The Impact of COVID-19 on the Diagnosis and Treatment of Lung Cancer at a Canadian Academic Center: A Retrospective Chart Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
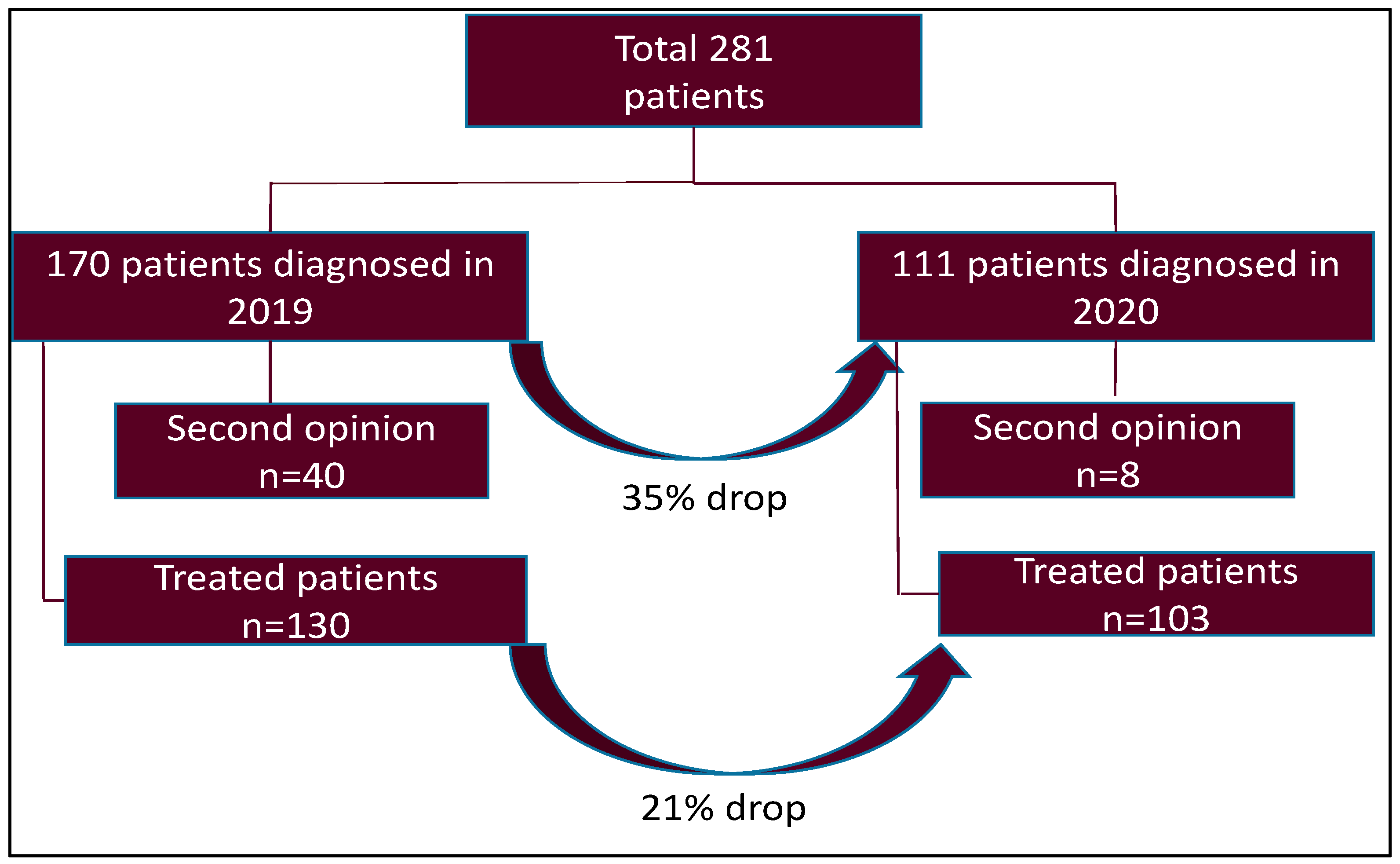
- Pre-COVID-19 cohort of patients diagnosed between 1 March 2019 and 29 February 2020.
- COVID-19 cohort of patients diagnosed between 1 March 2020 and 28 February 2021.
2.2. The Primary Objective
- To investigate the impact of the COVID-19 pandemic on lung cancer diagnoses and the lung cancer care trajectory of patients being treated at the Peter Brojde Lung Cancer Center by comparing the year 2019 to 2020.
2.3. Secondary Objectives
- To evaluate and compare the local wait times to the recommended guidelines before and during the COVID-19 era, and determine any repercussions of the COVID-19 pandemic on lung cancer care.
- To characterize any lung cancer treatment pattern changes attributed to the COVID-19 pandemic.
2.4. Data Collection
- Demographics: age, sex, smoking history;
- Diagnosis timing: referral date, date of first lung specialist consult, date of diagnosis;
- Disease characteristics: stage, histopathological diagnosis, molecular testing results;
- Treatment history: referral date, type of first definitive treatment (chemotherapy, radiotherapy, or surgery), start and end date of treatment.
2.5. Definitions of Wait Times
2.6. Statistical Analysis
3. Results
3.1. Wait Times
3.2. Molecular Testing
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jazieh, A.R.; Akbulut, H.; Curigliano, G.; Rogado, A.; Alsharm, A.A.; Razis, E.D.; Mula-Hussain, L.; Errihani, H.; Khattak, A.; De Guzman, R.B.; et al. Impact of the COVID-19 Pandemic on Cancer Care: A Global Collaborative Study. JCO Glob. Oncol. 2020, 6, 1428–1438. [Google Scholar] [CrossRef]
- Patt, D.; Gordan, L.; Diaz, M.; Okon, T.; Grady, L.; Harmison, M.; Markward, N.; Sullivan, M.; Peng, J.; Zhou, A. Impact of COVID-19 on Cancer Care: How the Pandemic Is Delaying Cancer Diagnosis and Treatment for American Seniors. JCO Clin. Cancer Inform. 2020, 4, 1059–1071. [Google Scholar] [CrossRef]
- QC Gouvernement. Analyse des Répercussions de la Pandémie de la COVID-19 sur les Soins et les Services en Cancérologie au Québec. 2020. Available online: https://publications.msss.gouv.qc.ca/msss/fichiers/2020/20-210-378W.pdf (accessed on 15 May 2021).
- Garassino, M.C.; Whisenant, J.G.; Huang, L.-C.; Trama, A.; Torri, V.; Agustoni, F.; Baena, J.; Banna, G.; Berardi, R.; Bettini, A.C.; et al. COVID-19 in patients with thoracic malignancies (TERAVOLT): First results of an international, registry-based, cohort study. Lancet Oncol. 2020, 21, 914–922. [Google Scholar] [CrossRef]
- Di Girolamo, C.; Walters, S.; Gildea, C.; Majano, S.B.; Rachet, B.; Morris, M. Can we assess Cancer Waiting Time targets with cancer survival? A population-based study of individually linked data from the National Cancer Waiting Times monitoring dataset in England, 2009–2013. PLoS ONE 2018, 13, e0201288. [Google Scholar] [CrossRef]
- Olsson, J.K.; Schultz, E.M.; Gould, M.K. Timeliness of care in patients with lung cancer: A systematic review. Thorax 2009, 64, 749–756. [Google Scholar] [CrossRef]
- Spurgeon, P.; Barwell, F.; Kerr, D. Waiting times for cancer patients in England after general practitioners’ referrals: Retrospective national survey. BMJ 2000, 320, 838–839. [Google Scholar] [CrossRef][Green Version]
- Minhas, R. Hitting the target and missing the point? Int. J. Clin. Pract. 2009, 63, 1275–1277. [Google Scholar] [CrossRef]
- Malin, J.L.; Asch, S.M.; Kerr, E.A.; McGlynn, E.A. Evaluating the quality of cancer care: Development of cancer quality indicators for a global quality assessment tool. Cancer 2000, 88, 701–707. [Google Scholar] [CrossRef]
- 2020 Canadian Cancer Statistics Special Report-EN. Available online: http://cancer.ca/Canadian-Cancer-Statistics-2020-EN (accessed on 10 May 2021).
- Tartarone, A.; Lerose, R. COVID-19 and cancer care: What do international guidelines say? Med. Oncol. 2020, 37, 1–5. [Google Scholar] [CrossRef]
- The Lung Cancer Working Party of The British Thoracic Society Standards of Care Committee BTS recommendations to respiratory physicians for organising the care of patients with lung cancer. Thorax 1998, 53 (Suppl. 1), S1–S8. [CrossRef]
- National Health Service. National Cancer Waiting Times Monitoring Dataset Guidance. 2020. Available online: https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2020/09/national-cancer-waiting-times-monitoring-dataset-guidance-v11-sep2020.pdf (accessed on 10 May 2021).
- Reyes, R.; López-Castro, R.; Auclin, E.; García, T.; Chourio, M.; Rodriguez, A.; López, L.; Laguna, J.; Lucena, C.; Molins, L.; et al. MA03.08 Impact of COVID-19 Pandemic in the Diagnosis and Prognosis of Lung Cancer. J. Thorac. Oncol. 2021, 16, S141. [Google Scholar] [CrossRef]
- Bissonnette, J.-P.; Sun, A.; Grills, I.S.; Almahariq, M.F.; Geiger, G.; Vogel, W.; Sonke, J.-J.; Everitt, S.; Mac Manus, M. Non-small cell lung cancer stage migration as a function of wait times from diagnostic imaging: A pooled analysis from five international centres. Lung Cancer 2021, 155, 136–143. [Google Scholar] [CrossRef]
- Depypere, L.P.; Daddi, N.; Gooseman, M.R.; Batirel, H.F.; Brunelli, A. The impact of coronavirus disease 2019 on the practice of thoracic oncology surgery: A survey of members of the European Society of Thoracic Surgeons (ESTS). Eur. J. Cardio-Thorac. Surg. 2020, 58, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Blais, N.; Bouchard, M.; Chinas, M.; Lizotte, H.; Morneau, M.; Spicer, J.; Martel, S. Consensus Statement: Summary of the Quebec Lung Cancer Network Recommendations for Prioritizing Patients with Thoracic Cancers in the Context of the COVID-19 Pandemic. Curr. Oncol. 2020, 27, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Dingemans, A.-M.C.; Soo, R.A.; Jazieh, A.R.; Rice, S.J.; Kim, Y.T.; Teo, L.L.; Warren, G.W.; Xiao, S.-Y.; Smit, E.F.; Aerts, J.G.; et al. Treatment Guidance for Patients With Lung Cancer During the Coronavirus 2019 Pandemic. J. Thorac. Oncol. 2020, 15, 1119–1136. [Google Scholar] [CrossRef]
- Hilzenrat, R.A.; Deen, S.A.; Yee, J.; Grant, K.A.; Ashrafi, A.S.; Coughlin, S.; McGuire, A.L. Thoracic Surgeon Impressions of the Impact of the COVID-19 Pandemic on Lung Cancer Care—Lessons from the First Wave in Canada. Curr. Oncol. 2021, 28, 940–949. [Google Scholar] [CrossRef]
- Martínez-Hernández, N.J.; Caballero Silva, U.; Cabañero Sánchez, A.; Campo-Cañaveral de la Cruz, J.L.; Obeso Carillo, A.; Jarabo Sarceda, J.R.; Sevilla López, S.; Cilleruelo Ramos, Á.; Recuero Díaz, J.L.; Call, S.; et al. Effect of COVID-19 on Thoracic Oncology Surgery in Spain: A Spanish Thoracic Surgery Society (SECT) Survey. Cancers 2021, 13, 2897. [Google Scholar] [CrossRef]
- Antonoff, M.; Backhus, L.; Boffa, D.J.; Broderick, S.R.; Brown, L.M.; Carrott, P.; Clark, J.M.; Cooke, D.; David, E.; Facktor, M.; et al. COVID-19 guidance for triage of operations for thoracic malignancies: A consensus statement from Thoracic Surgery Outcomes Research Network. J. Thorac. Cardiovasc. Surg. 2020, 160, 601–605. [Google Scholar] [CrossRef]
- Zaniboni, A.; Ghidini, M.; Grossi, F.; Indini, A.; Trevisan, F.; Iaculli, A.; Dottorini, L.; Moleri, G.; Russo, A.; Vavassori, I.; et al. A Review of Clinical Practice Guidelines and Treatment Recommendations for Cancer Care in the COVID-19 Pandemic. Cancers 2020, 12, 2452. [Google Scholar] [CrossRef]
- Nadpara, P.A.; Madhavan, S.S.; Tworek, C. Disparities in Lung Cancer Care and Outcomes among Elderly in a Medically Underserved State Population—A Cancer Registry-Linked Database Study. Popul. Health Manag. 2016, 19, 109–119. [Google Scholar] [CrossRef]
- Hubert, J.; Bourdages-Pageau, E.; Garneau, C.A.P.; Labbé, C.; Ugalde, P.A. Enhanced recovery pathways in thoracic surgery: The Quebec experience. J. Thorac. Dis. 2018, 10, S583–S590. [Google Scholar] [CrossRef]
- Quarterman, R.L.; McMillan, A.; Ratcliffe, M.B.; Block, M.I. Effect of preoperative delay on prognosis for patients with early stage non-small cell lung cancer. J. Thorac. Cardiovasc. Surg. 2003, 125, 108–114. [Google Scholar] [CrossRef]
- Fujita, K.; Ito, T.; Saito, Z.; Kanai, O.; Nakatani, K.; Mio, T. Impact of COVID-19 pandemic on lung cancer treatment scheduling. Thorac. Cancer 2020, 11, 2983–2986. [Google Scholar] [CrossRef]
| Wait Time | Mean Time (Days) | Guidelines |
|---|---|---|
| Referral → Lung cancer specialist | 14 | National Health Service [13] |
| Referral → Diagnosis | 30 | British Thoracic Society [12] |
| Referral → First treatment | 62 | National Health Service |
| Diagnosis → First treatment | 30 | British Thoracic Society |
| Decision-to-treat → First definitive treatment | 31 | British Thoracic Society |
| Diagnosis → First chemotherapy | 28 | British Thoracic Society |
| Surgery consult → Surgery | 28 | British Thoracic Society |
| Radiation consult → First radiation therapy | 42 | RAND Corporation [9] |
| Characteristics | 2019 n = 130 | 2020 n = 103 | |
|---|---|---|---|
| Age (mean; range) | 70 (40–96) | 71 (42–92) | |
| Sex (male/female) | 73/57 | 56/47 | |
| Cancer stage (n/%) | Early stage (T1–3N0–1M0) Locoregional (T1–4N2–3M0) Advanced/metastatic stage (TanyNanyM1) | 42 (32) 20 (15) 68 (53) | 33 (35) 11 (10) 59 (55) |
| Smoking history (n/%) | Former/current smoker Non-smoker | 99 (76) 1 31 (24) | 74 (74) 29 (26) |
| Treatment type: (n/%) | FDT 2 PT 3 | 110 (85) 20 (15) | 84 (82) 19 (18) |
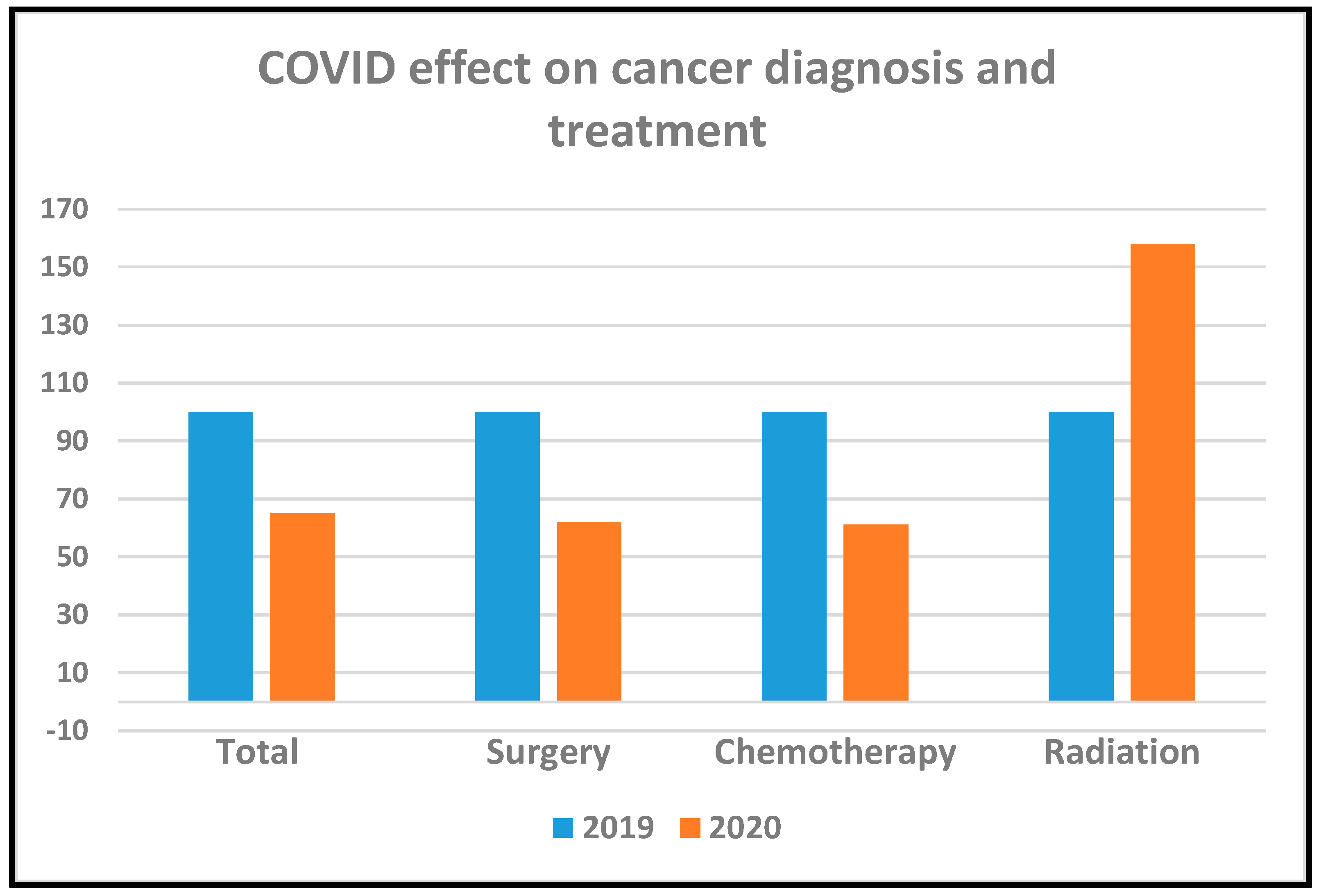
| Type of First Treatment | 2019 n = 110 | 2020 n = 84 | p-Value | |
|---|---|---|---|---|
| Radiosurgery (n/%) | 8 (7) | 18 (21) | <0.05 | |
| Chemotherapy (n/%): | Total Standard systemic chemotherapy Immunotherapy ± chemotherapy Targeted therapy | 60 (54) 21 (37) 23 (36) 17 (27) | 40 (47) 12 (30) 16 (40) 12 (30) | 0.07 |
| Surgery | 42 (38) | 26 (25) | 0.09 | |
| Interval | Recommended Wait Times (days) | 2019 n = 130 | 2020 n = 103 | p-Value | ||
|---|---|---|---|---|---|---|
| n | Mean (SD 1) Days | n | Mean (SD 1) Days | |||
| Referral → Lung cancer specialist | 14 | 130 | 12 (14) | 103 | 11 (13) | 0.67 |
| Referral → Diagnosis | 30 | 130 | 59 (51) | 103 | 59 (67) | 0.94 |
| Referral → First treatment | 62 | 130 | 79 (47) | 103 | 82 (71) | 0.76 |
| Wait for path report | - | 130 | 8 (7.3) | 103 | 8 (7.6) | 0.98 |
| Decision-to-treat to FDT 2 | 31 | 130 | 52 (48) | 103 | 51 (61) | 0.94 |
| Diagnosis to chemotherapy | 28 | 64 | 38 (25) | 39 | 34 (24) | 0.95 |
| Diagnosis to RT 3 | 42 | 24 | 35 (30) | 38 | 46 (33) | 0.31 |
| Surgical consult to surgery | 28 | 42 | 64 (43) | 27 | 76 (83) | 0.04 |
| Wait for molecular test results | 7 | 73 | 21.9 (9.9) | 51 | 21.6 (8.7) | 0.90 |
| Interval | Recommended Wait Time | 2019 | 2020 | p-Value |
|---|---|---|---|---|
| Proportion (%) | ||||
| Referral → Lung cancer specialist | 14 days | 90/130 (69) | 74/103 (72) | 0.35 |
| Referral → Diagnosis | 30 days | 52/130 (40) | 49/103 (48) | 0.15 |
| Referral → First treatment | 62 days | 56/130 (43) | 49/103 (48) | 0.29 |
| Diagnosis → First systemic chemotherapy 1 | 28 days | 24/64 (37) | 7/20 (35) | 0.45 |
| Diagnosis → First targeted chemotherapy | 28 days | 11/17 (64) | 5/7 (66) | 0.43 |
| Surgical consult → Surgery | 28 days | 6/42 (14) | 8/26 (30) | 0.12 |
| Radiation oncology consult → Radiation treatment | 42 days | 17/24 (71) | 30/38 (79) | 0.52 |
| Type of Molecular Test | 2019 n = 127 | 2020 n = 106 | p-Value | ||
|---|---|---|---|---|---|
| n | Mean (SD 1) Days | n | Mean (SD 1) Days | ||
| NGS 2 | 66 | 15 (6) | 62 | 18 (9) | 0.03 |
| Liquid biopsy | 9 | 6 (10) | 15 | 4 (18) | 0.81 |
| NanoString | 18 | 25 (11) | 19 | 27 (18) | 0.50 |
| Total | 100 | 16 (9) | 96 | 18 (14) | 0.11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kasymjanova, G.; Anwar, A.; Cohen, V.; Sultanem, K.; Pepe, C.; Sakr, L.; Friedmann, J.; Agulnik, J.S. The Impact of COVID-19 on the Diagnosis and Treatment of Lung Cancer at a Canadian Academic Center: A Retrospective Chart Review. Curr. Oncol. 2021, 28, 4247-4255. https://doi.org/10.3390/curroncol28060360
Kasymjanova G, Anwar A, Cohen V, Sultanem K, Pepe C, Sakr L, Friedmann J, Agulnik JS. The Impact of COVID-19 on the Diagnosis and Treatment of Lung Cancer at a Canadian Academic Center: A Retrospective Chart Review. Current Oncology. 2021; 28(6):4247-4255. https://doi.org/10.3390/curroncol28060360
Chicago/Turabian StyleKasymjanova, Goulnar, Aksa Anwar, Victor Cohen, Khalil Sultanem, Carmela Pepe, Lama Sakr, Jennifer Friedmann, and Jason S. Agulnik. 2021. "The Impact of COVID-19 on the Diagnosis and Treatment of Lung Cancer at a Canadian Academic Center: A Retrospective Chart Review" Current Oncology 28, no. 6: 4247-4255. https://doi.org/10.3390/curroncol28060360
APA StyleKasymjanova, G., Anwar, A., Cohen, V., Sultanem, K., Pepe, C., Sakr, L., Friedmann, J., & Agulnik, J. S. (2021). The Impact of COVID-19 on the Diagnosis and Treatment of Lung Cancer at a Canadian Academic Center: A Retrospective Chart Review. Current Oncology, 28(6), 4247-4255. https://doi.org/10.3390/curroncol28060360







