovannucci, E. Global burden of colorectal cancer: Emerging trends, risk factors and prevention strategies. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 713–732. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Won, Y.J.; Park, Y.R.; Jung, K.W.; Kong, H.J.; Lee, E.S.; Community of Population-Based Regional Cancer Registries. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2017. Cancer Res. Treat. 2020, 52, 335–350. [Google Scholar] [CrossRef] [PubMed]
- Park, B.; Lee, Y.Y.; Song, S.Y.; Shin, H.Y.; Suh, M.; Choi, K.S.; Jun, J.K. Trends of Colorectal Cancer Screening Rates in Korea: Korean National Cancer Screening Survey 2005–2020. Gut Liver. 2022. Online ahead of print. [Google Scholar] [CrossRef]
- Balducci, L. Management of cancer in the elderly. Oncology (Williston Park). 2006, 20, 135–143, discussion 144, 146, 51–52. [Google Scholar]
- World Health Organization (WHO). World Report on Disability; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Kim, S.H.; Lee, Y.H.; Oh, W.C.; Hwang, J.H.; Oh, M.A.; Lee, N.H.; Oh, D.E.; Kang, D.W.; Kwon, S.J.; Oh, G.K.; et al. 2017 Survey on the Actual Condition of the Disabled; Korea Ministry of Health and Welfare, Korea Institute for Health and Social Affairs: Seoul, Korea, 2017. [Google Scholar]
- Kim, H.W.; Shin, D.W.; Yeob, K.E.; Cho, I.Y.; Kim, S.Y.; Park, S.M.; Park, J.H.; Park, J.H.; Kawachi, I. Disparities in the Diagnosis and Treatment of Gastric Cancer in Relation to Disabilities. Clin. Transl. Gastroenterol. 2020, 11, e00242. [Google Scholar] [CrossRef]
- Cuypers, M.; Schalk, B.; Boonman, A.; Naaldenberg, J.; Leusink, G. Cancer-related mortality among people with intellectual disabilities: A nationwide population-based cohort study. Cancer 2022, 128, 1267–1274. [Google Scholar] [CrossRef]
- Kroll, T.; Jones, G.C.; Kehn, M.; Neri, M.T. Barriers and strategies affecting the utilisation of primary preventive services for people with physical disabilities: A qualitative inquiry. Health Soc. Care Community 2006, 14, 284–293. [Google Scholar] [CrossRef]
- Horner-Johnson, W.; Dobbertin, K.; Lee, J.C.; Andresen, E.M.; Expert Panel on Disability and Health Disparities. Disparities in health care access and receipt of preventive services by disability type: Analysis of the medical expenditure panel survey. Health Serv. Res. 2014, 49, 1980–1999. [Google Scholar] [CrossRef]
- Deroche, C.B.; McDermott, S.W.; Mann, J.R.; Hardin, J.W. Colorectal Cancer Screening Adherence in Selected Disabilities Over 10 Years. Am. J. Prev. Med. 2017, 52, 735–741. [Google Scholar] [CrossRef]
- Singal, N. Disability, poverty and education: Implications for policies and practices. Int. J. Incl. Educ. 2011, 15, 1047–1052. [Google Scholar] [CrossRef]
- Kim, S.; Kim, M.-I.; Han, D. Incidence Rates of Disability and Its Associated Factors among Korean Community-Dwelling Older Adults. Iran J. Public Health 2020, 49, 1718–1726. [Google Scholar] [CrossRef]
- National Health Insurance Sharing Service. Sample Research DB: Details of DB; Publisher National Health Insurance Service: Wonju, Korea, 2022. [Google Scholar]
- Ministry of Health and Welfare. Division Policy for People with Disabilities. Ministry of Health and Welfare: Sejong, Korea, 2022. [Google Scholar]
- Jeon, B.; Noguchi, H.; Kwon, S.; Ito, T.; Tamiya, N. Disability, poverty, and role of the basic livelihood security system on health services utilization among the elderly in South Korea. Soc. Sci. Med. 2017, 178, 175–183. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. The Criteria for Disability Rating [Korean]; Ministry of Health and Welfare: Sejong, Korea, 2015. [Google Scholar]
- Sundararajan, V.; Henderson, T.; Perry, C.; Muggivan, A.; Quan, H.; Ghali, W.A. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J. Clin. Epidemiol. 2004, 57, 1288–1294. [Google Scholar] [CrossRef] [PubMed]
- Bahk, J.; Kang, H.-Y.; Khang, Y.-H. Disability type–specific mortality patterns and life expectancy among dis-abled people in South Korea using 10-year combined data between 2008 and 2017. Prev. Med. Rep. 2022, 29, 101958. [Google Scholar] [CrossRef] [PubMed]
- Reeves, C.; Collingridge, D. Improving cancer care for people with disabilities. Lancet Oncol. 2022, 23, 446–447. [Google Scholar] [CrossRef]
- Park, S.; Son, K.; Park, J.-H.; Cho, B. Disparities in short-term and long-term all-cause mortality among Korean cancer patients with and without preexisting disabilities: A nationwide retrospective cohort study. Support Care Cancer 2011, 20, 963–970. [Google Scholar] [CrossRef]
- Choi, J.Y.; Yeob, K.E.; Hong, S.H.; Kim, S.Y.; Jeong, E.H.; Shin, D.W.; Park, J.H.; Kang, G.W.; Kim, H.S.; Park, J.H.; et al. Disparities in the Diagnosis, Treatment, and Survival Rate of Cervical Cancer among Women with and without Disabilities. Cancer Control 2021, 28, 10732748211055268. [Google Scholar] [CrossRef]
- Kwon, J.; Kim, S.Y.; Yeob, K.E.; Han, H.S.; Lee, K.H.; Shin, D.W.; Kim, Y.Y.; Park, J.H.; Park, J.H. The Effect of Disability on the Diagnosis and Treatment of Multiple Myeloma in Korea: A National Cohort Study. Cancer Res. Treat. 2020, 52, 1–9. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, E.P.; Ngo, L.H.; Chirikos, T.N.; Roetzheim, R.G.; Li, D.; Drews, R.E.; Iezzoni, L.I. Cancer Stage at Diagnosis and Survival among Persons with Social Security Disability Insurance on Medicare. Health Serv. Res. 2007, 42, 611–628. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Lee, J.S.; Lee, J.Y.; Gwack, J.; Park, J.H.; Kim, Y.I.; Kim, Y. Disparities between persons with and without disabilities in their participation rates in mass screening. Eur. J. Public Health 2009, 19, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Jeong, J.; Kim, Y.K.; Jun, E.-K.; Kim, S.Y.; Kim, H.J.; Lee, B.W. Has Disabled Access in Healthcare Institutions been Increased? A Case Study of Jongno-gu in Seoul, Korea. Korean J. Health Policy Adm. 2012, 22, 696–702. [Google Scholar] [CrossRef]
- Shin, D.W.; Cho, J.H.; Noh, J.M.; Han, H.; Han, K.; Park, S.H.; Kim, S.Y.; Park, J.H.; Park, J.H.; Kawachi, I. Disparities in the Diagnosis and Treatment of Lung Cancer among People with Disabilities. J. Thorac. Oncol. 2019, 14, 163–175. [Google Scholar] [CrossRef] [PubMed]
| Total | All-Cause Mortality | All-Cause 5-Year Mortality | |||||
|---|---|---|---|---|---|---|---|
| N | (%) | p-Value | N | (%) | p-Value | ||
| Disability | |||||||
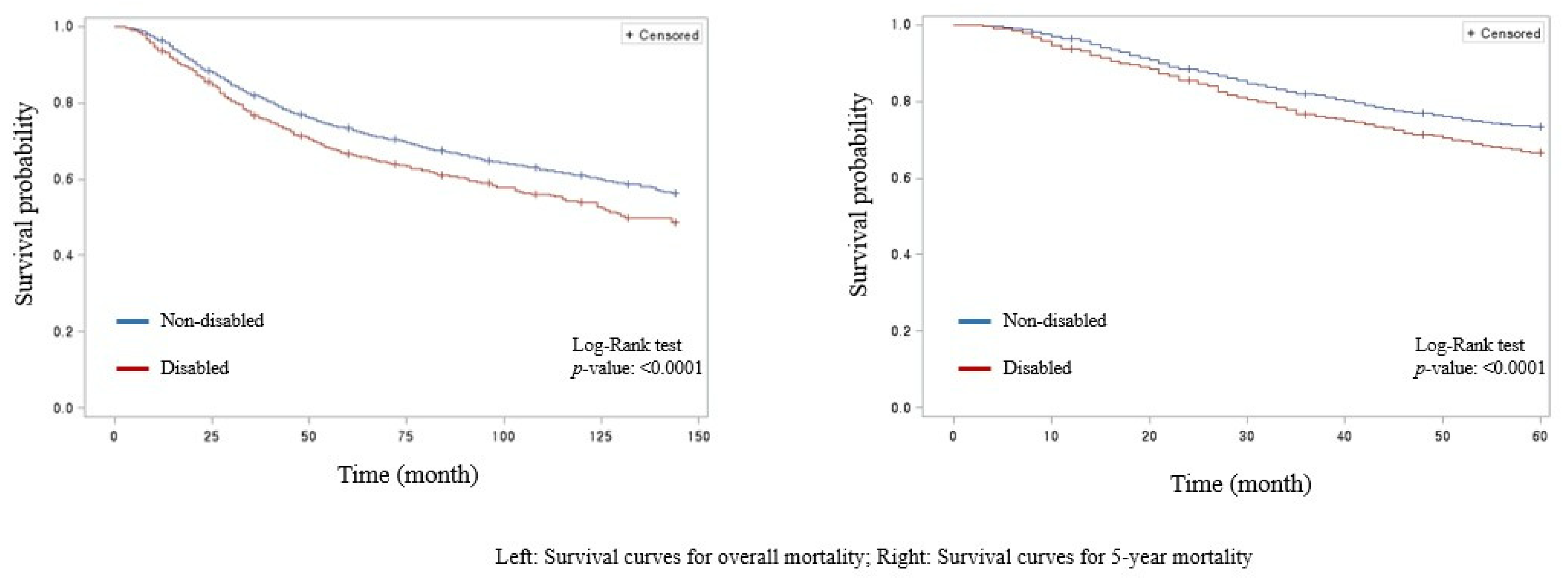
| No | 5341 | 1914 | (35.8) | <0.001 | 1405 | (26.3) | <0.001 |
| Yes | 999 | 420 | (42.0) | 328 | (32.8) | ||
| Disability severity | |||||||
| None | 5341 | 1914 | (35.8) | 0.011 | 1405 | (26.3) | 0.003 |
| Mild | 714 | 282 | (39.5) | 222 | (31.1) | ||
| Severe | 285 | 138 | (48.4) | 106 | (37.2) | ||
| Sex | |||||||
| Male | 3881 | 1494 | (38.5) | <0.001 | 1098 | (28.3) | 0.030 |
| Female | 2459 | 840 | (34.2) | 635 | (25.8) | ||
| Age | |||||||
| 60–69 | 2923 | 817 | (28.0) | <0.001 | 603 | (20.6) | <0.001 |
| 70–79 | 2904 | 1239 | (42.7) | 915 | (31.5) | ||
| ≥80 | 513 | 278 | (54.2) | 215 | (41.9) | ||
| Income | |||||||
| Q1 | 1437 | 567 | (39.5) | 0.110 | 423 | (29.4) | 0.130 |
| Q2 | 1111 | 403 | (36.3) | 308 | (27.7) | ||
| Q3 | 1750 | 640 | 36.6) | 474 | (27.1) | ||
| Q4 | 2042 | 724 | (35.5) | 528 | (25.9) | ||
| Type of healthcare insurance | |||||||
| Medical Aid | 355 | 171 | (48.2) | <0.001 | 125 | (35.2) | 0.003 |
| NHI Self employed | 1831 | 654 | (35.7) | 484 | (26.4) | ||
| NHI Employee | 4154 | 1509 | (36.3) | 1124 | (27.1) | ||
| Region | |||||||
| Urban | 4103 | 1449 | (35.3) | <0.001 | 1082 | (26.4) | 0.020 |
| Rural | 2237 | 885 | (39.6) | 651 | (29.1) | ||
| Chronic diseases | |||||||
| None | 715 | 243 | (34.0) | 0.100 | 186 | (26.0) | 0.400 |
| ≥1 | 5625 | 2091 | (37.2) | 1547 | (27.5) | ||
| CCI * | |||||||
| 0 | 1391 | 305 | (21.9) | <0.001 | 194 | (13.9) | <0.001 |
| 1 | 896 | 259 | (28.9) | 160 | (17.9) | ||
| 2 | 806 | 222 | (27.5) | 146 | (18.1) | ||
| ≥3 | 3247 | 1548 | (47.7) | 1233 | (38.0) | ||
| Type of treatment | |||||||
| Surgery only | 5102 | 1637 | (32.1) | <0.001 | 1151 | (22.6) | <0.001 |
| Surgery and chemo or radiotherapy | 788 | 362 | (45.9) | 270 | (34.3) | ||
| Chemo or radiotherapy only | 450 | 335 | (74.4) | 312 | (69.3) | ||
| Type of hospital | |||||||
| Tertiary hospital | 3918 | 1384 | (35.3) | 0.002 | 1017 | (26.0) | 0.002 |
| General hospital | 2422 | 950 | (39.2) | 716 | (29.6) | ||
| Total | 6340 | 2334 | (36.8) | 1733 | (27.3) | ||
| All-Cause Mortality | All-Cause 5-Year Mortality | |||||
|---|---|---|---|---|---|---|
| HR * | 95% CI * | HR * | 95% CI * | |||
| Disability | ||||||
| No | 1.00 | 1.00 | ||||
| Yes | 1.15 | (1.03 | 1.28) | 1.21 | (1.07 | 1.37) |
| Sex | ||||||
| Male | 1.00 | 1.00 | ||||
| Female | 0.81 | (0.74 | 0.88) | 0.85 | (0.77 | 0.93) |
| Age | ||||||
| 60–69 | 1.00 | 1.00 | ||||
| 70–79 | 1.82 | (1.66 | 1.99) | 1.73 | (1.55 | 1.92) |
| ≥80 | 3.18 | (2.76 | 3.66) | 2.91 | (2.47 | 3.42) |
| Income | ||||||
| Q1 | 1.00 | 1.00 | ||||
| Q2 | 1.03 | (0.90 | 1.19) | 1.05 | (0.90 | 1.23) |
| Q3 | 0.99 | (0.88 | 1.13) | 0.99 | (0.85 | 1.14) |
| Q4 | 0.93 | (0.82 | 1.05) | 0.92 | (0.79 | 1.06) |
| Type of healthcare insurance | ||||||
| Medical Aid | 1.00 | 1.00 | ||||
| NHI Self employed | 0.84 | (0.69 | 1.02) | 0.89 | (0.71 | 1.12) |
| NHI Employee | 0.86 | (0.71 | 1.03) | 0.91 | (0.73 | 1.12) |
| Region | ||||||
| Urban | 1.00 | 1.00 | ||||
| Rural | 1.1 | (1.01 | 1.20) | 1.07 | (0.97 | 1.19) |
| Chronic diseases | ||||||
| None | 1.00 | 1.00 | ||||
| ≥1 | 0.94 | (0.82 | 1.08) | 0.87 | (0.75 | 1.02) |
| CCI * | ||||||
| 0 | 1.00 | 1.00 | ||||
| 1 | 1.23 | (1.04 | 1.45) | 1.18 | (0.96 | 1.46) |
| 2 | 1.23 | (1.04 | 1.47) | 1.23 | (0.99 | 1.53) |
| ≥3 | 2.43 | (2.14 | 2.75) | 2.73 | (2.34 | 3.19) |
| Type of treatment | ||||||
| Surgery only | 1.00 | 1.00 | ||||
| Surgery and chemo or radiotherapy | 1.71 | (1.53 | 1.92) | 1.77 | (1.55 | 2.02) |
| Chemo or radiotherapy only | 4.41 | (3.90 | 4.99) | 4.86 | (4.27 | 5.54) |
| Type of hospital | ||||||
| Tertiary hospital | 1.00 | 1.00 | ||||
| General hospital | 1.09 | (1.00 | 1.19) | 1.12 | (1.01 | 1.23) |
| All-Cause Mortality | All-Cause 5-Year Mortality | ||||||
|---|---|---|---|---|---|---|---|
| HR * | 95% CI * | HR * | 95% CI * | ||||
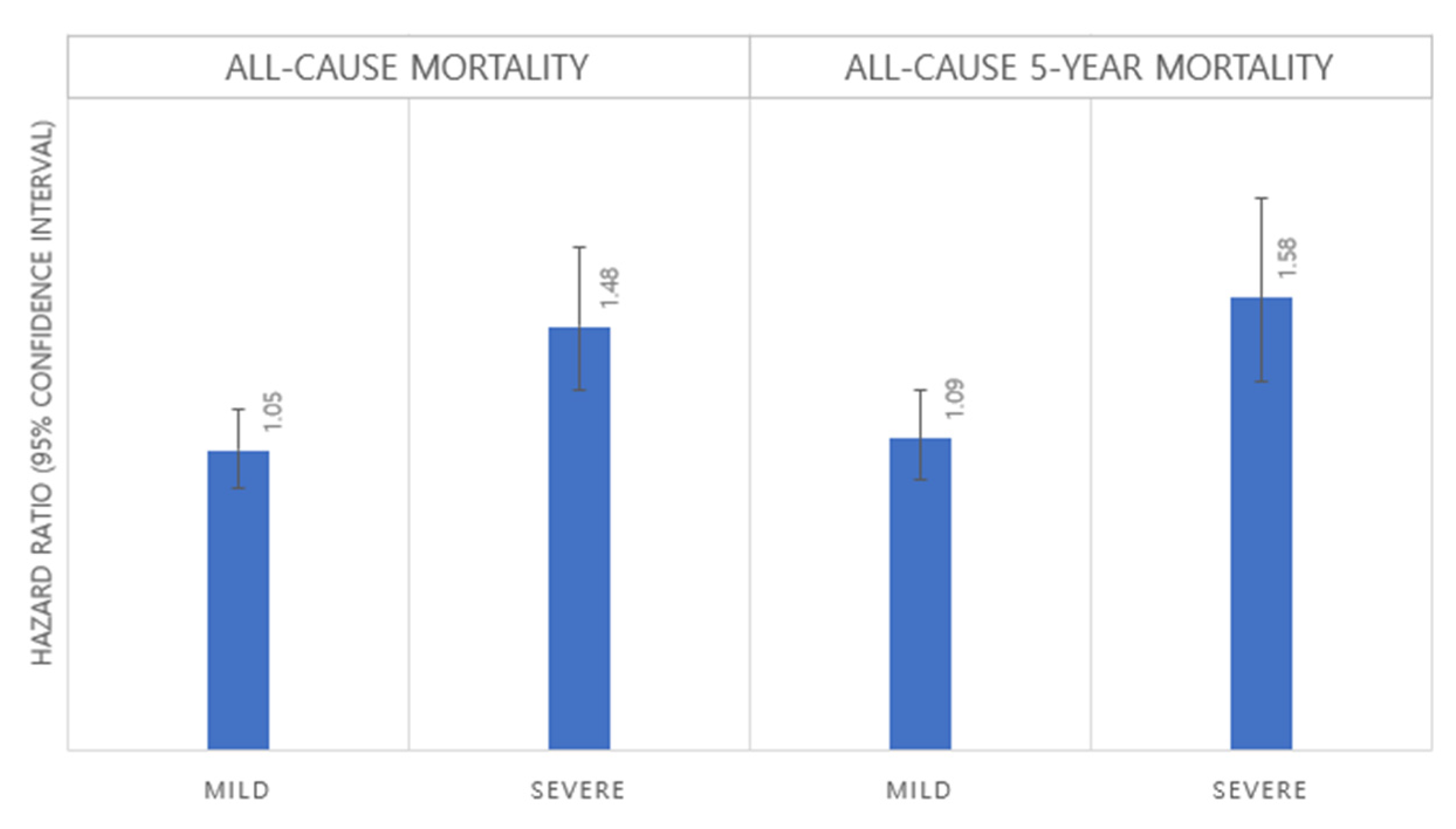
| Disability severity | Disability | ||||||
| Mild | No | 1.00 | 1.00 | ||||
| Yes | 1.05 | (0.92 | 1.19) | 1.09 | (0.95 | 1.26) | |
| Severe | No | 1.00 | 1.00 | ||||
| Yes | 1.48 | (1.24 | 1.76) | 1.58 | (1.29 | 1.93) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, W.-R.; Han, K.-T.; Choi, M.; Kim, W. Disparities in All-Cause Mortality in Older Patients with Colorectal Cancer According to Disability Status: A Nationwide Analysis. Curr. Oncol. 2022, 29, 7430-7438. https://doi.org/10.3390/curroncol29100584
Lee W-R, Han K-T, Choi M, Kim W. Disparities in All-Cause Mortality in Older Patients with Colorectal Cancer According to Disability Status: A Nationwide Analysis. Current Oncology. 2022; 29(10):7430-7438. https://doi.org/10.3390/curroncol29100584
Chicago/Turabian StyleLee, Woo-Ri, Kyu-Tae Han, Mingee Choi, and Woorim Kim. 2022. "Disparities in All-Cause Mortality in Older Patients with Colorectal Cancer According to Disability Status: A Nationwide Analysis" Current Oncology 29, no. 10: 7430-7438. https://doi.org/10.3390/curroncol29100584
APA StyleLee, W.-R., Han, K.-T., Choi, M., & Kim, W. (2022). Disparities in All-Cause Mortality in Older Patients with Colorectal Cancer According to Disability Status: A Nationwide Analysis. Current Oncology, 29(10), 7430-7438. https://doi.org/10.3390/curroncol29100584





