Occurrence of Arrhythmias in Women with Thyroid Cancer Receiving Suppressive Doses of Levothyroxine
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- (1)
- While maintaining normal free triiodothyronine concentrations, the use of suppressive doses of levothyroxine in patients after thyroidectomy for differentiated thyroid cancer does not cause statistically significant changes in maximum, average, or minimum heart rate.
- (2)
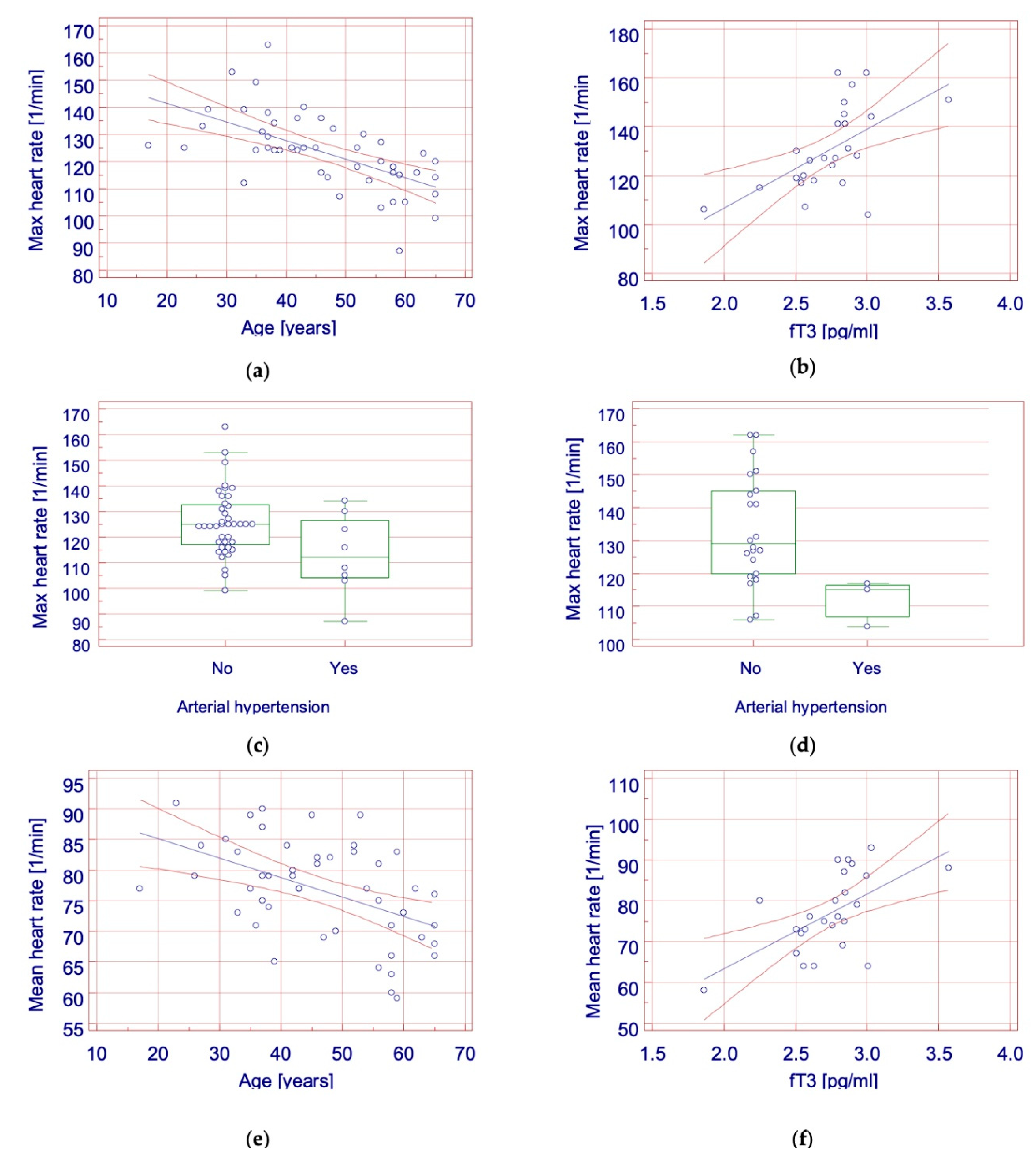
- The heart rate in patients with full TSH suppression depended on age and the presence of arterial hypertension. In patients with partial TSH suppression, no correlation was found between TSH activity and heart rate. The heart rate in the control group depended on free triiodothyronine concentration and the presence of arterial hypertension.
- (3)
- The use of suppressive doses of levothyroxine in patients after thyroidectomy for differentiated thyroid carcinoma does not significantly increase the risk of supraventricular or ventricular extrasystoles, or paroxysmal supraventricular tachycardia.
- (4)
- The use of TSH suppression after surgical treatment of differentiated thyroid carcinomas is safe in terms of arrhythmia induction and does not provoke clinically significant arrhythmia.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- DeLellis, R.A.; Lloyd, R.V.; Heitz, P.U. Pathology and Genetics: Tumors of Endocrine Organs; WHO classification of Tumors; IARC Press: Lyon, France, 2004. [Google Scholar]
- Wierzchowski, W.; Stachura, J. Endocrine gland diseases. In Pathology Means a Word about Disease; Stachura, J., Domagała, W., Eds.; Polska Akademia Umiejętności: Kraków, Poland, 2009; pp. 1111–1113. [Google Scholar]
- Schlumberger, M.J. Papillary and follicular thyroid carcinoma. N. Engl. J. Med. 1998, 338, 297–306. [Google Scholar] [CrossRef]
- Wojciechowska, U.; Didkowska, J. Zachorowania i Zgony na Nowotwory złośliwe w Polsce. Krajowy Rejestr Nowotworów, Centrum Onkologii-Instytut im. Marii Skłodowskiej-Curie. Available online: http://onkologia.org.pl/raporty/ (accessed on 16 January 2018).
- Jarząb, B.; Sporny, S.; Lange, D.; Włoch, J.; Lewiński, A.; Bałdys-Waligórska, A.; Barczyński, M.; Bręborowicz, D.; Brzeziński, J.; Bruszewska, E.; et al. Diagnosis and treatment of thyroid cancer—Polish recommendations. Endokrynol. Pol. 2010, 61, 518–568. [Google Scholar] [PubMed]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef]
- Jarząb, B.; Płaczkiewicz-Jankowska, E. Thyroid Cancer. In Interna Szczeklika; Gajewski, P., Ed.; Medycyna Praktyczna: Kraków, Poland, 2018; pp. 91–101, 1344–1349, TabI.B.5–13. [Google Scholar]
- Polikar, R.; Burger, A.G.; Scherrer, U.; Nicod, P. The thyroid and the heart. Circulation 1993, 87, 1435–1441. [Google Scholar] [CrossRef] [PubMed]
- Dewland, T.A.; Vittinghoff, E.; Mandyam, M.C.; Heckbert, S.R.; Siscovick, D.S.; Stein, P.K.; Psaty, B.M.; Sotoodehnia, N.; Gottdiener, J.S.; Marcus, G.M. Atrial ectopy as a predictor of incident atrial fibrillation: A cohort study. Ann. Intern. Med. 2013, 159, 721. [Google Scholar] [CrossRef]
- Biondi, B.; Palmieri, E.A.; Fazio, S.; Cosco, C.; Nocera, M.; Saccà, L.; Filetti, S.; Lombardi, G.; Perticone, F. Endogenous subclinical hyperthyroidism affects quality of life and cardiac morphology and function in young and middle-aged patients. J. Clin. Endocrinol. Metab. 2000, 85, 4701–4705. [Google Scholar]
- Sawin, C.T.; Geller, A.; Wolf, P.A.; Belanger, A.J.; Baker, E.; Bacharach, P.; Wilson, P.W.; Benjamin, E.J.; D’Agostino, R.B. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N. Engl. J. Med. 1994, 331, 1249–1252. [Google Scholar] [CrossRef] [PubMed]
- Forfar, J.C.; Miller, H.C.; Toft, A.D. Occult thyrotoxicosis: A reversible cause of “idiopathic” atrial fibrillation. Am. J. Cardiol. 1979, 44, 9–12. [Google Scholar] [CrossRef]
- Goodwin, J.F. Thyrotoxic auricular fibrillation treated with thiouracil. Br. Med. J. 1949, 1, 895–897. [Google Scholar] [CrossRef][Green Version]
- Woeber, K.A. Thyrotoxicosis and the heart. N. Engl. J. Med. 1992, 327, 94–98. [Google Scholar] [PubMed]
- Haïssaguerre, M.; Jaïs, P.; Shah, D.C.; Takahashi, A.; Hocini, M.; Quiniou, G.; Garrigue, S.; Le Mouroux, A.; Le Métayer, P.; Clémenty, J. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N. Engl. J. Med. 1998, 339, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Auer, J.; Scheibner, P.; Mische, T.; Langsteger, W.; Eber, O.; Eber, B. Subclinical hyperthyroidism as a risk factor for atrial fibrillation. Am. Heart J. 2001, 142, 838–842. [Google Scholar] [CrossRef] [PubMed]
- Biondi, B.; Fazio, S.; Carella, C.; Amato, G.; Cittadini, A.; Lupoli, G.; Saccà, L.; Bellastella, A.; Lombardi, G. Cardiac effects of long term thyrotropin-suppressive therapy with levo-thyroxine. J. Clin. Endocrinol. Metab. 1993, 77, 334–338. [Google Scholar] [PubMed]
- Shapiro, L.E.; Sievert, R.; Ong, L.; Ocampo, L.E.; Chance, R.A.; Lee, M.; Nanna, M.; Ferrick, K.; Surks, M.I. Minimal cardiac effects in asymptomatic athyreotic patients chronically treated with thyrotropin-suppressive doses of L-thyroxine. J. Clin. Endocrinol. Metab. 1997, 82, 2592–2595. [Google Scholar] [CrossRef] [PubMed]
- Ching, G.W.; Franklyn, J.A.; Stallard, T.J.; Daykin, J.; Sheppard, M.C.; Gammage, M.D. Cardiac hypertrophy as a result of long-term thyroxine therapy and thyrotoxicosis. Heart 1996, 75, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Berghout, A.; van de Wetering, J.; Klootwijk, P. Cardiac and metabolic effects in patients who present with a multinodular goitre. Neth. J. Med. 2003, 61, 318–322. [Google Scholar] [PubMed]
- Abonowara, A.; Quraishi, A.; Sapp, J.L.; Alqambar, M.H.; Saric, A.; O’Connell, C.M.; Rajaraman, M.M.; Hart, R.D.; Imran, S.A. Prevalence of atrial fibrillation in patients taking TSH suppression therapy for management of thyroid cancer. Clin. Investig. Med. 2012, 35, 152–156. [Google Scholar] [CrossRef]
- Klein Hesselink, E.N.; Lefrandt, J.D.; Schuurmans, E.P.; Burgerhof, J.G.; Groen, B.; Gansevoort, R.T.; van der Horst-Schrivers, A.N.; Dullaart, R.P.; Van Gelder, I.C.; Brouwers, A.H.; et al. Increased risk of atrial fibrillation after treatment for differentiated thyroid carcinoma. J. Clin. Endocrinol. Metab. 2015, 100, 4563–4569. [Google Scholar] [CrossRef]
- Gammage, M.D.; Parle, J.V.; Holder, R.L.; Roberts, L.M.; Hobbs, F.D.; Wilson, S.; Sheppard, M.C.; Franklyn, J.A. Association between serum free thyroxine concentration and atrial fibrillation. Arch. Intern. Med. 2007, 167, 928–934. [Google Scholar] [CrossRef]
- Selmer, C.; Olesen, J.B.; Hansen, M.L.; Lindhardsen, J.; Olsen, A.M.; Madsen, J.C.; Faber, J.; Hansen, P.R.; Pedersen, O.D.; Torp-Pedersen, C.; et al. The spectrum of thyroid disease and risk of new onset atrial fibrillation: A large population cohort study. BMJ 2012, 345, 7895. [Google Scholar] [CrossRef] [PubMed]
- Cappola, A.R.; Fried, L.P.; Arnold, A.M.; Danese, M.D.; Kuller, L.H.; Burke, G.L.; Tracy, R.P.; Ladenson, P.W. Thyroid status, cardiovascular risk, and mortality in older adults. JAMA 2006, 295, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Nanchen, D.; Gussekloo, J.; Westendorp, R.G.; Stott, D.J.; Jukema, J.W.; Trompet, S.; Ford, I.; Welsh, P.; Sattar, N.; Macfarlane, P.W.; et al. Subclinical thyroid dysfunction and the risk of heart failure in older persons at high cardiovascular risk. J. Clin. Endocrinol. Metab. 2012, 97, 852–861. [Google Scholar] [CrossRef]
- Rabbia, F.; Silke, B.; Conterno, A.; Grosso, T.; De Vito, B.; Rabbone, I.; Chiandussi, L.; Veglio, F. Assessment of cardiac autonomic modulation during adolescent obesity. Obes. Res. 2003, 11, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Freitas, I.M.; Miranda, J.A.; Mira, P.A.; Lanna, C.M.; Lima, J.R.; Laterza, M.C. Cardiac autonomic dysfunction in obese normotensive children and adolescents. Rev. Paul. Pediatr. 2014, 32, 244–249. [Google Scholar] [CrossRef]
- Nagai, N.; Matsumoto, T.; Kita, H.; Moritani, T. Autonomic nervous system activity and the state and development of obesity in Japanese school children. Obes. Res. 2003, 11, 25–32. [Google Scholar] [CrossRef]
- Khrisanapant, W.; Sengmeuang, P.; Pasurivong, O.; Kukongviriyapan, U. Does cardiac autonomic modulation exist in obese adolescents? Srinagarind. Med. J. 2008, 23, 234–239. [Google Scholar]
- Karasoy, D.; Bo Jensen, T.; Hansen, M.L.; Schmiegelow, M.; Lamberts, M.; Gislason, G.H.; Hansen, J.; Torp-Pedersen, C.; Olesen, J. Obesity is a risk factor for atrial fibrillation among fertile young women: A nationwide cohort study. Europace 2013, 15, 781–786. [Google Scholar] [CrossRef] [PubMed]
- Berkovitch, A.; Kivity, S.; Klempfner, R.; Segev, S.; Milwidsky, A.; Erez, A.; Sabbag, A.; Goldenberg, I.; Sidi, Y.; Maor, E. Body mass index and the risk of new-onset atrial fibrillation in middle-aged adults. Am. Heart J. 2016, 173, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Choi, E.K.; Lee, S.H.; Han, K.D.; Rhee, T.M.; Park, C.S.; Lee, S.R.; Choe, W.S.; Lim, W.H.; Kang, S.H.; et al. Atrial fibrillation risk in metabolically healthy obesity: A nationwide population-based study. Int. J. Cardiol. 2017, 240, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Foy, A.J.; Mandrola, J.; Liu, G.; Naccarelli, G.V. Relation of obesity to new-onset atrial fibrillation and atrial flutter in adults. Am. J. Cardiol. 2018, 121, 1072–1075. [Google Scholar] [CrossRef] [PubMed]
- Huxley, R.R.; Lopez, F.L.; Folsom, A.R.; Agarwal, S.K.; Loehr, L.R.; Soliman, E.Z.; Maclehose, R.; Konety, S.; Alonso, A. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: The atherosclerosis risk in communities (ARIC) study. Circulation 2011, 123, 1501–1508. [Google Scholar] [CrossRef]
- Zhang, Y.; Post, W.S.; Cheng, A.; Blasco-Colmenares, E.; Tomaselli, G.F.; Guallar, E. Thyroid Hormones and Electrocardiographic Parameters: Findings from the Third National Health and Nutrition Examination Survey. PLoS ONE 2013, 8, 59489. [Google Scholar]
| Arrhythmia | Age | |||
|---|---|---|---|---|
| 16–30 Years | 31–40 Years | 41–60 Years | >60 Years | |
| SVES | <50 | <50 | <100 | <100 |
| VES | <50 | <50 | <50 | <100 |
| PSVT | 0 | 0 | 0 | 0 |
| AF | 0 | 0 | 0 | 0 |
| Variable | Fully Suppressed TSH (n = 48) | Partially Suppressed TSH (n = 25) | Control Group (n = 25) | p-Value | Post Hoc |
|---|---|---|---|---|---|
| Age [years] | 46 (37–58) | 45 (40–56) | 32 (26–57) | 0.28 | |
| Hemoglobin [g/dL] | 13.34 (0.94) | 13.26 (1.19) | 13.56 (0.73) | 0.50 | |
| Total calcium [mmol/L] | 2.38 (0.14) | 2.36 (0.11) | 2.41 (0.11) | 0.37 | |
| Potassium [mEq/L] | 4.22 (0.28) | 4.27 (0.32) | 4.3 (0.37) | 0.58 | |
| Levothyroxine dose [μg/day] | 132.14 (116–150) | 121.43 (100–153) | NA | 0.59 | |
| TSH [µU/mL] | 0.025 (0.0096–0.046) | 0.224 (0.136–0.295) | 1.121 (0.778–1.505) | <0.001 | A≠B≠C |
| fT3 [pg/mL] | 2.84 (0.38) | 2.7 (0.33) | 2.74 (0.31) | 0.22 | |
| Arterial hypertension | |||||
| 8 (16.7) | 5 (20) | 3 (12) | 0.74 | ||
| Thyroid cancer | |||||
| Papillary | 41 (85.4) | 25 (92) | NA | 0.42 | |
| Other types | 7 (14.6) | 2 (8) | NA | ||
| Variable | Fully Suppressed TSH (n = 48) | Partially Suppressed TSH (n = 25) | Control Group (n = 25) | p-Value |
|---|---|---|---|---|
| Heart rate [1/min] | ||||
| Maximum | 123.5 (13.93) | 123.48 (12.62) | 130.76 (17.14) | 0.10 |
| Minimum | 52 (48.5–56) | 52 (47.75–57.25) | 48 (44.75–55.5) | 0.10 |
| Mean | 76.73 (8.12) | 77.12 (6.12) | 76.96 (9.56) | 0.98 |
| Arrhythmias | ||||
| SVES | 6 (12.5) | 4 (16) | 3 (12) | 0.90 |
| VES | 4 (8.3) | 0 (0) | 2 (8) | 0.33 |
| PSVT | 4 (8.3) | 3 (12) | 3 (12) | 0.84 |
| Variable | Fully Suppressed (n = 48) | Partially Suppressed (n = 25) | Control Group (n = 25) | |||
|---|---|---|---|---|---|---|
| Maximum heart rate | ||||||
| Pearson’s correlation | p-Value | r | p-Value | r | p-Value | r |
| Age | <0.001 | –0.609 | 0.11 | –0.324 | 0.32 | 0.206 |
| Hemoglobin | 0.6 | –0.078 | 0.85 | 0.040 | 0.81 | –0.050 |
| Total calcium | 0.26 | –0.167 | 0.78 | –0.059 | 0.46 | –0.160 |
| Potassium | 0.77 | –0.044 | 0.43 | –0.166 | 0.40 | –0.179 |
| Levothyroxine dose | 0.62 | –0.074 | 0.3 | –0.201 | Nd | Nd |
| TSH | 0.17 | 0.200 | 0.79 | –0.057 | 0.21 | 0.259 |
| fT3 | 0.39 | 0.127 | 0.91 | 0.226 | 0.002 | 0.582 |
| Mann-Whitney U test | p-Value | p-Value | p-Value | |||
| Cancer type | 0.21 | NA | 0.88 | NA | NA | NA |
| Arterial hypertension | 0.048 | NA | 0.95 | NA | 0.02 | NA |
| Minimum heart rate | ||||||
| Pearson’s correlation | p-Value | r | p-Value | r | p-Value | r |
| Age | 0.43 | –0.116 | 0.24 | 0.243 | 0.84 | –0.043 |
| Hemoglobin | 0.85 | 0.029 | 0.94 | 0.015 | 0.95 | –0.012 |
| Total calcium | 0.85 | 0.028 | 0.33 | –0.204 | 0.78 | 0.059 |
| Potassium | 0.46 | 0.109 | 0.62 | –0.105 | 0.90 | –0.027 |
| Levothyroxine dose | 0.73 | –0.052 | 0.80 | –0.053 | NA | NA |
| TSH | 0.37 | 0.133 | 0.32 | 0.209 | 0.20 | 0.267 |
| fT3 | 0.58 | 0.081 | 0.91 | 0.024 | 0.18 | 0.280 |
| Mann-Whitney U test | p-Value | p-Value | p-Value | |||
| Cancer type | 0.14 | NA | 0.21 | NA | NA | NA |
| Arterial hypertension | 0.41 | NA | 0.97 | NA | 0.83 | NA |
| Mean heart rate | ||||||
| Pearson’s correlation | p value | r | p value | r | p value | r |
| Age | 0.001 | –0.486 | 0.56 | –0.124 | 0.23 | –0.247 |
| Hemoglobin | 0.71 | –0.056 | 0.46 | 0.156 | 0.68 | 0.088 |
| Total calcium | 0.08 | –0.256 | 0.31 | 0.211 | 0.97 | 0.009 |
| Potassium | 0.82 | –0.034 | 0.63 | –0.101 | 0.44 | –0.165 |
| Levothyroxine dose | 0.45 | –0.111 | 0.19 | –0.273 | NA | NA |
| TSH | 0.15 | 0.212 | 0.32 | 0.208 | 0.74 | 0.071 |
| fT3 | 0.25 | 0.170 | 0.40 | 0.177 | 0.002 | 0.594 |
| Mann-Whitney U test | p-Value | p-Value | p-Value | |||
| Cancer type | 0.07 | NA | 0.88 | NA | NA | NA |
| Arterial hypertension | 0.12 | NA | 0.50 | NA | 0.3 | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaziród-Wolski, K.; Kowalska, A.; Sielski, J.; Biskup-Frużyńska, M.; Piotrowski, G. Occurrence of Arrhythmias in Women with Thyroid Cancer Receiving Suppressive Doses of Levothyroxine. Curr. Oncol. 2021, 28, 5009-5018. https://doi.org/10.3390/curroncol28060420
Kaziród-Wolski K, Kowalska A, Sielski J, Biskup-Frużyńska M, Piotrowski G. Occurrence of Arrhythmias in Women with Thyroid Cancer Receiving Suppressive Doses of Levothyroxine. Current Oncology. 2021; 28(6):5009-5018. https://doi.org/10.3390/curroncol28060420
Chicago/Turabian StyleKaziród-Wolski, Karol, Aldona Kowalska, Janusz Sielski, Magdalena Biskup-Frużyńska, and Grzegorz Piotrowski. 2021. "Occurrence of Arrhythmias in Women with Thyroid Cancer Receiving Suppressive Doses of Levothyroxine" Current Oncology 28, no. 6: 5009-5018. https://doi.org/10.3390/curroncol28060420
APA StyleKaziród-Wolski, K., Kowalska, A., Sielski, J., Biskup-Frużyńska, M., & Piotrowski, G. (2021). Occurrence of Arrhythmias in Women with Thyroid Cancer Receiving Suppressive Doses of Levothyroxine. Current Oncology, 28(6), 5009-5018. https://doi.org/10.3390/curroncol28060420





